Abstract
Objectives
We investigated the differences in clinical characteristics and musculoskeletal (MSK) conditions by cocaine use.
Methods
HealthStreet, a community engagement program assessed 7936 adults for medical conditions.
Results
Among 6145 African Americans (77%) and 1791 (23%) Caucasians, 15.5 % and 25% reported cocaine use, respectively. African-American cocaine users were older (p < .001) and more likely to report hypertension (p < .001) and HIV (p <.001) than Caucasian users. Compared to non-users, back pain was reported by 42% of African Americans (p < .001) and 48% of Caucasian cocaine users (p < .003). African-American cocaine users had significantly higher odds of back pain, 1.60 (95% CI 1.27, 2.04) and arthritis, 1.40 (95% CI 1.19, 1.64) than Caucasians.
Conclusions
Cocaine users are more likely to endorse MSK conditions than non-users. Racial disparities among users existed; however, how race affects health among users requires further research.
Keywords: : cocaine, health disparities, African Americans, musculoskeletal, arthritis, back pain
Addiction is a chronic relapsing disorder characterized by repetitive and compulsive drug-seeking behavior despite negative health or social consequences. Cocaine addiction is a significant worldwide public health problem that has somatic, psychological, psychiatric, socio-economic, and judicial complications.1,2 Cocaine remains the second most commonly used and trafficked illicit drug in the world after cannabis.3 Prevalence of cocaine use (lifetime-LT, past 12 months, and past 30 days) in the US is particularly high among males 15 to 34 years of age.4 Some of the most frequent complications associated with cocaine use are cardiovascular (acute coronary syndrome, cardiac arrhythmias, increased blood pressure); respiratory (fibrosis, interstitial pneumonitis, pulmonary hypertension, alveolar hemorrhage, asthma exacerbation, emphysema); neurological (strokes, aneurysms, seizures, headaches); and communicable diseases such as HIV/AIDS, hepatitis B and C, and sexual transmitted diseases (STDs).5,6 However, the association of musculoskeletal (MSK) complications including any kind of arthritis and back pain with cocaine use rarely have been studied and reported. Furthermore, many health conditions that are increased among cocaine users may result in joint pain, including hepatitis C virus (HCV) and HIV infections. Whereas HCV is common in cocaine users and has been linked to MSK conditions (peripheral neuropathies, arthritis, etc), support for this association has been limited by a lack of controls and/or adjustment for important confounders, most notably substance abuse.6 In the current study using data from a community engagement program in 3 geographic areas throughout the United States, we investigated the differences in clinical characteristics in general and MSK conditions in particular by cocaine versus non-cocaine use to understand the clinical risk factors among cocaine users. In addition, as a secondary objective, we also did a sensitivity analysis looking at racial differences by MSK.
Because of increased burden of diseases among African Americans, we hypothesized that LT cocaine users would report more chronic and infectious health conditions than non-cocaine users, and that more African-American users would report such conditions than Caucasian users.
Methods
HealthStreet
Details on the HealthStreet community engagement model have been published previously.7,8 Briefly, this effort strives to reduce disparities in healthcare and research participation. HealthStreet was established at Washington University, St. Louis (WUSTL) in 1989, and scaled up for used up in the Clinical and Translation Science Award (CTSA) there in 2007. In 2011, HealthStreet was initiated at the University of Florida (UF) by Drs Cottler and Striley and is funded partially through the UF CTSA. Utilizing a community health worker (CHW) model, HealthStreet: (1) assesses the community's health needs and health concerns; (2) links people, based on their needs and concerns, to medical and social services and opportunities to participate in research; (3) engages in bidirectional, health-promoting communication with and for the community; and (4) increases the community's trust in health research through meaningful collaborations.8,9
Data Collection
Data for HealthStreet at UF were collected and entered using REDCap (Research Electronic Data Capture) software—a secure, Web-based data capture tool.10 Data collected at WUSTL were entered into a secure Access database, as well.
Study Sample
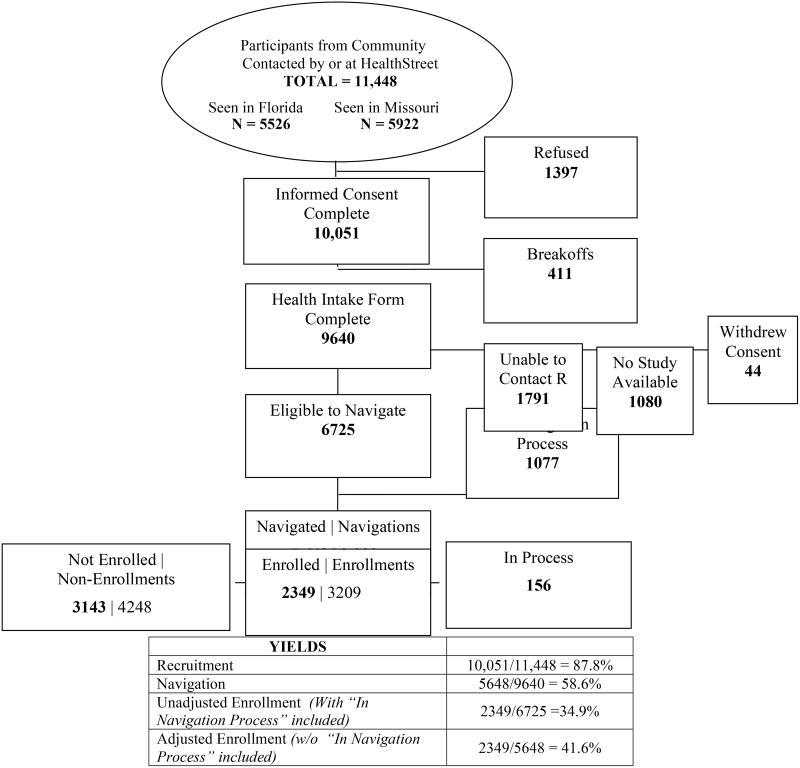
The HealthStreet sample for this analysis was comprised of African-American and Caucasian respondents from St. Louis, MO, Gainesville, FL, and Jacksonville, FL, who were administered a Health Intake assessment between September 2008 and February 2014 (Figure 1). As of February 2014, HealthStreet reached a total of 11,448 community members in Missouri and Florida, with over 10,000 respondents providing informed consent (Figure 1). Among these, 9640 (87.8%) completed the Health Intake form with CHWs. There was no significant difference between those who completed and those who did not complete the Health Intake form. The Health Intake includes demographic and family characteristics, health conditions, prioritized health concerns, medication and drug use, and healthcare access. It is an extensive intake form that includes major questions related to health containing both multiple-choice items as well as open-ended questions, eg, “Have you ever been told or have you ever had problem with X.”
Figure 1. HealthStreet Flowchart, St. Louis, Missouri and Gainesville/Jacksonville, Florida, September 2008 - February 20l4a.
Note. a Numbers in BOLD represent PEOPLE, not events.
Data Analyses
All analyses were stratified by reported race (African-American vs Caucasian) and completed using SAS version 9-4 software.10 Fisher's exact statistics were used to examine the differences in proportions among categorical demographic characteristics, chronic diseases, and other medical conditions between those reporting LT cocaine use compared to non-users, and 2-tailed Student's t-test statistics were used for continuous variables.11 Both univariate and multivariate logistic regression analyses were used to predict LT cocaine use. Confidence intervals (95% CI) are reported for all odds ratios (OR) generated through logistic regression analyses.
Results
Overall, the sample consisted of 7936 respondents, among whom 3753 (47.3%) lived in Florida and 4183 (52.7%) from Missouri. Over three-fourths (77.4%) were African Americans and 22.6% were Caucasians. Furthermore, 951 African-American respondents (15.5%) reported LT cocaine use compared to 453 Caucasian respondents (25.3%), as measured by the question, “Have you ever used cocaine or crack?” (Table 1).
Table 1. HealthStreet Participant Demographics and Musculoskeletal Comorbidities by Race and Self-Reported Lifetime Cocaine Use, Gainesville, Florida and St. Louis, Missouri (N = 7936).
| African-American (N = 6145) | Caucasian (N = 1791) | ||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Demographics | LT Cocaine Use (N = 951) | No LT Cocaine Use (N = 5194) | LT Cocaine Use (N = 453) | No LT Cocaine Use (N = 1338) | |||
|
|
|||||||
| N (%) | N (%) | p-value | N (%) | N (%) | p-value | ||
| Site | |||||||
| Florida | 339 (35.7%) | 2196 (42.3%) | <.001 | 291 (64.2%) | 927 (69.3) | .047 | |
| Missouri | 612 (64.4%) | 2998 (57.7%) | 162 (35.8%) | 411 (30.7) | |||
|
| |||||||
| Female | 397 (41.8%) | 3005 (57.9%) | <.001 | 190 (42.0%) | 760 (56.8) | <.001 | |
|
| |||||||
| Hispanic/Latino | 6 (0.6%) | 41 (0.8%) | NS | 7 (1.6%) | 39 (2.9%) | NS | |
|
| |||||||
| Mean Age (±SD), years | 47.9 (±9.2) | 37.9 (±14.5) | <.001 | 42.8 (±12.2) | 42.0 (±15.9) | NS | |
|
| |||||||
| Mean Years of Education (±SD) | 11.9 (±1.8) | 12.3 (±2.1) | <.001 | 12.6 (±2.4) | 13.3 (±2.7) | <.001 | |
|
| |||||||
| Marital Status | <.001 | <.001 | |||||
| Never Married | 522 (54.9%) | 3455 (66.5%) | 201 (44.4%) | 608 (45.4%) | |||
| Married | 116 (12.2%) | 1003 | 62 (13.7%) | 333 (24.9%) | |||
| Separated/Divorce/Widowed | 304 (32.0%) | (19.3%) | 189 (41.7%) | 395 (29.5%) | |||
|
| |||||||
| Unemployed | 702 (73.8%) | 3077 (59.2%) | <.001 | 316 (69.8%) | 768 (57.4%) | <.001 | |
|
| |||||||
| Veteran | 165 (17.4%) | 314 (6.1%) | <.001 | 61 (13.5%) | 138 (10.3%) | NS | |
|
| |||||||
| Medically Uninsured | 506 (53.2) | 2143 (41.3%) | <.001 | 279 (61.6%) | 533 (39.8%) | <.001 | |
|
| |||||||
| Chronic Diseases, Infections, and Musculoskeletal Symptoms | |||||||
|
| |||||||
| Back Pain (BP) | 398 (41.9%) | 1456 (28.0%) | <.001 | 215 (47.5%) | 498 (37.2%) | <.001 | |
|
| |||||||
| Arthritis | 320 (33.7%) | 939 (18.1%) | <.001 | 153 (33.8%) | 371 (27.7%) | .04 | |
|
| |||||||
| Hypertension | 405 (42.6%) | 1433 (27.6%) | <.001 | 108 (23.8%) | 341 (25.5%) | NS | |
|
| |||||||
| Type II Diabetes | 89 (9.4%) | 418 (8.1%) | 0.048 | 28 (6.2%) | 103 (7.7%) | NS | |
|
| |||||||
| Any Lifetime Hepatitis | 87 (9.2%) | 67 (1.3%) | <.001 | 63 (13.9%) | 36 (2.7%) | <.001 | |
|
| |||||||
| HIV | 44(4.6%) | 99 (1.9%) | <.001 | 7 (1.6%) | 17 (1.3%) | NS | |
|
| |||||||
| Any STDsa | 181 (19.0%) | 436 (8.4%) | <.001 | 72 (15.9%) | 64 (4.8%) | <.001 | |
|
| |||||||
| Past 30-day Opioid Use | 115 (12.1%) | 432 (8.3%) | <.001 | 78 (17.2%) | 166 (12.4%) | .027 | |
|
| |||||||
| Past 30-day Cigarette Use | 671 (70.6%) | 2150 (41.4%) | <.001 | 313 (69.1%) | 510 (38.1%) | <.001 | |
Note.
= chlamydia, gonorrhea, herpes, syphilis
NS = non-significant
Regardless of race, cocaine users compared to non-users were less likely to be female and educated, more likely to be unemployed, veterans, and medically uninsured. LT cocaine users also reported more risk factors than non-users, including past 30-day opioid and cigarette use. In terms of health problems, LT cocaine users endorsed all symptoms and conditions except for hypertension, diabetes, and HIV.
Among African Americans, we found differences between users and non-users for all factors except Hispanic ethnicity and diabetes, applying Bonferroni checks. Among Caucasians, there were no differences with respect to Hispanic ethnicity, age, veteran status, arthritis, hypertension, diabetes, and past 30-day opioid use. Other substance use was non-significant, and therefore, was not included in the analysis.
We next examined predictors of LT cocaine use stratified by race when controlled for other health risk and demographic factors of interest (Table 2). For both races, those with arthritis, LT hepatitis, back pain and history of STD were more likely to report cocaine use than their counterpart. HIV was not predictive of cocaine use among Caucasian users, and past 30-day opioid use was not predictive of cocaine use among African-American users. African-American users had significantly higher odds of reporting back pain compared to non-cocaine users [OR=1.60 (95% CI 1.27, 2.04)].
Table 2. Age-adjusted ORs Predicting Comorbidities of LT Cocaine Users among African-American and Caucasian HealthStreet Members, HealthStreet Gainesville, Florida and St. Louis, Missouri.
| African Americans (N = 6145) | Age-adjusted OR (95% CI) |
|---|---|
| Hypertension | 1.15 (0.99, 1.34) |
| Type II Diabetes | 0.77 (0.61, 0.99) |
| Arthritis | 1.40 (1.19, 1.64) |
| Any LT Hepatitis | 5.60 (4.02, 7.78) |
| HIV | 2.50 (1.70, 3.67) |
| Back Pain | 1.60 (1.27, 2.04) |
| Any STDsa | 3.06 (2.49, 3.75) |
| Past 30-day Opioid Use | 1.25 (0.99, 1.56) |
|
| |
| Caucasians (N = 1791) | Age-adjusted OR (95% CI) |
|
| |
| Hypertension | 0.92 (0.71,1.20) |
| Type II Diabetes | 0.87 (0.56, 1.35) |
| Arthritis | 1.38 (1.08, 1.76) |
| Any LT Hepatitis | 6.46 (4.16, 10.04) |
| HIV | 1.24 (0.51, 3.02) |
| Back Pain | 1.65 (1.27, 2.16) |
| Any STDsa | 3.74 (2.62, 5.34) |
| Past 30-day Opioid Use | 1.46 (1.09, 1.96) |
Note.
= Includes chlamydia, gonorrhea, herpes, and syphilis
With respect to race differences, the presence of any reported back pain or any kind of arthritis was further analyzed in LT cocaine and non-cocaine users after adjusting for age, STDs, and use of other illicit drugs (Table 3). The presence of LT hepatitis or past 30-day use of opioids increased the odds of reporting back pain/arthritis among cocaine users. Reporting any hepatitis, STD, past 30-day opioid use, and illicit substance use increased the odds of reporting back pain/arthritis among African Americans (Table 3).
Table 3. Adjusted Prevalence of Musculoskeletal Conditions (Back Pain/Arthritis) in Cocaine versus Non-cocaine Users (N = 7936)a.
| Caucasian LT Cocaine Users (N = 452) | ||||
|---|---|---|---|---|
|
|
||||
| Back Pain or Arthritis (N = 255) | No Back Pain or Arthritis (N = 197) | |||
|
|
||||
| N (%) | N (%) | p-value | Adjusted OR | |
| HIV/AIDS | 4 (1.6%) | 3 (1.5%) | NS | 0.85 (0.18, 4.01) |
| Any Hepatitis | 48 (18.8%) | 15 (7.6%) | .003 | 2.09 (1.11, 3.96) |
| STDsb | 43 (16.9%) | 29 14.7%) | NS | 1.21 (0.71, 2.05) |
| Past 30-day Opioid Use | 56 (22.0%) | 22 (11.2%) | .003 | 2.50 (1.44, 4.35) |
| LT Illicit Substance Usec | 232 (91.0%) | 184 (93.4%) | .015 | 0.54 (0.24, 1.21) |
|
|
||||
| Caucasian Non-LT Cocaine Users (N = 1332) | ||||
|
|
||||
| Back Pain or Arthritis (N = 255) | No Back Pain or Arthritis (N = 197) | |||
|
|
||||
| HIV/AIDS | 7 (1.1%) | 10 (1.4%) | NS | 0.53 (0.20, 1.44) |
| Any Hepatitis | 24 (3.8%) | 12 (1.7%) | NS | 1.61 (0.78, 3.32) |
| STDsb | 44 (6.9%) | 20 (2.9%) | .003 | 2.43 (1.39, 4.25) |
| Past 30-day Opioid Use | 124 (19.5%) | 42 (6.0%) | <.001 | 3.44 (2.35, 5.03) |
| LT Illicit Substance Usec | 298 (46.9%) | 288 (41.3%) | <.001 | 1.21 (0.96, 1.53) |
|
|
||||
| African-American LT Cocaine Users (N = 948) | ||||
|
|
||||
| Back Pain or Arthritis (N = 255) | No Back Pain or Arthritis (N = 197) | |||
|
|
||||
| HIV/AIDS | 27 (5.1%) | 17 (4.0%) | NS | 0.70 (0.70,2.46) |
| Any Hepatitis | 62 (11.8%) | 25 (5.9%) | .006 | 1.80 (1.09, 2.99) |
| STDsb | 113 (21.5%) | 68 (16.1%) | NS | 1.49 (1.06, 2.09) |
| Past 30-day Opioid Use | 96 (18.3%) | 19 (4.5%) | <.001 | 4.63 (2.76, 7.76) |
| LT Illicit Substance Usec | 438 (83.4%) | 325 (76.8%) | .019 | 1.50 (1.06, 2.13) |
|
|
||||
| African-American Non-LT Cocaine Users (N = 5177) | ||||
|
|
||||
| Back Pain or Arthritis (N = 255) | No Back Pain or Arthritis (N = 197) | |||
|
|
||||
| HIV/AIDS | 36 (1.9%) | 63(1.9%) | NS | 0.97 (0.63, 1.49) |
| Any Hepatitis | 45 (2.3%) | 22 (0.7%) | <.001 | 2.29 (1.35, 3.91) |
| STDsb | 207 (10.8%) | 228 (7.0%) | <.001 | 1.95 (1.58, 2.40) |
| Past 30-day Opioid Use | 280 (14.6%) | 150 (4.6%) | <.001 | 3.24 (2.61, 4.02) |
| LT Illicit Substance Usec | 807 (42.0%) | 1234 (37.9%) | <.001 | 1.43 (1.26, 1.63) |
Note.
= Adjusted for age and past 30-day cigarette use
= Includes chlamydia, gonorrhea, herpes, syphilis
= Includes club drugs, marijuana, heroin, speed/amphetamines, inhalants, and hallucinogens, and excludes cocaine use.
Discussion
Cocaine use in the United States continues to be a health problem.13 Despite the many successes that have resulted in combating cocaine use and other substance use disorders, published data suggest that African Americans continue to experience a disproportionate burden of cocaine abuse.14-16 This study compared health outcomes for African-American and Caucasian community LT cocaine users among community recruited persons from 3 geographic areas and 2 states of the United States in a cross-sectional study design. Based on conservative estimates, national studies have shown that peak drug use occurs between the ages of 18 and 20, with a steady decline with increasing age.17 The participants in the current study belonged to wide age range age, from the age of highest risk (younger group) into older ages considered as lower risk age; this makes the high prevalence of cocaine use among these participants all the more striking ie, 15.5% in African Americans and 25.3% in Caucasian LT cocaine users.
Considering the relationship of social factors with cocaine use, previous studies suggest a negative relationship between drug use and productivity.13,14 Our study supported the results of previous studies and as expected, found that drug users were more likely to be male and unemployed than non-users.
Based on the published data related to cardiovascular diseases (CVDs), African Americans are at high risk for hypertension, cardiovascular disease (CVD), and end-stage kidney disease.18,19 In the current study, though hypertension was a major health condition reported in African Americans, LT cocaine use was not found to be an independent predictor for hypertension for African Americans only. This further supports the existing literature and confirms that chronic cocaine use may be associated with acute but not chronic hypertension among African Americans.
MSK conditions in general and arthritis, and back pain in particular in adults is the leading cause of disability and is among the leading conditions causing work related disability.20,21 Over the next 25 years, the number of people affected and the social impact of diagnosed arthritis are projected to increase by 40% in the United States.22 In this study, cocaine use was associated with MSK conditions among study participants. We found increased odds of reporting back pain among African-American and Caucasian cocaine users after adjusting for other risk factors of interest. There may be many possible reasons for this association such as the presence of HIV or LT hepatitis related to cocaine use (among African Americans). Levimasole is now felt to contaminate the majority of the cocaine supply in the United States. The growing research on the use of levimasole has been associated with vasculopathy associated with positive perinuclear anti-neutrophil antibodies (p-ANCA) increasing the risk of MSK conditions, an area for further research.23-25
Similarly, in addition to arthritis, more LT cocaine users versus non-users reported back pain in our study regardless of race. Possible explanations could include chronic pain following trauma, mechanical back pain, or inflammatory back pain. Pain also may be referred from the aorta or renal organs. Furthermore, opioid and cigarette use within the past 30 days was greater among patients who reported LT cocaine use (Tables 1 and 2). We observed that those reporting LT cocaine use were twice as likely to report smoking cigarettes within the past 30 days compared to non-users (2.3; 1.9 – 2.8 in African Americans; 1.9; 1.4 – 2.6 in Caucasians).
The use of opioids for chronic non-malignant pain has accelerated in the United States. There is an increased incidence of opioid abuse, alcohol abuse/dependence among those with chronic pain as well as illicit substance abuse reported by some authors.25 In addition, Ives et al26 report that patients with cocaine or alcohol abuse are most likely to misuse opioids. In contrast, Mertens et al27 report higher prevalence of back pain and arthritis among patients dependent on narcotic analgesic agents but not in the cocaine group. Because of the cross-sectional study design, we could not show the temporal association; future longitudinal studies are needed to ascertain the cause-effect relationship between cocaine use and MSK conditions.
This study has several limitations. First, though a community-based population sample, this is a cross-section design and all findings are associational, and not necessarily causal. Future longitudinal studies are warranted. Second, LT cocaine use was defined on the basis of self-reported history; therefore, the prevalence of cocaine use in both African Americans and Caucasians may underestimate the true prevalence. This is also true for information regarding hepatitis, HIV, STDs and other medical conditions. Third, whereas LT cocaine users in this study were more likely to report a variety of medical conditions, we were unable to test whether the cocaine use or health problem came first. Again, longitudinal research with repeated measures is required to improve understanding of these relationships. Finally, further research is required to gain more understanding of the health disparities between African-American and Caucasian users and whether there are unique factors among drug users that contribute to these disparities.
Implications for Health Behavior or Policy
In this study, large community-based populations were used which represent diverse ethnic groups from 3 geographical areas and 2 states of the US. Notwithstanding study limitations, the findings have important health behavior and policy implications. LT cocaine use is a pervasive social problem associated with chronic medical conditions which may not be easily recognized. The impact of the consequences of cocaine use on health is underestimated. LT cocaine users are more likely to report a variety of medical conditions, although the current study does not allow for testing which came first. In addition, the likelihood of reporting these health consequences varies by race.
Acknowledgments
The project was funded by the Washington University-Clinical Translational Science Award (CTSA-UL1 RR024992) funded by the National Institute of Health (NIH), St. Louis, Missouri and University of Florida CTSA (UL1 RR029890 funded by the NIH, Gainesville, Florida). All authors have read and approved the manuscript and have no financial disclosures or conflicts of interest to report. We are indebted to all HealthStreet community health workers who collected data from the community. Last, but not the least, many thanks to Dr Sahel Arora who provided administrative support in manuscript editing, corrections and formatting.
Footnotes
Conflict of Interest Disclosure Statement: All authors of this manuscript declare no conflicts of interest.
Human Subject Approval Statement: HealthStreet at University of Florida (UF) was approved by the UF Institutional Review Board (IRB); HealthStreet at Washington University St. Louis (WUSTL) was approved by the WUSTL IRB. Community health workers administer informed consent forms with each community member to ensure that protected health information is collected and stored confidentially.
Contributor Information
Sunita Dodani, .
Corrine W. Ruktanonchai, .
Gurjit S. Kaeley, .
Krishna Vaddiparti, .
Catherine W. Striley, .
Linda B. Cottler, .
References
- 1.Finkel JB, Marhefka GD. Rethinking cocaine-associated chest pain and acute coronary syndromes. Mayo Clin Proc. 2011;86(12):1198–1207. doi: 10.4065/mcp.2011.0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karila L, Lowenstein W, Coscas S, et al. Complications of cocaine addiction. Rev Prat. 2009;59(6):825–829. [PubMed] [Google Scholar]
- 3.Karila L, Zarmdini R, Petit A, et al. Cocaine addiction: current data for the clinician. Presse Med. 2014;43(1):9–17. doi: 10.1016/j.lpm.2013.01.069. [DOI] [PubMed] [Google Scholar]
- 4.Turillazzi E, Bello S, Neri M, et al. Cardiovascular effects of cocaine: cellular, ionic and molecular mechanisms. Curr Med Chem. 2012;19(33):5664–5676. doi: 10.2174/092986712803988848. [DOI] [PubMed] [Google Scholar]
- 5.Kloner RA, Hale S, Alker K, Rezkalla S. The effects of acute and chronic cocaine use on the heart. Circulation. 1992;85(2):407–419. doi: 10.1161/01.cir.85.2.407. [DOI] [PubMed] [Google Scholar]
- 6.Tsui JI, Herman DS, Kettavong M, et al. Chronic pain and hepatitis C virus infection in opioid dependent injection drug users. J Addict Dis. 2011;30(2):91–97. doi: 10.1080/10550887.2011.554775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cottler LB, Callahan C, Striley CL. HealthStreet: a community-based approach to include mental health in public health research. In: Cottler LB, editor. Mental Health in Public Health: The Next 100 Years. New York, NY: Oxford University Press; 2011. pp. 247–273. [Google Scholar]
- 8.Cottler LB, Striley CW, O'Leary C, et al. Engaging the community in research with the HealthStreet model: national and international perspectives. In: Alving B, Dai K, Chan SHH, editors. Translational Medicine – What, Why, and How: An International Perspective. Vol. 3. Basel, Switzerland: Karger; 2013. pp. 98–109. [Google Scholar]
- 9.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.SAS Institute, Inc. SAS version 9.4. Cary, NC: SAS Institute Inc; 2013. [Google Scholar]
- 11.Storer BE, Kim C. Exact properties of some exact test statistics for comparing two binomial proportions. J Am Stat Assoc. 1990;85:146–155. [Google Scholar]
- 12.Merline AC, O'Malley PM, Schulenberg JE, et al. Substance use among adults 35 years of age: prevalence, adulthood predictors, and impact of adolescent substance use. Am J Public Health. 2004;94(1):96–102. doi: 10.2105/ajph.94.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weston BW, Krishnaswami S, Gray MT, et al. Cocaine use in inner city African American research volunteers. J Addict Med. 2009;3(2):83–88. doi: 10.1097/ADM.0b013e31817dd851. [DOI] [PubMed] [Google Scholar]
- 14.Results from the 2004 National Survey on Drug Use and Health. Rockville, MD: SAMHSA; 2006. Substance Abuse and Mental Health Services Administration (SAMHSA) [Google Scholar]
- 15.Baumeister SE, Tossmann P. Association between early onset of cigarette, alcohol and cannabis use and later drug use patterns: an analysis of a survey in European metropolises. Eur Addict Res. 2005;11(2):92–98. doi: 10.1159/000083038. [DOI] [PubMed] [Google Scholar]
- 16.Striley CW, Johnson SD, Cottler LB. Health care disparities among out-of treatment cocaine users in St. Louis. Mo Med. 2008;105(1):72–78. [PubMed] [Google Scholar]
- 17.Kandel D, Yamaguchi K. From beer to crack: developmental patterns of drug involvement. Am J Public Health. 1993;83(6):851–855. doi: 10.2105/ajph.83.6.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flack JM, Ferdinand KC, Nasser SA. Epidemiology of hypertension and cardiovascular disease in African Americans. J Clin Hypertens (Greenwich) 2003;5(1 Suppl 1):5–11. doi: 10.1111/j.1524-6175.2003.02152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norris KC, Thornhill-Joynes M, Robinson C, et al. Cocaine use, hypertension, and end-stage renal disease. Am J Kidney Dis. 2001;38(3):523–528. doi: 10.1053/ajkd.2001.26845. [DOI] [PubMed] [Google Scholar]
- 20.US Department of Health and Human Services. Healthy People 2010. [Accessed October 3, 2014]; Available at: http://www.cdc.gov/nchs/healthy_people/hp2010.htm.
- 21.Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41(5):778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 22.Sacks JJ, Luo YH, Helmick CG. Prevalence of specific types of arthritis and other rheumatic conditions in the ambulatory health care system in the United States, 2001-2005. Arthritis Care Res (Hoboken) 2010;62(4):460–464. doi: 10.1002/acr.20041. [DOI] [PubMed] [Google Scholar]
- 23.Lee KC, Ladizinski B, Nutan FN. Systemic complications of levamisole toxicity. J Am Acad Dermatol. 2012;67(4):791–792. doi: 10.1016/j.jaad.2011.11.969. [DOI] [PubMed] [Google Scholar]
- 24.Strazzula L, Brown KK, Brieva JC, et al. Levamisole toxicity mimicking autoimmune disease. J Am Acad Dermatol. 2013;69(6):954–959. doi: 10.1016/j.jaad.2013.07.037. [DOI] [PubMed] [Google Scholar]
- 25.Manchikanti L, Cash KA, Damron KS, et al. Controlled substance abuse and illicit drug use in chronic pain patients: an evaluation of multiple variables. Pain Physician. 2006;9(3):215–225. [PubMed] [Google Scholar]
- 26.Ives TJ, Chelminski PR, Hammett-Stabler CA, et al. Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Serv Res. 2006;6:46. doi: 10.1186/1472-6963-6-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mertens JR, Lu YW, Parthasarathy S, et al. Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: comparison with matched controls. Arch Intern Med. 2003;163(20):2511–2517. doi: 10.1001/archinte.163.20.2511. [DOI] [PubMed] [Google Scholar]