Abstract
Objectives
To describe (1) cardiac rehabilitation (CR) referral across cardiac units in a tertiary centre with eReferral; (2) characteristics associated with CR referral and enrolment and (3) the effects of peer navigation (PN) on referral and enrolment. This pilot was a 2 parallel-arm, randomised, single-blind trial with allocation concealment.
Setting
3 cardiac units (ie, interventional, general cardiology, and cardiac surgery) in 1 of 2 hospitals of a tertiary centre.
Participants
CR-eligible adult cardiac inpatients were randomised to PN or usual care. 94 (54.7%) patients consented, of which 46 (48.9%) were randomised to PN. Outcomes were ascertained in 76 (80.9%) participants.
Intervention
The PN (1) visited participant at the bedside, (2) mailed a card to participant's home reminding about CR and (3) called participant 2 weeks postdischarge to discuss CR barriers.
Outcome measures
The primary outcome of enrolment was defined as participant attendance at a scheduled CR intake appointment (yes/no). The secondary outcome was referral. Blinded outcome assessment was conducted 12 weeks postdischarge, via CR chart extraction.
Results
Those who received care on the cardiac surgery unit (77.9%) were more likely to be referred than those treated on the general cardiology (61.1%) or interventional unit (33.3%; p=0.04). Patients who had cardiac surgery, hypertension and hyperlipidaemia were significantly more likely, and those with congenital heart disease, cancer and a previous cardiac diagnosis were less likely to be referred. Participants referred to a site closer to home (76.2% of those referred) were more likely to enrol than those not (23.7%, p<0.05). PN had no effect on referral (77.6%, p=0.45) or enrolment (46.0%, p=0.24).
Conclusions
There is wide variability in CR referral, even within academic centres, and despite eReferral. Referral was quite high, and thus, PN did not improve CR utilisation. Results support triaging patients to the CR programme closest to their home.
Trial registration number
NCT02204449; Results.
Keywords: Physical and Rehabilitation Medicine, Health Services Research, Referral, Patient Navigation
Strengths and limitations of this study.
This is one of the few studies to investigate intrainstitutional variability in cardiac rehabilitation (CR) referral practices by ward, and to investigate the effects of patient referral triage to the cardiac rehabilitation programme closest to home on their subsequent enrolment.
The design of this study is a strength: This was a randomised controlled trial, with allocation concealment, and blinded outcome assessment.
With regard to limitations, first, a comparison group exposed to traditional cardiac rehabilitation referral approaches was not included in the design, therefore, it is unknown whether the CR referral and enrolment rates observed herein are truly higher than what would be observed without eReferral.
Second, the relatively low response rate suggests there may be some selection bias.
Third, the primary outcomes were ascertained via self-report for those re-referred closer to home, but via chart report for those who attended the within-institution CR programme.
Cardiovascular disease is among the leading causes of morbidity globally.1 With advances in acute treatment, patients are surviving their events, but remain at high risk of recurrence and subsequent mortality. Cardiac rehabilitation (CR) is an outpatient secondary prevention programme composed of structured exercise training, comprehensive education, and counselling, which has been shown to reduce recurrence and increase survival.2
Despite its proven benefits, CR remains grossly underused.3 4 Multifactorial barriers to both CR referral by providers and enrolment among eligible patients have been established.5 In their systematic review, Clark et al6 reported the key issues at the health system level included insufficient time and workload capacity to make the referral, and at the provider level included overreliance on physicians as gatekeepers, and judgements that patients were not likely to participate. In another systematic review by this group,7 lack of patient knowledge regarding CR services was associated with lower enrolment rates. Finally, in their systematic review, Cortés and Arthur5 found cardiac indication, older age, being a non-English speaker, being a woman, being unmarried, and being non-white were all associated with lower referral rates.
Emphatic calls to promote greater CR utilisation have been sounded by learned societies.8 9 Systematic CR referral has been demonstrated to significantly increase referral, and discussion with patients about CR at the bedside prior to discharge have been shown to increase their subsequent enrolment.10 11 Accordingly, targets of 85% inpatient CR referral and 70% enrolment have been established.12 Systematic referral strategies have the ancillary benefit of mitigating bias in patient referral.13
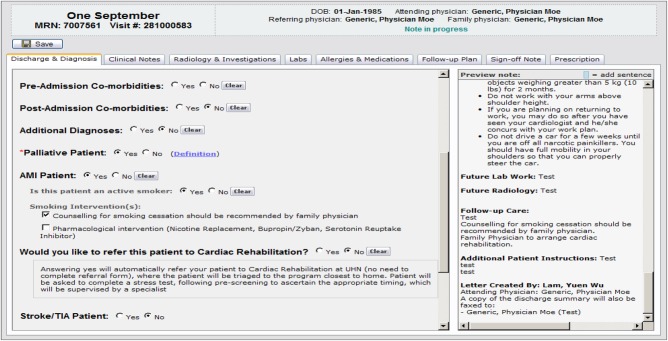
There is variability in institutional approaches to referral and patient communication regarding CR.14 To minimise costs associated with the referral process, our institution recently established electronic CR referral (eReferral), such that referral to CR appears as an option in the electronic discharge summary for all indicated cardiac patients (figure 1). To assess the potential added effect of patient education regarding CR at the bedside, in accordance with a recent successful trial of peer navigation,15 16 our institution recently expanded and augmented a peer-visiting programme for patients of coronary artery bypass graft surgery to all wards treating patients indicated for CR.
Figure 1.
eReferral screenshot from electronic discharge summary.
Peer navigation (also referred to as patient navigation) is a patient-centric intervention designed to eliminate barriers to timely healthcare.17 It is a one-on-one relationship between navigators, usually a trained layperson, and patients, in which the navigator provides education about the healthcare process and support.18 It has been implemented and tested in a variety of healthcare populations,19–21 including cardiac.15 16 Prior reviews of peer navigation interventions provide evidence that it may reduce health system barriers,22–26 such as those experienced by patients eligible for CR. Indeed, it has been recommended as an approach to overcoming barriers to CR use.27 28
Accordingly, the objectives of the current study were to: (1) describe CR referral rates across cardiac units in a tertiary cardiac centre with eReferral; (2) describe patient sociodemographic and clinical characteristics associated with referral and enrolment in such a centre and (3) describe the effects of peer navigation on CR referral and enrolment. It was hypothesised that eReferral would achieve high absolute rates of referral across both peer navigation and usual care groups, and that peer navigation would achieve significantly higher rates of enrolment among referred patients than usual care.
Method
Design and procedure
A pilot randomised controlled trial entitled ‘Cardiac Rehabilitation PEer navigation to promote Enrolment and Referral’ was undertaken to test the feasibility of a peer navigation intervention (independent variable) in increasing cardiac patients' referral to and enrolment in CR (dependent variables). This trial design was pragmatic,29 two parallel-arm, randomised (1:1), allocation-concealed and single-blind. A power calculation was deemed inappropriate as this was a pilot study.30 The protocol was reviewed and approved by the University Health Network Research Ethics Board and also the Committee on Research Involving Human Subjects at Stony Brook University.
On obtaining written informed consent, clinical data were extracted from inpatient charts to confirm CR eligibility. Included participants were then randomised to either receive the peer navigation intervention (see below) or usual care (eReferral, see below). The randomisation sequence was generated by a statistician unaffiliated with the study, and was stratified by sex in random blocks of 4, 8 and 12. Random assignment was concealed through the use of opaque envelopes.
CR enrolment and referral were the primary and secondary outcome measures, respectively. These outcomes were ascertained by a research assistant (LJ) blinded to random assignment 12 weeks postdischarge through extraction from the CR chart.
Setting
Participants were recruited from three cardiac units (ie, interventional cardiology, general cardiology and cardiac surgery) in one of two hospitals of an Academic Health Sciences Centre (University Health Network) in Toronto, Canada, between July and December 2014. CR is offered to patients at no charge in Ontario, as it is reimbursed by the provincial government health insurance (ie, single payer).
The eReferral system was instituted as part of usual care in June 2014. As shown in figure 1, when healthcare providers (ie, nurse-practitioners, hospitalists, cardiologists or cardiac specialists depending on the cardiac unit) are completing the electronic discharge summary for patients with a cardiac diagnosis or procedure indicated for CR, they must click ‘yes’ or ‘no’ whether they wish to refer the patient to CR. Therefore, eReferral is available on all the cardiology units. Where ‘yes’ is selected, the electronic discharge summary is copied into a queue which is managed by the CR staff. The CR staff then reviews the discharge summaries, and triages the patients accordingly.
As a tertiary cardiac care centre, non-local patients are frequently treated. Inpatient staff were instructed to refer all patients to the CR programme within the institution, regardless of their location of residence (see text in figure 1). This served to mitigate referral failure due to lack of inpatient staff awareness of CR programme locations proximate to patients' homes. Thereafter, CR programme staff reviewed the addresses of all referred patients, so that non-local patient referrals could be redirected to a programme closer to their place of residence (where available). On discussion with patients, referral information was faxed to the programme closer to their home.
Participants
Participants were adult cardiac inpatients eligible for CR, with one or more of the following CR-indicated diagnoses or procedures: acute coronary syndrome, percutaneous coronary intervention, coronary artery bypass graft surgery±valve surgery, arrhythmia, stable heart failure, congenital heart disease and/or non-disabling stroke. In addition, participants had to be proficient in English. Patients were excluded if: (1) they had any major musculoskeletal, neuromuscular, visual, cognitive or non-dysphoric psychiatric condition, or any serious or terminal illness not otherwise specified which would preclude CR eligibility based on CR guidelines as outlined by the Canadian Association of Cardiovascular Prevention and Rehabilitation,31 (2) they were being discharged to long-term care, (3) were unable to ambulate (ie, walk unaided at 2 mph, and hence, undergo a pre-CR exercise stress test) and/or (4) did not reside in Ontario where CR services are reimbursed.
Intervention
The peer navigation intervention was based on the approach previously tested in the USA by Benz Scott et al,15 16 with modifications to accommodate the local healthcare context. As the University Health Network hospitals had an eReferral system in place as part of usual care, the primary focus of the current intervention was to increase CR enrolment.
The intervention was delivered by two female CR peer navigators, who were University Health Network CR graduates and formal volunteers at the participating hospital. The navigators completed training with University Health Network Volunteer Services, and were trained by the study team to deliver CR-focused education and support. Training included review of scripts for all points of contact with participants.
The intervention consisted of three points of contact between participants and peer navigators. First, participants were visited at the bedside by the CR peer navigator to build rapport, provide written materials about the benefits of CR, and encourage the participant to obtain a CR referral from their healthcare provider before discharge from the hospital. The second point of contact occurred 1 week postdischarge, when a ‘get well soon’ card was mailed by the CR navigator to the participant's home, including the phone number of the University Health Network CR centre. For those not referred, the card included a message encouraging the participant to secure a referral from any of their physicians. The third and final point of contact occurred 2 weeks after discharge; the CR navigator called the participant to discuss any barriers to CR enrolment. Each point of contact was documented on a piloted form to establish consistency and fidelity.
Measures
Participant sociodemographic and clinical characteristics were extracted from participants' medical charts. These included age, sex, admission and discharge dates, cardiovascular diagnoses/procedures, risk factors, comorbidities, previous cardiac diagnoses, and contact information. The independent variable was study arm (ie, intervention vs usual care).
The primary outcome of enrolment was defined as participant attendance at a scheduled CR intake appointment (ie, risk factor assessment, exercise stress-testing, goal-setting; yes/no). This was ascertained through blind review of CR charts for local participants referred to the institution's CR programme. For participants referred to a programme closer to their home (re-referral), enrolment was ascertained via self-report through a phone call, again by a research assistant blind to random assignment.
The secondary outcome of referral (yes/no) was confirmed by reviewing the list of those received at the University Health Network's programme. Referral was defined as CR programme receipt of documentation from a healthcare provider to refer the participant dated during or subsequent to the index participant admission, whether it was a formal referral form, eReferral or a discharge summary from the hospital stay. Where no referral was found at the local University Health Network programme, participants were called to ascertain whether they had been referred to or enrolled in any other CR programmes, again by a research assistant blind to random assignment. Re-referral was evident by a fax cover sheet attached to the referral form, addressed to another CR programme.
Statistical analyses
First, the equivalence of participant sociodemographic and clinical characteristics by trial arm were tested using χ2 or t tests, as appropriate. To test the first objective, CR referral was described by cardiac ward.
To test the second objective, CR referral and enrolment (yes/no) were compared by participant sociodemographic and clinical characteristics using Fisher's exact tests or t tests, as applicable. To test the final objective, Fisher's exact tests were used to compare CR referral and enrolment by trial arm. IBM SPSSV.20 was used for all analyses.
Results
Respondent characteristics
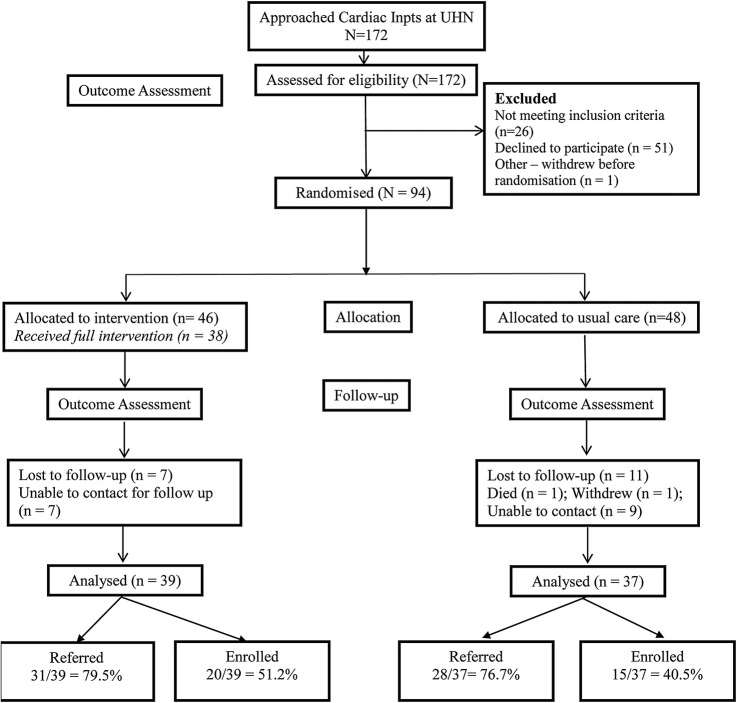
A diagram of patient flow is shown in figure 2. One hundred and seventy-two patients were approached, of whom 26 (15.1%) were ineligible for the following reasons: 15 (8.7%) were not proficient in English, 9 (5.2%) either did not live in Ontario or were leaving the province after discharge from hospital, and 2 (1.2%) had a medical condition which rendered them ineligible for CR. Overall, 94 patients consented and were randomised (1 patient consented but withdrew before randomisation), resulting in a study enrolment rate of 54.7%. One patient withdrew consent after randomisation, and 1 patient died prior to outcome assessment, resulting in a final sample of N=92.
Figure 2.
Participant recruitment flow diagram.
Table 1 displays participant sociodemographic and clinical characteristics. As shown, there were no significant differences in these characteristics by trial arm.
Table 1.
Sociodemographic and clinical characteristics by trial arm
| Characteristic | Intervention n=46 (48.9%) | Usual care n=48 (51.1%) | Total N=94 |
|---|---|---|---|
| Sociodemographic | |||
| Age (mean±SD) | 62.6±13.1 | 62.7±16.5 | 62.7±14.8 |
| Female sex | 14 (30.4) | 15 (31.3) | 30 (31.9) |
| Non-white | 8 (17.4) | 8 (17.0) | 16 (17.0) |
| Clinical | |||
| Cardiac rehabilitation indication (% yes)* | |||
| Valve surgery | 19 (41.3) | 22 (45.8) | 41 (43.6) |
| Coronary artery bypass graft surgery | 19 (41.3) | 16 (33.3) | 35 (37.2) |
| Arrhythmia or rhythm device | 16 (34.8) | 11 (22.9) | 27 (28.7) |
| Acute coronary syndrome | 10 (21.7) | 14 (29.1) | 24 (25.5) |
| Percutaneous coronary intervention | 9 (19.6) | 9 (18.8) | 18 (19.1) |
| Other (heart failure, congenital heart disease, non-disabling stroke) | 3 (6.5) | 7 (14.5) | 10 (10.6) |
| Risk factors (% yes) | |||
| Hyperlipidaemia | 29 (63.0) | 24 (50.0) | 58 (61.7) |
| Hypertension | 28 (60.9) | 25 (52.1) | 53 (56.4) |
| Diabetes | 7 (15.2) | 14 (29.1) | 21 (22.3) |
| Smoking | 4 (8.7) | 10 (29.2) | 14 (14.9) |
| Previous history of cardiac disease (% yes) | 42 (91.3) | 38 (79.2) | 80 (85.1) |
| Comorbidities (% yes) | |||
| Arthritis | 7 (15.2) | 4 (8.3) | 11 (11.7) |
| Cancer | 3 (6.5) | 6 (12.5) | 9 (9.6) |
| Length of stay (mean days±SD) | 9.3±4.6 | 10.8±9.4 | 10.0±7.4 |
| Discharged on weekend | 9 (19.6) | 8 (17.0) | 17 (18.1) |
*Indications are not mutually exclusive (eg, bypass surgery patients had concomitant valve repair).
As shown in figure 2, CR referral was ascertained for 84 (91.3%) participants and enrolment for 76 (82.6%) participants. There was no referral form received at University Health Network CR for eight (16.7%) participants randomised to usual care, who could not subsequently be reached by phone to confirm they were not referred to another programme. Nine (9.8%) participants could not be reached by phone to confirm enrolment.
There was no difference in whether outcomes were ascertained by randomised arm (p=0.25). With regard to sociodemographic and clinical characteristics, participants for whom outcomes were ascertained were not significantly different than participants for whom outcomes were not ascertained (data not shown).
CR referral and enrolment
Overall, 59 (77.6%) of the 76 study participants were referred (66/92 assuming no referral in those for whom outcomes were not ascertained; 71.7%), of which 45 (76.3%) were re-referred to a CR site closer to their home. Physicians were as likely to refer participants regardless of whether the CR programme ultimately re-referred them to a site closer to their home or not (p=0.29).
Overall, 35 (46.1%) of the 76 participants enrolled (or 35/92 assuming no enrolment in those for whom outcomes were not ascertained, 38.0%), with 30 (66.7%) of those re-referred to a site closer to home enrolling. Of the 59 referred, 59.3% enrolled. As shown in table 2, participants re-referred to a CR programme closer to their home were significantly more likely to enrol than those who were not (p=0.04).
Table 2.
Participant characteristics by cardiac rehabilitation referral and enrolment
| Referred (N=92) |
Enrolled (N=76) |
|||
|---|---|---|---|---|
| Characteristic | Yes n=66 (78.6%) | No n=26 (28.3%) | Yes n=35 (46.0%) | No n=41 (53.9%) |
| Sociodemographic | ||||
| Age (mean±SD) | 63.1±13.8 | 61.0±17.2 | 61.5±14.0 | 62.9±16.0 |
| Female sex | 21 (31.8) | 7 (26.9) | 12 (34.3) | 10 (24.4) |
| Non-white | 13 (19.7) | 4 (15.4) | 8 (22.9) | 6 (14.6) |
| Clinical | ||||
| Cardiac rehabilitation indication (% yes) | ||||
| Valve surgery | 29 (43.9) | 10 (38.5) | 18 (51.4) | 16 (39.0) |
| Coronary artery bypass graft surgery | 29 (43.9) | 6 (23.1) | 14 (40) | 14 (34.1) |
| Arrhythmia or rhythm Device | 18 (27.2) | 9 (34.6) | 10 (28.8) | 9 (22.0) |
| Acute coronary syndrome | 20 (30.3) | 4 (15.4) | 8 (22.9) | 11 (26.8) |
| Percutaneous coronary intervention | 14 (21.2) | 4 (15.4) | 7 (20.0) | 8 (19.5) |
| Heart failure | 2 (3.0) | 5 (19.2)* | 2 (5.7) | 3 (7.3) |
| Risk factors (% yes) | ||||
| Hypertension | 40 (60.6) | 12 (46.2) | 21 (60) | 22 (53.7) |
| Hyperlipidaemia | 41 (62.1) | 11 (42.3) | 21 (60.0) | 25 (61.0) |
| Smoking (% current) | 12 (18.2) | 2 (7.7) | 5 (14.3) | 6 (14.6) |
| Diabetes | 17 (25.8) | 4 (15.4) | 7 (20.0) | 11 (26.8) |
| Previous history of cardiac disease (% yes) | 56 (84.8) | 23 (88.5) | 30 (85.7) | 36 (87.8) |
| Comorbidities | ||||
| Arthritis | 9 (13.6) | 2 (7.7) | 5 (14.3) | 4 (9.8) |
| Cancer | 3 (4.5) | 5 (19.2)* | 2 (5.7) | 5 (12.2) |
| Length of stay (mean days±SD) | 9.2±4.7 | 11.3±10.9** | 9.4±4.4 | 8.2±4.8 |
| Discharged on weekend | 12 (18.2) | 6 (23.1) | 9 (25.7) | 6 (14.6) |
| Referred to site closer to home | – | – | 30 (85.7)* | 15 (36.6) |
*p<0.05, **p<0.01.
With regard to objective 1, there were significant differences in CR referral depending on the cardiology unit from which a participant was discharged (p=0.04). Participants who received inpatient care on the cardiac surgery unit (77.9%) were more likely to be referred than those treated on the general cardiology (61.1%) or the interventional cardiology unit (33.3%).
With regard to the second objective, sociodemographic and clinical characteristics associated with CR referral are shown in table 2. As displayed, there were no differences in the sociodemographic characteristics of those referred versus not referred, but differences were observed based on clinical characteristics. With regard to cardiac indication for CR, participants with heart failure were less often referred (p=0.02). With regard to comorbidities, participants with cancer were significantly less likely to be referred than those without (p<0.05). Finally, those who were referred to CR had a shorter length of stay in the hospital than those not referred (p<0.01).
Sociodemographic and clinical characteristics associated with CR enrolment are also shown in table 2. As displayed, there were no significant differences in these characteristics among those who enrolled versus those who did not.
Effects of peer navigation on CR utilisation
Intervention fidelity
Of the 46 participants randomised to the navigation intervention, 38 (82.6%) received all three contacts. One (2.2%) participant did not receive the bedside visit and 7 (15.2%) participants did not receive the postdischarge phone call. In addition, 4 (8.7%) participants did not receive their initial bedside contact prior to hospital discharge, but instead, the content was delivered via a telephone call to the participant at their home within 3 days of discharge.
Among the sample for whom outcomes were ascertained (n=76), CR referral did not significantly differ between the navigated group (n=31, 79.5%) and usual care (n=28, 75.7%; p=0.45). Enrolment also did not significantly differ between groups (n=20, 51.3% in the peer navigation arm; n=15, 40.5% for usual care, p=0.27).
If we assume no referral or enrolment among those for whom there was no referral form at University Health Network, yet they could not be reached by phone (n=92), referral still did not significantly differ between the navigated group (n=37, 80.4%) and usual care (n=29, 63.0%; p=0.05). Enrolment also did not significantly differ between groups in this larger sample (n=20, 51.3% in the peer navigation arm; n=15, 40.5% for usual care, p=0.24).
Discussion
There is wide variability in CR referral practices even within academic institutions by cardiac wards, which could be due to cultural norms, healthcare provider practice variation, or the severity of illness (eg, surgical patients vs non-invasive procedures). Despite institution of an eReferral strategy across the academic institution, patients on the surgery unit were more likely to be referred than those on other units, and this finding is consistent with previous studies.32 33 Indeed, there was a 40% difference in the proportion of patients referred by unit in the same institution. The eReferral strategy did, however, appear to mitigate sociodemographic biases oft-observed in CR referral,5 and patient referral was consistent on weekends as well as weekdays. Moreover, this is one of the first studies, to the best of our knowledge, to document higher rates of CR enrolment where patients are triaged to CR sites closer to their home.
Prior studies have demonstrated that systematic referral strategies can decrease referral bias.13 Although a larger sample than reported here is required to be conclusive, there did not appear to be age, sex or ethnocultural biases in referral or enrolment patterns. This is a positive sign and suggests that eReferral has potential to mitigate bias in physician decisions related to these non-clinical characteristics.
However, there were differences in the clinical characteristics of patients referred. Patients with heart failure were less likely to be referred than those without, although this finding should be interpreted with caution due to the low number of participants with this indication in the sample. This is disconcerting, given the established benefits of CR for heart failure patients,34 and that Canadian CR guidelines promote heart failure as an indication for CR.31 Moreover, heart failure is now a reimbursed indication for CR in the USA,35 36 and in Ontario where this study was undertaken, there are recommendations for CR referral for heart failure patients.37 Greater awareness of the evidence of benefit and these policy changes may be needed before we see changes in referral practice.
Second, patients with comorbid cancer were less often referred than those without. This may be appropriate, depending on the stage of cancer and therapy. Finally, patients who had a shorter length of inpatient hospital stay were more likely to be referred than those with a longer stay. This is somewhat surprising given that patients on the bypass unit, which traditionally has longer lengths of stay, were more often referred than angioplasty patients, who have a shorter stay. Patients with a longer length of stay may have complications, more comorbidities, or more severe or complex disease, which would preclude participation in CR.
Owing to the high rate of inpatient referral observed in over three-quarters of patients, the addition of peer navigation did not have a significant impact on patient enrolment as hypothesised, although firm conclusions cannot be drawn as this was a pilot study. A larger sample may be needed to observe differences in enrolment by peer navigation exposure, particularly in the context of eReferral. Thus, the first hypothesis in this pilot was confirmed, but the second was disconfirmed. Potential explanations for the lack of replication of findings from the peer navigation trial by Benz Scott et al15 include the eReferral strategy implemented at the institution as outlined previously. In the trial conducted in the USA, there was no referral strategy in the usual care arm. In the intervention arm, the peer navigators facilitated contact between the patient and the CR centre. Based on the results of this pilot, the decision has been made not to proceed to a full-scale trial.
Implications
There are three key policy implications of these findings. First, re-referring patients to programmes closer to home should be a ‘best practice’ for cardiac care, as it may improve patient enrolment rates. There may be financial disincentive to re-refer where CR programmes are reimbursed based on patient volumes. However, there are so many patients who do not access CR, that programmes should always have sufficient patients to ensure financial soundness. Second, system-wide CR referral strategies, such as eReferral, should be broadly instituted as a means of ensuring high CR referral rates.
Third and finally, on a related note, given the variation in CR referral between wards despite eReferral, education of healthcare providers will still be required to ensure consistent CR referral practices. There is a need to provide repeated education/in-services to cardiac healthcare providers, feedback on the proportion of patients referred in relation to targets, and reminders about the benefits of CR participation for patients, and recommendations to refer patients in clinical practice guidelines, particularly on interventional cardiology units. If the high rates of CR referral observed on cardiac surgery units could be replicated across all cardiac units, we would be much closer to achieving the 85% target.12
Strengths and limitations
The current study is one of the few to investigate both intrainstitutional variability in CR referral practices by ward, and the effects of referral triage to the CR programme closest to home on subsequent patient enrolment. Therefore, a strength of this research is its' novel contribution to the literature. A second strength is the use of a randomised controlled design, as well as allocation concealment, with blinded outcome assessment.
Nonetheless, caution is warranted in interpreting these results. First, a comparison group exposed to traditional CR referral approaches was not included in the design, therefore, it is unknown whether the CR referral and enrolment rates observed herein are truly higher than what would be observed without eReferral. Second, the relatively low response rate (54.7%) suggests there may be some selection bias. Third, the primary outcomes were ascertained via self-report for those re-referred closer to home but via chart report for those who attended the within-institution CR programme. This may have biased findings. Fourth, the study was conducted at a single institution (albeit with two hospitals), which, while appropriate for a pilot study, limits generalisability of findings. Finally, generalisability is limited to academic cardiac centres in jurisdictions where CR is available at no charge to patients.
In conclusion, CR referral across cardiac units in the same institution vary by 40% despite an eReferral strategy, with the rates highest observed on the cardiac surgery unit. Patients with heart failure, comorbid cancer, and longer lengths of inpatient stay were less often referred than those without. With regard to enrolment, those who had their referral redirected to a site located closer to their home were more likely to enrol. Finally, likely due to the eReferral system implemented institution-wide, the peer navigation intervention did not impact CR referral or enrolment.
Footnotes
Contributors: SFA-F made substantial contributions to the acquisition and analysis of the data, drafting the work. LBS made substantial contributions to the conception and design of the work, revised the manuscript critically for important intellectual content, and gave final approval of the manuscript. LJ acquired the outcome data, revised the manuscript critically for important intellectual content, and gave final approval of the manuscript. SLG made substantial contributions to the design of the work and interpretation of the data, drafted and gave final approval of the manuscript.
Funding: This research was supported by a generous donation from Ms. Katherine Munkley to the Toronto General and Western Hospital Foundation, Peter Munk Cardiac Centre campaign, and funding from the Stony Brook University, Office of the Senior Vice President for Health Sciences.
Competing interests: None declared.
Ethics approval: University Health Network Ethics Board and York University Ethics Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Mendis S, Puska P, Norrving B, eds. Global Atlas on cardiovascular disease prevention and control. Geneva: World Health Organization, 2011. [Google Scholar]
- 2.Anderson L, Oldridge N, Thompson DR et al. Exercise-based cardiac rehabilitation for coronary heart disease: cochrane Systematic Review and Meta-Analysis. J Am Coll Cardiol 2016;67:1–12. 10.1016/j.jacc.2015.10.044 [DOI] [PubMed] [Google Scholar]
- 3.Turk-Adawi K, Sarrafzadegan N, Grace SL. Global availability of cardiac rehabilitation. Nat Rev Cardiol 2014;11:586–696. 10.1038/nrcardio.2014.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Colella TJ, Gravely S, Marzolini S et al. Sex bias in referral of women to outpatient cardiac rehabilitation? A meta-analysis. Eur J Prev Cardiol 2015;22:423–41. 10.1177/2047487314520783 [DOI] [PubMed] [Google Scholar]
- 5.Cortés O, Arthur HM. Determinants of referral to cardiac rehabilitation programs in patients with coronary artery disease: a systematic review. Am Heart J 2006;151:249–56. 10.1016/j.ahj.2005.03.034 [DOI] [PubMed] [Google Scholar]
- 6.Clark AM, King-Shier KM, Duncan A et al. Factors influencing referral to cardiac rehabilitation and secondary prevention programs: a systematic review. Eur J Prev Cardiol 2013;20:692–700. 10.1177/2047487312447846 [DOI] [PubMed] [Google Scholar]
- 7.Clark AM, King-Shier KM, Thompson DR et al. A qualitative systematic review of influences on attendance at cardiac rehabilitation programs after referral. Am Hear J 2012;164:835–45. 10.1016/j.ahj.2012.08.020 [DOI] [PubMed] [Google Scholar]
- 8.Arena R, Williams M, Forman DE et al. , American Heart Association Exercise, Cardiac Rehabilitation and Prevention Committee of the Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Council on Nutrition, Physical Activity and Metabolism. Increasing referral and participation rates to outpatient cardiac rehabilitation: the valuable role of healthcare professionals in the inpatient and home health settings: a science advisory from the American heart association. Circulation 2012;125:1321–9. 10.1161/CIR.0b013e318246b1e5 [DOI] [PubMed] [Google Scholar]
- 9.Balady GJ, Fletcher BJ, Froelicher ES et al. Cardiac rehabilitation programs: a statement for healthcare professionals from the American Heart Association. Circulation 1994;90:1602–10. 10.1161/01.CIR.90.3.1602 [DOI] [PubMed] [Google Scholar]
- 10.Grace SL, Russell KL, Reid RD. Effect of cardiac rehabilitation referral strategies on utilization rates: a prospective, controlled study. Arch Intern Med 2011;171:235–41. 10.1001/archinternmed.2010.501 [DOI] [PubMed] [Google Scholar]
- 11.Gravely-Witte S, Leung YW, Nariani R et al. Effects of cardiac rehabilitation referral strategies on referral and enrollment rates. Nat Rev 2010;7:87–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grace SL, Chessex C, Arthur H et al. Systematizing inpatient referral to cardiac rehabilitation 2010: Canadian Association of Cardiac Rehabilitation and Canadian Cardiovascular Society joint position paper endorsed by the Cardiac Care Network of Ontario. Can J Cardiol 2011;27:192–9. 10.1016/j.cjca.2010.12.007 [DOI] [PubMed] [Google Scholar]
- 13.Grace SL, Leung YW, Reid R et al. The role of systematic inpatient cardiac rehabilitation referral in increasing equitable access and utilization. J Cardiopulm Rehabil Prev 2012;32:41–7. 10.1097/HCR.0b013e31823be13b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grace SL, Angevaare KL, Reid RD et al. CRCARE Investigators. Effectiveness of inpatient and outpatient strategies in increasing referral and utilization of cardiac rehabilitation: A prospective, multi-site study. Implement Sci 2012;7:120 10.1186/1748-5908-7-120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benz Scott L, Gravely S, Sexton TR et al. Examining the effect of a patient navigation intervention on outpatient cardiac rehabilitation awareness and enrollment. J Cardiopulm Rehabil Prev 2013;33:281–91. 10.1097/HCR.0b013e3182972dd6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benz Scott L, Gravely S, Sexton TR. Effect of patient navigation on enrollment in cardiac rehabilitation. JAMA Intern Med 2013;173:244–6. 10.1001/2013.jamainternmed.1042 [DOI] [PubMed] [Google Scholar]
- 17.Freeman HP. The history, principles, and future of patient navigation: commentary. Semin Oncol Nurs 2013;29:72–5. 10.1016/j.soncn.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 18.Freeman HP. Patient navigation: a community centered approach to reducing cancer mortality. J Cancer Educ 2006;21(1 Suppl):S11–14. 10.1207/s15430154jce2101s_4 [DOI] [PubMed] [Google Scholar]
- 19.Bradford JB, Coleman S, Cunningham W. HIV System Navigation: an emerging model to improve HIV care access. AIDS Patient Care STDS 2007;21(Suppl 1):S49–58. 10.1089/apc.2007.9987 [DOI] [PubMed] [Google Scholar]
- 20.Van Walleghem N, MacDonald CA, Dean HJ. The Maestro Project: a patient navigator for the transition of care for youth with type 1 diabetes. Diabetes Spectr 2011;24:9–13. 10.2337/diaspect.24.1.9 [DOI] [Google Scholar]
- 21.Sullivan C, Leon JB, Sayre SS et al. Impact of navigators on completion of steps in the kidney transplant process: a randomized, controlled trial. Clin J Am Soc Nephrol 2012;7:1639–45. 10.2215/CJN.11731111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naylor K, Ward J, Polite BN. Interventions to improve care related to colorectal cancer among racial and ethnic minorities: a systematic review. J Gen Intern Med 2012;27:1033–46. 10.1007/s11606-012-2044-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paskett ED, Harrop JP, Wells KJ. Patient navigation: a n update on the state of the science. CA Cancer J Clin 2011;61:237–49. 10.3322/caac.20111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robinson-White S, Conroy B, Slavish KH et al. Patient navigation in breast cancer: A systematic review. Cancer Nurs 2010;33:127–40. 10.1097/NCC.0b013e3181c40401 [DOI] [PubMed] [Google Scholar]
- 25.Wells KJ, Battaglia TA, Dudley DJ et al. Patient Navigation Research Program. Patient navigation: State of the art or is it science? Cancer 2008;113:1999–2010. 10.1002/cncr.23815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Whop LJ, Valery PC, Beesley VL et al. Navigating the cancer journey: a review of patient navigator programs for Indigenous cancer patients. Asia Pac J Clin Oncol 2012;8:e89–96. 10.1111/j.1743-7563.2012.01532.x [DOI] [PubMed] [Google Scholar]
- 27.Davidson PM. Another piece of the puzzle: Wait times call for integrated patient, provider, and system solutions for cardiac rehabilitation. Circ Cardiovasc Qual Outcomes 2015;8:539–40. 10.1161/CIRCOUTCOMES.115.002292 [DOI] [PubMed] [Google Scholar]
- 28.Benz Scott L. A call for intervention research to overcome barriers to women's enrollment in outpatient cardiac rehabilitation programs. J Womens Health (Larchmt) 2010;19:1951–3. 10.1089/jwh.2010.2416 [DOI] [PubMed] [Google Scholar]
- 29.Chalkidou K, Tunis S, Whicher D et al. The role for pragmatic randomized controlled trials (pRCTs) in comparative effectiveness research. Clin Trials 2012;9:436–46. 10.1177/1740774512450097 [DOI] [PubMed] [Google Scholar]
- 30.Arain M, Campbell MJ, Cooper CL et al. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;10:67 10.1186/1471-2288-10-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stone J, Suskin N, Arthur H. Canadian guidelines for cardiac rehabilitation and cardiovascular disease prevention: translating knowledge into action. 3rd edn Winnipeg, MB, Canada: Canadian Association of Cardiac Rehabilitation, 2009. [Google Scholar]
- 32.Brady S, Purdham D, Oh P et al. Clinical and sociodemographic correlates of referral for cardiac rehabilitation following cardiac revascularization in Ontario. Hear Lung 2013;42:320–5. 10.1016/j.hrtlng.2013.07.001 [DOI] [PubMed] [Google Scholar]
- 33.British Heart Foundation. The National Audit of Cardiac Rehabilitation Annual Statistical Report 2013 beating heart disease together. 2013.
- 34.Taylor RS, Sagar VA, Davies EJ et al. Exercise-based rehabilitation for heart failure. Cochrane Database Syst Rev 2014;4:CD003331 10.1002/14651858.CD003331.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rehabilitation AA of C and P, ed. American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 5th edn Chicago: American Association of Cardiovascular and Pulmonary Rehabilitation, 2013. [Google Scholar]
- 36.Forman DE. Rehabilitation practice patterns for patients with heart failure: the United States perspective. Heart Fail Clin 2015;11:89–94. [DOI] [PubMed] [Google Scholar]
- 37.Health Quality Ontario and Ministry of Health and Long Term Care. Quality-based procedures: clinical handbook for heart failure (acute and postacute). Toronto: Health Quality Ontario, 2015. http://www.hqontario.ca/evidence/evidence-process/episodes-of-care#community-chf [Google Scholar]