Abstract
Background:
Although physical activity (PA) has long been associated with cardiovascular disease (CVD), assessment of PA status has never been used as a part of CVD risk prediction tools. The aim of the present work was to examine whether the inclusion of PA status in a CVD risk model improves its predictive accuracy.
Methods:
Data from the 10-year follow-up (2002–2012) of the n = 2020 participants (aged 18–89 years) of the ATTICA prospective study were used to test the research hypothesis. The HellenicSCORE (that incorporates age, sex, smoking, total cholesterol, and systolic blood pressure levels) was calculated to estimate the baseline 10-year CVD risk; assessment of PA status was based on the International Physical Activity Questionnaire. The estimated CVD risk was tested against the observed 10-year incidence (i.e., development of acute coronary syndromes, stroke, or other CVD according to the World Health Organization [WHO]-International Classification of Diseases [ICD]-10 criteria). Changes in the predictive ability of the nested CVD risk model that contained the HellenicSCORE plus PA assessment were evaluated using Harrell's C and net reclassification index.
Results:
Both HellenicSCORE and PA status were predictors of future CVD events (P < 0.05). However, the estimating classification bias of the model that included only the HellenicSCORE was significantly reduced when PA assessment was included (Harrel's C = 0.012, P = 0.032); this reduction remained significant even when adjusted for diabetes mellitus and dietary habits (P < 0.05).
Conclusions:
CVD risk scores seem to be more accurate by incorporating individuals’ PA status; thus, may be more effective tools in primary prevention by efficiently allocating CVD candidates.
Keywords: Cardiovascular disease, diet, physical activity, prevention, risk prediction
INTRODUCTION
To achieve more effective cardiovascular disease (CVD) prevention, the European Society of Cardiology (ESC) strongly suggested the individual overall risk estimation through risk scores.[1] The Framingham Heart Study was the pioneer in this field;[2] however, due to methodological concerns raised for its application to different populations, the ESC proposed the Systematic COronary Risk Evaluation (SCORE) project.[3,4,5] Despite the work has been done, the accuracy and use in daily practice of CVD risk prediction models is still a matter of concern.[6,7,8] Under this context, attempts have been made to test whether risk models’ classification ability is improved by the inclusion of lifestyle aspects.[9,10] It is widely accepted that physical activity (PA) stands as an effective lifestyle approach that protects against noncommunicable diseases, such as CVD, obesity, hypertension, as well as childhood obesity, through various mechanisms.[11,12] However, to the best of our knowledge, PA status has never been used as a component in a CVD risk prediction tool.
Thus, the aim of the present work was to evaluate whether the inclusion of PA status in a risk model that already contained overall CVD risk assessment using the SCORE has an impact on the accuracy of the model's predictions.
METHODS
To evaluate the aforementioned research hypothesis, the data set of the ATTICA study was used.[13]
Sampling procedure at baseline examination
The ATTICA is a prospective observational study that was carried in Greece and specifically in the greater metropolitan Athens area, which included 78% urban and 22% rural regions. The study was carried out during 2001–2002. The main aims of the study were to evaluate the prevalence of CVD risk factors and the 10-year (2002–2012) incidence of the disease and its predictors. Of the initially 4056 randomly allocated individuals, 3042 agreed to participate (75% participation rate); there were no sociodemographic differences between those agreed to participate and the rest (all P's > 0.05); 1514 of the participants were men (18–87 years) and 1528 were women (18–89 years). All participants were free of CVD or cancer at baseline examination, as assessed through a detailed clinical evaluation by the study's physicians. Details about the methodology and procedures of the ATTICA study have been presented elsewhere.[9,13]
Funding
The Hellenic Cardiology Society, the Hellenic Atherosclerosis Society, the Graduate Program in Applied Nutrition and Dietetics of Harokopio University, and the Coca-Cola SA funded this study by research grants (KE252/ELKE/HUA).
Ethics
The Institutional Ethics Committees (First Cardiology Clinic, School of Medicine, University of Athens, and Harokopio University) have approved the study's protocol.
Measurements at baseline examination
Various baseline sociodemographic, biological, clinical, behavioral, and lifestyle characteristics of the participants were recorded through face-to-face interviews and clinical examinations that were carried on by the study's investigators. Arterial blood pressure was measured at the end of the baseline physical examination following standard procedures.[9] Participants whose blood pressure levels were greater or equal to 140/90 mmHg or were under antihypertensive medication were classified as hypertensive. Serum total cholesterol levels were measured using chromatographic enzymic method in a Technicon automatic analyzer RA-1000 (Dade Behring, Marburg, Germany). Hypercholesterolemia was defined as total cholesterol levels >200 mg/dl or the use of lipids-lowering agents. Blood glucose levels (mg/dl) were measured with a Beckman Glucose Analyzer (Beckman Instruments, Fullerton, CA, USA); diabetes mellitus (Type 2) was defined according to the American Diabetes Association diagnostic criteria (i.e., blood glucose levels >125 mg/dl classified participants as having diabetes). C-reactive protein was measured by particle-enhanced immuno-nephelometry. The International Physical Activity Questionnaire (IPAQ) was used as an index of weekly energy expenditure using frequency (times/week), duration (min/time), and intensity of sports or other habits.[14] To reduce skewness of the variable metabolic equivalents of task (MET)-min/week, the tertiles of METs were used in the present analysis (<150, 150–720, ≥720 MET-min weekly) rather than the IPAQ cut-offs. Furthermore, as regards smoking habits, smokers were defined as those who were smoking at least one cigarette/day during the past year or had recently stopped smoking (within last year); the rest were defined as nonsmokers. The MedDietScore was used to evaluate adherence to the Mediterranean diet; it is an index consisting of 11 questions regarding consumption frequency of the main foods of the Mediterranean diet pyramid. In particular, individual ratings (from 0 to 5 or the reverse) were assigned in each of the 11 food groups according to their position in the Mediterranean diet pyramid. Thus, the score ranges from 0 to 55. Higher values of this diet score indicate greater adherence to the Mediterranean diet. The MedDietScore has been previously validated and extensively used.[15,16]
Evaluation of estimated 10-year risk
The estimated 10-year CVD risk of the participants was calculated using the HellenicSCORE, which is a calibrated version of the ESC SCORE.[5] Briefly, to calibrate the ESC SCORE model for the Greek population, national mortality and prevalence data regarding systolic blood pressure, total serum cholesterol, and smoking habits, by age group and gender, were used; whereas, annual CVD death rates were obtained from the WHO mortality database for 2002.[17] The applied calibration method has been recommended by D’Agostino et al.,[18] and both the ESC SCORE and the HellenicSCORE have been extensively been used in clinical practice and research, as well.
Follow-up examination (2002–2012)
During 2011–2012, the ATTICA study's investigators performed the 10-year follow-up (2002–2012). Of the n = 3042 initially enrolled participants, n = 2583 were found during the follow-up (15% lost to follow-up). For the present work, data from n = 2020 participants with accurate CVD evaluation were used. Among other characteristics, information about participants’: (a) Vital status (death from any cause or due to CVD), (b) development of coronary heart disease (CHD) (i.e., myocardial infarction, angina pectoris, other identified forms of ischemia-WHO-ICD coding 410–414.9, 427.2, 427.6-, heart failure of different types, and chronic arrhythmias-WHO-ICD coding 400.0–404.9, 427.0–427.5, 427.9-), and (c) development of stroke (WHO-ICD coding 430–438) was assessed. These outcomes were used here to calculate individuals’ observed CVD risk and compare it with the estimated risk mentioned above.
Statistical analysis
Unadjusted, nonfatal, and fatal incidence rates of combined CVD outcomes (i.e., CHD or stroke) were calculated as the ratio of new cases to the number of people participated in the follow-up. Continuous variables were presented as mean values ± standard deviation or median (interquartile range) and qualitative variables were presented as frequencies (and percentages). Associations between categorical variables were tested using the Chi-square test. Comparisons between mean values of normally distributed variables between those who developed an event and the rest of the participants were performed using Student's t-test, after controlling for equality of variances using the criterion suggested by Levene. Distribution of the continuous variables was tested for normality through P-P plots. For continuous variables that were not normally distributed (i.e., C-reactive protein levels), the Mann–Whitney nonparametric test was applied to evaluate the differences in the distributions of the skewed variables between those who developed a CVD event and the CVD-free participants. Analysis of Variance was used to evaluate comparisons between mean values of normally distributed variables for the tertiles of METs, whereas the Kruskal–Wallis test was applied to evaluate the differences in the distributions of the skewed variables among the tertiles of METs. The hazard ratios (HRs) of developing a CVD event during the 10-year period, with their 95% confidence intervals (CIs), were estimated using Cox proportional hazards models. The proportionality of hazards was assessed using the appropriate graph and statistical test (Schoenfeld residuals). The time-to-CVD-event was recorded on annual basis. Log-rank test was also applied to evaluate differences between groups of participants as regards CVD incidence. Certain variables of biological interest were forced in the final models. Corresponding HR curves were adjusted for HellenicSCORE, diabetes mellitus, and levels of C-reactive protein. Calibration of the multivariable survival models was performed by comparing predicted probabilities and actual observed risk. Improvement in goodness of fit after adding MedDietScore to established risk factors was assessed by the likelihood ratio test. The incremental predictive value of HellenicSCORE by PA ascertainment over established risk factors already included in the model was assessed using Harrell's C-index for censored time-to-event data (measure for model discrimination with larger values indicating better discrimination).[19,20] Harrell's C of inverse HR was used as a measure of the predictive power of survival regression models after splitting data into training and test sets to avoid over-optimistic estimates and statistics derived with the STATA procedures “somers d” and “lincom.”[21,22] All reported P values were based on two-sided tests. SPSS version 21 (Statistical Package for Social Sciences, SPSS Inc., Chicago, IL, USA) software was used for all other statistical calculations.
RESULTS
Ten-year cardiovascular disease incidence rate
The combined, fatal, and nonfatal, 10-year CVD incidence was n = 317 (15.7%) (mean follow-up time 8.41 years). Of the n = 317 cases, n = 198 (19.7%) were men and n = 119 (11.7%) were women (P for gender difference <0.001). Moreover, 46 out of 317 events were fatal (n = 34 men) and thus, the overall 10-year fatal CVD rate was 1.8% (3.4% for men and 1.2% for women). Baseline characteristics of the participants by CVD status at 10-year are presented in Table 1. Participants who developed CVD were older, men, had increased blood lipids, systolic/diastolic blood pressure, glucose, C-reactive protein, as well as lower levels of adherence to the Mediterranean diet (all P < 0.001). No significant difference was detected as regards to other characteristics of the participants [Table 1].
Table 1.
Characteristics of the ATTICA study's participants (n=2020) according to the 10-year fatal or nonfatal incidence of cardiovascular disease

Baseline characteristics of the participants by METs’ tertiles are presented in Table 2. As it can be seen, the group of active participants consisted of men, nonsmokers, and lower C-reactive protein levels. No significant difference was detected as regards to other characteristics of the participants [Table 2].
Table 2.
Characteristics of the ATTICA study's participants (n=2020) according to the physical activity tertiles of the participants

Estimated 10-year cardiovascular disease risk using the HellenicSCORE
The HellenicSCORE was divided into seven classes (i.e., <1%, 1%, 2%, 3–4%, 5–9%, 10–14%, and >14% risk of developing fatal CVD events during the next 10-years based on the baseline information) according to the classification given by the ESC SCORE.[4] A highly significant association between those who developed a CVD event and classes of HellenicSCORE was observed, since much more people who were classified in the higher classes of CVD risk, developed an event actually [Table 3].
Table 3.
10-year (2001-2011) fatal and nonfatal incidence of cardiovascular disease, in men and women participated in the ATTICA study, according to the HellenicSCORE classification
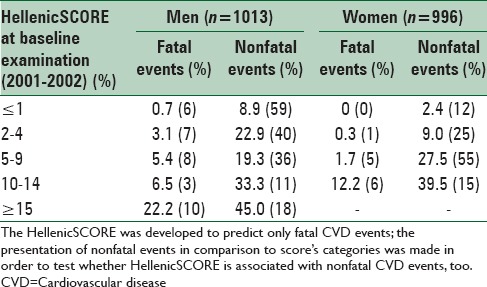
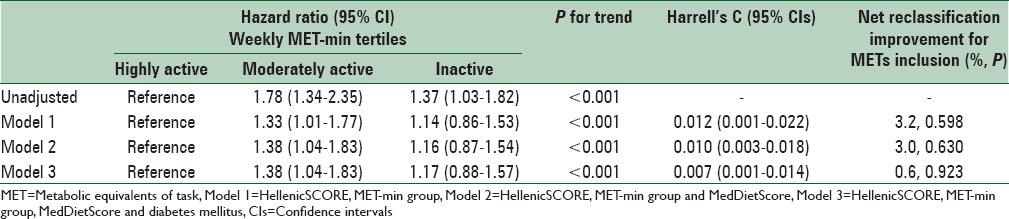
Concerning the 10-year risk for fatal CVD, PA status and HellenicSCORE were modeled separately to examine the explanatory ability of each factor. Furthermore, the two factors were modeled together to evaluate the additive ability of the PA assessment in predicting fatal CVD events. Physical inactivity status was positively associated with future CVD fatal events (HR for lowest vs. highest PA tertile = 1.91, 95% CI: 0.95, 3.84). Moreover, the HellenicSCORE was also a significant predictor of fatal CVD events (HR per 1 class increase = 2.08, 95% CI: 1.71, 2.54).
Although the HellenicSCORE has been developed for predicting fatal CVD events, the aforementioned analyses were also performed for the overall CVD outcomes [Table 4]. Specifically, the unadjusted model that included only PA status revealed that the lowest versus highest tertile was positively associated with future fatal and nonfatal CVD events (HR = 1.37, 95% CI: 1.03, 1.82); similarly, the unadjusted model that included only the HellenicSCORE was also highly significant in predicting fatal and nonfatal CVD events (HR = 2.05, 95% CI: 1.69, 2.5). Then, HellenicSCORE and PA status were modeled together. Both HellenicSCORE (HR per 1 class increase = 1.83, 95% CI: 1.48, 2.26) and PA status (HR lowest vs. highest class = 1.33, 95% CI: 1.01, 1.77) remained significantly and independently associated with 10-year fatal and nonfatal CVD risk. Moreover, when the PA status was taken into account in addition to the HellenicSCORE, the incremental ability of the final risk model in predicting fatal and nonfatal CVD events was improved (Harrell's C = 0.012, P = 0.03). Regarding residual CVD risk that could not be adequately estimated only with HellenicSCORE, the discriminating ability of PA status over additional predictors was further explored. The nested models included the HellenicSCORE as well as the level of adherence to the Mediterranean diet (through the MedDietScore), C-reactive protein, and diabetes mellitus, as the major CVD risk factors that were not incorporated in the HellenicSCORE. When PA status was taken into account over HellenicSCORE and MedDietScore, the incremental ability of the risk model in predicting CVD fatal events was improved (Harrell's C = 0.010, P = 0.008) [Table 4]. However, the inclusion of PA status did not manage to increase the reclassification properties of the models already including the HellenicSCORE [Table 4]. When C-reactive protein levels were included in the risk model, the PA status lost its incremental classification ability (Harrell's C = 0.003 P = 0.440). Moreover, the interaction between PA group and C-reactive protein levels was not significant (P = 0.535).
Table 4.
Results from survival models that evaluated the association between physical activity level with the 10-year risk for cardiovascular disease events (n=2020), and calibration parameters of the estimated models
DISCUSSION
In the present work, it was revealed that the inclusion of PA in a CVD risk prediction model improves tool's correct classification ability. In particular, the inclusion of participants’ PA status in a model that already contained the HellenicSCORE (that incorporates the risk derived from age, sex, smoking, cholesterol, and blood pressure levels), as well as history of diabetes and dietary habits evaluation, increased model's accuracy in predicting future CVD events. The latter finding deserves further attention from a public health perspective, since the incorporation in daily setting will improve CVD risk management at both individual and population level, through accurately “allocating” the potential future CVD “candidate.” Moreover, accurate determination of the potential CVD candidate reduces false positive results, improves accreditation to risk assessment tools, and above all, provides to the physicians and healthcare providers a practical tool for defending against the increasing burden of cardiac diseases.
Recent epidemiological reports in Europe presented decreasing CVD incidence and confirmed the existence of effective screening tools, treatments, and medical practice nowadays,[1] while more CVD events occur due to lifestyle factors, such as unhealthy dietary habits, physical inactivity, and smoking, suggesting that there is still residual CVD risk that might be treated with a lifestyle-targeted approach.[2] Simultaneously, the statistical prediction of CVD risk has received much interest during the few past years. Consequently, several prediction models have been developed for the prevention of CVD,[23] but still, the set of risk factors is, more or less, limited, so, several investigators claim that the effort of risk prediction still needs more attention.[6] Inaccuracies in the predictions were mainly attributed to the lack of important information that should have been incorporated in these models, such as dietary habits, PA status, and other lifestyle factors. In a recent report from our team, the MedDietScore assessment was strongly associated with better calibration of the predictions when included in the model containing the traditional CVD risk factors.[9]
As regards the protective role of PA against CVD, this is not surprising, as it is widely accepted that being physically active offers protection against CVD development through several biological paths, such as reducing arterial blood pressure, reducing inflammation, balancing body weight of subjects, increasing insulin sensitivity and decreasing depression levels, and should be treated separately than traditional CVD risk factors and dietary habits.[7,24,25,26,27]
From a methodological point-of-view, it is recognized that there are two elements that describe the reliability of risk prediction models, calibration, and discrimination. According to what has been previously discussed, presence of bias in CVD risk prediction may be considered as a fact in cardiovascular epidemiology. For example, regarding the performance of Framingham risk functions on European populations, it has been observed that the score sheets overestimate CVD risk in Southern European populations.[28] Previous studies have suggested that in Northern European populations, the Framingham Heart Study score sheets predict with accuracy the number of observed CVD events.[29] On the contrary, validation studies have shown that Framingham sheets overestimate the individual risk of CVD in representative British and Denmark populations.[30] These inaccuracies in prediction were not attributed to the incidence differences of the various manifestations of CVD (i.e., fatal, hard, and mild). However, homogeneity analysis revealed that these discrepancies in estimating actual risk were not attributed to differences in the traditional CVD risk factors levels. Thus, there is a need for proposing additional factors that might reduce bias in CVD risk prediction models. In the present work, it was revealed that PA assessment seems to play an important role in increasing the accuracy of a CVD risk model's prediction.
Strengths and limitations
Strength of the present work is that middle-aged population was studied for developing CVD, which is very important when addressing patho-biological research hypotheses concerning CVD prevention. Although the assessment of various clinical risk factors performed once, and may be prone to measurement error. However, applied methodology was similar to those of other prospective epidemiological studies globally and the results are comparable. Concerning the assessment of PA status, the use of IPAQ provides an assessment bending on the previous week, suggesting that the results cannot be extrapolated to future times. Thus, it is possible that major changes in PA status may have occurred within the decade, but this is the most commonly used methodology for evaluating the effect of PA on CVD risk. The sample used for the validation procedure (i.e., the ATTICA study's database) may not be representative of the whole Greek population, but it should be underlined that roughly half of the population lives in the surveyed area. Furthermore, the incorporation of PA status directly in the SCORE tool, as age groups, sex, smoking categories, etc., may indeed reveal tools predictive value. However, the relatively small number of observed events in the ATTICA study did not allow for such analysis.
CONCLUSIONS
Based on a large, population-based sample of men and women, it was revealed that the estimation bias of future CVD events is still high. In particular, although a widely accepted tool was used to predict future cardiac events (i.e., the ESC SCORE), approximately, one-tenth of the participants were misclassified. Moreover, inclusion of lifestyle characteristics, such as PA habits, in the risk models, increased CVD risk prediction accuracy. The results of this work have not been confirmed in other populations, yet however, the addition of PA assessment in CVD risk prediction models, on the top of dietary habits’ assessment and clinical factors, may help clinicians and public health policy makers to better predict, and consequently, prevent new CVD events.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) Eur Heart J. 2012;33:1635–701. doi: 10.1093/eurheartj/ehs092. [DOI] [PubMed] [Google Scholar]
- 2.Kannel WB, McGee D, Gordon T. A general cardiovascular risk profile: The Framingham study. Am J Cardiol. 1976;38:46–51. doi: 10.1016/0002-9149(76)90061-8. [DOI] [PubMed] [Google Scholar]
- 3.Pyörälä K. Assessment of coronary heart disease risk in populations with different levels of risk. Eur Heart J. 2000;21:348–50. doi: 10.1053/euhj.1999.1927. [DOI] [PubMed] [Google Scholar]
- 4.Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 5.Panagiotakos DB, Fitzgerald AP, Pitsavos C, Pipilis A, Graham I, Stefanadis C. Statistical modelling of 10-year fatal cardiovascular disease risk in Greece: The HellenicSCORE (a calibration of the ESC SCORE project) Hellenic J Cardiol. 2007;48:55–63. [PubMed] [Google Scholar]
- 6.Panagiotakos D. Health measurement scales: Methodological issues. Open Cardiovasc Med J. 2009;3:160–5. doi: 10.2174/1874192400903010160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooney MT, Dudina AL, Graham IM. Value and limitations of existing scores for the assessment of cardiovascular risk: A review for clinicians. J Am Coll Cardiol. 2009;54:1209–27. doi: 10.1016/j.jacc.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Georgousopoulou EN, Pitsavos C, Yannakoulia M, Panagiotakos DB. The role of dietary patterns’ assessment in the predictive ability of cardiovascular disease risk estimation models: A review. Int J Food Sci Nutr. 2014;65:3–8. doi: 10.3109/09637486.2013.827634. [DOI] [PubMed] [Google Scholar]
- 9.Georgousopoulou EN, Panagiotakos DB, Pitsavos C, Stefanadis C ATTICA Study Group. Assessment of diet quality improves the classification ability of cardiovascular risk score in predicting future events: The 10-year follow-up of the ATTICA study (2002-2012) Eur J Prev Cardiol. 2015;22:1488–98. doi: 10.1177/2047487314555095. [DOI] [PubMed] [Google Scholar]
- 10.Dhana K, Ikram MA, Hofman A, Franco OH, Kavousi M. Anthropometric measures in cardiovascular disease prediction: Comparison of laboratory-based versus non-laboratory-based model. Heart. 2015;101:377–83. doi: 10.1136/heartjnl-2014-306704. [DOI] [PubMed] [Google Scholar]
- 11.LeFevre ML. U.S. Preventive Services Task Force. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: U.S Preventive Services Task Force Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: US Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2014;161:587–93. doi: 10.7326/M14-1796. [DOI] [PubMed] [Google Scholar]
- 12.Marandi SM, Minasian V, Kelishadi R, Khalighinejad P, Borojeni MM, Borghi SH. Short-term effects of a physical activity intervention on obesity and cardiovascular fitness of 12-14-year-old boy students. Int J Prev Med. 2014;5(Suppl 2):S114–9. doi: 10.4103/2008-7802.157668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pitsavos C, Panagiotakos DB, Chrysohoou C, Stefanadis C. Epidemiology of cardiovascular risk factors in Greece: Aims, design and baseline characteristics of the ATTICA study. BMC Public Health. 2003;3:32. doi: 10.1186/1471-2458-3-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Papathanasiou G, Georgoudis G, Georgakopoulos D, Katsouras C, Kalfakakou V, Evangelou A. Criterion-related validity of the short International Physical Activity Questionnaire against exercise capacity in young adults. Eur J Cardiovasc Prev Rehabil. 2010;17:380–6. doi: 10.1097/HJR.0b013e328333ede6. [DOI] [PubMed] [Google Scholar]
- 15.Panagiotakos DB, Pitsavos C, Stefanadis C. Dietary patterns: A Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr Metab Cardiovasc Dis. 2006;16:559–68. doi: 10.1016/j.numecd.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 16.Panagiotakos D, Kalogeropoulos N, Pitsavos C, Roussinou G, Palliou K, Chrysohoou C, et al. Validation of the MedDietScore via the determination of plasma fatty acids. Int J Food Sci Nutr. 2009;60(Suppl 5):168–80. doi: 10.1080/09637480902810338. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Mortality Data Statistics Web Site. WHO. [Last cited on 2006 Feb 10]. Available from: http://www.who.int/whosis/mort/table1.cfm?path=whosis,mort,mort_table1#language=english .
- 18.D’Agostino RB, Sr , Grundy S, Sullivan LM, Wilson P; CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: Results of a multiple ethnic groups investigation. JAMA. 2001;286:180–7. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 19.Cox DR, Oakes D. London, United Kingdom: Chapman and Hall Publisher; 1998. Analysis of Survival Data – Monographs on Statistics and Applied Probability. [Google Scholar]
- 20.Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation. 2007;115:928–35. doi: 10.1161/CIRCULATIONAHA.106.672402. [DOI] [PubMed] [Google Scholar]
- 21.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–87. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 22.Newson RB. Comparing the predictive powers of survival models using Harrell's C or Somers’ D. Stata J. 2010;10:339–58. [Google Scholar]
- 23.Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, et al. European guidelines on cardiovascular disease prevention in clinical practice: Full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) Eur J Cardiovasc Prev Rehabil. 2007;14(Suppl 2):S1–113. doi: 10.1097/01.hjr.0000277983.23934.c9. [DOI] [PubMed] [Google Scholar]
- 24.Hamer M, Ingle L, Carroll S, Stamatakis E. Physical activity and cardiovascular mortality risk: Possible protective mechanisms? Med Sci Sports Exerc. 2012;44:84–8. doi: 10.1249/MSS.0b013e3182251077. [DOI] [PubMed] [Google Scholar]
- 25.Macniven R, Engelen L, Kacen MJ, Bauman A. Does a corporate worksite physical activity program reach those who are inactive. Findings from an evaluation of the Global Corporate Challenge? Health Promot J Austr. 2015;26:142–5. doi: 10.1071/HE14033. [DOI] [PubMed] [Google Scholar]
- 26.White DK, Gabriel KP, Kim Y, Lewis CE, Sternfeld B. Do short spurts of physical activity benefit cardiovascular health? The CARDIA study. Med Sci Sports Exerc. 2015;47:2353–8. doi: 10.1249/MSS.0000000000000662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Antonogeorgos G, Panagiotakos DB, Pitsavos C, Papageorgiou C, Chrysohoou C, Papadimitriou GN, et al. Understanding the role of depression and anxiety on cardiovascular disease risk, using structural equation modeling; the mediating effect of the Mediterranean diet and physical activity: The ATTICA study. Ann Epidemiol. 2012;22:630–7. doi: 10.1016/j.annepidem.2012.06.103. [DOI] [PubMed] [Google Scholar]
- 28.Graham IM. The importance of total cardiovascular risk assessment in clinical practice. Eur J Gen Pract. 2006;12:148–55. doi: 10.1080/13814780600976282. [DOI] [PubMed] [Google Scholar]
- 29.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72. doi: 10.1002/sim.2929. [DOI] [PubMed] [Google Scholar]
- 30.Marrugat J, D’Agostino R, Sullivan L, Elosua R, Wilson P, Ordovas J, et al. An adaptation of the Framingham coronary heart disease risk function to European Mediterranean areas. J Epidemiol Community Health. 2003;57:634–8. doi: 10.1136/jech.57.8.634. [DOI] [PMC free article] [PubMed] [Google Scholar]


