Abstract
Purpose of review
Research on the health of transgender and gender nonconforming people has been limited with most of the work focusing on transition-related care and HIV. This review summarizes research to date on the overall development and quality of life of transgender and gender nonconforming adults, and makes recommendations for future research.
Recent findings
Pervasive stigma and discrimination attached to gender nonconformity affect the health of transgender people across the lifespan, particularly when it comes to mental health and wellbeing. Despite the related challenges, transgender and gender nonconforming people may develop resilience over time. Social support and affirmation of gender identity play herein a critical role. While there is a growing awareness of diversity in gender identity and expression among this population, a comprehensive understanding of biopsychosocial development beyond the gender binary and beyond transition is lacking.
Summary
Greater visibility of transgender people in society has revealed the need to understand and promote their health and quality of life broadly, including but not limited to gender dysphoria and HIV. This means addressing their needs in context of their families and communities, sexual and reproductive health, and successful aging. Research is needed to better understand what factors are associated with resilience and how it can be effectively promoted.
Keywords: Transgender, gender identity, lifespan development, quality of life
Introduction
Public awareness about transgender and gender nonconforming (TGNC) people has recently reached unprecedented heights. The field of transgender health is experiencing a corresponding surge in interest from health providers and policy makers. However, research to inform practice, education, and policy is lagging behind. Examples of TGNC people have been documented across cultures and throughout history. Crossdressing and TGNC identities were first medicalized in the early 20th century, but transgender health did not emerge as a field until the publication of Harry Benjamin’s book The Transsexual Phenomenon (1). That same year, Johns Hopkins University started providing gender-affirming care followed by the University of Minnesota and other medical centers across the United States (2). Research evaluated how well transgender people functioned as members of the other sex after hormone therapy and surgery (3, 4). Unfortunately, 15 years later, most of these university-based clinics had closed, except for the University of Minnesota and the University of Texas Medical Branch.
In the 1980s and 90s, clinical services were primarily provided in private practice and little transgender health research was being conducted in the United States. Coming from a marginalized position, even within the Lesbian, Gay, Bisexual, and Transgender (LGBT) community, TGNC people came together, empowered themselves, and began to redefine their identity and experience both within and outside of the gender binary (5–7). This renewed visibility led to a stronger coalition between the transgender and the LGB communities. A surge in research followed, particularly as public health reports revealed that TGNC people are disproportionately affected by HIV (8–12). LGBT community health centers began to serve transgender people in larger numbers and facilitated community-based research. Findings indicated that TGNC people’s HIV risk had to be understood in light of their overall health affected by social stigma and lack of access to care (13).
In 2011, the NIH commissioned a report from the Institute of Medicine to review the status of LGBT health research, identify gaps and opportunities, and make corresponding recommendations. The review showed that there were more gaps than research, and the IOM recommended NIH implement a broad research agenda in LGBT health and prioritize creation of an evidence-base for transgender care (14). To assist NIH in developing such a research agenda, TransNet, a newly formed U.S. network of transgender health researchers, organized a workshop in May of 2015. This report is from the workshop’s group charged to review research on adult development and quality of life and make recommendations for future research.
Transgender Identity and Gender Dysphoria
TGNC people are a diverse group of individuals whose gender identity differs from their sex assigned at birth (14). Gender dysphoria refers to distress that some TGNC individuals may experience at some point in their lives as a result of incongruence between their gender identity and birth sex, which may include discomfort with gender role and primary and secondary sex characteristics. Gender dysphoria is a diagnosis in the Diagnostic Statistical Manual of Mental Disorders, 5th Edition (15). However, transgender is an identity, not a disorder, and the diagnosis is only applicable when TGNC people experience distress or impaired social / occupational functioning as a result of the incongruence.
Gender dysphoria improves with gender-affirming treatment. Satisfaction with treatment is high (> 80%, regrets < 2%) (16). However, outcome research has primarily followed a binary model of gender, evaluating treatment with hormones, social transition, and surgery, in that order. Gender identity and expression, and gender-affirming interventions have become increasingly diverse. This diversity and the corresponding outcomes have not been systematically evaluated.
Identity Development
Theories of transgender identity development include typologies and stage models. Typologies differentiate TGNC individuals based on age of onset of gender dysphoria (17), degree of crossgender identification (18, 19) or gender role nonconformity (20, 21), and sexual orientation (22, 23). Stage models describe a series of developmental tasks (24–28). For example, Bockting & Coleman (24) distinguish among five stages, acknowledging how stigma attached to gender nonconformity shapes psychosocial identity development (Table 1). Stage models are informed by qualitative research and clinical experience, yet have not been tested empirically. Project AFFIRM, a longitudinal study of transgender identity development across the lifespan (R01HD79603), includes an examination of developmental tasks and stages.
Table 1.
Developmental Stages of Transgender Identity Development
| Stage | Challenges/tasks |
|---|---|
| Pre-coming out | Feeling different; stigma; early resilience or concealment |
| Coming out | Acknowledgment to self and others; taking calculated risks |
| Exploration | Experimentation; stereotyped notions of femininity and masculinity; personal attractiveness and sexual competence; transforming shame into pride |
| Intimacy | Desire for intimacy and first relationships in preferred gender role; facing fear of abandonment; sexual orientation identity |
| Identity integration | Grief; less preoccupation with identity labels; tolerance of gender ambiguity |
Most research on identity development has focused on the period of social and medical transition. Multiple challenges have been documented in qualitative research, with stigma as an overarching theme affecting mental health (e.g., contributing to increased risk for suicide) (29). Clinical research has focused on the role of transition in alleviating gender dysphoria. However, with a few exceptions (30, 31), what has not been studied is how different ways of transitioning affect health, wellbeing, and quality of life. Generational differences in the approach to transition have been observed clinically, but little research to date has examined such differences.
Social Stigma, Minority Stress, and Resilience
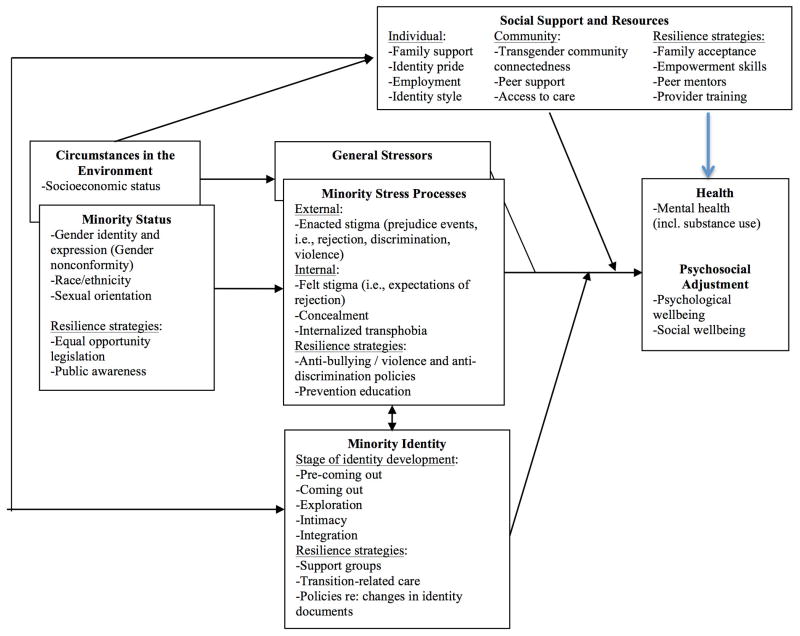
According to the minority stress model (32–34), stigma and prejudice result in added stress beyond general stress also faced by nontransgender people, causing an increase in mental and physical disorders (e.g., depression, anxiety, substance use, hypertension, asthma). Meyer (32) described both distal and proximal minority stress processes. Distal processes are experiences of rejection and discrimination (enacted stigma); proximal processes refer to stress as a result of the internalization of prejudice and stigma. For TGNC people, distal processes include non-affirmation of gender identity (35,36). Proximal processes include internalized transphobia, perceived rejection and expectations of being rejected or discriminated against (felt stigma), and hiding stigmatized status (concealment). Against these stressors, gender minorities forge resilience, coping, social support, and use of other resources (37). The minority stress model describes the impact on health as the net outcome of these negative (stress) and positive (resilience and coping) processes.
TGNC people report verbal harassment, physical abuse, and sexual assault; employment and housing discrimination; and difficulties accessing health and support services (38, 39, 29). A test of the minority stress model with a national sample of the U.S. transgender population showed that discrimination was associated with psychological distress (Bockting et al., 2013). Family support and identity pride were associated with less distress, and support from other transgender people buffered the negative impact of discrimination on mental health. Similarly, in a study of transgender women in NYC, gender-related abuse predicted depression (40, 41), mitigated by community connectedness (35).
Qualitative research has generated other factors of resilience yet to be tested quantitatively, including identity affirmation, awareness of oppression, hope and future outlook, social activism and being a positive role model for others (42). These findings provide support for the minority stress model, yet the mechanisms involved have not been adequately studied. Understanding of such mechanisms is necessary to inform interventions. Project AFFIRM (R01HD79603) is currently testing the development of resilience over time (Fig. 1).
Figure 1.
Adaptation of the minority stress model to transgender health
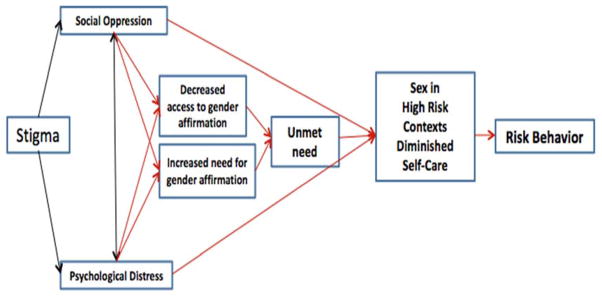
Gender Affirmation
Gender affirmation refers to an interpersonal, interactive process whereby a person receives social recognition and support for gender identity and expression (24, 43, 35). Sevelius (44) proposed a Model of Gender Affirmation to provide a framework for research and interventions focused on sexual risk-taking and self-care among transgender women (Fig. 2). A high need for gender affirmation coupled with low access to gender-affirming procedures results in an unmet need for affirmation, which constitutes identity threat. TGNC people may attempt to reduce identity threat by seeking affirmation in contexts that pose risks and undervalue health-seeking behaviors. Interventions that emphasize self-care motivated by empowerment, gender pride, and understanding gender-based power inequalities, may be successful in building sexual negotiation skills and healthy behaviors supported by a sense of self-worth. An unmet need for gender affirmation predicted risk behavior among HIV negative transgender women and treatment failure among HIV positive women (45). Access to gender affirmation, both social and medical, is related to better mental health (46–48). Gender affirmation within and outside of the gender binary is a promising area for future research.
Figure 2.
Model of Gender Affirmation.
Reproduced with permission from [36] Sevelius, Jae M. “Gender Affirmation: A Framework For Conceptualizing Risk Behavior Among Transgender Women Of Color”. Sex Roles 68, no. 11–12 (2012): 675–689.
Quality of Life
Quality of life includes mental health, wellbeing, physical function, social function, satisfaction, and happiness. Data from probability samples is lacking in virtually all of these domains. Data from community samples indicate high rates of depression (44%) (38), suicidal ideation and attempts (54% and 31%, respectively) (11). Rates of excessive drinking were comparable to those among LGB people (22%), while rates of marijuana (24%) and other drugs (12%) were high (49). Transgender men reported lower quality of life than both female and male norms (Newfield et al., 2006). However, a review of quality of life after hormone therapy and transition indicated that the majority (80%) showed improvement, including more stable relationships, better psychosocial adjustment, overall happiness and contentment (50, 51). Perceived financial, professional, and employment status also improved.
Intersectionality
Identity development and quality of life may be affected by sex, type of TGNC identity, sexual orientation, race/ethnicity, geographical location (52), and socioeconomic status (53). Study samples vary in representation of these characteristics. Transgender women are more often the focus than transgender men; few studies have focused on genderqueer / nonbinary identities (54). In public health research, inner-city transgender women of color are overrepresented because they carry a higher burden in HIV and its social determinants. In clinical samples, transgender women of color are underrepresented, reflecting unequal access to care. There are important differences based on these characteristics that need to be better understood to tailor interventions. For example, rural transgender men reported higher levels of depression and lower levels of self esteem than their urban counterparts (52), and genderqueer individuals reported higher levels of stigma than other TGNC individuals; their rates of depression and anxiety were higher (53% and 39%, respectively) (55–57).
Sexual and Reproductive Health
Sexual orientation
TGNC individuals may be attracted to men, women, and/or other TGNC people. Sexual orientation may affect transgender identity development and vice versa (58). For example, transgender men attracted to women may identify as lesbian before coming out as transgender, while other transgender men or women may not explore their attractions toward men until after transition (59, 24, 60, 61). Vulnerabilities and sexual health needs may differ by sexual orientation (62, 63).
HIV
Research has shown disproportionate prevalence of HIV, AIDS-related mortality, and uncontrolled viral load among transgender women (64, 11). Transgender men who have sex with men reported high rates of sexual risk behavior (62, 63, 65). Few tailored interventions have been tested (66, 67, 68, 8, 13, 69, 70, 71, 72), yet several trials are underway (R01HD057595; R01MH094323; UR6PS000422; R01MH106373, R34MH102109, R34DA038541). There are no transgender-specific guidelines for PrEP, despite evidence suggesting unique barriers to uptake and adherence (45, 73).
HIV-positive transgender women are less likely to receive Anti-Retroviral Treatment (ART) and showed worse adherence than other groups (74, 75). They face complex psychosocial challenges that complicate their access to HIV care, including past negative experiences, giving priority to transition-related care, and concerns about ART and hormone interactions (76, 77). Interventions need to address lack of adherence self-efficacy. Integration of hormonal and HIV care may facilitate adherence and decrease self-administered hormone use (78, 79).
Sexual functioning and satisfaction
Few studies have assessed sexual functioning. In an intervention study (69), TGNC participants reported difficulty getting aroused (38%), low sexual desire (34%), difficulty reaching orgasm alone or with a partner (35% and 28%, respectively); some transgender women attributed their sexual functioning problems to hormone therapy (13%). A review of research on sexual functioning after hormones and surgery, mostly conducted in Europe, found rates of low sexual desire among transgender women comparable to those of nontransgender women, while sexual desire of transgender men increased with hormone therapy and surgery (80).
Reproductive health
In a recent study of transgender men who had delivered a child, 80% used their own eggs, 61% had used testosterone previously, and some pregnancies were unplanned (81). Questions remain about long-term fertility and best practices to preserve (before hormone therapy) or regain (after hormone therapy) fertility in both transgender men and women, and to retain ovaries after hysterectomy for possible future harvesting in transgender men. Questions also remain about the impact of prior testosterone use on a current pregnancy, how long before pregnancy testosterone should be discontinued, and how to counsel a pregnant patient who still has circulating testosterone levels.
Sex work
Sex work is common, particularly among transgender women, attributed to economic hardship, employment discrimination, and lack of health insurance coverage for transgender-specific care (82). HIV prevalence is more than five times as high among transgender compared to nontransgender female sex workers, and substantially higher than among transgender women not engaged in sex work (83). Qualitative research suggests that transgender women may be introduced to sex work by finding community on the street and, initially, as part of their quest to affirm gender identity (66). Research is needed to understand sex work in context of identity development and to test interventions aimed to reduce harm and improve sex work conditions (84).
Relationships, Family, and Community
Few studies have focused on TGNC people’s relationships and family. Of 10,739 articles in scholarly family therapy journals, only 9 focused on transgender issues (0.0008%) (85). Studies are mostly qualitative and samples are small. Some studies conceptualize how parents or spouses deal with a loved one’s transition, depicting loss, grief and cognitive restructuring (86, 87, 88). While family support is a protective factor in coping with minority stress and associated with better quality of life (38, 89, 90), family rejection is as high as 57% and 19% reported family violence (39). Among transgender women of color, family rejection in childhood had lifelong negative sequelae (91).
Research on families with a transgender parent is scarce. An early study by Green (92) showed that children of transgender parents did not differ from children raised in more traditional settings. A few studies examined changes in the parent-child relationship after transition (93, 94, 39, 95, 96); younger age at transition and a positive relationship between parents proved protective (94).
TGNC people’s work life is also largely unexamined. Social stigma may disrupt or delay education and career development, and transgender people worry about the impact of transition on the job. In a U.S. national survey, 38% of transgender adults reported problems getting a job and 23% reported losing a job because of being transgender (38). TGNC people are more likely to be unemployed (33% vs. 12%) and live under the poverty level (31% vs. 9%) (53). Research is needed to better understand the challenges encountered in the workplace and how these can be prevented or overcome.
Incarceration is a public health concern disproportionately affecting transgender women. Among a U.S. sample of 3,878 transgender women, 19% reported incarceration (96). Transgender women of color were 1.8 to 3.3 times more likely to report incarceration than White women. The housing of TGNC people in custody in sex-segregated facilities and their access to care remain contentious. Interventions are needed for transgender women affected by the syndemic of incarceration, HIV, mental illness, and substance use (e.g., R34DA038541).
Brain Development
Research on the brain of TGNC individuals can clarify etiology of gender dysphoria and provide clinically relevant information about the effects of puberty suppression and gender-affirming hormone therapy on the brain. Post mortem studies conducted in the Netherlands (97–100) have linked gender dysphoria to sex differences in the brain. MRI studies using voxel based morphometry, cortical thickness, and diffusion tensor imaging indicate that the transgender man’s brain phenotype consists of a mixture of feminine, masculine and defeminized characteristics, whereas the transgender woman’s phenotype consists of feminine, masculine and demasculinized characteristics (101–108). fMRI studies have focused on sexually dimorphic characteristics, such as mental rotation (109–111), handedness (112), and response to erotic stimuli (113–115). PET studies have addressed hypothalamic responses to putative pheromones acting in a sexually dimorphic manner (Berglund et al, 2008). These studies point toward the existence of distinct phenotypes of the brain for both transgender women and men. More integrative work is necessary to illuminate etiology and understand the effects of hormone therapy on the brain and related health and quality of life indicators.
Opportunities include testing the hypothesis that TGNC people may experience a form of intersexuality of the brain. For example, studies could correlate AR, ER, CYP19, CYP17 and other gene polymorphisms and structural brain data. Another potential area of research concerns the role of body perception and image in the development of gender dysphoria (116–119). MRI cortical structural findings in both transgender women and men have shown initial support for such a role (120, 121). The neural network of body representation appears to differ between transgender and nontransgender individuals (122). For research on etiology, it should be recognized that TGNC people are not a homogeneous group. MRI studies must compare the expression of sex differences in TGNC people of varying sexual orientation and age of onset of gender dysphoria.
While serious short-term complications of gender-affirming hormone therapy appear uncommon (123), the longer-term effects on vulnerability to cardiovascular disease, metabolic disease, and cancer are not well understood (124). Studies that examined the effects of hormones on the brain (125, 126, 121) showed dramatic changes in intracranial volume, cortical thickness, volume of sub-cortical structures, and fractional anisotropy. Transgender women experienced a decrease of gray matter that produces an expansion of the ventricles, while transgender men experienced an increase of intracranial volume, cortical thickness and FA values. These results were interpreted as deep changes in brain metabolism in relation to androgen suppression in transgender women and exogenous testosterone in transgender men (121).
Among nontrangender women, menopausal estrogen therapy has been associated with smaller regional volumes in frontal, temporal and limbic regions as well as the hippocampus (127, 128). Among women aged 65 and older, estrogen therapy was associated with greater brain atrophy (128). In addition, female sex steroids increase the risk of meningioma (129). These data are relevant for aging among TGNC people; the metabolic mechanism that produces changes in the brain of those receiving lifelong hormone therapy needs to be better understood.
Aging and End-of-Life
Transgender people aged 50 and older are at higher risk for poor physical health, disability, depression, and perceived stress (130) compared to their LGB counterparts. These differences are in part due to fear of accessing health services, lack of physical activity, internalized stigma, victimization, and lack of social support. Barriers to care are amplified by the lack of available culturally competent services. In addition, ageism, lack of affordable housing, and lack of family support appear to besiege TGNC older adults (131–136).
It is not uncommon for TGNC individuals to present for transition-related care in mid or later life when social, identity, and biological forces appear to converge and affect the clinical presentation (137). Changes in cortisol secretion and the down regulation of sex steroids and other hormones possibly intensify gender dysphoria (138). The impact of these factors on quality of life of transgender older adults has not been adequately studied.
A review of research on end-of-life care yielded no studies related to TGNC people in hospice or similar situations (139). This despite reports that transgender people fear that their gender identity will not be respected in long-term care and hospice facilities (140). One case report outlined some of the challenges transgender elders and their providers might face (141).
Recommendations for Future Research
Based on the above review and discussions at the May, 2015 NIH workshop on transgender health research, we recommend the following priority areas for future research on adult development and quality of life:
1. Intervention research to reduce stigma and promote resilience
Population studies with probability samples are needed to more accurately determine the prevalence and predictors of health concerns among TGNC people. This will inform research to understand the mechanism of how stigma and minority stress affect health; what constitutes resilience and how it develops over time; and what interventions (individual, family, community, and societal) can effectively promote health across the lifespan.
2. Impact of transition, medical and social, on quality of life
In addition to research on benefits and risks of medical interventions, the impact of transition on quality of life needs to be better understood. This includes mental health and wellbeing, education and employment, housing, social function, satisfaction and happiness.
3. Diversity in gender identity and expression (particularly for nonbinary identities), and ethnic/racial intersectionality
The full spectrum of diversity within this heterogeneous population needs to be further described and accounted for. This includes identifying heightened vulnerability for health concerns among subgroups based on type of transgender identity or race/ethnicity.
4. The role of family, social, and community support (incl. faith community) in quality of life
While social support has repeatedly been shown to serve as a protective factor, the various sources of support need to be better understood to inform interventions. This includes understanding the needs of families and communities.
5. Sexual and reproductive health, dating, relationships, sexual functioning and satisfaction, assisted reproductive technologies, and HIV
Sexual orientation and the impact of stigma on dating and relationships of TCNC people are understudied. Research is needed on sexual functioning and satisfaction, and how it is affected by transition-related care. While an increasing number of TGNC people access reproductive technologies, evidence to guide treatment lags behind. HIV remains a significant concern and research is needed to address transgender-specific risks and barriers to prevention and care. Evidence is lacking to inform appropriate screening for other sexual health concerns (e.g., pelvic and prostate exams).
6. The impact of medical interventions on brain development
Methodological advances are improving our understanding of brain development, providing new opportunities to understand how transgender-specific care affects the brain and related health and quality of life indicators. Moreover, neuroscience can contribute to understanding sexual differentiation of the brain and its implications for health and human development.
7. Successful aging, including end-of-life care
A life course perspective should examine TGNC people’s quality of life across the lifespan while accounting for diversity in gender identity and expression (i.e., including nonbinary identities). We recommend a biospsychosocial approach, examining the impact of life course events, experiences, and interventions (e.g., hormone therapy) on the dimensions of successful aging (physical and mental health, social engagement and wellbeing).
Acknowledgments
Financial support and sponsorship
This work was supported in part by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health (R13HD084267), the Endocrine Society, the Tawani Foundation, the World Professional Association for Transgender Health (WPATH), and the Program in Human Sexuality at the University of Minnesota Medical School. The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health, the Endocrine Society, or WPATH. Dr. Guillamon’s research was supported by grant PSI2014-58004-P from the Spanish Government.
Contributor Information
Walter Bockting, .
Eli Coleman,
Madeline B. Deutsch,
Antonio Guillamon,
Ilan Meyer,
Walter Meyer, III,
Sari Reisner,
Jae Sevelius,
Randi Ettner,
References
- 1.Benjamin H, Lal G, Green R, Masters R. The transsexual phenomenon. New York, N.Y: Ace Pub. Co; 1966. [Google Scholar]
- 2.Hastings . Inauguration of a research project on transsexualism in a university medical center. In: Green R, Money J, editors. Transsexualism and sex reassignment. 1. Baltimore: The Johns Hopkins Press; 1969. pp. 243–251. [Google Scholar]
- 3.Hasting D. Postsurgical adjustment of male transsexual patients. Clinics In Plastic Surgery. 1974;1(2):335–344. [PubMed] [Google Scholar]
- 4.Hastings D, Markland C. Post-surgical adjustment of twenty-five transsexuals (male-to-female) in the university of Minnesota study. Arch Sex Behav. 1978;7(4):327–336. doi: 10.1007/BF01542041. http://dx.doi.org/10.1007/bf01542041. [DOI] [PubMed] [Google Scholar]
- 5.Feinberg L. Transgender warriors. Boston: Beacon Press; 1996. [Google Scholar]
- 6.Bornstein K, Bornstein K. Gender outlaw. New York: Routledge; 1994. [Google Scholar]
- 7.Stone S. The empire strikes back: A posttransexual manifesto. In: Epstein, Straub K, editors. Body guards: The cultural politics of gender ambiguity. 1. New York: Routledge; 1991. pp. 280–604. [Google Scholar]
- 8.Hook M. In: Transgender and HIV: Risks, Prevention, and Care. Bockting Walter, Kirk Sheila., editors. Binghampton, NY: The Haworth Press; 2001. [Google Scholar]
- 9.Bockting WO, Avery E. Transgender health and HIV prevention. Binghamton, NY: The Haworth Press; 2005. [Google Scholar]
- 10.Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: Implications for public health intervention. American journal of public health. 2001 Jun;91(6):915. doi: 10.2105/ajph.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herbst J, Jacobs E, Finlayson T, McKleroy V, Neumann M, Crepaz N. Estimating HIV Prevalence and Risk Behaviors of Transgender Persons in the United States: A Systematic Review. AIDS Behav. 2007;12(1):1–17. doi: 10.1007/s10461-007-9299-3. http://dx.doi.org/10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- 12.Nemoto T, Operario D, Keatley J, Han L, Soma T. HIV Risk Behaviors Among Male-to-Female Transgender Persons of Color in San Francisco. Am J Public Health. 2004;94(7):1193–1199. doi: 10.2105/ajph.94.7.1193. http://dx.doi.org/10.2105/ajph.94.7.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bockting W, Huang C, Ding H, Robinson B, Rosser B. Are Transgender Persons at Higher Risk for HIV Than Other Sexual Minorities? A Comparison of HIV Prevalence and Risks. International Journal Of Transgenderism. 2005;8(2–3):123–131. http://dx.doi.org/10.1300/j485v08n02_11. [Google Scholar]
- 14.Institute of Medicine. The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. 2001. [PubMed] [Google Scholar]
- 15.Association A. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5®) Washington, D.C: American Psychiatric Publishing; 2013. [Google Scholar]
- 16.Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, Fraser L, et al. Standards Of Care For The Health Of Transsexual, Transgender, And Gender-Nonconforming People, Version 7. International Journal of Transgenderism. 2012;13(4):165–232. [Google Scholar]
- 17.Person E, Ovesey L. The transsexual syndrome in males: II. Secondary transsexualism. American journal of psychotherapy. 1974 Apr; doi: 10.1176/appi.psychotherapy.1974.28.2.174. [DOI] [PubMed] [Google Scholar]
- 18.Buhrich Neil, McConaghy Neil. Clinical Comparison Of Transvestism And Transsexualism. Aust NZ J Psychiatry. 1977;11(2):83–86. doi: 10.3109/00048677709159542. [DOI] [PubMed] [Google Scholar]
- 19.Buhrich Neil, McConaghy Neil. Three Clinically Discrete Categories Of Fetishistic Transvestism. Arch Sex Behav. 1979;8(2):151–157. doi: 10.1007/BF01541235. [DOI] [PubMed] [Google Scholar]
- 20.Bockting Walter. Transgender Identity Development. In: Tolman DL, Diamonded L, editors. American Psychological Association’S Handbook Of Sexuality And Psychology. 1. Washington D.C: American Psychological Association; 2013. [Google Scholar]
- 21.Bockting Walter. The Impact Of Stigma On Transgender Identity Development And Mental Health. In: Kreukels BPC, Steensma TD, De Vriesed LC, editors. Gender Dysphoria And Disorders Of Sex Development: Progress In Care And Knowledge. 1. New York: Springer; 2014. pp. 319–330. [Google Scholar]
- 22.Blanchard Ray. Typology Of Male-To-Female Transsexualism. Arch Sex Behav. 1985;14(3):247–261. doi: 10.1007/BF01542107. [DOI] [PubMed] [Google Scholar]
- 23.Blanchard R. The classification and labeling of nonhomosexual gender dysphorias. Archives of sexual behavior. 1989 Aug 1;18(4):315–34. doi: 10.1007/BF01541951. [DOI] [PubMed] [Google Scholar]
- 24.Bockting Walter, Coleman E. Developmental Stages Of The Transgender Coming Out Process: Toward An Integrated Identity. In: Ettner R, Monstrey S, Eylered E, editors. Principles Of Transgender Medicine And Surgery. 1. New York: The Haworth Press; 2007. pp. 185–208. [Google Scholar]
- 25.Devor Aaron. Witnessing And Mirroring: A Fourteen Stage Model Of Transsexual Identity Formation. WGLM. 2004;8(1):41–67. [Google Scholar]
- 26.Gagne p, Tewksbury r, Mcgaughey d. Coming Out and Crossing Over: Identity Formation And Proclamation In A Transgender Community. Gender & Society. 1997;11(4):478–508. [Google Scholar]
- 27.Lev Arlene Istar. Transgender Emergence. New York: The Haworth Clinical Practice Press; 2004. [Google Scholar]
- 28.Lewins Frank W. Transsexualism In Society. South Melbourne: Macmillan Education Australia; 1995. [Google Scholar]
- 29.Reisner Sari L, Greytak Emily A, Parsons Jeffrey T, Ybarra Michele L. Gender Minority Social Stress In Adolescence: Disparities In Adolescent Bullying And Substance Use By Gender Identity. The Journal of Sex Research. 2014;52(3):243–256. doi: 10.1080/00224499.2014.886321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lawrence AA. Factors Associated With Satisfaction Or Regret Following Male-To-Female Sex Reassignment Surgery. Archives of Sexual Behavior. 2003;32(4):299–315. doi: 10.1023/a:1024086814364. [DOI] [PubMed] [Google Scholar]
- 31.Newfield Emily, Hart Stacey, Dibble Suzanne, Kohler Lori. Female-To-Male Transgender Quality Of Life. Qual Life Res. 2006;15(9):1447–1457. doi: 10.1007/s11136-006-0002-3. [DOI] [PubMed] [Google Scholar]
- 32.Hendricks Michael L, Testa Rylan J. A Conceptual Framework For Clinical Work With Transgender And Gender Nonconforming Clients: An Adaptation Of The Minority Stress Model. Professional Psychology: Research and Practice. 2012;43(5):460–467. [Google Scholar]
- 33.Meyer Ilan H. Prejudice, Social Stress, And Mental Health In Lesbian, Gay, And Bisexual Populations: Conceptual Issues And Research Evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frost David M, Lehavot Keren, Meyer Ilan H. Minority Stress And Physical Health Among Sexual Minority Individuals. J Behav Med. 2013;38(1):1–8. doi: 10.1007/s10865-013-9523-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nuttbrock Larry A, Bockting Walter O, Hwahng Sel, Rosenblum Andrew, Mason Mona, Macri Monica, Becker Jeffrey. Gender Identity Affirmation Among Male-To-Female Transgender Persons: A Life Course Analysis Across Types Of Relationships And Cultural/Lifestyle Factors. Sexual and Relationship Therapy. 2009;24(2):108–125. [Google Scholar]
- 36.Sevelius Jae M. Gender Affirmation: A Framework For Conceptualizing Risk Behavior Among Transgender Women Of Color. Sex Roles. 2012;68(11–12):675–689. doi: 10.1007/s11199-012-0216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pflum Samantha R, Testa Rylan J, Balsam Kimberly F, Goldblum Peter B, Bongar Bruce. Social Support, Trans Community Connectedness, And Mental Health Symptoms Among Transgender And Gender Nonconforming Adults. Psychology of Sexual Orientation and Gender Diversity. 2015;2(3):281–286. [Google Scholar]
- 38.Bockting Walter O, Miner Michael H, Romine Rebecca E Swinburne, Hamilton Autumn, Coleman Eli. Stigma, Mental Health, And Resilience In An Online Sample Of The US Transgender Population. Am J Public Health. 2013;103(5):943–951. doi: 10.2105/AJPH.2013.301241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grant J, Mottet L, Tanis J. Injustice At Every Turn: A Report Of The National Transgender Discrimination Survey. Washington D.C: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2011. [Google Scholar]
- 40.Nuttbrock Larry, Hwahng Sel, Bockting Walter, Rosenblum Andrew, Mason Mona, Macri Monica, Becker Jeffrey. Psychiatric Impact Of Gender-Related Abuse Across The Life Course Of Male-To-Female Transgender Persons. Journal of Sex Research. 2010;47(1):12–23. doi: 10.1080/00224490903062258. [DOI] [PubMed] [Google Scholar]
- 41.Nuttbrock Larry, Bockting Walter, Rosenblum Andrew, Hwahng Sel, Mason Mona, Macri Monica, Becker Jeffrey. Gender Abuse, Depressive Symptoms, And HIV And Other Sexually Transmitted Infections Among Male-To-Female Transgender Persons: A Three-Year Prospective Study. Am J Public Health. 2013;103(2):300–307. doi: 10.2105/AJPH.2011.300568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Singh Anneliese A, Hays Danica G, Watson Laurel S. Strength In The Face Of Adversity: Resilience Strategies Of Transgender Individuals. Journal of Counseling & Development. 2011;89(1):20–27. [Google Scholar]
- 43.Melendez Rita M, Pinto Rogério. ’It’s Really A Hard Life’: Love, Gender And HIV Risk Among Male-To-Female Transgender Persons. Culture, Health & Sexuality. 2007;9(3):233–245. doi: 10.1080/13691050601065909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sevelius JM. Gender affirmation: A framework for conceptualizing risk behavior among transgender women of color. Sex roles. 2013 Jun 1;68(11–12):675–89. doi: 10.1007/s11199-012-0216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Deutsch Madeline B, Glidden David V, Sevelius Jae, Keatley Joanne, McMahan Vanessa, Guanira Juan, Kallas Esper G, Chariyalertsak Suwat, Grant Robert M. HIV Pre-Exposure Prophylaxis In Transgender Women: A Subgroup Analysis Of The Iprex Trial. The Lancet HIV. 2015;2(12):e512–e519. doi: 10.1016/S2352-3018(15)00206-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ainsworth Tiffiny A, Spiegel Jeffrey H. Quality Of Life Of Individuals With And Without Facial Feminization Surgery Or Gender Reassignment Surgery. Qual Life Res. 2010;19(7):1019–1024. doi: 10.1007/s11136-010-9668-7. [DOI] [PubMed] [Google Scholar]
- 47.Colton Meier Stacey L, Fitzgerald Kara M, Pardo Seth T, Babcock Julia. The Effects Of Hormonal Gender Affirmation Treatment On Mental Health In Female-To-Male Transsexuals. Journal of Gay & Lesbian Mental Health. 2011;15(3):281–299. [Google Scholar]
- 48.Nuttbrock L, Rosenblum A, Blumenstein R. Transgender Identity Affirmation And Mental Health. International Journal of Transgenderism. 2002;6(4):97–03. [Google Scholar]
- 49.Gonzalez C, Bockting WO. Predictors Of Substance Use Among An Online Sample Of The U.S. Transgender Population. n.d [Google Scholar]
- 50.Murad Mohammad Hassan, Elamin Mohamed B, Garcia Magaly Zumaeta, Mullan Rebecca J, Murad Ayman, Erwin Patricia J, Montori Victor M. Hormonal Therapy And Sex Reassignment: A Systematic Review And Meta-Analysis Of Quality Of Life And Psychosocial Outcomes. Clinical Endocrinology. 2010;72(2):214–231. doi: 10.1111/j.1365-2265.2009.03625.x. [DOI] [PubMed] [Google Scholar]
- 51.Zubiaurre-Elorza L, Junque C, Gomez-Gil E, Segovia S, Carrillo B, Rametti G, Guillamon A. Cortical Thickness In Untreated Transsexuals. Cerebral Cortex. 2012;23(12):2855–2862. doi: 10.1093/cercor/bhs267. [DOI] [PubMed] [Google Scholar]
- 52.Horvath Keith J, Iantaffi Alex, Swinburne-Romine Rebecca, Bockting Walter. A Comparison Of Mental Health, Substance Use, And Sexual Risk Behaviors Between Rural And Non-Rural Transgender Persons. Journal of Homosexuality. 2014;61(8):1117–1130. doi: 10.1080/00918369.2014.872502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Conron Kerith J, Scott Gunner, Stowell Grace Sterling, Landers Stewart J. Transgender Health In Massachusetts: Results From A Household Probability Sample Of Adults. Am J Public Health. 2012;102(1):118–122. doi: 10.2105/AJPH.2011.300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Diamond LD, Pardo ST, Butterworth MR. Transgender Experience And Identity. In: Schwartzed SJ, editor. Handbook Of Identity Theory And Research. 1. New York: Springer; 2011. pp. 629–647. [Google Scholar]
- 55.Budge Stephanie L, Kinton Rossman H, Howard Kimberly AS. Coping And Psychological Distress Among Genderqueer Individuals: The Moderating Effect Of Social Support. Journal of LGBT Issues in Counseling. 2014;8(1):95–117. [Google Scholar]
- 56.Factor Rhonda, Rothblum Esther. Exploring Gender Identity And Community Among Three Groups Of Transgender Individuals In The United States: Mtfs, Ftms, And Genderqueers. Health Sociology Review. 2008;17(3):235–253. [Google Scholar]
- 57.Harrison J, Grant J, Herman JL. A Gender Not Listed Here: Genderqueers, Gender Rebels, And Otherwise In The National Transgender Discrimination Survey. LGBTQ Public Policy Journal at the Harvard Kennedy School. 2012;2(1) [Google Scholar]
- 58.Iantaffi Alex, Bockting Walter O. Views From Both Sides Of The Bridge? Gender, Sexual Legitimacy And Transgender People’s Experiences Of Relationships. Culture, Health & Sexuality. 2011;13(3):355–370. doi: 10.1080/13691058.2010.537770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Auer Matthias K, Fuss Johannes, Höhne Nina, Stalla Günter K, Sievers Caroline. Transgender Transitioning And Change Of Self-Reported Sexual Orientation. PLoS ONE. 2014;9(10):e110016. doi: 10.1371/journal.pone.0110016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kuper Laura E, Nussbaum Robin, Mustanski Brian. Exploring The Diversity Of Gender And Sexual Orientation Identities In An Online Sample Of Transgender Individuals. Journal of Sex Research. 2012;49(2–3):244–254. doi: 10.1080/00224499.2011.596954. [DOI] [PubMed] [Google Scholar]
- 61.Rowniak Stefan, Chesla Catherine. Coming Out For A Third Time: Transmen, Sexual Orientation, And Identity. Arch Sex Behav. 2012;42(3):449–461. doi: 10.1007/s10508-012-0036-2. [DOI] [PubMed] [Google Scholar]
- 62.Feldman Jamie, Romine Rebecca Swinburne, Bockting Walter O. HIV Risk Behaviors In The U.S. Transgender Population: Prevalence And Predictors In A Large Internet Sample. Journal of Homosexuality. 2014;61(11):1558–1588. doi: 10.1080/00918369.2014.944048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Reisner SL, White Hughto JM, Pardee D, Sevelius J. Syndemics And Gender Affirmation: HIV Sexual Risk In Female-To-Male Trans Masculine Adults Reporting Sexual Contact With Cisgender Males. International Journal of STD & AIDS. 2015 doi: 10.1177/0956462415602418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Baral Stefan D, Poteat Tonia, Strömdahl Susanne, Wirtz Andrea L, Guadamuz Thomas E, Beyrer Chris. Worldwide Burden Of HIV In Transgender Women: A Systematic Review And Meta-Analysis. The Lancet Infectious Diseases. 2013;13(3):214–222. doi: 10.1016/S1473-3099(12)70315-8. [DOI] [PubMed] [Google Scholar]
- 65.Sevelius Jae. There’s No Pamphlet For The Kind Of Sex I Have”: HIV-Related Risk Factors And Protective Behaviors Among Transgender Men Who Have Sex With Nontransgender Men. Journal of the Association of Nurses in AIDS Care. 2009;20(5):398–410. doi: 10.1016/j.jana.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bockting WO, Robinson BE, Rosser BRS. Transgender HIV Prevention: A Qualitative Needs Assessment. AIDS Care. 1998;10(4):505–525. doi: 10.1080/09540129850124028. [DOI] [PubMed] [Google Scholar]
- 67.Bockting WO, Rosser BS, Scheltema K. Transgender HIV prevention: Implementation and evaluation of a workshop. Health Education Research. 1999 Apr 1;14(2):177–83. doi: 10.1093/her/14.2.177. [DOI] [PubMed] [Google Scholar]
- 68.Bockting WO, Rosser BS, Coleman E. Clinical Update: Transgender HIV Prevention: A Model Education Workshop. Journal of the Gay and Lesbian Medical Association. 2000 Dec 1;4(4):175–83. [Google Scholar]
- 69.Bockting WO, Robinson BE, Forberg J, Scheltema K. Evaluation Of A Sexual Health Approach To Reducing HIV/STD Risk In The Transgender Community. AIDS Care. 2005;17(3):289–303. doi: 10.1080/09540120412331299825. [DOI] [PubMed] [Google Scholar]
- 70.Garofalo Robert, Johnson Amy K, Kuhns Lisa M, Cotten Christopher, Joseph Heather, Margolis Andrew. Life Skills: Evaluation Of A Theory-Driven Behavioral HIV Prevention Intervention For Young Transgender Women. Journal of Urban Health. 2012;89(3):419–431. doi: 10.1007/s11524-011-9638-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nemoto Tooru, Operario Don, Keatley JoAnne, Nguyen Hongmai, Sugano Eiko. Promoting Health For Transgender Women: Transgender Resources And Neighborhood Space (TRANS) Program In San Francisco. Am J Public Health. 2005;95(3):382–384. doi: 10.2105/AJPH.2004.040501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Taylor Raekiela D, Bimbi David S, Joseph Heather A, Margolis Andrew D, Parsons Jeffrey T. Girlfriends: Evaluation Of An HIV-Risk Reduction Intervention For Adult Transgender Women. AIDS Education and Prevention. 2011;23(5):469–478. doi: 10.1521/aeap.2011.23.5.469. [DOI] [PubMed] [Google Scholar]
- 73.Remien Robert H, Bauman Laurie J, Mantell Joanne E, Tsoi Benjamin, Lopez-Rios Javier, Chhabra Rosy, DiCarlo Abby, et al. Barriers And Facilitators To Engagement Of Vulnerable Populations In HIV Primary Care In New York City. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2015;69:S16–S24. doi: 10.1097/QAI.0000000000000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Melendez Rita M, Exner Theresa A, Ehrhardt Anke A, Dodge Brian, Remien Robert H, Rotheram-Borus Mary-Jane, Lightfoot Marguerita, Hong Daniel. Health And Health Care Among Male-To-Female Transgender Persons Who Are HIV Positive. Am J Public Health. 2006;96(6):1034–1037. doi: 10.2105/AJPH.2004.042010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sevelius Jae M, Carrico Adam, Johnson Mallory O. Antiretroviral Therapy Adherence Among Transgender Women Living With HIV. Journal of the Association of Nurses in AIDS Care. 2010;21(3):256–264. doi: 10.1016/j.jana.2010.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sevelius Jae M, Patouhas Enzo, Keatley JoAnne G, Johnson Mallory O. Barriers And Facilitators To Engagement And Retention In Care Among Transgender Women Living With Human Immunodeficiency Virus. Annals of Behavioral Medicine. 2013;47(1):5–16. doi: 10.1007/s12160-013-9565-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vázquez Enid. A Transgender Therapy Primer. [Accessed October 15, 2015];Positively Aware. 2015 http://www.positivelyaware.com/archives/2008/08_04/transgender_therapy_primer.html.
- 78.Grimaldi J, Jacobs J. The HIV Hormone Bridge: Connecting Impoverished HIV+ Transsexual Sex Workers To HIV Medical Care. International Conference On AIDS. 1998 [Google Scholar]
- 79.Zevin B, Martinez L. HIV Infection And Transgender Medicine. [Accessed November 15, 2015];HIV In Site. Last modified 2007. http://HIVInfectionandTransgenderMedicine.
- 80.Klein Carolin, Gorzalka Boris B. Sexual Functioning In Transsexuals Following Hormone Therapy And Genital Surgery: A Review (CME) Journal of Sexual Medicine. 2009;6(11):2922–2939. doi: 10.1111/j.1743-6109.2009.01370.x. [DOI] [PubMed] [Google Scholar]
- 81.Light Alexis D, Obedin-Maliver Juno, Sevelius Jae M, Kerns Jennifer L. Transgender Men Who Experienced Pregnancy After Female-To-Male Gender Transitioning. Obstetrics & Gynecology. 2014;124(6):1120–1127. doi: 10.1097/AOG.0000000000000540. [DOI] [PubMed] [Google Scholar]
- 82.Nadal Kevin L, Davidoff Kristin C, Fujii-Doe Whitney. Transgender Women And The Sex Work Industry: Roots In Systemic, Institutional, And Interpersonal Discrimination. Journal of Trauma & Dissociation. 2014;15(2):169–183. doi: 10.1080/15299732.2014.867572. [DOI] [PubMed] [Google Scholar]
- 83.Operario Don, Soma Toho, Underhill Kristen. Sex Work And HIV Status Among Transgender Women. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2008;48(1):97–103. doi: 10.1097/QAI.0b013e31816e3971. [DOI] [PubMed] [Google Scholar]
- 84.Poteat Tonia, Wirtz Andrea L, Radix Anita, Borquez Annick, Silva-Santisteban Alfonso, Deutsch Madeline B, Khan Sharful Islam, Winter Sam, Operario Don. HIV Risk And Preventive Interventions In Transgender Women Sex Workers. The Lancet. 2015;385(9964):274–286. doi: 10.1016/S0140-6736(14)60833-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Blumer Markie LC, Green Mary S, Knowles Sarah J, Williams April. Shedding Light On Thirteen Years Of Darkness: Content Analysis Of Articles Pertaining To Transgender Issues In Marriage/Couple And Family Therapy Journals. Journal of Marital and Family Therapy. 2012;38:244–256. doi: 10.1111/j.1752-0606.2012.00317.x. [DOI] [PubMed] [Google Scholar]
- 86.Norwood Kristen. Transitioning Meanings? Family Members’ Communicative Struggles Surrounding Transgender Identity. Journal of Family Communication. 2012;12(1):75–92. [Google Scholar]
- 87.Pearlman Sarah F. Terms Of Connection. Journal of GLBT Family Studies. 2006;2(3–4):93–122. [Google Scholar]
- 88.Joslin-Roher Emily, Wheeler Darrell P. Partners In Transition: The Transition Experience Of Lesbian, Bisexual, And Queer Identified Partners Of Transgender Men. Journal of Gay & Lesbian Social Services. 2009;21(1):30–48. [Google Scholar]
- 89.Budge Stephanie L, Adelson Jill L, Howard Kimberly AS. Anxiety And Depression In Transgender Individuals: The Roles Of Transition Status, Loss, Social Support, And Coping. Journal of Consulting and Clinical Psychology. 2013;81(3):545–557. doi: 10.1037/a0031774. [DOI] [PubMed] [Google Scholar]
- 90.Esteva de Antonio Isabel, Gómez-Gil Esther. ”Coordination Of Healthcare For Transsexual Persons. Current Opinion in Endocrinology & Diabetes and Obesity. 2013;20(6):585–591. doi: 10.1097/01.med.0000436182.42966.31. [DOI] [PubMed] [Google Scholar]
- 91.Koken JA, Bimbi DS, Parsons JT. Experiences of familial acceptance–rejection among transwomen of color. Journal of Family Psychology. 2009 Dec;23(6):853. doi: 10.1037/a0017198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Green R. Sexual identity of 37 children raised by homosexual or transsexual parents. The American Journal of Psychiatry. 1978 Jun; doi: 10.1176/ajp.135.6.692. [DOI] [PubMed] [Google Scholar]
- 93.White Tonya, Ettner Randi. Disclosure, Risks And Protective Factors For Children Whose Parents Are Undergoing A Gender Transition. WGLM. 2004;8(1):129–145. [Google Scholar]
- 94.White Tonya, Ettner Randi. Adaptation And Adjustment In Children Of Transsexual Parents. European Child & Adolescent Psychiatry. 2006;16(4):215–221. doi: 10.1007/s00787-006-0591-y. [DOI] [PubMed] [Google Scholar]
- 95.Church HA, O’Shea D, Lucey JV. Parent–Child Relationships In Gender Identity Disorder. Irish Journal of Medical Science. 2013;183(2):277–281. doi: 10.1007/s11845-013-1003-1. [DOI] [PubMed] [Google Scholar]
- 96.Reisner Sari L, Bailey Zinzi, Sevelius Jae. Racial/Ethnic Disparities In History Of Incarceration, Experiences Of Victimization, And Associated Health Indicators Among Transgender Women In The U.S. Women & Health. 2014;54(8):750–767. doi: 10.1080/03630242.2014.932891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhou Jiang-Ning, Hofman Michel A, Gooren Louis JG, Swaab Dick F. A Sex Difference In The Human Brain And Its Relation To Transsexuality. Nature. 1995;378(6552):68–70. doi: 10.1038/378068a0. [DOI] [PubMed] [Google Scholar]
- 98.Kruijver FPM. Male-To-Female Transsexuals Have Female Neuron Numbers In A Limbic Nucleus. Journal of Clinical Endocrinology & Metabolism. 2000;85(5):2034–2041. doi: 10.1210/jcem.85.5.6564. [DOI] [PubMed] [Google Scholar]
- 99.Garcia-Falgueras A, Swaab DF. A Sex Difference In The Hypothalamic Uncinate Nucleus: Relationship To Gender Identity. Brain. 2008;131(12):3132–3146. doi: 10.1093/brain/awn276. [DOI] [PubMed] [Google Scholar]
- 100.Taziaux Melanie, Swaab Dick F, Bakker Julie. Sex Differences In The Neurokinin B System In The Human Infundibular Nucleus. The Journal of Clinical Endocrinology & Metabolism. 2012;97(12):E2210–E2220. doi: 10.1210/jc.2012-1554. [DOI] [PubMed] [Google Scholar]
- 101.Luders Eileen, Sánchez Francisco J, Gaser Christian, Toga Arthur W, Narr Katherine L, Hamilton Liberty S, Vilain Eric. Regional Gray Matter Variation In Male-To-Female Transsexualism. NeuroImage. 2009;46(4):904–907. doi: 10.1016/j.neuroimage.2009.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Luders Eileen, Sánchez Francisco J, Tosun Duygu, Shattuck David W, Gaser Christian, Vilain Eric, Toga Arthur W. Increased Cortical Thickness In Male-To-Female Transsexualism. Journal of Behavioral and Brain Science. 2012;02(03):357–362. doi: 10.4236/jbbs.2012.23040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Savic I, Arver S. Sex Dimorphism Of The Brain In Male-To-Female Transsexuals. Cerebral Cortex. 2011;21(11):2525–2533. doi: 10.1093/cercor/bhr032. [DOI] [PubMed] [Google Scholar]
- 104.Rametti Giuseppina, Carrillo Beatriz, Gómez-Gil Esther, Junque Carme, Segovia Santiago, Gomez Ángel, Guillamon Antonio. White Matter Microstructure In Female To Male Transsexuals Before Cross-Sex Hormonal Treatment. A Diffusion Tensor Imaging Study. Journal of Psychiatric Research. 2011;45(2):199–204. doi: 10.1016/j.jpsychires.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 105.Rametti Giuseppina, Carrillo Beatriz, Gómez-Gil Esther, Junque Carme, Zubiarre-Elorza Leire, Segovia Santiago, Gomez Ángel, Guillamon Antonio. The Microstructure Of White Matter In Male To Female Transsexuals Before Cross-Sex Hormonal Treatment. A DTI Study. Journal of Psychiatric Research. 2011;45(7):949–954. doi: 10.1016/j.jpsychires.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 106.Zubiaurre-Elorza Leire, Junque Carme, Gómez-Gil Esther, Guillamon Antonio. Effects Of Cross-Sex Hormone Treatment On Cortical Thickness In Transsexual Individuals. The Journal of Sexual Medicine. 2014;11(5):1248–1261. doi: 10.1111/jsm.12491. [DOI] [PubMed] [Google Scholar]
- 107.Simon Lajos, Kozák Lajos R, Simon Viktória, Czobor Pál, Unoka Zsolt, Szabó Ádám, Csukly Gábor. Regional Grey Matter Structure Differences Between Transsexuals And Healthy Controls—A Voxel Based Morphometry Study. PLoS ONE. 2013;8(12):e83947. doi: 10.1371/journal.pone.0083947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kranz GS, Hahn A, Kaufmann U, Kublbock M, Hummer A, Ganger S, Seiger R, et al. White Matter Microstructure In Transsexuals And Controls Investigated By Diffusion Tensor Imaging. Journal of Neuroscience. 2014;34(46):15466–15475. doi: 10.1523/JNEUROSCI.2488-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sommer IEC, Cohen-Kettenis PT, van Raalten T, vd Veer AJ, Ramsey LE, Gooren LJG, Kahn RS, Ramsey NF. Effects Of Cross-Sex Hormones On Cerebral Activation During Language And Mental Rotation: An Fmri Study In Transsexuals. European Neuropsychopharmacology. 2008;18(3):215–221. doi: 10.1016/j.euroneuro.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 110.Carrillo Beatriz, Gómez-Gil Esther, Rametti Giuseppina, Junque Carme, Gomez Ángel, Karadi Kazmer, Segovia Santiago, Guillamon Antonio. Cortical Activation During Mental Rotation In Male-To-Female And Female-To-Male Transsexuals Under Hormonal Treatment. Psychoneuroendocrinology. 2010;35(8):1213–1222. doi: 10.1016/j.psyneuen.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 111.Schöning Sonja, Engelien Almut, Bauer Christine, Kugel Harald, Kersting Anette, Roestel Cornelia, Zwitserlood Pienie, et al. Neuroimaging Differences In Spatial Cognition Between Men And Male-To-Female Transsexuals Before And During Hormone Therapy. Journal of Sexual Medicine. 2009;7(5):1858–1867. doi: 10.1111/j.1743-6109.2009.01484.x. [DOI] [PubMed] [Google Scholar]
- 112.Wisniewski Amy B, Prendeville Mary T, Dobs Adrian S. Handedness, Functional Cerebral Hemispheric Lateralization, And Cognition In Male-To-Female Transsexuals Receiving Cross-Sex Hormone Treatment. Arch Sex Behav. 2005;34(2):167–172. doi: 10.1007/s10508-005-1794-x. [DOI] [PubMed] [Google Scholar]
- 113.Gizewski Elke R, Krause Eva, Schlamann Marc, Happich Friederike, Ladd Mark E, Forsting Michael, Senf Wolfgang. Specific Cerebral Activation Due To Visual Erotic Stimuli In Male-To-Female Transsexuals Compared With Male And Female Controls: An Fmri Study. Journal of Sexual Medicine. 2009;6(2):440–448. doi: 10.1111/j.1743-6109.2008.00981.x. [DOI] [PubMed] [Google Scholar]
- 114.Oh Seok-Kyun, Kim Gwang-Won, Yang Jong-Chul, Kim Seok-Kwun, Kang Heoung-Keun, Jeong Gwang-Woo. Brain Activation In Response To Visually Evoked Sexual Arousal In Male-To-Female Transsexuals: 3.0 Tesla Functional Magnetic Resonance Imaging. Korean J Radiol. 2012;13(3):257. doi: 10.3348/kjr.2012.13.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kim Gwang-Won, Jeong Gwang-Woo. Neural Mechanisms Underlying Sexual Arousal In Connection With Sexual Hormone Levels. NeuroReport. 2014;25(9):699–706. doi: 10.1097/WNR.0000000000000159. [DOI] [PubMed] [Google Scholar]
- 116.First Michael B. Desire For Amputation Of A Limb: Paraphilia, Psychosis, Or A New Type Of Identity Disorder. Psychological Medicine. 1999;35(6):919–928. doi: 10.1017/s0033291704003320. [DOI] [PubMed] [Google Scholar]
- 117.Ramachandran VS, McGeoch Paul D. Occurrence Of Phantom Genitalia After Gender Reassignment Surgery. Medical Hypotheses. 2007;69(5):1001–1003. doi: 10.1016/j.mehy.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 118.Fisher Alessandra D, Castellini Giovanni, Bandini Elisa, Casale Helen, Fanni Egidia, Benni Laura, Ferruccio Naika, et al. Cross-Sex Hormonal Treatment And Body Uneasiness In Individuals With Gender Dysphoria. The Journal of Sexual Medicine. 2013;11(3):709–719. doi: 10.1111/jsm.12413. [DOI] [PubMed] [Google Scholar]
- 119.Becker Inga, Nieder Timo O, Cerwenka Susanne, Briken Peer, Kreukels Baudewijntje PC, Cohen-Kettenis Peggy T, Cuypere GrietDe, Hebold Haraldsen Ira R, Richter-Appelt Hertha. Body Image In Young Gender Dysphoric Adults: A European Multi-Center Study. Arch Sex Behav. 2015 doi: 10.1007/s10508-015-0527-z. [DOI] [PubMed] [Google Scholar]
- 120.Savic I, Arver S. Sex Dimorphism Of The Brain In Male-To-Female Transsexuals. Cerebral Cortex. 2011;21(11):2525–2533. doi: 10.1093/cercor/bhr032. [DOI] [PubMed] [Google Scholar]
- 121.Zubiaurre-Elorza Leire, Junque Carme, Gómez-Gil Esther, Guillamon Antonio. Effects Of Cross-Sex Hormone Treatment On Cortical Thickness In Transsexual Individuals. The Journal of Sexual Medicine. 2014;11(5):1248–1261. doi: 10.1111/jsm.12491. [DOI] [PubMed] [Google Scholar]
- 122.Lin Chia-Shu, Ku Hsiao-Lun, Chao Hsiang-Tai, Tu Pei-Chi, Li Cheng-Ta, Cheng Chou-Ming, Su Tung-Ping, Lee Ying-Chiao, Hsieh Jen-Chuen. Neural Network Of Body Representation Differs Between Transsexuals And Cissexuals. PLoS ONE. 2014;9(1):e85914. doi: 10.1371/journal.pone.0085914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wierckx Katrien, Van Caenegem Eva, Schreiner Thomas, Haraldsen Ira, Fisher Alessandra, Toye Kaatje, Kaufman Jean Marc, T’Sjoen Guy. Cross-Sex Hormone Therapy In Trans Persons Is Safe And Effective At Short-Time Follow-Up: Results From The European Network For The Investigation Of Gender Incongruence. The Journal of Sexual Medicine. 2014 doi: 10.1111/jsm.12571. n/a–n/a. [DOI] [PubMed] [Google Scholar]
- 124.Gooren Louis J. Care Of Transsexual Persons. New England Journal of Medicine. 2011;364(13):1251–1257. doi: 10.1056/NEJMcp1008161. [DOI] [PubMed] [Google Scholar]
- 125.Pol HEH, Cohen-Kettenis PT, Van Haren NEM, Peper JS, Brans RGH, Cahn W, Schnack HG, Gooren LJG, Kahn RS. Changing Your Sex Changes Your Brain: Influences Of Testosterone And Estrogen On Adult Human Brain Structure. European Journal of Endocrinology. 2006;155(suppl_1):S107–S114. [Google Scholar]
- 126.Rametti Giuseppina, Carrillo Beatriz, Gómez-Gil Esther, Junque Carme, Zubiaurre-Elorza Leire, Segovia Santiago, Gomez Ángel, Karadi Kazmer, Guillamon Antonio. Effects Of Androgenization On The White Matter Microstructure Of Female-To-Male Transsexuals. A Diffusion Tensor Imaging Study. Psychoneuroendocrinology. 2012;37(8):1261–1269. doi: 10.1016/j.psyneuen.2011.12.019. [DOI] [PubMed] [Google Scholar]
- 127.Casanova Ramon, Espeland Mark A, Goveas Joseph S, Davatzikos Christos, Gaussoin Sarah A, Maldjian Joseph A, Brunner Robert L, et al. Application Of Machine Learning Methods To Describe The Effects Of Conjugated Equine Estrogens Therapy On Region-Specific Brain Volumes. Magnetic Resonance Imaging. 2011;29(4):546–553. doi: 10.1016/j.mri.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Resnick SM, Espeland MA, Jaramillo SA, Hirsch C, Stefanick ML, Murray AM, Ockene J, Davatzikos C. Postmenopausal Hormone Therapy And Regional Brain Volumes: The WHIMS-MRI Study. Neurology. 2009;72(2):135–142. doi: 10.1212/01.wnl.0000339037.76336.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wigertz A. Risk Of Brain Tumors Associated With Exposure To Exogenous Female Sex Hormones. American Journal of Epidemiology. 2006;164(7):629–636. doi: 10.1093/aje/kwj254. [DOI] [PubMed] [Google Scholar]
- 130.Fredriksen-Goldsen KI, Cook-Daniels L, Kim HJ, Erosheva EA, Emlet CA, Hoy-Ellis CP, Goldsen J, Muraco A. Physical And Mental Health Of Transgender Older Adults: An At-Risk And Underserved Population. The Gerontologist. 2013;54(3):488–500. doi: 10.1093/geront/gnt021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Witten Tarynn M, Evan Eyler A. Hate Crimes And Violence Against The Transgendered. Peace Review. 1999;11(3):461–468. [Google Scholar]
- 132.Cahill Sean, South Ken. Policy Issues Affecting Lesbian, Gay, Bisexual, And Transgender People In Retirement. San Francisco, Calif: Generations; 2002. [Google Scholar]
- 133.Cook-Daniels Loree. Lesbian, Gay Male, Bisexual And Transgendered Elders: Elder Abuse And Neglect Issues. Journal of Elder Abuse & Neglect. 1998;9(2):35–49. [Google Scholar]
- 134.Witten Tarynn M. Life Course Analysis—The Courage To Search For Something More. Journal of Human Behavior in the Social Environment. 2003;8(2–3):189–224. [Google Scholar]
- 135.Witten TM, Eyler AE. Transgender Aging And The Care Of The Elderly Transgendered Patient. In: Ettner R, Monstrey S, Eylered AE, editors. Principles Of Transgender Medicine And Surgery. 1. New York: The Haworth Press; 2007. pp. 343–372. [Google Scholar]
- 136.Kimmel Douglas. Lesbian, Gay, Bisexual, And Transgender Aging Concerns. Clinical Gerontologist. 2013;37(1):49–63. [Google Scholar]
- 137.Ettner Randi, Wylie Kevan. Psychological And Social Adjustment In Older Transsexual People. Maturitas. 2013;74(3):226–229. doi: 10.1016/j.maturitas.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 138.Ettner Randi. Care Of The Elderly Transgender Patient. Current Opinion in Endocrinology & Diabetes and Obesity. 2013;20(6):580–584. doi: 10.1097/01.med.0000436183.34931.a5. [DOI] [PubMed] [Google Scholar]
- 139.Harding Richard, Epiphaniou Eleni, Chidgey-Clark Jayne. Needs, Experiences, And Preferences Of Sexual Minorities For End-Of-Life Care And Palliative Care: A Systematic Review. Journal of Palliative Medicine. 2012;15(5):602–611. doi: 10.1089/jpm.2011.0279. [DOI] [PubMed] [Google Scholar]
- 140.Witten TM, Eyler AE. Transgender Aging And The Care Of The Elderly Transgendered Patient. In: Ettner R, Monstrey S, Eylered AE, editors. Principles Of Transgender Medicine And Surgery. 1. New York: The Haworth Press; 2007. pp. 343–372. [Google Scholar]
- 141.Marshall Alexandra, Yarber William L, Sherwood-Laughlin Catherine M, Gray Mary L, Estell David B. Coping And Survival Skills: The Role School Personnel Play Regarding Support For Bullied Sexual Minority-Oriented Youth. J School Health. 2015;85(5):334–340. doi: 10.1111/josh.12254. [DOI] [PubMed] [Google Scholar]