Introduction
Pilomatricomas, or benign calcifying epitheliomas of Malherbe, are the most common hair follicle tumors. Rarely, these tumors may exceed 5 cm and are referred to as giant pilomatricomas. We report the case of an otherwise healthy 18-year-old Hispanic man with a firm, itchy, painful, and ulcerated tumor on the anterior aspect of the chest.
Case report
On presentation, the patient had an 8-cm × 9-cm firm, exophytic, pedunculated, reddish tumor with punctate ulcerations, yellow serous drainage, and linear hypertrophic scars at the base (Fig 1). The tumor was noted 6 years prior and had been slowly growing since. He denied any prior surgery or trauma to the affected area. There was no family history of similar lesions or known genetic syndromes. Biopsy results were nonspecific, including skin with hemorrhage and increased vasculature with large fibrohistiocytic cells. These histologic changes were considered reactive and unrepresentative of the larger mass. Therefore, the entire tumor was completely excised under tumescent anesthesia, sectioned, and submitted for further histopathologic analysis. Sectioning of the mass found significant calcification of the involved tissue (Fig 2). A delayed repair was planned pending further histologic evaluation.
Fig 1.
Giant pilomatricoma. An 18-year-old Hispanic man with an 8-cm × 9-cm firm, exophytic, pedunculated, reddish tumor with punctate ulcerations and yellow serous drainage on the anterior aspect of the chest.
Fig 2.
Gross macroscopic image of the sectioned tumor shows diffuse calcification after complete excision.
Routine hematoxylin-eosin staining of the tumor found aggregates of basaloid, matrical cornified material with shadow cells and calcification surrounded by fibrosis and granulomatous inflammation (Fig 3). Extensive loose, myxoid connective tissue stroma with increased capillaries and scattered, stellate, multinucleated fibrohistiocytic giant cells were also noted (Fig 4). No mitotic figures or aytpical cells were noted. Gram stain found no pathogenic organisms, and tissue cultures were negative for anaerobic, aerobic, and atypical fungal organisms. These findings were consistent with a diagnosis of pilomatricoma with superimposed features of an angiomyxoma. Two days later, the patient underwent a delayed layered closure of the 9-cm × 12-cm defect resulting in a 27-cm linear wound traversing the anterior aspect of the chest. At 1 month, the patient was healing appropriately without complication.
Fig 3.
Routine hematoxylin-eosin stain shows a collection of basaloid cells, central matrical cornification with ghost cells, multinucleated giant cells, fibrosis, and surrounding granulomatous inflammation.
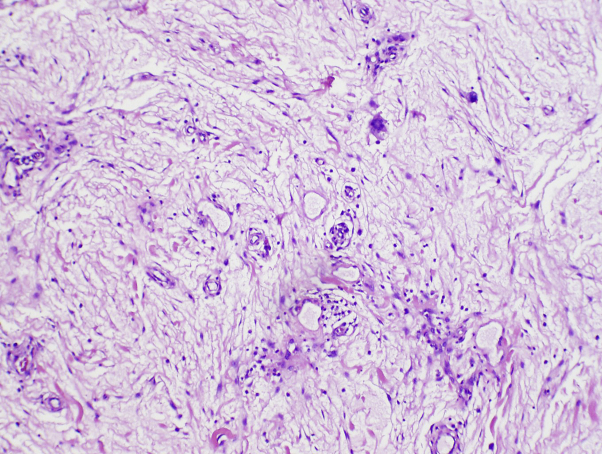
Fig 4.
Routine hematoxylin-eosin stain shows extensive loose, myxoid connective tissue stroma with increased capillaries and scattered, stellate, multinucleated fibrohistiocytic giant cells.
Discussion
Pilomatricomas, or benign calcifying epitheliomas of Malherbe, are the most common hair follicle tumors and typically present either within the first 2 decades of life or after age 60.1 First described in 1880 by Malherbe and Chenatais as sebaceous gland tumors, Forbis and Helwig later clarified that pilomatricomas originate from the hair follicle matrix cells.1, 2, 3 More than half of these tumors are located on the head, neck, or upper torso.1, 4, 5
The clinical presentation of a pilomatricoma is variable, including exophytic, bullous, anetodermic, lymphangiectatic, perforating/ulcerating, multiple, and familial variants.1, 3, 6, 7 Typically, they manifest as tender, solitary, well-circumscribed, flesh-colored or red/blue nodules on the head or neck. Additionally, familial-type and multiple pilomatricomas are associated with a number of known genetic syndromes including myotonic dystrophy, xeroderma pigmentosum, Gardner's syndrome, Turner's syndrome, basal cell nevus syndrome, and Rubinstein-Taybi syndrome.1, 5, 6 Histologically, pilomatricomas are characterized by a cystic lesion containing an admixture of basaloid cells, central matrical cornification with ghost cells (matrical cells with faint nuclei), calcification/ossification (75%), transitional cells, and foreign body–type multinucleated giant cells.4 The presence of mitotic figures and epidermal ulceration are also common features, although malignant transformation (ie, pilomatrical carcinoma) is rare.4, 5
Giant pilomatricomas were first described by Krausen et al8 in 1974. Although no standard definition for giant pilomatricomas exists, these growths are generally defined as tumors larger than 5 cm.1, 4, 7 Giant pilomatricomas are rare and represent a small proportion (<10%) of pilomatricomas.2 Compared with more typical pilomatricomas, these large neoplasms tend to have higher rates of ulceration and secondary infection presumably caused by inadvertent, repeated external trauma.3 To date, approximately 30 giant pilomatricomas have been reported in the scientific literature.6
The pathogenesis of pilomatricomas has not been completely elucidated. However, the Wnt/beta-catenin signaling pathway has been shown to be upregulated in normal matrix cells of the hair follicle.9 Activating mutations in beta-catenin also appear to be fundamental to the development of pilomatricomas and pilomatrical carcinomas.1, 6, 9 Chan et al9 reported that at least 75% of the pilomatricomas they studied harbored beta-catenin–stabilizing activating mutations.9
Al-Brahim and Radhi10 reported 3 cases of superficial angiomyxoma with co-occurring histologic features of a pilomatricoma in the absence of any known familial or other underlying pathology. The first of these cases was an adult male with a 6.7-cm cystic mass on the trunk. The second and third cases were in pediatric patients with 1.5-cm solitary lesions on the trunk and left arm, respectively. None of the patients had a personal or family history of multiple or pigmented lesions. While acknowledging that secondary myxoid changes are often seen in many mesenchymal tumors, Al-Brahim and Radhi10 suggest that pilomatricomas may originate from the epithelial components of angiomyxomas. However, Perez Tato et al11 report a case of a 4-cm truncal mass with histologic findings of a superficial angiomyxoma with trichofolliculoma. Allen et al12 also reviewed the histology of 30 superficial angiomyxomas in 28 patients and reported that less than a third (9 of 30) of these cases contained definitive epithelial components. Finally, Calonje et al13 reviewed the histology of 39 cases of superficial angiomyxomas and reported that only 20% of the primary lesions or their recurrence contained epithelial structure. Neither of the latter publications reported pilomatricoma as an associated finding of superficial angiomyxoma.
We report the case of a follicular neoplasm on the chest of an adolescent patient with histologic features consistent with a giant pilomatricoma with angiomyxoid stroma, although there were insufficient features to make a diagnosis of superficial angiomyxoma per se. Our report, in conjunction with other studies, suggests that an alternate hypothesis to that proposed by Al-Brahim and Radhi10 could be that superficial angiomyxomas or angiomyxoid stroma may represent a secondary finding of preexisting epithelial or hair follicle tumors. Nevertheless, we acknowledge that the association of pilomatricomas with superficial angiomyxomas/angiomyxoid stroma may be purely coincidental and recognize that neither case reports nor retrospective histologic analyses are able to decipher the temporal, etiologic association of these tumors.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Souto M.P., Matsushita Mde M., Matsushita Gde M. An unusual presentation of giant pilomatrixoma in an adult patient. J Dermatol Case Rep. 2013;7:56–59. doi: 10.3315/jdcr.2013.1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zamanian A., Farshchian M., Farshchian M. Clinical and histopathologic study of pilomatricoma in Iran between 1992 and 2005. Pediatr Dermatol. 2008;25:268–269. doi: 10.1111/j.1525-1470.2008.00650.x. [DOI] [PubMed] [Google Scholar]
- 3.Yamauchi M., Yotsuyanagi T., Saito T. Three cases of giant pilomatrixoma–considerations for diagnosis and treatment of giant skin tumours with abundant inner calcification present on the upper body. J Plast Reconstr Aesthet Surg. 2010;63:e519–e524. doi: 10.1016/j.bjps.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Mundinger G.S., Steinbacher D.M., Bishop J.A. Giant pilomatricoma involving the parotid: case report and literature review. J Craniomaxillofac Surg. 2011;39:519–524. doi: 10.1016/j.jcms.2010.03.017. [DOI] [PubMed] [Google Scholar]
- 5.Nadershah M., Alshadwi A., Salama A. Recurrent giant pilomatrixoma of the face: a case report and review of the literature. Case Rep Dent. 2012;2012:197273. doi: 10.1155/2012/197273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Do J.E., Noh S., Jee H.J. Familial multiple pilomatricomas showing clinical features of a giant mass without associated diseases. Int J Dermatol. 2013;52:250–252. doi: 10.1111/j.1365-4632.2010.04867.x. [DOI] [PubMed] [Google Scholar]
- 7.Lozzi G.P., Soyer H.P., Fruehauf J. Giant pilomatricoma. Am J Dermatopathol. 2007;29:286–289. doi: 10.1097/DAD.0b013e318053db45. [DOI] [PubMed] [Google Scholar]
- 8.Krausen A.S., Ansel D.G., Mays B.R., Jr. Pilomatrixoma masquerading as a parotid mass. Laryngoscope. 1974;84:528–535. doi: 10.1288/00005537-197404000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Chan E.F., Gat U., McNiff J.M. A common human skin tumour is caused by activating mutations in beta-catenin. Nat Genet. 1999;21:410–413. doi: 10.1038/7747. [DOI] [PubMed] [Google Scholar]
- 10.Al-Brahim N., Radhi J.M. Cutaneous angiomyxoma and pilomatricoma: a new combination. Ann Diagn Pathol. 2010;14:328–330. doi: 10.1016/j.anndiagpath.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Perez Tato B., Saez A.C., Fernandez P.R. Superficial angiomyxoma with trichofolliculoma. Ann Diagn Pathol. 2008;12:375–377. doi: 10.1016/j.anndiagpath.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Allen P.W., Dymock R.B., MacCormac L.B. Superficial angiomyxomas with and without epithelial components. Report of 30 tumors in 28 patients. Am J Surg Pathol. 1988;12:519–530. doi: 10.1097/00000478-198807000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Calonje E., Guerin D., McCormick D. Superficial angiomyxoma: clinicopathologic analysis of a series of distinctive but poorly recognized cutaneous tumors with tendency for recurrence. Am J Surg Pathol. 1999;23:910–917. doi: 10.1097/00000478-199908000-00008. [DOI] [PubMed] [Google Scholar]