Abstract
Background
To date, no investigators have examined electronically recorded self-weighing behavior beyond nine months or the underlying mechanisms of how self-weighing may impact weight change.
Objective
1) Examine electronically recorded self-weighing behavior in a weight loss study; 2) examine the possible mediating effects of adherence to energy intake (EI) and energy expenditure (EE) goals on the association between self-weighing and weight change.
Design
This was a secondary analysis of the self-efficacy enhancement (SE) arm of the Self Efficacy Lifestyle Focus (SELF) trial, an 18-month randomized clinical trial.
Participants/setting
The study was conducted at the University of Pittsburgh (2008–2013). Overweight or obese adults with at least one additional cardiovascular risk factor were eligible.
Intervention
Participants in the SE arm were given a scale (Carematix, Inc.) and instructed to weigh at least 3 days/week or every other day. The scale date- and time-stamped each weighing episode, storing up to 100 readings.
Main outcome measures
Weight was assessed every six months. Adherence to EI goal and EE goal was calculated on a weekly basis using paper diary data.
Statistical analyses performed
Linear mixed modeling and mediation analyses were used.
Results
The sample (N=55) was 80% female, 69% Non-Hispanic White, with mean (SD) 55.0 (9.6) years old and a BMI of 33.1 (3.7) kg/m2. Adherence to self-weighing declined over time (p<0.001). From baseline to 6 months, there was a significant mediation effect of adherence to EI (p=0.02) and EE goals (p=0.02) on the association between adherence to self-weighing and percent weight change. Mediation effects were not significant during the second and third 6-month periods of the study.
Conclusions
The objectively measured adherence to self-weighing declined over 18 months. During the first six months, self-weighing directly impacted weight change and indirectly impacted weight change through changes in EI and EE.
Keywords: self-weighing, weight loss, behavior, energy intake, energy expenditure, electronic scale
Background
Self-monitoring of body weight has been recommended as a component of standard behavioral treatment (SBT) for weight loss1, a strategy also recommended by the Clinical Guidelines for Treatment of Overweight and Obesity of the National Heart, Lung, and Blood Institute.2 Recent studies have demonstrated that frequent self-weighing is associated with greater weight loss3–7, less weight regain8,9 and better weight gain prevention.10–12
A weakness of the reported studies was the method used to assess self-weighing. Most of the studies used self-report methods and queried the participants retrospectively about the frequency of self-weighing (e.g., daily, weekly). For example, some studies used a single question asking about frequency of self-weighing with response options being never, about once a year or less, every other month, once a month, once a week, once a day, or more than once a day.6,9–16 However, these self-report methods might not accurately reflect the actual weighing behavior because self-reporting tends to provide an over-reporting17,18 or recall bias19 of self-weighing frequency. Thus, more objective measures of self-weighing frequency are needed to validate the association of a self-weighing intervention strategy with weight loss.
To the best of our knowledge, only three of the recent studies have used electronic scales to objectively measure self-weighing behaviors.4,5,20 Vanwormer and colleagues used a telemonitoring scale (Thin-Link, Cardiocom, LLC., Chanhassen, MN) that transmitted weight data automatically to the research center through a telephone land line.5 Gokee-LaRose reported using a scale that stored weight data for 31 days.4 Steinberg et al. used a smart scale that displayed current weight and sent the data directly to a website (www.bodytrace.com) via the wireless cellular network.20 The limitations of these studies included small and homogeneous samples and short-term follow-up (e.g. 6 months), limiting the generalizability of the findings.
Additionally, a few studies reported adherence to self-weighing over a short period of time, e.g., six months. Gokee-Larose et al. reported that at the end of a 10-week intervention approximately 90% of the participants weighed themselves daily, a rate that decreased significantly at the 20-week follow-up.4 This pattern of initial high level of adherence to self-weighing followed by a gradual decrease after approximately 3 months has also been reported by others.14,20 Further, previously published studies have provided evidence for a gradual decline in adherence to self-monitoring of diet and exercise, which becomes worse when treatment sessions and interventionist contact decrease.21 Although research related to self-monitoring of diet and exercise is extensive, it remains unclear whether the pattern of adherence to self-weighing, a component of self-monitoring, is similar to or differs from that of long-term self-monitoring of diet and exercise.
Moreover, no study has reported the underlying mechanisms of how self-weighing impacts weight change. Mediation analysis can determine the impact of each link in a hypothetical chain of events and define the contribution of different program components, which provides an explicit check on an intervention’s theoretical underpinnings and whether the proposed change process was achieved.22 Exploring these mechanisms will provide data to inform interventions to better counsel participants on the use of self-weighing for weight management.
According to self-regulation theory, motivation for behavioral change results from the interplay among awareness, self-observation, recording, and self-evaluation.23 Regular self-weighing may permit an individual to increase his or her awareness of eating and exercise behaviors, which may result in changes in balance of energy intake and expenditure, which may impact weight loss. 24 Therefore, we conducted mediation analysis to examine if self-weighing impacted weight loss through changes in eating and exercise behaviors.
The aims of our study were to 1) examine electronically recorded self-weighing behavior in a long-term weight loss study; and 2) examine the potential mediating effects of adherence to energy intake / expenditure goals on the association between self-weighing and percent weight change. Mediation analysis may identify the underlying process or mechanisms for the impact of self-weighing on weight change
Methods
Study design
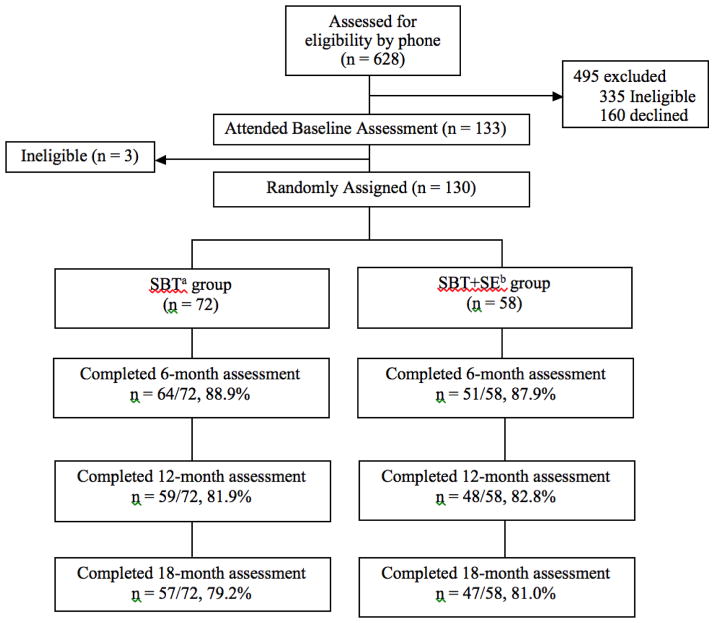
This was a secondary analysis of data (N=58) from the self-efficacy enhancement (SBT+SE) arm of the Self-Efficacy Lifestyle Focus (SELF) trial. Since only the participants in SBT+SE group were provided an electronic scale to weigh themselves at home, only the data from the SBT+SE arm was used for data analysis. The SELF trial was a 2-group, single-center, 18-month randomized clinical trial of a behavioral weight loss intervention for obese/overweight adults (Figure 1).25 The study was conducted at the University of Pittsburgh (2008–2013). The primary outcome of the SELF trial was weight loss maintenance. Both groups received a standard behavior treatment (SBT) intervention to promote weight loss that included a calorie- and fat-restricted diet.26 SBT is comprised of group-based cognitive-behavioral intervention strategies, daily dietary goals, weekly physical activity goals, as well as self-monitoring of dietary intake and physical activity. Group meetings were held in-person at the research center weekly for the first month, every two weeks in the second month, and monthly for the remainder of the first year; then, every 6 weeks for months 13–18. In addition to the group sessions, participants in the SBT+SE group met in person with their interventionist on a one-to-one basis. The interventionists for the trial were master-level registered dietitians/nutritionists and exercise physiologists. They implemented the self-efficacy based strategies and worked with the participant to develop jointly tailored, incremental goals for diet and physical activity to facilitate weight loss. During the first 12 months, the one-to-one sessions were held every two weeks; thereafter sessions were held at least monthly. Telephone sessions were available in place of face-to-face sessions at participant’s request. Individuals in the SBT+SE group were also provided with a scale (Carematix, Inc., Chicago, IL) to weigh themselves at home at least three times per week or every other day. The University of Pittsburgh Institutional Review Board approved the study protocol and all participants provided written informed consent.
Figure 1.
Assessment and Assignment of Participants in Self-Efficacy Lifestyle Focus (SELF) Trial
aSBT=standard behavioral treatment; bSE=self-efficacy enhancement
Reproduced with permission from Burke LE, et al, 201525 © 2015 The Obesity Society.
Sample
Overweight or obese adults with at least one additional risk factor for cardiovascular disease, e.g., dyslipidemia, hypertension, cigarette smoking, were eligible. During screening for eligibility, participants were asked to reasonably assess whether or not they would be able to commit to an 18-month intervention. They were excluded if they were planning a pregnancy or relocation that would prevent them from attending the group sessions. To minimize attrition, individuals who participated in weight loss treatment within the last 6 months were not eligible. Assessments were conducted every six months throughout the study as described below.
Measures
Socio-demographic Questionnaire
Baseline socio-demographic factors were assessed with The Socio-demographic and Lifestyle Questionnaire, a self-administered, standardized questionnaire developed by the Center for Chronic Disorders at the University of Pittsburgh.
Weight
A digital scale (Tanita Corporation of America, Inc., Arlington Heights, IL, USA) was used to measure weight in pounds at baseline, 6, 12, and 18 months. Participants wore light clothing, no shoes, and had fasted overnight. Weight was transformed into percent change relative to baseline levels (t=0). That is, percent weight change was defined as ([weightt − weight0] / weight0) × 100%, t = 6, 12, 18 months.
Self-weighing
Each self-weighing episode at home was date- and time-stamped using the scale provided, which stored a maximum of 100 readings that were uploaded every 3 months to a server in the research center. If data could not be transmitted from the scale to the server in the research center, the scale was returned to the manufacturing company for retrieval of the weight data. Some of the retrieved data remained incomplete as a result of: 1) missing date-stamps due to technical issues and 2) missing both date-stamps and weights.
The outcome variables for analysis were calculated in two ways over three six-month blocks of time: 1) frequency of self-weighing was defined as the mean number of days of self-weighing per week; 2) percent time adherent: (number of weeks adherent to self-weighing / total number of weeks in each 6-month block) × 100%, where adherence for each week was defined as self-weighing ≥3 days / week.
Adherence to energy intake (EI) goal
Adherence to energy intake goals was calculated on a weekly basis using the data from the paper diary recording of dietary intake. Adherence to the EI goal was calculated by dividing the total number of calories consumed per week by the weekly calorie goal, then multiplying by 100 to express the value as a percentage, e.g., if a participant with a daily calorie goal of 1800 kilocalories (kcal) [weekly goal = 12,600] reported consuming 10,500 total kcal in a week, the level of adherence to the energy goal was calculated as 83.3% (10,500/12,600 × 100%).27 Adherence to the EI goal was categorized as adherent (reported consuming 85%–115% of the weekly goals) and non-adherent (reported consuming <85% or >115% of the weekly goals) on a weekly basis. If a diary was not returned, adherence to EI goals was coded as non-adherent for that week. For the analysis, the proportion of weeks participants were adherent to the EI goal was calculated, dividing the number of weeks adherent to the calorie goal by the total number of weeks in each six-month period.
Adherence to energy expenditure (EE) goal
Adherence to energy expenditure goal was calculated on a weekly basis using the data from the paper diary recording exercise minutes. Adherence was calculated using the reported weekly minutes spent exercising divided by the weekly goal. For example, adherence for a person reporting 140 minutes of exercise per week with a goal of 150 minutes, would be 93% (140/150 × 100%). Since the exercise goal was increased over the first six weeks, the denominator was changed accordingly. Adherence to the EE goal was examined as a binary variable based on whether participants achieved the goal each time their diaries was submitted (adherent: ≥100% of weekly goal, nonadherent: <100% of weekly goal). The adherence was coded as 0 if a diary was not returned for the week. For the data analysis, the percentage of weeks that participants adhered to the EE goal in each six-month period was calculated.
Statistical Analysis
Statistical analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC. 2012) and Mplus (version 7.31, Muthén & Muthén, Los Angeles, CA, 2012) for Windows. Significance was set at ≤ 0.05 for two-sided hypothesis testing. Summary statistics were reported as mean and standard deviation (SD) as well as frequencies as number (n) and percent (%). The normality of variables was assessed using the Shapiro-Wilk test and histograms were also reviewed.
Linear mixed modeling was used to examine the longitudinal association between self-weighing and weight change over 18 months. The scale data that were missing a date-stamp due to transmission issues were imputed using data retrieved by the company while the scale data that were missing dates and weights were coded as missing. In linear mixed models, individuals with missing data at some time points are included in the analysis, not deleted. Sensitivity analyses were conducted using participants with missing data and coding the missing as zero. Also, the conclusions did not change when the analysis was conducted using the smaller sample with complete data. The results from sensitivity analyses supported the robustness of our findings.
Mediation analysis28 was used to assess the extent that EI or EE was a mechanism or process (mediator) that affected the relationship between percent weight change and self-weighing. The steps, models, and effects used in these analyses are displayed in Table 1. Model 1 assessed the total effect, the impact of self-weighing on percent weight change. Model 2 assessed the effect of self-weighing on EI or EE. Model 3 assessed the effect of EI or EE on percent weight change. Model 4 assessed the direct effect of self-weighing by adjusting for EI or EE. Since adherence to EI and EE were highly collinear, they could not be included together in any model. When the results in the first three models were significant then a mediating effect might exist.29 In the fourth model, if self-weighing was not significant, evidence for complete mediation existed. If both self-weighing and EI or EE are significant in Model 4, evidence for partial mediation exists. The indirect effect represents the portion of the relationship between self-weighing and percent weight change that is mediated by EI or EE. The indirect effect was calculated by multiplying the beta coefficient of the mediator (EI or EE) from the model with only the mediator and the outcome (percent weight change) and the coefficient of the mediator from the model with both self-weighing and the mediator. Statistics for the indirect effect were generated using a bootstrap method with 5000 repetitions. All model fit indices indicated a good fit for the mixed linear models.
Table 1.
The steps, models, and effects used in the analyses of data from Self-Efficacy Lifestyle Focus (SELF) Trial
| Models | Effects |
|---|---|
| Model 1 | Total effect: the impact of self-weighing on percent weight change |
| Model 2 | The effect of self-weighing on EIa or EEb |
| Model 3 | The effect of EI or EE on percent weight change |
| Model 4 | Direct effect of self-weighing by adjusting for EI or EE |
EI = energy intake,
EE = energy expenditure
Results
Fifty-five participants were included in the analysis (three were excluded for new diagnoses of type2 diabetes or cancer, or did not use the scale for weighing). Seventeen (31.0%) participants had complete data for self-weighing. Of the 7550 self-weighing records, 15.3% were imputed using retrieved dates. At baseline, 80% of the participants were female, 69% Non-Hispanic White, 64% married or cohabiting, and 67% had a household income >$50,000. The participants had a mean age of 55.0 (9.6) years, 15.9 (2.6) mean years of education, and a mean BMI of 33.1 (3.7)
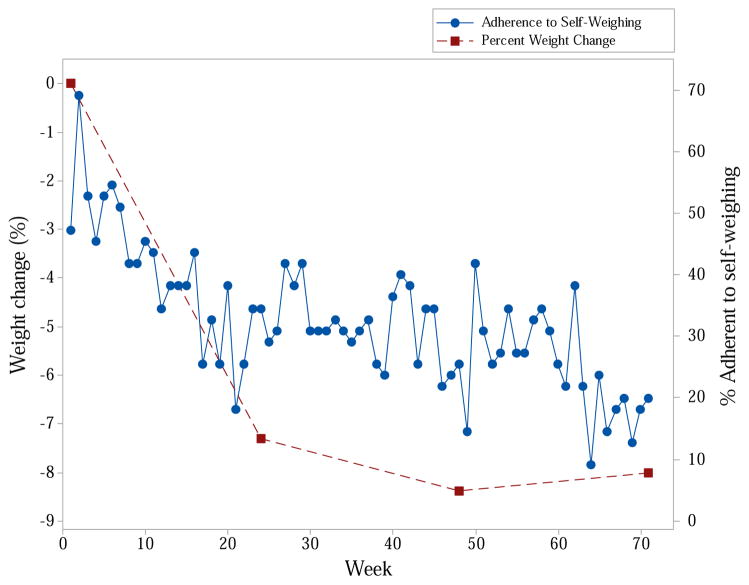
During the first 6 months, the mean days of self-weighing per week was 2.2 (1.1); declined to 1.8 (1.1) over the second 6-month period and to 1.5 (1.20) in the final 6-months (F=12.14, p<0.001). Percent time of adherence to self-weighing declined over the three times from 44.1% to 36.9% to 29.3% (F=23.23, p<0.001). The percentage of participants adherent to self-weighing also declined over the 18 months (Figure 2). The percent weight change was −7.3%, −8.4%, and −8.0% at 6, 12 and 18 months (F=5.98, p=0.005), respectively.
Figure 2.
Percentage of Sample Adherent to Self-Weighing and Percent Weight Change over Time in Self-Efficacy Lifestyle Focus (SELF) Trial
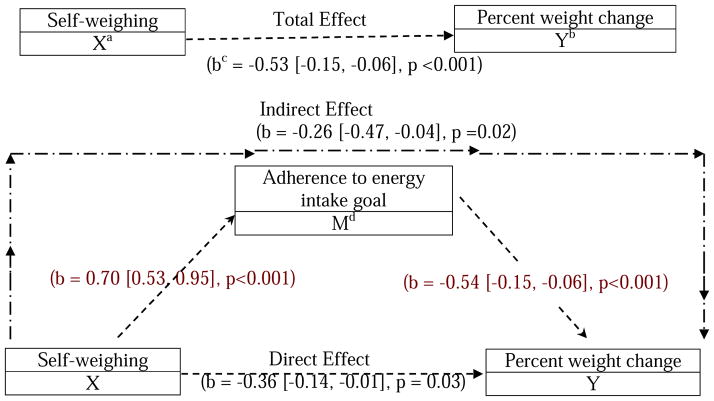
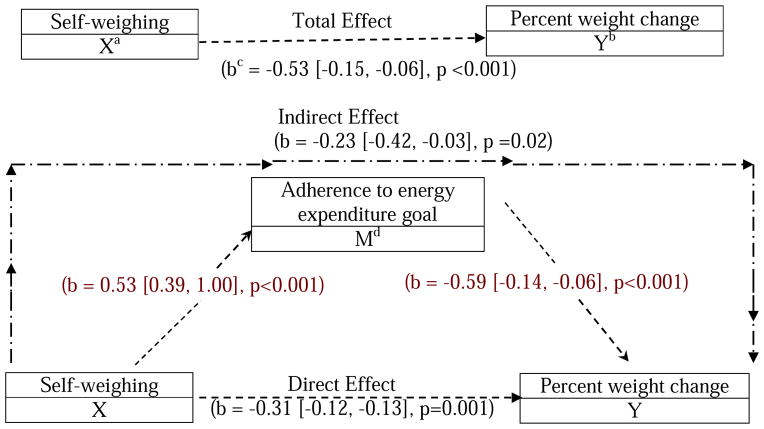
The percent time that participants were adherent to self-weighing was linearly associated with percent weight change over 18 months (b=−0.032, p=0.047), indicating that an increase in one week of adherence to self-weighing resulted in 0.03% of weight loss over 18 months. For the mediation effect, from baseline to 6 months, there was an association between adherence to self-weighing and percent weight change (total effect, b=−0.53, p<0.001), indicating that an increase in one week of adherence to self-weighing resulted in 0.53% of weight loss during the first 6 months of study. When examining adherence to EI goal as a mediator (Figure 3), there was a significant direct (b=−0.36, p=0.03) and indirect (b=−0.26, p=0.02) effect of self-weighing on percent weight change. Similarly, when examining adherence to EE goal as a mediator (Figure 4), there was also a significant direct (b=−0.31, p=0.001) and indirect (b=−0.23, p=0.02) effect of self-weighing on percent weight change. These results indicate that both adherence to EI and EE goals had a partial mediation effect on the association between adherence to self-weighing and weight change for the first 6 months since the total, direct and indirect effects were all significant. All the models fit well.
Figure 3.
Mediation Effect of Adherence to Energy Intake Goal from 0 to 6 Months in Self-Efficacy Lifestyle Focus (SELF) Trial
aX = predictor, bY= outcome, cb= beta coefficients from the linear mixed models, followed by the 95% CI and p-values, dM = mediator
Figure 4.
Mediation Effect of Adherence to Energy Expenditure Goal from 0 to 6 Months in Self-Efficacy Lifestyle Focus (SELF) Trial
aX = predictor, bY= outcome, cb= beta coefficients from the linear mixed models, followed by the 95% CI and p-values, dM = mediator
However, during the second and third 6-month period, adherence to the EI goal had no significant mediation since the indirect effects were not significant (the second 6 months: indirect (b=0.12, p=0.19); the third 6 months: indirect (b=−0.005, p=0.52). Adherence to the EE goal had a significant mediation effect during the second 6 months: indirect (b=−0.03, p=0.01), while there was no significant mediation effect during the third 6 months: indirect (b=−0.02, p=0.09).
Discussion
This is the first study to look at the mediation effects of using the longitudinal objectively assessed self-weighing data. The use of date-stamped data from an electronic scale revealed that adherence to self-weighing declined throughout the 18-month follow-up. Both adherence to EI and EE goals showed partial mediation effects on the association between adherence to self-weighing and weight change during the first 6 months of the follow-up.
Data from this study in which participants used an electronic scale that documented the weighing events, confirmed that self-weighing was significantly associated with weight loss. The data also demonstrated a decline in adherence to self-weighing over the 18-month weight loss study, a pattern that is consistent with self-weighing adherence even over shorter periods (e.g., six months).4,12,14,20 Moreover, data from this investigation replicated the pattern of declining adherence over time that is commonly observed in numerous other lifestyle behaviors, e.g., self-monitoring of diet, changing one’s eating habits27,21, and exercise programs.30 This growing body of evidence demonstrating a decline in adherence across numerous behavioral domains heightens the need for the development of new strategies that can enhance and sustain adherence to lifestyle interventions that target weight loss.
Our mediation results showed that adherence to both EI and EE goals had partial mediation effects on the association between adherence to self-weighing and weight change during the first 6-month period, indicating that self-weighing not only directly impacts weight change but also indirectly impacts weight outcome through changes in dietary intake and exercise behaviors. The magnitude of the effect of self-weighing on weight change was reduced when either EE or EI was added to the models. The beta coefficient changed from −.53 to −0.36 for EI and −0.53 to −0.31 for EE, indicating that the effect of self-weighing on percent weight loss decreased after adjusting the EI goal or EE goal. By observing the scale readings, participants may observe small weight changes and relate this to current diet or exercise behaviors, which in turn can support improved self-regulation of related behaviors. Realization of how body weight fluctuates may allow individuals to focus on their behaviors rather than weight outcomes. The results did not demonstrate significant mediation effects of adherence to EI and EE goals during the second and third 6-month period of study, which may be explained by the declining adherence and thus the increasing amount of missing data that reduced the variability for each behavior variable.
The definition of adherence to prescribed self-weighing protocols varies across reported studies. VanWormer et al. defined adherence to self-weighing as the percentage of days self-weighed (i.e., total number of days self-weighed divided by the total number of days in the active treatment phase).5 Gokee-Larose et al. reported the proportion of participants who, at the end of the 10-week intervention and the 20-week follow-up, had adhered to weighing themselves daily.4 Other investigators have simply reported mean days per week of self-weighing.31 The inconsistent definition of adherence used across studies underscores the need for established measures and a consistent definition of adherence to self-weighing so that adherence can be compared across studies and different populations.
In this study, some self-weighing data were incomplete due to technical issues, e.g., data not transmitted via the modem. Advances in technology permit real-time transmission of self-weighing data, limiting data loss. Thus, the use of currently available technology-supported scales that provide date- and time-stamped measures of self-weighing may facilitate future studies of adherence to self-weighing and its association with weight change.
The main limitation of this study is missing data due to technical issues encountered with the scale that was available at the onset of our study. Also, the generalizability of these findings may be limited due to the predominantly Non-Hispanic-White female sample. Additionally, the use of paper-and-pencil diaries rather than use of mobile technology to collect data in real time and thus avoid recall of food intake or the use of wearable sensors to collect objective measures of EE to examine adherence to exercise is a limitation. A major strength of the study was the use of a scale equipped with a date-stamp to document self-weighing episodes and adherence during an 18-month weight loss intervention study. This is also the first paper to explore the underlying mechanism of how self-weighing impacts weight change. Exploring the role of mediators will provide data to inform interventions to better counsel participants on the use self-weighing for weight management.
Conclusion
In conclusion, the data from the electronic scales in this study demonstrated that adherence to self-weighing over 18 months was significantly associated with weight change. This was the first study to use an electronic scale that stored data with a date stamp, permitting the examination of documented adherence to self-weighing. The study was also the first one to examine the underlying mechanism of the impact of self-weighing on weight change and therefore adds to the literature supporting the use of electronic self-weighing as a strategy to enhance weight loss. The findings from the mediation analysis provide evidence for researchers to develop new strategies that address self-weighing in future weight loss interventions as a means to enhance individual’s ability to self-regulate food intake and the level of physical activity.
Acknowledgments
Funding/Support Disclosure: P01 NR010949-01 Adherence and HRQoL: Translation of Interventions, and R01 Self-Efficacy Based Treatment for Long-Term Weight Loss, MidCareer Mentorship Award NIH K24NR010742
Footnotes
ClinicalTrial registration: NCT00896194
Conflict of Interest: Authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cooper Z, Fairburn CG. A new cognitive behavioural approach to the treatment of obesity. Behav Res Ther. 2001;39(5):499–511. doi: 10.1016/s0005-7967(00)00065-6. [DOI] [PubMed] [Google Scholar]
- 2.National Institute of Health. National Heart Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 3.Lally P, Chipperfield A, Wardle J. Healthy habits: efficacy of simple advice on weight control based on a habit-formation model. Int J Obes (Lond) 2008;32(4):700–707. doi: 10.1038/sj.ijo.0803771. [DOI] [PubMed] [Google Scholar]
- 4.Gokee-Larose J, Gorin AA, Wing RR. Behavioral self-regulation for weight loss in young adults: a randomized controlled trial. Int J Behav Nutr Phys Act. 2009;6:10. doi: 10.1186/1479-5868-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.VanWormer JJ, Martinez AM, Martinson BC, et al. Self-weighing promotes weight loss for obese adults. Am J Prev Med. 2009;36(1):70–73. doi: 10.1016/j.amepre.2008.09.022. [DOI] [PubMed] [Google Scholar]
- 6.Welsh EM, Sherwood NE, VanWormer JJ, Hotop AM, Jeffery RW. Is frequent self-weighing associated with poorer body satisfaction? Findings from a phone-based weight loss trial. J Nutr Educ Behav. 2009;41(6):425–428. doi: 10.1016/j.jneb.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zheng Y, Mattos M, Sereika SM, et al. Association between Objectively Recorded Self-Weighing and Weight Change in a Weight Loss Trial. Annals of Behavioral Medicine. 2013;45(Suppl):s124. [Google Scholar]
- 8.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006;355(15):1563–1571. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 9.Sherwood NE, Crain AL, Martinson BC, et al. Enhancing long-term weight loss maintenance: 2 year results from the Keep It Off randomized controlled trial. Prev Med. 2013;56(3–4):171–177. doi: 10.1016/j.ypmed.2012.12.014. doi:110.1016/j.ypmed.2012.1012.1014. Epub 2012 Dec 1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household obesity prevention: Take Action--a group-randomized trial. Obesity (Silver Spring) 2011;19(10):2082–2088. doi: 10.1038/oby.2010.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.VanWormer JJ, Linde JA, Harnack LJ, Stovitz SD, Jeffery RW. Self-weighing frequency is associated with weight gain prevention over 2 years among working adults. Int J Behav Med. 2012;19(3):351–358. doi: 10.1007/s12529-011-9178-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gokee LaRose J, Tate DF, Gorin AA, Wing RR. Preventing weight gain in young adults: a randomized controlled pilot study. Am J Prev Med. 2010;39(1):63–68. doi: 10.1016/j.amepre.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sherwood NE, Jeffery RW, Pronk NP, et al. Mail and phone interventions for weight loss in a managed-care setting: weigh-to-be 2-year outcomes. Int J Obes (Lond) 2006;30(10):1565–1573. doi: 10.1038/sj.ijo.0803295. [DOI] [PubMed] [Google Scholar]
- 14.Linde JA, Jeffery RW. Testing a brief self-directed behavioral weight control program. Behav Med. 2011;37(2):47–53. doi: 10.1080/08964289.2011.568992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jeffery RW, French SA. Preventing weight gain in adults: the pound of prevention study. Am J Public Health. 1999;89(5):747–751. doi: 10.2105/ajph.89.5.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kong A, Beresford SA, Alfano CM, et al. Self-monitoring and eating-related behaviors are associated with 12-month weight loss in postmenopausal overweight-to-obese women. J Acad Nutr Diet. 2012;112(9):1428–1435. doi: 10.1016/j.jand.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Daniels T, Goodacre L, Sutton C, Pollard K, Conway S, Peckham D. Accurate assessment of adherence: self-report and clinician report vs electronic monitoring of nebulizers. Chest. 2011;140(2):425–432. doi: 10.1378/chest.09-3074. [DOI] [PubMed] [Google Scholar]
- 18.Ross-Degnan D, Pierre-Jacques M, Zhang F, et al. Measuring adherence to antiretroviral treatment in resource-poor settings: the clinical validity of key indicators. BMC Health Serv Res. 2010;10:42. doi: 10.1186/1472-6963-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stone AA, Turkkan JS, Bachrach CA, Jobe JB, Kurtzman HS, Cain VS, editors. The Science of Self-Report: Implications for Research and Practice. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- 20.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. The efficacy of a daily self-weighing weight loss intervention using smart scales and email. Obesity (Silver Spring) 2013 doi: 10.1002/oby.20396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011;111(1):92–102. doi: 10.1016/j.jada.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lockwood CM, DeFrancesco CA, Elliot DL, Beresford SA, Toobert DJ. Mediation analyses: applications in nutrition research and reading the literature. J Am Diet Assoc. 2010;110(5):753–762. doi: 10.1016/j.jada.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kanfer F, Goldstein A. Helping people change. 4. New York: Pergamon Press; 1990. [Google Scholar]
- 24.Butryn ML, Phelan S, Hill JO, Wing RR. Consistent self-monitoring of weight: a key component of successful weight loss maintenance. Obesity (Silver Spring) 2007;15(12):3091–3096. doi: 10.1038/oby.2007.368. [DOI] [PubMed] [Google Scholar]
- 25.Burke LE, Ewing LJ, Ye L, et al. The SELF trial: A self-efficacy-based behavioral intervention trial for weight loss maintenance. Obesity (Silver Spring) 2015 doi: 10.1002/oby.21238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burke LE, Choo J, Music E, et al. PREFER study: a randomized clinical trial testing treatment preference and two dietary options in behavioral weight management--rationale, design and baseline characteristics. Contemporary clinical trials. 2006;27(1):34–48. doi: 10.1016/j.cct.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 27.Acharya SD, Elci OU, Sereika SM, et al. Adherence to a behavioral weight loss treatment program enhances weight loss and improvements in biomarkers. Patient Prefer Adherence. 2009;3:151–160. doi: 10.2147/ppa.s5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lockhart G, MacKinnon DP, Ohlrich V. Mediation analysis in psychosomatic medicine research. Psychosom Med. 2011;73(1):29–43. doi: 10.1097/PSY.0b013e318200a54b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goodpaster BH, Delany JP, Otto AD, et al. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. JAMA : the journal of the American Medical Association. 2010;304(16):1795–1802. doi: 10.1001/jama.2010.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. Daily self-weighing and adverse psychological outcomes: a randomized controlled trial. Am J Prev Med. 2014;46(1):24–29. doi: 10.1016/j.amepre.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]