Granulomatous mycosis fungoides (GMF) is an unusual histologic subtype of cutaneous T-cell lymphoma.1 The diagnosis of GMF is usually established after observation of a granulomatous inflammatory reaction associated with a malignant lymphoid infiltrate. Epidermotropism, a clue to diagnosis in classical mycosis fungoides (MF) may be absent in about 47% of cases of GMF.2 In some instances, the granulomatous component may be intense and obscures the lymphomatous component of the infiltrate.1 There are no distinctive clinical patterns associated with GMF.1, 3
Case report
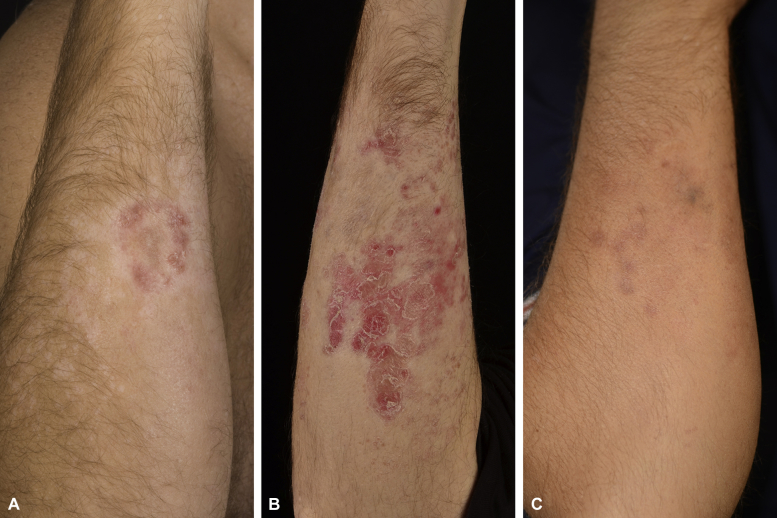
In 1998 a 28 year-old male patient presented with desquamating erythema on his left auricle (Fig 1, A). On exam he also had erythematous scaly plaques on his forearms and trunk associated with surrounding alopecia (Fig 2, A).
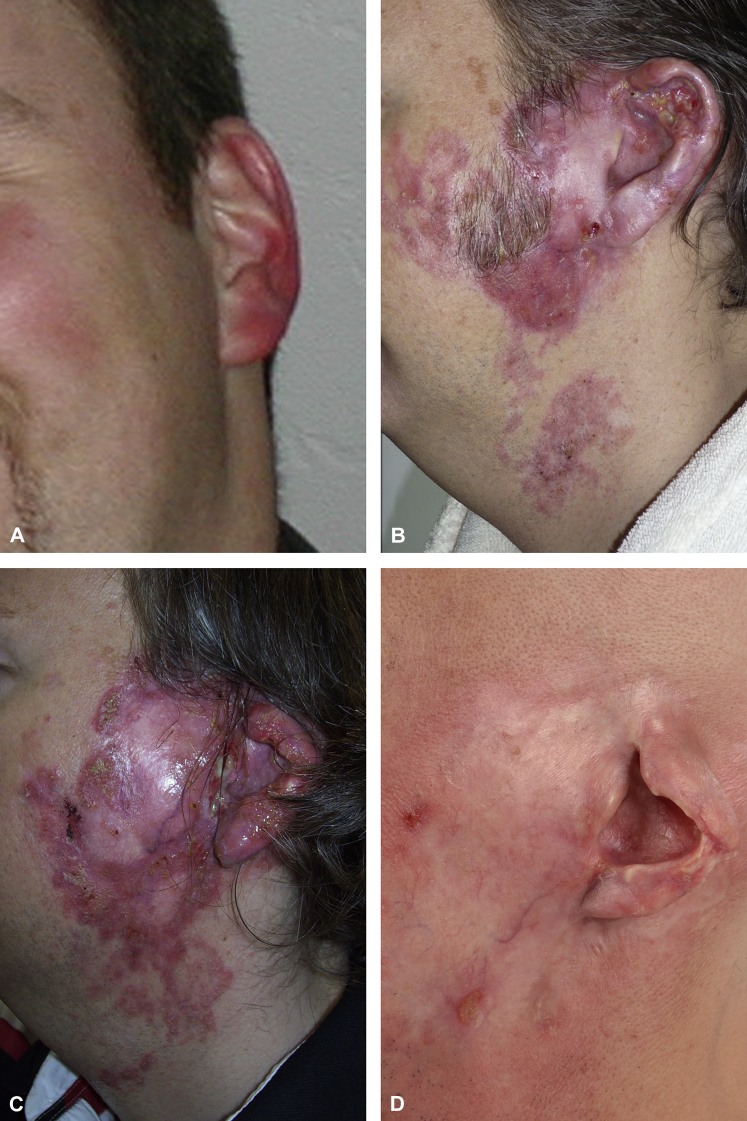
Fig 1.
Clinical presentation of the ear from 1998 until 2013. A, Erythema and desquamation of the left auricle (1998). B, Development of plaque formation and ulceration (2012). C, Erythematous, infiltrated plaque and purulent ulcerations, especially in the area of the tragus and helix leading to mutilation of the helix (March 2013). D, After soft x-ray therapy. Almost complete healing, leaving a scar plate and subtotal destruction of the helix (December 2013).
Fig 2.
Clinical presentation of the right forearm since 2007. A, Erythematous, alopecic scaly lesion (October 2011). B, Erythematous, scaly, psoriasiform lesions diffusely arranged on the forearm; alopecia within the lesions (February 2013). C, After cessation of therapy. Only discrete livid papules; alopecia within the lesion (August 2013).
Thirteen years later the now 44-year-old patient presented with painful ulcers on his left ear, which recently had started to expand. The ear and preauricular region appeared erythematous with profound purulent fistulas and tender ulcerations. The clinical findings were suggestive of an ulcerated basal cell carcinoma or lupus vulgaris (Fig 1, B). Previous use of antieczematous, antipsoriatic, and antifungal therapies with topical steroids, calcineurin inhibitors, antibiotics, and antiseptics and systemic and topical antifungals had not made any improvement. In one previous biopsy from the ear, Mycobacterium gordonae grew in a culture; however, polymerase chain reaction results were negative. The etiologic relevance was considered questionable, and the appropriate systemic antibiotic therapy did not show any effects.
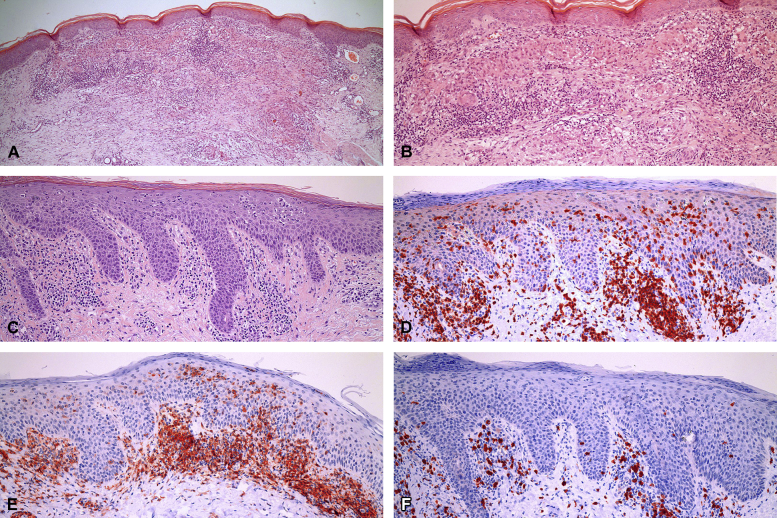
The histopathologic evaluation of biopsy specimens from the ear and forearm found a lymphohistiocytic, lichenoid inflammatory infiltrate with epitheloid giant cell granulomas (Fig 3, A and B). On the basis of the clinical findings of a chronic ulceration and histologic evidence of granulomas, we favored a disease induced by bacteria or intracellular parasites. However, the cultures were negative for mycobacteria and leishmania. Several dermatopathologists were consulted, and a germ-poor mycobacteriosis, pinta, and smoldering lymphoma were considered. However, the analysis of the T-cell receptor (TCR) gamma gene found a monoclonal amplification product on a polyclonal background.
Fig 3.
Histologic examination of the forearm biopsy. A and B, Lymphohistiocytic inflammatory infiltrate with formation of epitheloid giant cell granuloma. C-F, Lichenoid lymphohistiocytic inflammatory infiltrate, exocytosis of lymphocytes. (A-F, Hematoxylin-eosin stain; original magnifications: A, ×25; B-F, ×100. Immunohistochemistry: D, anti-CD3 staining in red; E, anti-CD4 staining in red; F, anti-CD8 staining in red.)
A swab of a preauricular fistula grew Pseudomonas aeruginosa and Staphylococcus aureus, which was positive for Panton-Valentine leukocidin . However, the appropriate systemic antibiotic therapy did not yield a therapeutic effect.
Lack of therapeutic success led the patient to consult with another dermatologic department, which favored the diagnosis of lupus vulgaris. Without microbiological evidence, systemic quadruple therapy with rifampicin, isoniazid, ethambutol, and pyrazinamide was prescribed without benefit.
In December 2012, the case was discussed with another dermatopathologist. In one edge of the lichenoid infiltrate, epidermotropism was detected, which led to the diagnosis of MF with an unusual granulomatous pattern.
New biopsy samples obtained in January 2013 from the forearm and ear now showed substantial exocytosis of lymphocytes. The subepithelial infiltrate was dominated by atypical lymphocytes with hyperchromatic nuclei. The TCR gene of both biopsies now showed a monoclonal rearrangement confirming the diagnosis of MF. A retrospective re-evaluation of our tissue obtained in 2011 (new recuts: Pautrier microabscess, Fig 3, C and epidermotropism of CD4-positive lymphocytes by only scattered CD8-positive T cells, Fig 3, D-F) confirmed the diagnosis of MF with severe granulomatous component.
For therapy, the patient received low-dose interferon alfa (INF-α) with 3 million international units subcutaneously 3 times a week and additional photochemotherapy starting in January 2013. The therapy with INF-α led to an improvement of the lesions; however, hematotoxicity (lymphocytes <1500 g/L) led to discontinuation of INF-α in November 2013. The consecutive therapy with bexarotene had to be stopped as well after 8 weeks because of leukopenia. Percutaneous fractional radiation treatment of the left face with a cumulative dose of 30 Gy was applied and resulted in complete remission of the ear tumor (Fig 1, D). Staging has not found any signs of systemic involvement to date.
Discussion
We report a case of GMF, a rare subtype of MF. The histologic diagnosis is usually difficult because of a predominantly granulomatous infiltrate with only little epidermotropism, which led us to favor an infectious disease. Clinically, the lesions did not present as typical MF with eczematous scaly digitated maculae/plaques on the trunk but rather inconspicuous erythema on the ear in the beginning and alopecia on the forearms. In addition to this unusual clinical presentation, the diagnosis of MF was also hampered by the peculiar clinical course with isolated progress of the lesion on the ear while the lesions on the arm remained in an eczematous stage. Not until the ear lesion progressed into the tumor stage did we favor MF over an infectious disease such as atypical mycobacteriosis.
Granulomatous infiltrates are an unusual phenomenon in cutaneous lesions of MF.1 The incidence is estimated in the literature to about 6.3% of cases.4 The degree of the associated histiocytic response may be variable. It has been postulated that by the diagnosis of granulomatous cutaneous lymphoma, the granulomatous component represents at least 25% of the infiltrate.2 The granuloma formation can be very extensive, and the findings are, as presented here, often initially misdiagnosed as granulomatous dermatitis.2
The granulomatous changes may precede, develop simultaneously, or develop after the signs of cutaneous lymphoma. The cutaneous granulomas have a mostly epitheloid appearance.1 The exact pathogenetic mechanism of granuloma formation in cutaneous lymphomas is unknown.1
There is no distinctive clinical pattern associated with the granulomatous variant of MF.1, 3 In contrast, granulomatous slack skin, a distinct subtype of MF, is characterized by a typical clinical picture with bulky skin folds.2 The interval from the onset of symptoms to diagnosis of GMF is estimated in the literature to about 8.4 years.4 The correct diagnosis is based on histopathologic features, immunohistochemistry, and TCR rearrangement.4, 5 According to recent studies, extracutaneous manifestations are more frequent in GMF and occur earlier than in classical MF. Five-year survival rate of GMF is 66% worse than that in classical MF.1
The therapy guidelines for GMF are similar to those of the classical MF.6 As in our patient, treatment with photochemotherapy, if necessary, in combination with INF-α, bexarotene, or radiation treatment can be applied. GMF is a rare form of MF, which is, as in this case, a challenge to diagnose.
Acknowledgments
The authors thank Heinz Kutzner (Germany), Dirk Elston (USA), and Josef Zelger (Austria) for their expert opinions. The authors thank Philip E. LeBoit (USA), clearly favoring MF in this case, and Peter von den Driesch (Germany) for finally confirming the diagnosis.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Gallardo F., Garcia-Muret M.P., Servitje O. Cutaneous lymphomas showing prominent granulomatous component: clinicopathological features in series of 16 cases. JEADV. 2009;23:639–647. doi: 10.1111/j.1468-3083.2008.03020.x. [DOI] [PubMed] [Google Scholar]
- 2.Kempf W., Ostheeren-Machaelis S., Paulli M. Granulomatous Mycosis fungoides and Granulomatous Slack Skin. A Multicenter study of the cutaneous lymphoma Histopathology Task Force Group of the European Organization for Research and Treatment of Cancer (EORTC) Arch Dermatol. 2008;144:1609–1617. doi: 10.1001/archdermatol.2008.46. [DOI] [PubMed] [Google Scholar]
- 3.Morihara K., Katoh N., Takenaka H. Granuloatous mycosis fungoides presenting as poikiloderma. Clin Exp Dermatlol. 2008;34:718–720. doi: 10.1111/j.1365-2230.2008.03013.x. [DOI] [PubMed] [Google Scholar]
- 4.Li J.Y., Pulitzer M.P., Myskowski P.L. A case-control study of clinocopathologic features, prognosis, and therapeutic responses in patients with granulomatous mycosis fungoides. J Am Acad Dermatol. 2013;69:366–374. doi: 10.1016/j.jaad.2013.03.036. [DOI] [PubMed] [Google Scholar]
- 5.Gutte R., Kharkar V., Mahajan S. Granulomatous mycosis fungoides with hypohidrosis mimicking lepromatous leprosy. Indian J Dermatol Venereol Leprol. 2010;76:686–690. doi: 10.4103/0378-6323.72470. [DOI] [PubMed] [Google Scholar]
- 6.Wollina U. Cutaneous T cell lymphoma: update on treatment. Int J Dermatol. 2012;51:1019–1036. doi: 10.1111/j.1365-4632.2011.05337.x. [DOI] [PubMed] [Google Scholar]