Introduction
Pruritic papular eruption of HIV (PPE) represents an intensely pruritic papular rash with greatest severity on the extensor surfaces of extremities. It is one of the most common cutaneous manifestations in HIV-infected individuals, in whom prevalence ranges between 11% and 46% depending on geographic location.1, 2, 3, 4, 5 Persistent or recurrent PPE despite effective antiretroviral therapy (ART) may be associated with higher viral load at ART initiation.6 Although pathogenesis is uncertain, an exaggerated immunologic reaction to arthropod bites has been suggested because of geographical restriction to the tropics, localization to the extremities, similarity in histology, and increased peripheral eosinophil counts.1 The optimum treatment pathway is poorly defined because of lack of evidence for different treatment modalities.
We report a case of recurrent PPE responding well to oral thalidomide during a 3-month treatment period.
Case report
A 44-year-old Zimbabwean woman living in the United Kingdom since 1998 had HIV diagnosed in 2006. At the time of diagnosis, her CD4 count was 204 cells per cubic millimeter and viral load was 498,000 copies per milliliter. ART was started, which resulted in a sustained suppression of HIV viremia (viral load <40 copies/mL, CD4 >600 cells per cubic millimeter).
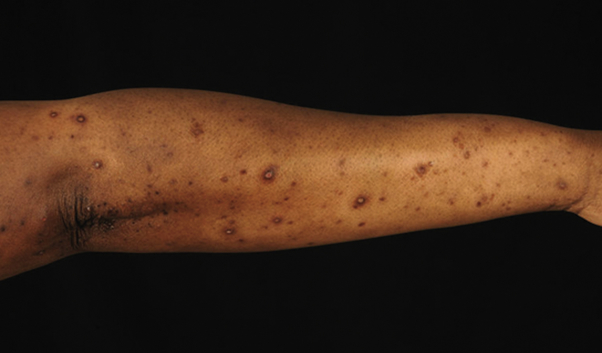
A year later a pruritic eruption developed starting on the upper arms and spreading to the hands, thighs, and back. Initial treatment with topical betamethasone valerate 0.1% was effective, but a relapse occurred 4 years later. On returning she described a 1-month history of an intensely pruritic rash affecting the trunk, arms, and legs. Examination found numerous monomorphic hyperpigmented papules on the extensor surface of the limbs and on the trunk (Fig 1). The face, hands, feet, and mucous membranes were spared.
Fig 1.
Pruritic papular eruption. Baseline appearance of the upper limb shows a papular rash affecting the extensor surface.
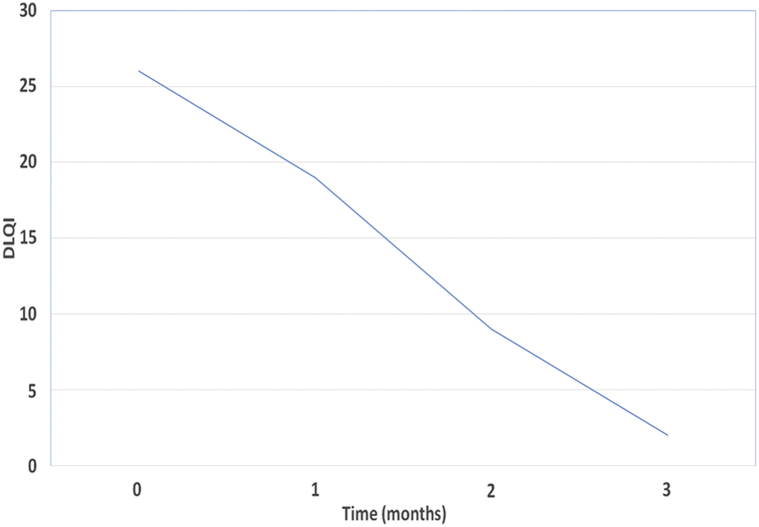
Histologic analysis found a dermal perivascular lymphocytic infiltrate with scattered eosinophils (Fig 2). The patient had PPE diagnosed based on the clinical findings and histology.
Fig 2.
Pruritic papular eruption. Histologic confirmation of the diagnosis shows a perivascular lymphocytic infiltrate to the dermis with scattered eosinophils. (Hematoxylin-eosin stain.)
Initial management with clobetasol propionate 0.05% ointment applied daily and high dose oral antihistamines was minimally effective. Thirty narrowband ultraviolet B phototherapy treatments led to significant improvement, but a relapse occurred 2 weeks after termination of therapy.
Dapsone was considered but precluded because of glucose-6-phosphate dehydrogenase deficiency. Based on its efficacy in HIV-infected patients with prurigo nodularis, the patient was prescribed a trial of thalidomide at a dose of 100 mg daily.7 Before commencement of treatment, the patient was counselled regarding the risks of peripheral neuropathy and teratogenicity. Two forms of contraception, condoms and an intrauterine device, were used throughout the treatment period.
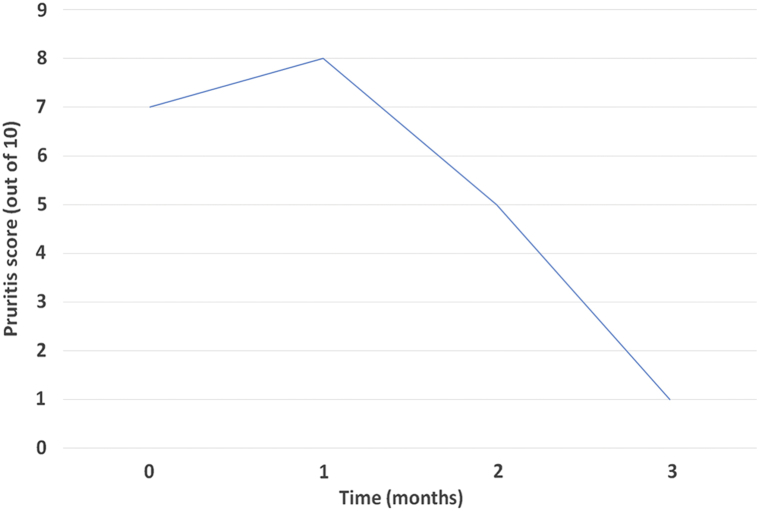
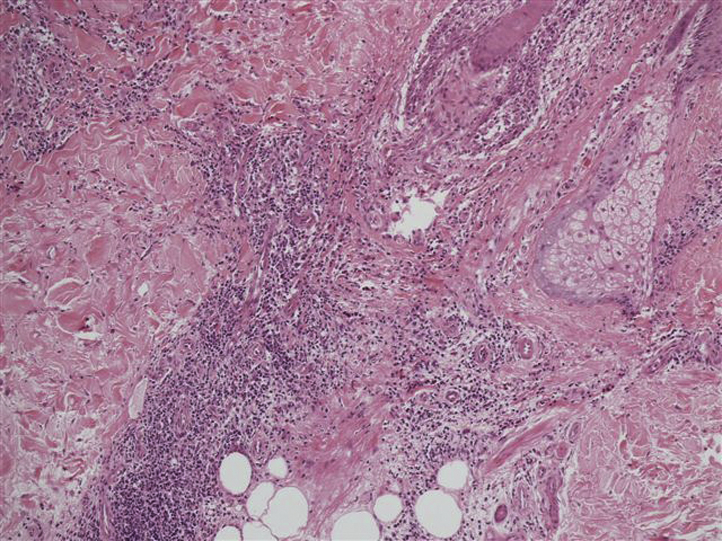
We measured baseline severity and response to treatment using the Dermatology Life Quality Index (DLQI) and a 10-cm visual analogue score (VAS) for pruritus. At the start of treatment, DLQI was 26/30 and VAS was 7/10. By 3 months of treatment, there was almost complete resolution of symptoms with a DLQI of 2/30 and VAS 1/10 (Fig 3, Fig 4). Thalidomide was withheld at 3 months followed by a 4-month remission. At the time of flare of the rash and pruritus, thalidomide was recommenced at the same daily dose, which led to similar improvement in symptoms. Treatment was withheld by the patient at 5 months. She reported only few residual pruritic papules, treated with topical betamethasone valerate 0.1% cream. PPE remains suppressed 5 months after treatment discontinuation. There were no significant adverse effects and no clinical evidence of thalidomide-induced peripheral neuropathy during either treatment period.
Fig 3.
Graph shows the reduction in DLQI during the treatment period from 26 down to 2.
Fig 4.
Graph shows the reduction in VAS pruritus score from 7 down to 1.
Discussion
Differential diagnoses to consider in patients with HIV and pruritus include PPE, prurigo nodularis, and eosinophilic folliculitis. In our case, there was no perifollicular inflammation on histology, which would be expected with eosinophilic folliculitis. In contrast to prurigo nodularis, the rash was papular rather than nodular, and the histology lacked typical features of compact orthohyperkeratosis, acanthosis, hypergranulosis, and papillary dermal fibrosis with vertical alignment of collagen fibers.8
Few studies have identified beneficial therapeutic approaches for PPE, and these are primarily observational studies, case series, or case reports. Currently, there are no randomized controlled trials undertaken to study interventions for PPE. For diagnosis before ART commencement, dramatic responses have been documented in response to ART initiation, with one study reporting complete resolution without recurrence in 86% of their cohort.9 Initial skin treatment in these circumstances may involve potent topical corticosteroids and high-dose oral antihistamines.10, 11 Narrowband ultraviolet B and psoralen and ultraviolet A have been reported to be effective, although the period of remission may be brief.12 Other systemic treatments reported to be effective in observational studies are dapsone and pentoxyfylline.11, 13
Oral thalidomide requires strict monitoring for the development of peripheral neuropathy, reported to occur in up to 55.6% of treated dermatologic patients.14 Compliance with pregnancy prevention is important as exposure to the fetus can lead to multiple birth defects, including phocomelia and thumb absence/hypoplasia.15 The mechanism for treating pruritic skin disease is not well characterized but may involve a combination of actions. Thalidomide acts as a central depressant with sedative properties, which may be beneficial in disrupting the itch-scratch cycle.16 In prurigo nodularis, a local effect on proliferated neural tissue has been suggested.17 Suppression of tumor necrosis factor alfa and increased production of cytokines, including interleukin-2 and interleukin-12 may also play a role.18
Our decision to run a trial of thalidomide was based on its efficacy and relative safety in a small case series of patients with HIV and prurigo nodularis and also its previously demonstrated efficacy in other pruritic conditions. In the case series by Maurer et al,7 all 8 subjects had a greater than 50% reduction of pruritus over an average of 3.4 months, and 7 of 8 patients had greater than 50% reduction in clinical scoring. The treatment was generally well tolerated without significant adverse effects, although a reversible thalidomide-induced peripheral neuropathy developed in 3 of 8 patients. No correlation was found between thalidomide and reduction of CD4 count. Viral load was not measured during thalidomide therapy.9 Our patient had sustained virologic suppression throughout both thalidomide treatment periods with viral load less than 40 copies per milliliter and CD4 counts between 600 and 800 cells per cubic millimeter.
We present a case of recurrent PPE responding to oral thalidomide. Further studies are needed to identify the optimum dosing regimen, efficacy, and safety in this population.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Resneck J.S., Van Beek M., Furmanski L. Etiology of pruritic papular eruption with HIV infection in uganda. JAMA. 2004;292:2614–2621. doi: 10.1001/jama.292.21.2614. [DOI] [PubMed] [Google Scholar]
- 2.Colebunders R., Mann J.M., Francis H. Generalized papular pruritic eruption in African patients with human immunodeficiency virus infection. AIDS. 1987;1:117–121. [PubMed] [Google Scholar]
- 3.Sivayathorn A., Srihra B., Leesanguankul W. Prevalence of skin disease in patients infected with human immunodeficiency virus in Bangkok, Thailand. Ann Acad Med Singapore. 1995;24:528–533. [PubMed] [Google Scholar]
- 4.Rosatelli J.B., Machado A.A., Roselino A.M. Dermatoses among Brazilian HIV-positive patients: correlation with the evolutionary phases of AIDS. Int J Dermatol. 1997;36:729–734. doi: 10.1046/j.1365-4362.1997.00293.x. [DOI] [PubMed] [Google Scholar]
- 5.Liautaud B., Pape J., DeHovitz J.A. Pruritic skin lesions. A common initial presentation of acquired immunodeficiency syndrome. Arch Dermatol. 1989;125:629–632. doi: 10.1001/archderm.125.5.629. [DOI] [PubMed] [Google Scholar]
- 6.Chua S.L., Amerson E.H., Leslie K.S. Factors associated with pruritic papular eruption of human immunodeficiency virus (HIV) infection in the antiretroviral therapy eta. Br J Dermatol. 2014;170:832–839. doi: 10.1111/bjd.12721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maurer T., Poncelet A., Berger T. Thalidomide treatment for prurigo nodularis in human immunodeficiency virus-infected subjects: efficacy and risk of neuropathy. Arch Dermatol. 2004;140:845–849. doi: 10.1001/archderm.140.7.845. [DOI] [PubMed] [Google Scholar]
- 8.Weigelt N., Metze D., Ständer S. Prurigo nodularis: systematic analysis of 58 histological criteria in 136 patients. J Cutan Pathol. 2010;37:578–586. doi: 10.1111/j.1600-0560.2009.01484.x. [DOI] [PubMed] [Google Scholar]
- 9.Castelnuovo B., Byakwaga H., Menten J., Schaefer P., Kamya M., Colebunders R. Can response of a pruritic papular eruption to antiretroviral therapy be used as a clinical parameter to monitor virological outcome? AIDS. 2008;22:269–273. doi: 10.1097/QAD.0b013e3282f313a9. [DOI] [PubMed] [Google Scholar]
- 10.Navarini A.A., Stoeckle M., Navarini S. Antihistamines are superior to topical steroids in managing human immunodeficiency virus (HIV)-associated papular pruritic eruption. Int J Dermatol. 2010;49:83–86. doi: 10.1111/j.1365-4632.2009.04279.x. [DOI] [PubMed] [Google Scholar]
- 11.Lakshmi S.J., Rao G.R., Ramalakshmi, Satyasree, Rao K.A., Prasad P.G., Kumar Y.H. Pruritic papular eruptions of HIV: A clinicopathologic and therapeutic study. Indian J Dermatol Venereol Leprol. 2008;74:501–503. doi: 10.4103/0378-6323.44318. [DOI] [PubMed] [Google Scholar]
- 12.Bellavista S., D'antuono A., Infusino S.D., Trimarco R., Patrizi A. Pruritic papular eruption in HIV: a case successfully treated with NB-UVB. Dermatol Ther. 2013;26:173–175. doi: 10.1111/j.1529-8019.2013.01545.x. [DOI] [PubMed] [Google Scholar]
- 13.Berman B., Flores F., Burke G. Efficacy of pentoxifylline in the treatment of papular pruritic eruption of HIV-infected persons. J Am Acad Dermatol. 1998;38:955–959. doi: 10.1016/s0190-9622(98)70159-8. [DOI] [PubMed] [Google Scholar]
- 14.Bastuji-Garin S., Ochonisky S., Bouche P. Incidence and risk factors for thalidomide neuropathy: a prospective study of 135 dermatologic patients. J Invest Dermatol. 2002;119:1020–1026. doi: 10.1046/j.1523-1747.2002.19502.x. [DOI] [PubMed] [Google Scholar]
- 15.Martínez-Frías M.L. The thalidomide experience: review of its effects 50 years later. Med Clin (Barc) 2012;139:25–32. doi: 10.1016/j.medcli.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 16.Daly B.M., Shuster S. Antipruritic action of thalidomide. Acta Derm Venereol. 2000;80:24–25. doi: 10.1080/000155500750012450. [DOI] [PubMed] [Google Scholar]
- 17.van den Broek H. Treatment of prurigo nodularis with thalidomide. Arch Dermatol. 1980;116:571–572. doi: 10.1001/archderm.116.5.571. [DOI] [PubMed] [Google Scholar]
- 18.Corral L., Kaplan G. Immunomodulation by thalidomide and thalidomide analogues. Ann Rheum Dis. 1999;58(Suppl 1):I107–I113. doi: 10.1136/ard.58.2008.i107. [DOI] [PMC free article] [PubMed] [Google Scholar]