Abstract
Objective
To evaluate whether clinical anxiety in children presenting to a pediatric pain management center is associated with a poorer treatment response for those who completed pain-focused cognitive behavioral therapy (CBT).
Study design
The total sample consisted of 175 children, 40 of whom completed CBT for chronic pain. The Screen for Anxiety Related Emotional Disorders (SCARED) was completed at initial evaluation and outcome measures (average pain intensity and the Functional Disability Inventory [FDI]) were collected during the initial evaluation and at the end of CBT. Group differences in outcomes were examined following CBT. The role of anxiety in CBT initiation and completion was also explored.
Results
Presence of clinical anxiety was associated with greater initiation and/or completion of pain-focused CBT but also a poorer treatment response. Specifically, the group with subclinical anxiety exhibited a substantial reduction in pain intensity, and the group with clinical anxiety exhibited a more limited response to treatment (F (1, 36) = 13.68 p < 0.01). A similar effect was observed for FDI, such that the group with clinical anxiety had a significantly smaller response to treatment (F (1, 38) = 4.33 p < 0.05). The differences in pain and disability between groups following CBT suggest moderate effects (Cohen’s d = 0.77 and 0.78, respectively).
Conclusions
Although youth with clinical anxiety are more likely to start and/or complete pain-focused CBT, anxiety has an adverse impact on CBT treatment response in children with chronic pain. Identification of patients with anxiety and use of tailored behavioral interventions may improve clinical outcomes.
Keywords: pediatric pain, anxiety, cognitive behavioral therapy, treatment response
Chronic pain, or pain lasting for three months or longer, is highly prevalent in pediatric populations, impacting 15%-40% of youth (1, 2). Children with chronic pain may experience significant impairment, including increased healthcare utilization (3, 4), academic difficulties and social problems (3). For a large number of youth with chronic pain, symptoms persist for five years or longer (5-7). Cognitive behavioral therapy (CBT) focused on pain coping skills training is known to improve outcomes for youth with chronic pain in research trials (8-10) and in clinical settings (11, 12). CBT is of particular importance in pediatric chronic pain populations given the potential risks and side effects of pharmacotherapy for pain. Unfortunately, CBT remains ineffective for a significant portion (~25%) of youth with chronic pain (9, 11). Comorbid anxiety is thought to contribute to a failure to respond to treatment. For example, anxiety adversely impacts treatment response in adults with chronic pain (13) though literature is currently lacking in pediatric populations. Anxiety (14) is highly prevalent in children with chronic pain, affecting up to two thirds of this population (15-17). Youth with chronic pain and co-occurring anxiety may be at greatest risk for increased pain-related impairment (18, 19). At present, it is unknown if the presence of anxiety diminishes treatment response to standard CBT interventions for pediatric pain.
The purpose of this study was to evaluate the impact of anxiety on treatment response to CBT in a sample of pediatric pain patients. We hypothesized that patients who presented with clinically significant anxiety at their initial pain clinic evaluation would show less robust changes in treatment outcomes (functional disability, pain intensity) following a course of CBT compared with those who presented with subclinical levels of anxiety. A secondary aim was to determine the impact of anxiety on decisions to both participate in and complete CBT for chronic pain.
Methods
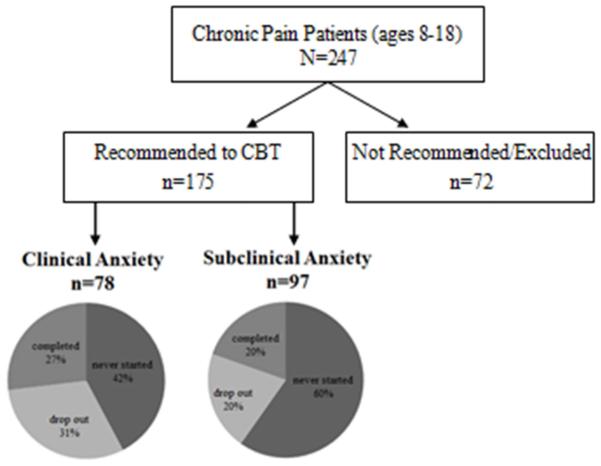
Participants were youth with chronic pain and their caregiver(s) who completed an evaluation at a multidisciplinary pain management center at a large Midwestern children’s hospital and were then referred to the pediatric behavioral medicine service to receive CBT for pain management. Two studies focusing on pain and disability outcomes and response to CBT in a larger sample of youth with chronic pain seen in our clinics have been published (11, 12). Participants in the current IRB-approved investigation (Figure 1) were included in this study if they: (1) reported pain for three months or greater during a pain clinic evaluation between November 2011 and October 2015; (2) were between 8 and 18 years of age; (3) were screened for the presence of anxiety; and (4) were recommended to complete a course of pain-focused CBT treatment at our institution.
Figure 1.
Youth with clinical anxiety more frequently utilize CBT for pain than youth with subclinical anxiety (χ2= 5.30, p < 0.05). Of the total population of 247 patients, 175 were recommended for CBT. Once participating in CBT, youth completed CBT at similar rates regardless of anxiety status.
The following demographic information was collected from the electronic medical record (EMR): sex, age, and pain diagnosis at the initial evaluation.
Screen for Child Anxiety Related Disorders – Child Report (SCARED) – the SCARED is a brief and widely used screening instrument to assess for the presence of clinically significant anxiety symptoms in youth based on the DSM-IV-TR (20) anxiety disorder diagnoses. The SCARED is validated for use in children ages 8 and above (21, 22), and in pediatric pain samples (19). Patients report the frequency of their anxiety symptoms over the past three months on a 41-item measure with responses including “Not True,” “Sometimes True,” and “Often True”. Total scores range from 0-82, with higher scores reflecting greater levels of anxiety. The presence of clinically significant anxiety was defined as a total score ≥25, which is the standard cut-off point based on psychometric research indicating optimal sensitivity and specificity (21, 22). This measure was collected at the initial pain clinic evaluation.
The following patient-reported measures were used to measure response to CBT in line with our prior research (11). These measures were collected at the initial pain clinic evaluation and during the final CBT treatment session.
The Functional Disability Inventory (FDI) (23) is a 15-item, self-report instrument assessing a child’s perception of his or her difficulty completing common daily activities because of pain. It has good evidence of psychometric validity and reliability (24, 25), has been used in multiple pediatric pain populations, and has limited clinician burden in terms of length, administration, scoring, and interpretation (25). Items are scored on a 5-point Likert scale, ranging from 0 to 4 (“No Trouble” to “Impossible”). Total scores range from 0 to 60. Higher scores indicate greater functional disability. Clinical cut-off scores were developed to represent no/minimal (≤12), moderate (13–29), and severe (≥30) levels of disability (26).
Average pain intensity in the past week was collected on a 0–10 numeric rating scale based on a validated pain assessment tool, the Brief Pain Inventory (BPI) (27, 28).
Procedure
As part of the standard multi-disciplinary pain clinic evaluation, patients completed clinical assessment measures including demographic information, functional disability, and average pain intensity ratings. If patients agreed to participate in a larger clinic-based research project, additional measures, including the SCARED, were administered. As part of usual care, the multidisciplinary pain clinic team decided in collaboration with the patients/families if pain-focused CBT was appropriate for the patient (Figure 1). Common reasons for not recommending a patient for outpatient CBT at our center included patient distance to clinic, a medical team recommendation for a more intensive treatment approach (i.e., inpatient treatment), another psychiatric comorbidity (e.g., severe depression with suicidal ideation) requiring immediate treatment, high levels of patient functioning and lack of patient/family interest. CBT for chronic pain typically uses a blend of cognitive strategies (e.g., distraction, thought modification, problem solving) and behavioral approaches (e.g., activity pacing, relaxation training, parental instruction of behavioral strategies) to improve functioning and reduce pain symptoms in youth (9). Pain-focused CBT was provided by licensed clinical psychologists with a specialty in pediatric chronic pain management (80%) and advanced psychology trainees (20%) under the direct supervision of a licensed pediatric pain psychologist. Participants completed clinical outcome measures (FDI, pain intensity) throughout treatment as part of standard clinical care. The current study utilized the data completed during the initial evaluation and during the final active CBT session (after all pain coping skills were taught), which was noted by the provider in the patient EMR. Additional details of the study procedure, including collection of clinical outcome measures and description of the content of pain-focused CBT, have been previously published (11, 12).
Statistical analyses
Statistical analyses were accomplished using IBM SPSS Version 22. The sample was grouped based on presence or absence of clinically significant anxiety and sociodemographic differences were examined. Pearson χ2 tests were used to determine if the frequency of youth entering and completing CBT varied as a function of anxiety status. For those who completed a course of pain-focused CBT, a two-way mixed model analysis of variance was conducted to explore the impact of anxiety and CBT on clinical outcome measures (functional disability and average pain intensity) from the initial evaluation to the end of CBT treatment. Cohen d effect sizes were used to compare differences in outcome scores following CBT between the groups with and without clinical anxiety. Cohen (29) defined the magnitude of effect sizes as follows: small, d = .2, medium, d = .5, and large, d = .8 .
Results
Clinical Characteristics of the Total Pain Clinic Sample
A total of 247 patients completed an initial pain clinic evaluation, of which 175 completed measures of interest for this study and were recommended for pain-focused CBT at our center (Figure 1). Of those, 91 never initiated CBT, 44 initiated CBT but then dropped out prior to completing active treatment, and 40 completed a full course of treatment. Of those with clinical anxiety (n = 78, 44.6%), 42% never initiated CBT, 31% initiated CBT but then dropped out, and 27 % completed CBT. Of those with subclinical levels of anxiety (n = 97, 55.4%), 60% never started CBT, 20% started but then dropped out, and 20% completed CBT. Differences in those who a) never started CBT versus those who initiated and/or completed CBT and b) completed CBT versus did not complete CBT (including those who never started CBT) were examined. Pearson chi-squared test revealed a significant difference (χ2= 5.30, p < 0.05 between those who never started CBT and those who initiated CBT (with or without completion), suggesting that youth with clinically significant anxiety were more likely to start and/or complete a course of pain-focused CBT (57.7%) compared with those with subclinical levels of anxiety (40.2%). There was not a significant effect of anxiety status between CBT treatment completers and non-completers (χ2= 1.32, p = 0.25).
The sample was predominantly female and Caucasian, consistent with other pediatric pain populations (26). Demographic characteristics (age, sex, race, and ethnicity) were similar across treatment completers and non-completers (Table I). In addition, insurance status (use of either public or private insurance) was consistent across groups, with approximately two thirds of patients covered by private insurance (data gathered via EMR). Lastly, patients within these groups were categorized by moderate levels of pain and pain-related disability. Treatment completers were categorized by clinical levels of anxiety on average compared with those who never started or failed to complete a course of pain-focused CBT.
Table 1.
Demographics, Disability, Pain and Anxiety Scores in Total Pain Clinic Sample
| Recommended to Pain-Focused CBT (Total N=175) | |||
|---|---|---|---|
| Variable | Never Started (N=91) |
Dropped Out (N=44) |
Completed (N=40) |
| Age M (SD) | 14.41 (2.54) | 14.36( 2.51) | 14.35 (2.50) |
| Sex N (% female) | 68 (74.72) | 35 (79.54) | 34 (85) |
| Race N (% Caucasian) | 83 (91.21) | 41 (93.18) | 37 (92.5) |
| Ethnicity N (% Non-Hispanic) | 87 (95.60) | 43 (97.72) | 40 (100) |
| Insurance N (% private) | 60 (65.93) | 28 (63.64) | 25 (62.5) |
| FDI M (SD) | 23.27 (12.26) | 17.12 (12.02) | 24.95 (11.10) |
| Pain M (SD) | 5.79 (1.87) | 4.90 (2.56) | 5.61 (1.87) |
| Anxiety M (SD) | 19.86 (13.28) | 22.84 (14.57) | 25.35 (15.50) |
Note. FDI = Functional Disability Inventory.
Clinical Characteristics of Treatment Completers
A total of 40 participants (80% female) between the ages 9-18 (mean age = 14.4) completed a course of pain-focused CBT between 2011 and 2015, 21 with clinically significant anxiety, and 19 not meeting the clinical cut-off (Table II). The mean SCARED total score in the group with clinical anxiety was 36.52 (SD=12.04, range 25-70), whereas the mean SCARED total score in the group with subclinical anxiety was 13.00 (SD=7.28, range 0-23), with only two of those participants reporting no anxiety symptoms at all. Common pain complaints included abdominal (n=14), back (n=6), joint (n=5) generalized (n=4), headache (n=2), and other (n=9) pain. Fisher exact tests and independent sample t tests revealed no statistically significant differences between the group with clinical anxiety and the group with subclinical anxiety in terms of demographic characteristics (age and sex) and length of treatment.
Table 2.
Clinical Characteristics of Treatment Completers By Anxiety
| Clinical Anxiety (N=21) |
Subclinical Anxiety (N=19) |
|
|---|---|---|
| Mean Age (SD) | 14.90 (2.57) | 13.74 (2.66) |
| Sex N (% female) | 19 (90.5) | 13 (68.4) |
| Pain Location N (%) | ||
| Abdominal | 8 (38.10) | 6 (31.58) |
| Back | 3 (14.29) | 3 (15.79) |
| Joint | 1 (4.76) | 4 (21.05) |
| Generalized/widespread | 3 (14.29) | 1 (5.26) |
| Headache | 2 (9.52) | 0 (0) |
| Other | 4 (19.05) | 5 (26.32) |
| Number of CBT Sessions M (SD) | 6.52 (1.60) | 6.47 (1.68) |
Note. “Other” pain location category includes knee pain (n=2), complex regional pain syndrome (n=2), ankle (n=2), leg pain (n=1), neck (n=1), chest (n=1). Sessions includes sum of the initial evaluation and active CBT pain-focused sessions (when all coping skills were taught).
Treatment Outcomes by Anxiety
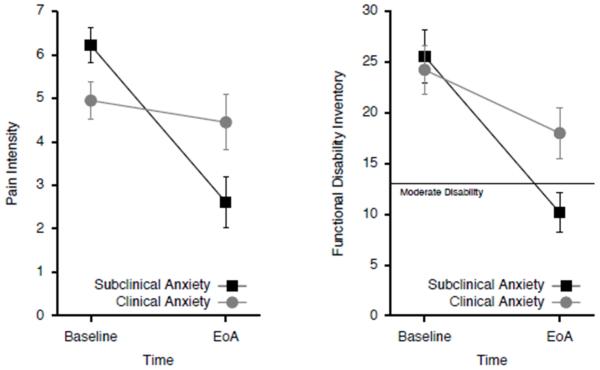
At the end of active treatment, there was a significant main effect for CBT on pain (F (1, 36) = 23.89, p < 0.001; Figure 2). However, the group without anxiety exhibited a substantial reduction in pain intensity, and the group with anxiety exhibited a limited response to treatment. Examination of the interaction effect confirmed that the reduction in average pain intensity was significantly smaller in the group with clinically significant anxiety than for the group with subclinical anxiety at the end of CBT (F (1, 36) = 13.68, p < 0.01).
Figure 2.
Youth with subclinical anxiety responded better to pain-focused CBT than youth with clinical anxiety. Specifically, these patients exhibited significantly larger reductions in perceived pain (p<0.01) and disability (p<0.05) following CBT (end of active treatment; EoA) than patients with clinical anxiety. Similarly, disability scores patients with subclinical anxiety dropped from moderate to minimal levels, and patients with clinical anxiety remained moderately disabled after treatment (right panel).
CBT also produced a significant main effect on disability (F (1, 38) = 24.06, p < 0.001, Figure 2). Further, examination of the interaction effect revealed that the reduction of disability was significantly smaller in the group with clinical anxiety at the end of CBT (F (1, 38) = 4.33, p < 0.05). The group with clinical anxiety continued to exhibit moderate levels of functional disability (FDI score = 18.00) as compared with the group with subclinical anxiety who demonstrated minimal levels of functional disability (FDI score = 10.16), based on published clinical reference points (26). Youth with clinically significant anxiety exhibited <7 point decrease in functional disability at the end of active treatment following a course of pain-focused CBT, whereas youth without clinically significant anxiety exhibited a >15 point decrease in functional disability, which is clinically meaningful (30). Cohen d effect sizes suggest moderate differences in both pain (0.77) and functional disability (0.78) levels at the end of active treatment in participants with clinically significant anxiety as compared with those with subclinical anxiety.
Discussion
Although chronic pain is common in childhood, the availability and utilization of specialized CBT for the management of pain is rare. Thus, this study addresses an important and understudied topic and identified a potentially modifiable factor - anxiety - which may adversely impact outcomes in youth with chronic pain. Our findings indicate that children and adolescents with chronic pain who reported clinically significant anxiety were more likely to initiate and/or complete pain-focused CBT. It is plausible that patients who present with clinically significant anxiety and chronic pain may be more likely to seek behavioral treatment given the increased clinical complexity of such patients and therefore greater clinical need. It may also be possible that presence of anxiety may lead to increased adherence to treatment recommendations from medical providers. Unfortunately, these youth were also less likely to improve following intervention when compared with their counterparts without anxiety. Despite initially presenting with comparable levels of pain intensity and disability, youth with clinically significant anxiety experienced minimal reductions in pain intensity and remained at least moderately disabled. In contrast, the group with subclinical anxiety experienced strong reductions in pain levels and demonstrated functioning within the minimal impairment range at the end of CBT treatment. These findings suggest that a more tailored treatment approach beyond traditional pain coping focused CBT may be warranted in youth with chronic pain and comorbid anxiety to improve patient outcomes.
Our findings continue to support research that indicates that clinically significant anxiety in patients with chronic pain is highly prevalent (18, 19, 31-33). The results of this investigation speak to the importance of anxiety screening in youth with chronic pain conditions in order to predict those patients who might be at greatest risk for poor outcomes - as they might respond less than optimally to standard pain-focused CBT. The SCARED, used in the current study, is a brief (21, 22), validated (19, 21, 22), and freely available (http://psychiatry.pitt.edu/research/tools-research/assessment-instruments) screening instrument endorsed by the American Academy of Pediatrics (34) to assess for child anxiety in medical settings. Given the high rate (75%) of overall positive treatment response to pain-focused CBT in a clinical sample of patients with undifferentiated anxiety levels (11), the present findings are particularly striking as they indicate that clinically elevated anxiety adversely impacts treatment response.
Further, the minimal improvement in functional disability scores on the FDI should be 7.8 points or greater to indicate true clinical improvement (30). Thus, the difference between the <7 point decrease in functional disability exhibited by youth with clinical anxiety compared with the >15 point decrease for the youth with subclinical anxiety following a course of pain-focused CBT is clinically meaningful.
Taken together, these findings suggest that current empirically supported CBT treatments for chronic pain (8) may be necessary but not sufficient to adequately meet the needs of patients with clinically significant anxiety, and the use of more tailored interventions to systematically address pain and anxiety might be needed for the subgroup with clinical anxiety.
Of note, the CBT treatment provided in our clinic was specific to coping with pain, which includes instruction in a blend of behavioral (e.g., relaxation, activity pacing) and cognitive (e.g., problem solving, positive thinking) strategies specific to coping with pain. Patients were generally referred elsewhere if additional anxiety or mood issues required further care. However, if a model was employed in the future in which comorbid anxiety was also addressed in treatment, pain patients could also receive training in anxiety-specific coping strategies that are not traditionally addressed in standard pain-coping skills treatment, which include techniques such as graded exposure, social skills/assertiveness training, and in-depth cognitive restructuring, which may bolster their treatment outcomes. In addition, patients could learn to apply some pain coping skills (relaxation training, positive thinking) to anxiety-provoking situations that were not directly related to pain (e.g., treatment of school avoidance which may exacerbate disability).
The current investigation is subject to limitations associated with the realities of treatment delivery in the clinical setting (e.g., pain of different etiologies, lack of uniform treatment duration, failure to complete services, female predominance) and the small numbers of patients who receive services from multi-disciplinary pain clinics. There is very limited research examining the effect of CBT for pediatric chronic pain in real world settings. Although our rates of CBT uptake are low (~50%), they are comparable with the other only published study examining uptake of CBT for pediatric chronic pain (35). Importantly, pain-focused CBT was delivered using a standardized toolkit across providers. Thus, there was considerable uniformity in techniques taught across participants. Moreover, these data allow for broader generalizability to “real world” settings as they are likely to be more representative of clinical practices where evidence-based CBT interventions (8) are routinely employed for the treatment of pediatric chronic pain. In addition, the ability to examine sex differences in the utilization and efficacy of CBT is limited by the large portion of the patients who were female, who reflect the typical population seen in the chronic pain clinic (26). However, findings in adults indicate that sex does not impact the response for chronic pain (36, 37).
This investigation may lead to several promising future lines of research. Increased attention to improving retention rates of CBT for chronic pain is of utmost importance. Testing different modalities of treatment (e.g., incorporation of web-based components into the treatment) may address some commonly identified barriers to CBT by reducing the need for weekly in person visits. Pain heterogeneity is a strength of the current investigation in terms of study generalizability; however, it would also be prudent to explore differences in outcomes based on anxiety across pain subtypes in future research. Certain pain subtypes, such as widespread pain (38) and abdominal pain (39) may have higher rates of anxiety compared with other chronic pain populations and may require a more tailored approach to care. It would also be valuable to examine changes in anxiety over the course of CBT for pain. The findings from this study also suggest further investigation focused on designing and testing tailored behavioral approaches to target both anxiety and pain symptoms in youth with chronic pain. At present, there is some evidence that improvements in pain can be made when anxiety is addressed at least in an intensive inpatient rehabilitation program that includes CBT (40) Thus, modifications of existing treatment protocols and future examination of the role of anxiety in relationship to pain-focused CBT treatment outcomes in a traditional outpatient setting is warranted.
In summary, these findings have important implications for youth with chronic pain who present to tertiary care pain clinics and also for youth with chronic pain who present to primary care or subspecialty clinics (ie, gastroenterology, neurology etc.) where it may be plausible to intervene early and perhaps forestall the progression from acute (and perhaps less functionally disabling pain) to chronic pain. Across these various medical settings, these findings may be readily translated into clinical practice by incorporating a routine assessment of patient anxiety levels during standard medical care. Accordingly, the impact on improving patient outcomes in clinical practice is likely to be significant. For patients who exhibit clinically significant levels of anxiety, a tailored CBT approach that targets both pain coping and anxiety may be optimal for improving pain-related outcomes.
Acknowledgments
Supported by the National Institutes of Health (HD F32, 1F32HD078049 – 01A1 [postdoctoral training grant to N.C.], and K24 AR056687 [midcareer mentorship award to S.K.-Z.]).
Footnotes
No reprints of this article are requested.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare on conflicts of interest.
References
- 1.King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, et al. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain. 2011;152(12):2729–38. doi: 10.1016/j.pain.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 2.Stanford EA, Chambers CT, Biesanz JC, Chen E. The frequency, trajectories and predictors of adolescent recurrent pain: A population-based approach. Pain. 2008;138(1):11–21. doi: 10.1016/j.pain.2007.10.032. [DOI] [PubMed] [Google Scholar]
- 3.Campo JV, Comer DM, Jansen-McWilliams L, Gardner W, Kelleher KJ. Recurrent pain, emotional distress, and health service use in childhood. J Pediatr. 2002;141(1):76–83. doi: 10.1067/mpd.2002.125491. [DOI] [PubMed] [Google Scholar]
- 4.Ho IK, Goldschneider KR, Kashikar-Zuck S, Kotagal U, Tessman C, Jones B. Healthcare utilization and indirect burden among families of pediatric patients with chronic pain. J Musculoskelet Pain. 2008;16(3):155–64. [Google Scholar]
- 5.Størdal K, Nygaard EA, Bentsen BS. Recurrent abdominal pain: a five-year follow-up study. Acta Pædiatrica. 2005;94(2):234–6. doi: 10.1111/j.1651-2227.2005.tb01897.x. [DOI] [PubMed] [Google Scholar]
- 6.Walker LS, Guite JW, Duke M, Barnard JA, Greene JW. Recurrent abdominal pain: a potential precursor of irritable bowel syndrome in adolescents and young adults. J Pediatr. 1998;132(6):1010–5. doi: 10.1016/s0022-3476(98)70400-7. [DOI] [PubMed] [Google Scholar]
- 7.Kashikar-Zuck S, Cunningham N, Sil S, Bromberg MH, Lynch-Jordan AM, Strotman D, et al. Long-term outcomes of adolescents with juvenile-onset fibromyalgia in early adulthood. Pediatrics. 2014;133(3):e592–e600. doi: 10.1542/peds.2013-2220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kashikar-Zuck S, Ting T, Arnold L, Bean J, Powers S, Graham T, et al. Cognitive behavioral therapy for the treatment of juvenile fibromyalgia: A multisite, single-blind, randomized, controlled clinical trial. Arthritis Rheum. 2012;64(1):297–305. doi: 10.1002/art.30644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eccleston C, Palermo TM, Williams ACC, Lewandowski Holley A, Morley S, Fisher E, et al. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. The Cochrane Library. 2014;5:1–94. doi: 10.1002/14651858.CD003968.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Veek SM, Derkx BH, Benninga MA, Boer F, de Haan E. Cognitive behavior therapy for pediatric functional abdominal pain: A randomized controlled trial. Pediatrics. 2013;132(5):e1163–e72. doi: 10.1542/peds.2013-0242. [DOI] [PubMed] [Google Scholar]
- 11.Lynch-Jordan AM, Sil S, Cunningham NR, Joffe N, Slater SK, Tran ST, et al. Measuring treatment response in an outpatient pediatric pain program. Clin Pract Pediatr Psychol. 2015;3(1):1–11. [Google Scholar]
- 12.Lynch-Jordan A, Sil S, Peugh J, Cunningham N, Kashikar-Zuck S, Goldschneider K. Differential changes in functional disability and pain intensity over the course of psychological treatment for children with chronic pain. Pain. 2014;155(10):1955–61. doi: 10.1016/j.pain.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matcham F, Norton S, Scott DL, Steer S, Hotopf M. Symptoms of depression and anxiety predict treatment response and long-term physical health outcomes in rheumatoid arthritis: secondary analysis of a randomized controlled trial. Rheumatology (Oxford) 2015 doi: 10.1093/rheumatology/kev306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th American Psychiatric Publishing; Arlington, VA: 2013. [Google Scholar]
- 15.Dufton LM, Dunn MJ, Compas BE. Anxiety and somatic complaints in children with recurrent abdominal pain and anxiety disorders. J Pediatr Psychol. 2009;34(2):176–86. doi: 10.1093/jpepsy/jsn064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knook LM, Konijnenberg AY, van der Hoeven J, Kimpen JL, Buitelaar JK, van Engeland H, et al. Psychiatric disorders in children and adolescents presenting with unexplained chronic pain: What is the prevalence and clinical relevancy? Eur Child Adolesc Psychiatry. 2011;20(1):39–48. doi: 10.1007/s00787-010-0146-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kashikar-Zuck S, Parkins IS, Graham TB, Lynch AM, Passo M, Johnston M, et al. Anxiety, mood, and behavioral disorders among pediatric patients with juvenile fibromyalgia syndrome. Clin J Pain. 2008;24(7):620–6. doi: 10.1097/AJP.0b013e31816d7d23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cunningham NR, Cohen MB, Farrell MK, Mezoff AG, Lynch-Jordan A, Kashikar-Zuck S. Concordant parent-child reports of anxiety predict impairment in youth with functional abdominal pain. J Pediatr Gastroenterol Nutr. 2014;60(3):312–7. doi: 10.1097/MPG.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mano KEJ, Evans JR, Tran ST, Khan KA, Weisman SJ, Hainsworth KR. The psychometric properties of the Screen for Child Anxiety Related Emotional Disorders in pediatric chronic pain. J Pediatr Psychol. 2012;37(9):999–1011. doi: 10.1093/jpepsy/jss069. [DOI] [PubMed] [Google Scholar]
- 20.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th American Psychiatric Publishing; Washington, DC: 2000. [Google Scholar]
- 21.Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36(4):545–53. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Birmaher B, Brent D, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999;38(10):1230–6. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Walker LS, Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. J Pediatr Psychol. 1991;16(1):39–58. doi: 10.1093/jpepsy/16.1.39. [DOI] [PubMed] [Google Scholar]
- 24.Claar RL, Walker LS. Functional assessment of pediatric pain patients: psychometric properties of the functional disability inventory. Pain. 2006;121(1-2):77–84. doi: 10.1016/j.pain.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palermo TM, Long AC, Lewandowski AS, Drotar D, Quittner AL, Walker LS. Evidence- based assessment of health-related quality of life and functional impairment in pediatric psychology. J Pediatr Psychol. 2008;33(9):983–96. doi: 10.1093/jpepsy/jsn038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kashikar-Zuck S, Flowers S, Claar R, Guite J, Logan D, Lynch-Jordan A, et al. Clinical utility and validity of the Functional Disability Inventory among a multicenter sample of youth with chronic pain. Pain. 2011;152(7):1600–7. doi: 10.1016/j.pain.2011.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cleeland C, Ryan K. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23(2):129–38. [PubMed] [Google Scholar]
- 28.Turk DC, Dworkin RH, Revicki D, Harding G, Burke LB, Cella D, et al. Identifying important outcome domains for chronic pain clinical trials: an IMMPACT survey of people with pain. Pain. 2008;137(2):276–85. doi: 10.1016/j.pain.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 29.Cohen J. A power primer. Psychol Bull. 1992;112(1):155–9. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 30.Sil S, Arnold LM, Lynch-Jordan A, Ting TV, Peugh J, Cunningham N, et al. Identifying treatment responders and predictors of improvement after cognitive-behavioral therapy for juvenile fibromyalgia. Pain. 2014;155(7):1206–12. doi: 10.1016/j.pain.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cunningham NR, Lynch-Jordan A, Mezoff AG, Farrell MK, Cohen MB, Kashikar-Zuck S. Importance of addressing anxiety in youth with functional abdominal pain: suggested guidelines for physicians. J Pediatr Gastroenterol Nutr. 2013;56(5):469–74. doi: 10.1097/MPG.0b013e31828b3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen LL, Vowles KE, Eccleston C. The impact of adolescent chronic pain on functioning: Disentangling the complex role of anxiety. J Pain. 2010;11(11):1039–46. doi: 10.1016/j.jpain.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 33.Wendland M, Jackson Y, Stokes LD. Functional disability in paediatric patients with recurrent abdominal pain. Child Care Health Dev. 2010;36(4):516–23. doi: 10.1111/j.1365-2214.2010.01087.x. [DOI] [PubMed] [Google Scholar]
- 34.American Academy of Pediatrics Addressing Mental Health Concerns in Primary Care: A Clinician's Toolkit2010, revised. 2012 [Google Scholar]
- 35.Simons LE, Logan DE, Chastain L, Cerullo M. Engagement in multidisciplinary interventions for pediatric chronic pain: parental expectations, barriers, and child outcomes. Clin J Pain. 2010;26(4):291–9. doi: 10.1097/AJP.0b013e3181cf59fb. [DOI] [PubMed] [Google Scholar]
- 36.McCracken LM, Turk DC. Behavioral and cognitive–behavioral treatment for chronic pain: outcome, predictors of outcome, and treatment process. Spine. 2002;27(22):2564–73. doi: 10.1097/00007632-200211150-00033. [DOI] [PubMed] [Google Scholar]
- 37.Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive–behavioral therapy for chronic pain. Pain. 2007;127(3):276–86. doi: 10.1016/j.pain.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 38.Cunningham NR, Tran ST, Lynch-Jordan AM, Ting TV, Sil S, Strotman D, et al. Psychiatric Disorders in Young Adults Diagnosed with Juvenile Fibromyalgia in Adolescence. J Rheumatol. 2015 doi: 10.3899/jrheum.141369. jrheum. 141369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tran ST, Jastrowski Mano KE, Anderson Khan K, Davies WH, Hainsworth KR. Patterns of anxiety symptoms in pediatric chronic pain as reported by youth, mothers, and fathers. Under Revision. [Google Scholar]
- 40.Benore E, D'Auria A, Banez GA, Worley S, Tang A. The influence of anxiety reduction on clinical response to pediatric chronic pain rehabilitation. Clin J Pain. 2015;31(5):375–83. doi: 10.1097/AJP.0000000000000127. [DOI] [PubMed] [Google Scholar]