A verrucous epidermal nevus (VEN) is a skin disorder that commonly presents at birth and is frequently resistant to multiple treatment modalities.1 Physical therapeutic approaches have been used, but recurrences are common, and topical treatments seem to be ineffective.2 Here, we report a case of recalcitrant VEN successfully treated with photodynamic therapy (PDT) using indocyanine green (ICG).
Case report
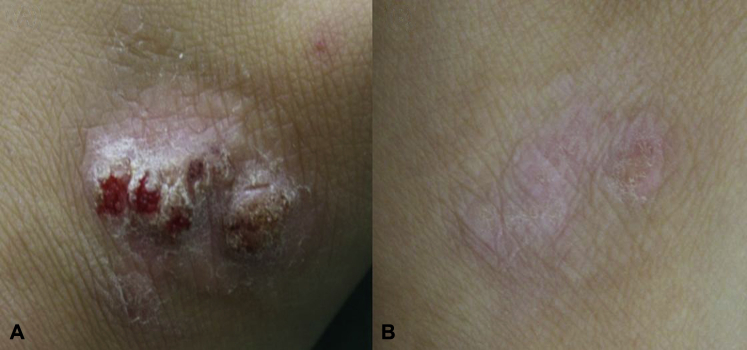
A 24-year-old woman visited our department with cutaneous lesions associated with intermittent severe pruritus. These lesions initially developed in early childhood on the back of her left hand. On physical examination, we observed a 5- × 4-cm erythematous verrucous plaque with scales and abrasions, likely a result of irritation, on the back of the left hand (Fig 1, A). A skin biopsy specimen of the lesion showed hyperkeratosis, papillomatosis, and acanthosis with elongation of the rete ridges. Perivascular inflammatory cells such as lymphocytes and histiocytes were observed in the dermis (Fig 2), with a negative result on human papillomavirus staining. The patient was diagnosed with an inflammatory VEN. She was treated with 3 sessions of carbon-dioxide (CO2) laser treatment and topical calcipotriol 0.005% plus betamethasone propionate for 3 months. The Sharplan 20 C (Laser Industries, Tel Aviv, Israel) was used for CO2 laser in super pulse and continuous cutting modes, set to a wavelength of 10,600 nm, 1-mm spot, and power output of 1 to 2 W. CO2 laser treatments resulted in a temporary volume decrease, but inflammatory reactions with severe itching were observed, and there was recurrence a few months later. Considering the size of the lesion and scar formation after treatments, we attempted management with trichloroethane, 5-fluorouracil, bleomycin, and cryotherapy. These regimens led to a poor response with a volume decrease of only 10% to 20%. Therefore, PDT was initiated: 25 mg of ICG was applied in a 1-mm-thick layer with a 5-mm margin of normal appearing skin. Pretreatment with superficial CO2 ablation was performed to smooth the verrucous lesion. Ablation was achieved using a defocused 1-mm beam and a low power output of 0.5 W with rapid side-to-side hand movements. The ICG-treated area was covered with an occlusive polyurethane film for 1 hour. The lesion was then treated with 2 passes of intense pulsed light (IPL) (CIPL P-NAIN System, Jeisys Medical Inc, Tokyo, Japan). The parameters were wavelength of 550 to 800 nm, fluence of 23 J/cm2, and 171 pulses in 12 milliseconds per shot. The patient reported mild pain and itching during treatment without any severe side effects. After 6 treatment sessions over 11 months, the cosmetic and clinical responses were excellent, and the patient was very satisfied (Fig 1, B). After 2 years of follow-up, no recurrence has been observed.
Fig 1.
A, A 5- × 4-cm erythematous verrucous plaque with scales and abrasions on the back of the patient's left hand. B, After 6 treatment sessions in 11 months, the cosmetic and clinical response was excellent.
Fig 2.
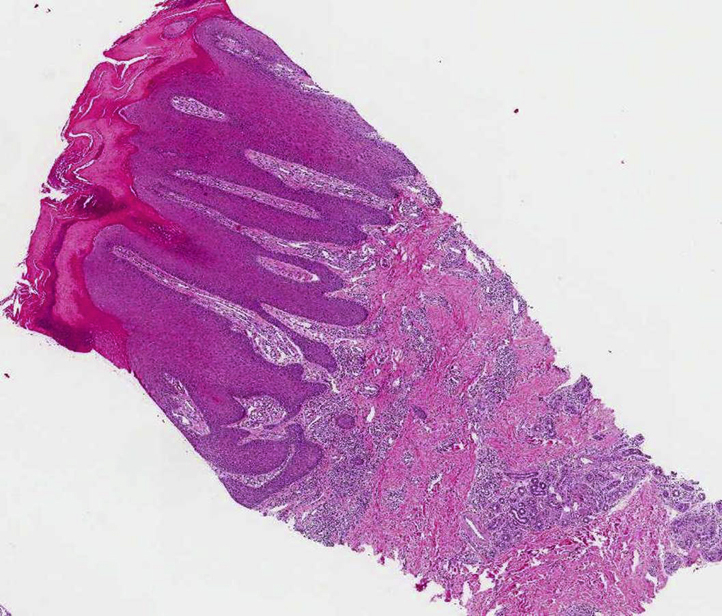
Skin biopsy specimen from a skin lesion showed hyperkeratosis, papillomatosis, and acanthosis with elongation of the rete ridges and perivascular inflammatory cells in the dermis. (Hematoxylin-eosin stain; original magnification: ×40.)
Discussion
Epidermal nevi are a hamartomas of the skin and have multiple clinical variants including a verrucous type. A VEN consists of hyperplasia of the epidermis and typically appears as verrucous papules or well-demarcated papillomatous plaques that are skin-colored to brown. These tumors can be located anywhere, including the head, trunk, or extremities.3 The lesions on our patient appeared on an exposed area, leading to cosmetic problems associated with a reduced quality of life. A VEN usually has a poor response to many different treatment modalities; surgical excision has to date been the most reliable treatment. However, surgical excision might not be possible when a skin lesion is very extensive, and it might cause scarring. Many other treatment modalities have been reported, including topical agents, cryotherapy, lasers, electrofulguration, and chemical peels, with various clinical outcomes.1, 2 In this case, the patient refused surgical excision because of concerns of postoperative scarring. Combined treatment with trichloroethane, 5-fluorouracil, bleomycin, and cryotherapy produced a poor response. Given the patient's financial concerns, we chose the least expensive photosensitizing agent, ICG, for PDT.
ICG has a known phototoxic effect in HaCaT cells,4, 5 which is a spontaneously transformed aneuploid immortal keratinocyte cell line originating from adult human skin. Based on the patient's histologic finding of epidermal hyperplasia, we assumed that PDT using ICG would irradiate the proliferating keratinocytes in the VEN. The epidermal nevus did not have the factors that could intrinsically respond to IPL alone (eg, excessive vascularity, melanin, or hair components). Even though the absorption peak of ICG was observed at 780 nm, there was spectral absorption between 600 to 800 nm. In addition, we used a wavelength range of 550 to 800 nm for IPL to achieve the best effects of photoactivation. Thus, IPL activated ICG at a range of wavelengths surrounding the absorption peak.
PDT is primarily used for treatment of several cutaneous nonmelanoma cancers. It is now being increasingly used for treatment of a variety of other skin diseases. Topical PDT has been used in inflammatory dermatoses including psoriasis, lichen sclerosus, and cutaneous sarcoidosis, with good response.6, 7, 8 ICG is a water-soluble tricarbocyanine dye with a peak spectral absorption at 780 nm, and its intravenous application has been Food and Drug Administration–approved since 1959 for determination of cardiac output, liver function diagnostics, and ophthalmic angiography. There are various reports on the use of ICG in the dermatologic field for treatment of mild to moderate acne, augmentation of the therapeutic effect of diode lasers in port-wine stains, and PDT of actinic keratosis. Compared with conventional photosensitizers, such as aminolevulinic acid and methylaminolevulinic acid, ICG is considered a good alternative material with minimal side effects and fair therapeutic efficacy.9, 10
Based on the presented case, PDT using ICG has substantial advantages in treating a VEN. It is less painful, leads to less scarring, and can be used to treat widespread areas relatively inexpensively. In addition, photoprotection with ICG is not necessary as its spectral absorption is in the near-infrared range. Treatment with PDT using ICG produced similar results to 2 previous case reports, in which verrucous epidermal nevi were treated with PDT using methylaminolevulinic acid.1, 2 PDT may be shown to be a useful tool to treat verrucous epidermal nevi. To date, there have been no reports of VEN successfully treated with PDT using ICG, and further controlled studies with a large number of patients and long-term follow-up are needed.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Sim J.H., Kang Y., Kim Y.C. Verrucous epidermal nevus successfully treated with photodynamic therapy. Eur J Dermatol. 2010;20:814–815. doi: 10.1684/ejd.2010.1092. [DOI] [PubMed] [Google Scholar]
- 2.Parera E., Gallardo F., Toll A., Gil I., Sanchez-Schmidt J., Pujol R. Inflammatory linear verrucous epidermal nevus successfully treated with methyl-aminolevulinate photodynamic therapy. Dermatol Surg. 2010;36:253–256. doi: 10.1111/j.1524-4725.2009.01401.x. [DOI] [PubMed] [Google Scholar]
- 3.Ho V.C.Y. Benign epithelial tumors. In: Freedberg I.M., Eizen A.Z., Wolff K., editors. Fitzpatrick's dermatology in general medicine. 5th ed. McGraw-Hill; New York: 1999. pp. 873–890. [Google Scholar]
- 4.Fickweiler S., Szeimies R.M., Bquumler W. Indocyanine green: intracellular uptake and phototherapeutic effects in vitro. J Photochem Photobiol B. 1997;38:178–183. doi: 10.1016/s1011-1344(96)07453-2. [DOI] [PubMed] [Google Scholar]
- 5.Abels C., Fickweiler S., Weiderer P. Indocyanine green and laser irradiation induce photooxidation. Arch Dermatol Res. 2000;292:404–411. doi: 10.1007/s004030000147. [DOI] [PubMed] [Google Scholar]
- 6.Radakovic-Fijan S., Blecha-Thalhammer U., Schleyer V. Topical aminolevulinic acid-based photodynamic therapy as a treatment option for psoriasis? Results of a randomized, observer blinded study. Br J Dermatol. 2005;152:279–283. doi: 10.1111/j.1365-2133.2004.06363.x. [DOI] [PubMed] [Google Scholar]
- 7.Biniszkiewicz T., Olejek A., Kozak-Darmas I. Therapeutic effects of 5-ALA-induced photodynamic therapy in vulvar lichen sclerosus. Photodiag Photodyn Ther. 2005;2:157–160. doi: 10.1016/S1572-1000(05)00062-1. [DOI] [PubMed] [Google Scholar]
- 8.Karrer S., Abels C., Wimmershoff M.B. Successful treatment of cutaneous sarcoidosis using topical photodynamic therapy. Arch Dermatol. 2002;138:581–584. doi: 10.1001/archderm.138.5.581. [DOI] [PubMed] [Google Scholar]
- 9.Jang M.S., Doh K.S., Kang J.S., Jeon Y.S., Suh K.S., Kim S.T. A comparative split-face study of photodynamic therapy with indocyanine green and indole-3-acetic acid for the treatment of acne vulgaris. Br J Dermatol. 2011;165:1095–1100. doi: 10.1111/j.1365-2133.2011.10472.x. [DOI] [PubMed] [Google Scholar]
- 10.Klein A., Szeimies R.M., Bäumler W. Indocyanine green-augmented diode laser treatment of port-wine stains: clinical and histological evidence for a new treatment option from a randomized controlled trial. Br J Dermatol. 2012;167:333–342. doi: 10.1111/j.1365-2133.2012.10950.x. [DOI] [PubMed] [Google Scholar]