Abstract
Background:
Intensity of depressive symptoms could be exacerbated due to the paucity of appropriate treatments. We assessed the effectiveness of bibliotherapy and text messaging, which aimed at amelioration of patient's behavior and consciousness, which could lead to suicide prevention.
Methods:
This was a randomized clinical trial implemented in rural health centers of Isfahan district (Iran). Health centers were assigned in three trials consisting of the booklet, text messaging, and control groups. Each group consisted of 70 patients. Inclusion criteria were being affected by depressive symptom, <18 years, and cell phone accessibility. Mental retardation, drug and alcohol abuse, visual disability, dementia, suicide attempt history, electrotherapy, and receiving psychological interventions were our not met criteria. Our patient outcomes comprised intensity of depressive symptom and treatment compliance. The first two trials were requested to study instructive booklets in 30 days while the second cohort was demanded to study the booklet in accordance with the daily delivered text messaging.
Results:
Out of 210 individuals, 198 patients finished this study. The intensity of depressive symptom was significantly affected through time and group factors as well as time-group interaction (F = 12.30, P < 0.001). Based on treatment compliance, the interactive effect of group factor and the time factor was statistically significant.
Conclusions:
It seems that bibliotherapy could efficiently decrease the intensity of depressive symptoms. Nevertheless, in comparison with our booklet trial, the text messaging group achieved neither durable nor significant success; thus, bibliotherapy could be utilized as a complementary methodology aiming depression treatment.
Keywords: Behavior therapy, bibliotherapy, cognitive therapy, depressive symptom, psychotherapy, text messaging
INTRODUCTION
Epidemiological studies documented that depression is one of contemporary and psychological complaints since it is the fourth contributory reason of morbidity, and this position is swiftly escalating as the second in 2020.[1,2] In a study, which was conducted in Iran, female and male depression were in the second and ninth places (in 2004), respectively, when these ranking were determined in accordance with the disability-adjusted life year.[3] Depression is assumed as one of the chronic, recurrent, and debilitating diseases, which is commonly associated with other psychological disorders. On the other hand, not only depression treatment enhances capacity of affected women for sensitive parenting, but also management of this psychological disorder prevents developmental retardations (MRs) (such as poor language or low IQ), which may occur in the infants of the depressed parents. Management of this dilemma requires continuous and efficient care; nevertheless, neither primary care nor tailored treatment is applied for depressed individuals.[4,5,6]
Treatments of depressive symptoms are based on pharmaceutical and/or psychological approaches while psychotherapy efficacy resembles the former approach.[7]
Cognitive behavioral therapy (CBT), as a novel discovery, which is applied in the scope of psychotherapy has proved its efficacy.[8] Indeed, CBT exerts ameliorations of self-concept, pessimistic view toward the world, and negative thoughts of the future, which are defined as Beck triad of depression.[9,10,11] This therapeutic approach generally pursued face-to-face methods; nevertheless, these procedures failed to promote thorough achievement. It seems that this failure could be attributable to patient's humiliation and laxity, as well as the paucity of competent physicians, and the need for high disbursement.[12,13]
Bibliotheraphy is one of the most appropriate, applicable as well as inexpensive treatment approaches, which is recognized as a self-help guide; hence, it is less dependent to direct supervision of medical staff.[12,13] Its success; nevertheless, might be declined due to the paucity of enough patient's momentum in treatment procedure, especially when the patient's motivation did not suffice.[14,15]
Mobile phone based psychological intervention is assumed to promote both the health surveillance and treatment strategies, which are cost-effective and time-unlimited.[16] Indeed, text messaging intervention delivers suitable, real-time self-monitoring, and specialized provision for individuals, who are affected by depressive symptoms.[17,18]
To the best of our knowledge, there was not any publication evaluating the results of concomitant application of cell phone and bibliotherapy in depressive symptom treatment. In fact, we decided to evaluate the impacts of text messaging interventions, which aimed to inspire the affected patients to peruse bibliotherapy.
METHODS
This was a randomized clinical trial and multi-central study, which assessed the impressions of concomitant application of bibliotherapy and text messaging on the patient's recovery, as well as their treatment compliance. Our protocols were approved by the Medical Ethics Committee of Isfahan University of Medical Sciences, and informed consent was obtained from the patients (Project number = 393454).
Our study was conducted in rural health centers of Isfahan district, Iran. These centers were allocated to three trials, which included (1) control, (2) booklet, and (3) booklet and text messaging. Patient's demographic information, which included age, sex, marital status, and level of the literacy, was recorded by trained paramedics. Our survey outcomes comprised depression intensity and treatment compliance.
Study population
This experiment was conducted on individuals affected by depressive symptoms, who inhabited in rural areas of Isfahan district in Iran. The patients whose ages were over 18 years old and had accessibility to cell phones met our inclusion criteria. Not met criteria consisted of mental retardation (MR), visual disability leading to reading impediments, dementia, suicide attempt history, electrotherapy, and receiving the psychological intervention, as well as drug abuse and alcohol addiction. Our exclusion criteria were a patient disinclination to continue our treatment strategy.
Sampling and randomization
Initially, we divided Isfahan district, which was comprised 24 rural health centers, into eight clusters in accordance with their cultural, economic, and social likeness. Importantly, every cluster consisted in one control and two interventional groups. Then, every group was randomly assigned as either interventional, which consisted of “booklet,” “booklet associated with text messaging” groups, or control group.
Sample size
Patient recovery, which was consisted in Beck II questionnaire, was applied for sample size determination. Standard deviation and the test power were 10.5, and 80%, respectively, (α = 0.05, d = 5). Initially, 63 patients allocated to each group; however, considering 10% attrition, every group consisted of 70 patients.
Questionnaires
As mentioned earlier, our study was established on two questionnaires encompassing Beck II depression and medication adherence rating scale (MARS).
Beck II depression questionnaire
Beck II questionnaire comprised 21 items, which considered physical, behavioral and cognitive symptoms of the disease. The questionnaire validity and reliability were confirmed (Cronbach's α = 0.87, and r = 0.74) when it was translated to Persian (the ethnic language of our study population).[19]
Medication adherence rating scale questionnaire
Five questions, which had Likert scale form fluctuating between 1 (for the option being all of the time) and 5 (for the one suggesting never), constituted MARS questionnaire. We calculated sum of the scales differing from 5 to 25. In fact, the lowest sum of the scales indicated less patient's compliance. Furthermore, suitability of questionnaire reliability was previously documented (sensitivity: 70%, specificity: 38.9%, and Cronbach's α = 0.94).[20]
Interventions
This clinical trial was based upon two interventions (bibliotherapy and text messaging). Indeed, we aimed to treat “booklet and text messaging” group through booklet package associated with short messaging service; however, the “booklet” group just received the booklet.
Booklets, which were our bibliotherapy tools, were disseminated between our eligible patients of interventional groups, and we asked them or their guardians to read the booklet in 30 days. In fact, we concomitantly treated one trial of our patients with text messaging and booklet, whom we requested to study in accordance with the daily text messaging. After these procedures, we ask them to reply Beck II and MARS questionnaires two more times. Obviously, these questionnaires were responded three times: (1) Before the intervention (2) immediately after cessation of our intervention (3) 3 months after the cessation of our intervention.
Content of the booklet
Our booklet content was based on educational points documented by World Health Organization and other valid websites. These points were previously applied and cited by different articles while the overall context of our booklet was original. This booklet was written in accordance with the patient's culture.[21,22,23,24]
To elaborate, in this booklet a man, who was affected by depressive symptoms, gave an account of his experience in following psychotherapist help. The first chapter of the booklet, represented depression signs and symptoms, and the patient decided to find psychotherapy help to eliminate his depressive symptoms. A psychologist provided the patient with some description regarding psychotherapy and advantages of pharmaceutical treatments. In the second chapter, this psychologist depicted some negative ideas and thoughts (such as anger, contempt, disgust, and guilt) for the patient. In addition, the therapist provided the patient some efficient coping strategies against insomnia. The third chapter concerned appropriate solutions for overcoming the negative thoughts. The patient was also instructed in sleep hygiene. Fourth chapter tried to persuade the patient to find and conduct some suitable hobbies. Moreover, it promoted appropriate strategies, which aimed to overcome the patient's insomnia. The fifth and sixth (last) chapters tried to ameliorate the patient's capacity in problem dealing. Our booklet was not only fictional but also it was illustrated through the pictures to motivate our depressed individuals.
Importantly, we made further improvements of the booklet contents in accordance with ideas suggested by one psychologist, as well as one psychiatrist and two community medicine specialists. Additionally, a pilot study, which was preceded our study, provided us with patient's notions to ameliorate booklet's size, writing font, and pictures, as well as its vague contents.
The booklet contents tried to introduce the most current negative thoughts (such as black and white thinking, labeling, minimizing positive thoughts, emotional reasoning, etc.), which could potentially lead to depressive symptoms. The booklet encouraged the patient to check his/her negative thoughts with others and different perspectives. Not only the patients were fortified about the instructive strategies, which aimed at taking an observer role, but also these individuals were coaxed to break habits, which make them feel worse.
Text messages
Our text messaging contents, which were daily delivered (at 10 o’clock am), included either persuading passages, which tried to cajole the patients to study some special pages of the booklet, or aphorism (words of wisdom). Each sort of the text messaging was discretely delivered in odd or pair days. Importantly, we urged two community medicine specialists to review and validate all of the messages.
Statistical analyzing
All analyses performed by using SPSS version 18 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to present the demographic data. We used two-sample t-test and Chi-square test for the comparison of continuous variables, and categorical variables, respectively.
A repeated measures ANOVA was utilized to compare variables regarding the severity of depressive symptoms and treatment compliance scores for each group at different times. Analysis of the outcomes was based on intention to treat basis. Finally, ANCOVA was utilized to control confounder factors.
RESULTS
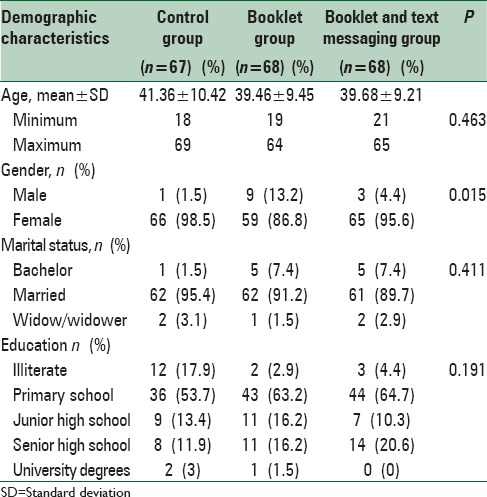
Out of 210 individuals, 198 patients finished this study [Figure 1]. Mean ages of the patients in booklet, text messaging, and control groups were 41.36 ± 10.42, 39.46 ± 9.45, and 39.68 ± 9.21 respectively. Ages, marital status, and educational levels of the patients did not differ significantly between our trials; nevertheless, frequency of sex significantly differed (P = 0.01) [Table 1].
Figure 1.
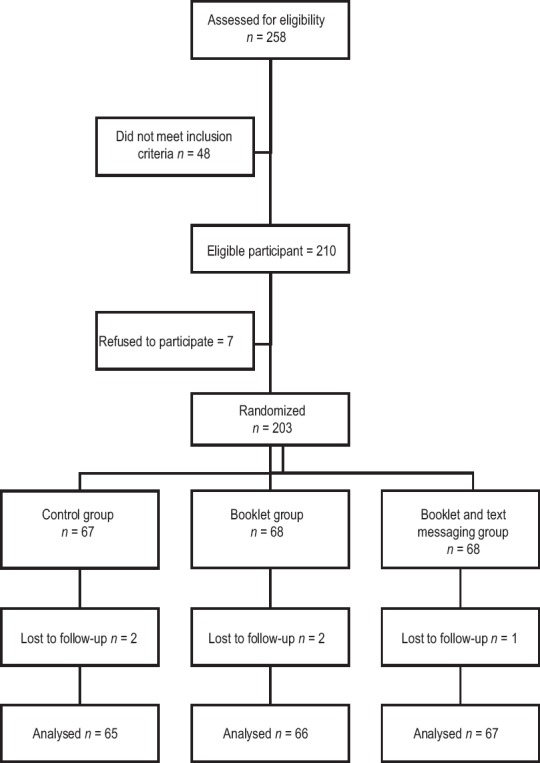
Flow diagram of depressed patients assigned to control, booklet or booklet and text messaging group
Table 1.
Demographic characteristics of depressed patients assigned to control, booklet or booklet and text messaging group
Repeated measures ANOVA documented that intensity of depressive symptoms was significantly affected through time and group factors as well as time-group interaction (F = 12.30, P < 0.001) [Table 2].
Table 2.
Analysis of variance for the evaluation of the main and interactive effects of time and treatment on depression intensity and treatment adherence in depressed patients
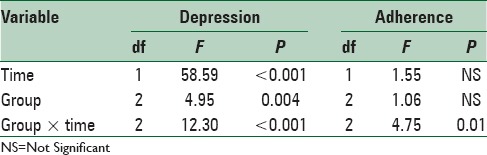
Based on treatment compliance interactive effect of group factor and the time factor was statistically significant [Table 2].
Post-hoc Bonferroni showed a significant difference in intensity of depressive symptoms between our interventional and control groups (P = 0.01); nevertheless, neither of the interventional groups differed in intensity of depressive symptoms [Table 3].
Table 3.
Comparison of the mean differences in depression intensity and treatment adherence between booklet, text messaging and control groups
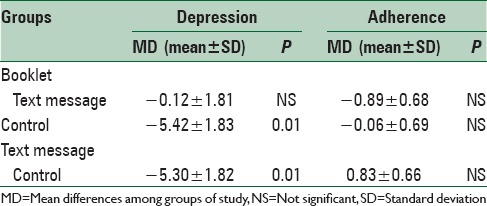
Data regarding patient's treatment compliance and variations occurred in the intensity of depressive symptoms at different times (before, immediately after the treatment, and 3 months after the intervention) have been shown in Table 4.
Table 4.
Comparison of the mean differences in depression intensity and treatment adherence between booklet, text messaging and control groups in three times: (1) Before treatment, (2) after treatment, (3) 3 months after the interventions
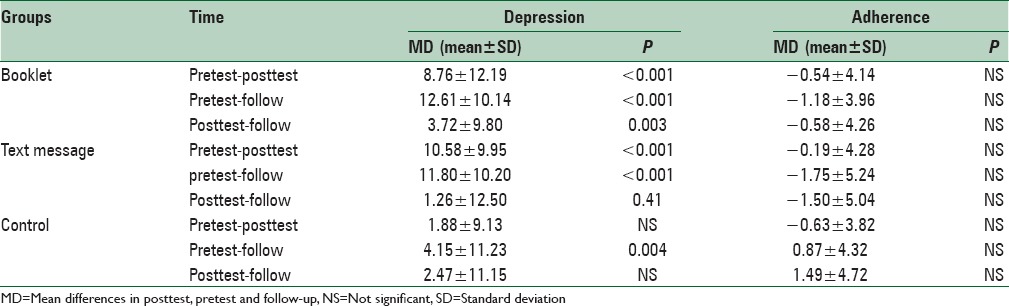
In fact, depressive symptom intensity of the patients treated through booklets significantly differed before and after the intervention (P < 0.001). Depressive symptom intensity of this group significantly differed when we compared the data not only before and 3 months after the intervention but also immediately and 3 months after the treatment (P < 0.001, and P = 0.003, respectively).
Depressive symptom intensity of the patients allocated in text messaging group significantly differed before and after the treatment (P < 0.001). Furthermore, comparison of depressive symptom intensity differed before and 3 months after the intervention (P < 0.001).
In addition, depressive symptom intensity of control group significantly differed before and 3 months after the intervention (P = 0.004).
Figure 2 shows mean of Beck score in baseline and fallow up times by intervention arm.
Figure 2.
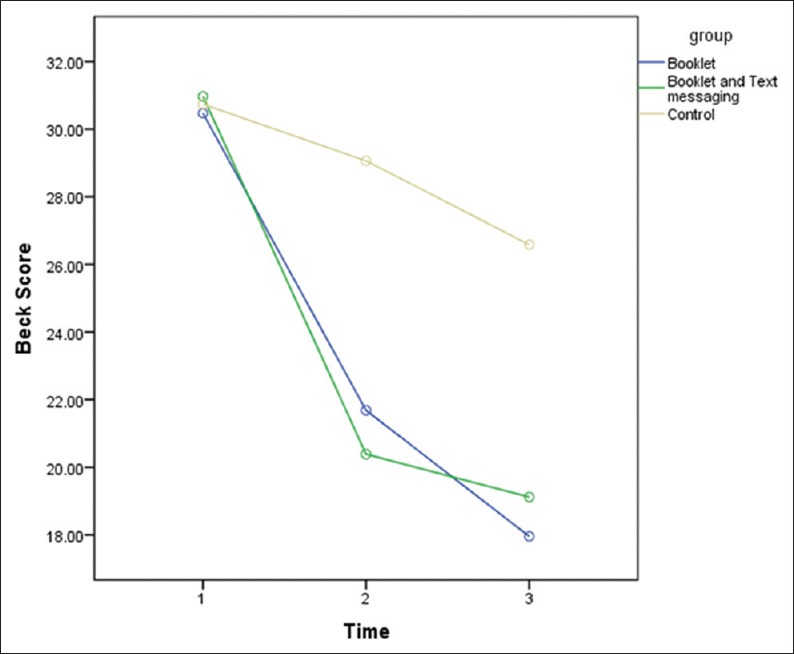
Mean of Beck score in baseline and follow-up times by intervention arm in control, booklet or booklet and text messaging group
Neither of the groups showed significant variations of the treatment compliance in different times comprising before the treatment, after the treatment or during the following up procedure [Table 4]. Gender distribution in the groups was unequal. Thus, ANCOVA analysis was applied. This application showed the insignificant impact of gender distribution.
DISCUSSION
The results of this study showed that the treatment approaches significantly decreased depressive symptom intensity in rural areas. Indeed, in comparison with our control group, depressive symptom intensity of the booklet, and the text messaging trials obviously ameliorated. Accordingly, the above-mentioned instructive interventions, are potent treatments for depression disorder while by comparison with the major city inhabitants, neither psychologists nor mental health services is easily available for the individuals residing in rural areas.[25] In most parts of the world, patients hardly access for CBT unless they reside in areas being close to the major academic center.[26] In addition, the majority of the patients, who are living in rural areas, are affected by a strong culture, which hampers face-to-face mental health services. In turn, the rural communities seem to have a propensity for self-reliance and self-managing.[27]
On the other hand, depressive symptom intensity, in either of the groups, significantly varied in different times. To elaborate, patients treated through bibliotherapy were quickly recuperated and the recovery process was on a continuum during the follow-up (3 months after the intervention). Immediately after the intervention, patients allocated in text messaging group achieved significant recovery; nevertheless, their recuperation process declined after the treatment. Three months after the intervention, our control group achieved obvious recovery when intensity of their depressive symptoms was compared with before the treatment; nevertheless, in comparison with the other groups, decline of depressive symptom intensity was negligible. This recovery might be ascribed to pharmaceutical approaches, which were recommended by primary health care. However, different studies addressed rural poverty as an unsolved problem and political debate in developing countries; therefore, low cost of CBT, especially when it is performed through bibliotherapy, can potentially diminish treatment expenditure.[28,29] For example, Tucker et al. postulated that high cost was recognized as a major treatment impediment for nearly over half of the rural area inhabitants. Not surprisingly, CBT-based bibliotherapy could be efficiently applied in rural areas challenging with economic problems.[30]
Neither of our treatment strategies significantly affected treatment compliance. Moreover, treatment adherence changes of each group were insignificant in different times; on the contrary, time-group interaction significantly affected patient compliance. It seems that our CBT method could efficiently impact rural area inhabitants. Indeed, we tried to provide our clienteles with appropriate bibliotherapy being in accordance with the current belief of our patients, which discourage them to apply appropriate medications.[26] In addition, stigma more significantly impedes current pharmaceutical treatments in rural areas; therefore, our instructive interventions could be practically applied for community health promotion.[29]
This research and previous ones documented that cognitive dysfunction should be assumed as crucial risk factor contributing toward treatment in compliance and exacerbation of depressive symptoms intensity. Indeed, individuals affected by depressive symptoms commonly challenge cognitive dysfunction, which jeopardizes seeking of treatment recommendations.[31,32] Moreover, beliefs concerning medication side effects could negatively affect medical adherence.[33] Not surprisingly, many researches were undertaken to utilize CBT for depressive symptoms. For example, Baumel demonstrated that CBT obviously resulted in remission of depressive symptoms.[34] In another study, patients significantly recuperated from depressive symptoms when pharmaceutical approaches were associated with CBT.[35] In addition, CBT cost-effectiveness was shown in refractory depressive symptoms, which were resistant to conventional pharmacotherapy.[36]
Accordingly, our research, as well as the previous ones, demonstrated that CBT mitigated patient's depressive symptoms.[37,38] It seems that this effectiveness could be attributable to indirect and direct impacts of CBT, which were conducted through the promotion of treatment compliance and psychological approaches respectively.[39,40]
Our instructive interventions aimed to regulate self-conscious emotion through alterations of thoughts and behaviors stemmed from consciousness and experiences. In fact, these instructions, which were mostly performed through the booklets, encouraged the patients to alter their negative opinions behaviors and self-conscious emotions. “Identification of negative thoughts,” as well as the “changing negative thought patterns and behaviors” were recognized as our proposed mechanisms, which led to the above-mentioned goals. Hence, bibliotherapy can be applied in health promotion system of different communities when it train people to harness frequencies, intensities, and durations of their negative moods.[41]
The results of this study showed indirect instructions, which was conducted in our interventional groups, decreased depressive symptom intensity. Our text messaging group and the booklet one, however, did not differ significantly in depressive symptom intensity. Furthermore, depressive symptom intensity of text messaging trial that was sought in following up period was not ameliorated. On the contrary, patients of the booklet trial, which did not receive text messages showed significant amelioration in the following period. It seems that CBT instructed through booklet had the most pivotal and persistent role in the reduction of depressive symptom intensity. These findings were in accordance with some of the previous studies, which well documented that bibliotherapy persistently diminished depressive symptom intensity. For example, Songprakun and McCann achieved persistent treatment gains while their CBT approach based upon bibliotherapy. They postulated that this kind of interventional method was convenient and could be easily applied by their patients at any time.[42]
Though many researchers documented positive impacts of text messages in different mental and health related issues (such as smoking, alcohol abuse, depression medical incompliance, aggressive behaviors, and diabetes self-managements), some bodies of literature proved that the efficacy of this kind of intervention was evanescent. For instance, Agyapong et al. postulated that positive outcomes of text messaging, which aimed at CBT of patients affected by depressive symptoms, were not sustainable beyond the intervention.[43,44,45,46]
The results of our study were in accordance with the above-mentioned articles when the supportive impact of text messaging could not be found beyond the CBT intervention. It seems that the subjects allocated to text messaging group were contingent upon text message; hence, in comparison with the other subjects, they had less concentration and dependency on booklet while text message was being discontinued. However, further investigations are indispensable to elaborate definite causes of unsustainable impacts of text messaging.[47]
Limitations
We could not evaluate text messaging impacts during the following period due to the cessation of the text messages. Gender distribution was unequal while male's frequency was rare; thus, data analysis of gender subgroups was impractical; besides, the results could not be generalized to males.
CONCLUSIONS
CBT, which is a nonpharmaceutical approach, should be noticed as well as the other conventional treatments. It seems that the above-mentioned procedure could be utilized as a complementary methodology aiming treatment of depressive symptoms.
ACKNOWLEDGEMENTS
This study was funded by research chancellor of Isfahan University of Medical Sciences (IUMS) as a dissertation project (no = 393454). The authors’ heartfelt thanks are extended to all the patients who so kindly agreed to contribute toward this study. Our profound gratefulness and deepest thanks are extended to all of the paramedics of health centers who so kindly agreed to collaborate in this study in spite of their high workload. Furthermore, we are greatly thankful of Dr. Nahid Geramian and the other staff of mental health unit (Health Vice Chancellor, IUMS, Isfahan, Iran) for their support throughout the project.
Footnotes
Source of Support: Research chancellor of Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Cizza G, Ronsaville DS, Kleitz H, Eskandari F, Mistry S, Torvik S, et al. Clinical subtypes of depression are associated with specific metabolic parameters and circadian endocrine profiles in women: The power study. PLoS One. 2012;7:e28912. doi: 10.1371/journal.pone.0028912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watts S, Mackenzie A, Thomas C, Griskaitis A, Mewton L, Williams A, et al. CBT for depression: A pilot RCT comparing mobile phone vs. computer. BMC Psychiatry. 2013;13:49. doi: 10.1186/1471-244X-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naghavi M, Abolhassani F, Pourmalek F, Lakeh M, Jafari N, Vaseghi S, et al. The burden of disease and injury in Iran 2003. Popul Health Metr. 2009;7:9. doi: 10.1186/1478-7954-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simon GE, VonKorff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. BMJ. 2000;320:550–4. doi: 10.1136/bmj.320.7234.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trivedi MH, Lin EH, Katon WJ. Consensus recommendations for improving adherence, self-management, and outcomes in patients with depression. CNS Spectr. 2007;12(8 Suppl 13):1–27. [PubMed] [Google Scholar]
- 6.Khadivi R, Shakeri M, Ghobadi S. The Efficiency of mental health integration in primary health care: A ten-year study. Int J Prev Med. 2012;3(Suppl 1):S139–45. [PMC free article] [PubMed] [Google Scholar]
- 7.Carlbring P, Lindner P, Martell C, Hassmén P, Forsberg L, Ström L, et al. The effects on depression of Internet-administered behavioural activation and physical exercise with treatment rationale and relapse prevention: Study protocol for a randomised controlled trial. Trials. 2013;14:35. doi: 10.1186/1745-6215-14-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fann JR, Bombardier CH, Vannoy S, Dyer J, Ludman E, Dikmen S, et al. Telephone and in-person cognitive behavioral therapy for major depression after traumatic brain injury: A randomized controlled trial. J Neurotrauma. 2015;32:45–57. doi: 10.1089/neu.2014.3423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ballard ED, Patel AB, Ward M, Lamis DA. Future disposition and suicidal ideation: Mediation by depressive symptom clusters. J Affect Disord. 2015;170:1–6. doi: 10.1016/j.jad.2014.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shafi AM, Shafi RM. Cultural influences on the presentation of depression. Open J Psychiatr. 2014;4:390. [Google Scholar]
- 11.Huang J, Sherraden M, Purnell JQ. Impacts of Child Development Accounts on maternal depressive symptoms: Evidence from a randomized statewide policy experiment. Soc Sci Med. 2014;112:30–8. doi: 10.1016/j.socscimed.2014.04.023. [DOI] [PubMed] [Google Scholar]
- 12.HANDI Project Team, Usher T. Bibliotherapy for depression. Aust Fam Physician. 2013;42:199–200. [PubMed] [Google Scholar]
- 13.Rohde P, Stice E, Shaw H, Brière FN. Indicated cognitive behavioral group depression prevention compared to bibliotherapy and brochure control: Acute effects of an effectiveness trial with adolescents. J Consult Clin Psychol. 2014;82:65–74. doi: 10.1037/a0034640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mead N, MacDonald W, Bower P, Lovell K, Richards D, Roberts C, et al. The clinical effectiveness of guided self-help versus waiting-list control in the management of anxiety and depression: A randomized controlled trial. Psychol Med. 2005;35:1633–43. doi: 10.1017/S003329170500560X. [DOI] [PubMed] [Google Scholar]
- 15.Rohde P, Stice E, Shaw H, Gau JM. Cognitive-behavioral group depression prevention compared to bibliotherapy and brochure control: Nonsignificant effects in pilot effectiveness trial with college students. Behav Res Ther. 2014;55:48–53. doi: 10.1016/j.brat.2014.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alvarez-Jimenez M, Alcazar-Corcoles MA, González-Blanch C, Bendall S, McGorry PD, Gleeson JF. Online, social media and mobile technologies for psychosis treatment: A systematic review on novel user-led interventions. Schizophr Res. 2014;156:96–106. doi: 10.1016/j.schres.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 17.Whittaker R, Merry S, Stasiak K, McDowell H, Doherty I, Shepherd M, et al. MEMO – A mobile phone depression prevention intervention for adolescents: Development process and postprogram findings on acceptability from a randomized controlled trial. J Med Internet Res. 2012;14:e13. doi: 10.2196/jmir.1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Proudfoot J, Clarke J, Birch MR, Whitton AE, Parker G, Manicavasagar V, et al. Impact of a mobile phone and web program on symptom and functional outcomes for people with mild-to-moderate depression, anxiety and stress: A randomised controlled trial. BMC Psychiatry. 2013;13:312. doi: 10.1186/1471-244X-13-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory – Second edition: BDI-II-PERSIAN. Depress Anxiety. 2005;21:185–92. doi: 10.1002/da.20070. [DOI] [PubMed] [Google Scholar]
- 20.Baljani E, Rahimi J, Amanpour E, Salimi S, Parkhashjoo M. Effects of a nursing intervention on improving self-efficacy and reducing cardiovascular risk factors in patients with cardiovascular diseases. HAYAT. 2011;17:45–54. [Google Scholar]
- 21.Donker T, Bennett K, Bennett A, Mackinnon A, van Straten A, Cuijpers P, et al. Internet-delivered interpersonal psychotherapy versus internet-delivered cognitive behavioral therapy for adults with depressive symptoms: Randomized controlled noninferiority trial. J Med Internet Res. 2013;15:e82. doi: 10.2196/jmir.2307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Depression Program. [Last cited on 2014 Mar 31]. Available from: https://www.ecouch.anu.edu.au/ecouch/dep_launch .
- 23.10-Day Insomnia Tutorial. [Last cited on 2014 Mar 31]. Available from: http://www.insomnia-free.com/chronic-insomnia-relief.html .
- 24.“I Had a Black Dog: His Name was Depression”. [Last accessed on 2014 Mar 31]. Available from: http://www.who.int/mental_health/management/depression/en/
- 25.Griffiths KM, Christensen H, Jorm AF. Mental health literacy as a function of remoteness of residence: An Australian national study. BMC Public Health. 2009;9:92. doi: 10.1186/1471-2458-9-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones E, Manassis K, Arnold P, Ickowicz A, Mendlowitz S, Nowrouzi B, et al. Translating Cognitive Behavioral Therapy for Anxious Youth to Rural-Community Settings via Tele-Psychiatry. Community Ment Health J. 2015;51:852–6. doi: 10.1007/s10597-015-9882-4. [DOI] [PubMed] [Google Scholar]
- 27.Griffiths KM, Christensen H. Internet-based mental health programs: A powerful tool in the rural medical kit. Aust J Rural Health. 2007;15:81–7. doi: 10.1111/j.1440-1584.2007.00859.x. [DOI] [PubMed] [Google Scholar]
- 28.Soltani A, Angelsen A, Eid T, Naieni MS, Shamekhi T. Poverty, sustainability, and household livelihood strategies in Zagros, Iran. Ecol Econ. 2012;79:60–70. [Google Scholar]
- 29.Brenes GA, Danhauer SC, Lyles MF, Hogan PE, Miller ME. Barriers to mental health treatment in rural older adults. Am J Geriatr Psychiatry. 2015 doi: 10.1016/j.jagp.2015.06.002. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tucker M, Oei TP. Is group more cost effective than individual cognitive behaviour therapy? The evidence is not solid yet. Behav Cogn Psychother. 2007;35:77–91. [Google Scholar]
- 31.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 32.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;16:CD000011. doi: 10.1002/14651858.CD000011.pub3. [DOI] [PubMed] [Google Scholar]
- 33.Bane C, Hughes CM, McElnay JC. The impact of depressive symptoms and psychosocial factors on medication adherence in cardiovascular disease. Patient Educ Couns. 2006;60:187–93. doi: 10.1016/j.pec.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Baumel S. Lincolnwood, IL: Keats Publishing; 2000. Dealing with Depression Naturally: Alternatives and Complementary Therapies for Restoring Emotional Health. [Google Scholar]
- 35.Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med. 2000;342:1462–70. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- 36.Hollinghurst S, Carroll FE, Abel A, Campbell J, Garland A, Jerrom B, et al. Cost-effectiveness of cognitive-behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: Economic evaluation of the CoBalT trial. Br J Psychiatry. 2014;204:69–76. doi: 10.1192/bjp.bp.112.125286. [DOI] [PubMed] [Google Scholar]
- 37.Safren SA, Hendriksen ES, Mayer KH, Mimiaga MJ, Pickard R, Otto MW. Cognitive-behavioral therapy for HIV medication adherence and depression. Cogn Behav Pract. 2004;11:415–24. [Google Scholar]
- 38.Safren SA, O’Cleirigh C, Tan JY, Raminani SR, Reilly LC, Otto MW, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol. 2009;28:1–10. doi: 10.1037/a0012715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abbasian F, Najimi A, Ghasemi G, Afshar H, Meftagh SD. The effectiveness of the cognitive-behavioral strategies of stress management training on social adjustment of depressed women. J Res Health. 2013;3:303–9. [Google Scholar]
- 40.Abbasian F, Najimi A, Meftagh SD, Ghasemi G, Afshar H. The effect of stress management training on stress and depression in women with depression disorders: Using cognitive-behavioral techniques. J Educ Health Promot. 2014;3:70. doi: 10.4103/2277-9531.134819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muñoz RF. The prevention of depression: Current research and practice. Appl Prev Psychol. 1994;2:21–33. [Google Scholar]
- 42.Songprakun W, McCann TV. Evaluation of a bibliotherapy manual for reducing psychological distress in people with depression: A randomized controlled trial. J Adv Nurs. 2012;68:2674–84. doi: 10.1111/j.1365-2648.2012.05966.x. [DOI] [PubMed] [Google Scholar]
- 43.Agyapong VI, McLoughlin DM, Farren CK. Six-months outcomes of a randomised trial of supportive text messaging for depression and comorbid alcohol use disorder. J Affect Disord. 2013;151:100–4. doi: 10.1016/j.jad.2013.05.058. [DOI] [PubMed] [Google Scholar]
- 44.Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009;36:165–73. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 45.Rajabi A, Ghasemzadeh A, Ashrafpouri Z, Saadat M. Effects of counseling by mobile phone short message service (SMS) on reducing aggressive behavior in adolescence. Procedia Soc Behav Sci. 2012;46:1138–42. [Google Scholar]
- 46.Aboujaoude E, Salame W, Naim L. Telemental health: A status update. World Psychiatry. 2015;14:223–30. doi: 10.1002/wps.20218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vodopivec-Jamsek V, de Jongh T, Gurol-Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database Syst Rev. 2012;12:CD007457. doi: 10.1002/14651858.CD007457.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]


