Abstract
Objective
To determine the incidence of cardiopulmonary resuscitation (CPR) in pediatric intensive care units (PICU) and subsequent outcomes.
Design, Setting, and Patients
Multi-center prospective observational study of children 30 minutes, p30 minutes of CPR.
Conclusions
These data establish that contemporary PICU CPR, including long durations of CPR, results in high rates of survival to hospital discharge (45%) and favorable neurologic outcomes among survivors (89%). Rates of survival with favorable neurologic outcomes were similar among cardiac and non-cardiac patients. The rigorous prospective, observational study design avoided the limitations of missing data and potential selection biases inherent in registry and administrative data.
Keywords: cardiopulmonary resuscitation (CPR), cardiac arrest, intensive care, children, Incidence, survival
INTRODUCTION
Based on registry and administrative data, more than 6,000 children in the United States receive in-hospital cardiopulmonary resuscitation (CPR) each year, mostly in pediatric intensive care units (PICUs).1,2 In a prospective study from the early 1990s, CPR was provided for 1.8% of 11,165 admissions at 32 North American multi-disciplinary pediatric ICUs, and 13.7% survived to hospital discharge.3 More recent data from three single-center pediatric cardiac intensive care unit studies demonstrate cardiac arrests in 3 – 6% of children admitted, suggesting a higher incidence in this population.4–6 Although there have been many changes in critical care and increased focus on CPR quality since the 1990’s, the current incidence and outcome from CPR in pediatric ICUs is not known.
Published outcomes from CPR in PICUs vary.7 Although the survival rate following PICU CPR was 13.7% in the 1990s,3 more recent PICU CPR data from the American Heart Association’s Get With The Guidelines-Resuscitation (GWTG-R) in-hospital cardiac arrest registry found that 22% of children survived to hospital discharge.8 In contrast, a single center pediatric cardiac ICU study in an overlapping time period reported a survival rate of 46%, suggesting that post-CPR outcomes may be better among children with cardiac disease.4 Similarly, Get With The Guidelines-Resuscitation registry data suggest that cardiac arrest outcomes are superior among the children post-cardiac surgery compared with others.9
Much of the published PICU CPR outcome data are based on registry or administrative databases which are limited by challenges of missing neurologic outcome data and potential patient enrollment ascertainment bias. The Eunice Shriver Kennedy National Institute of Child Health and Human Development’s Collaborative Pediatric Critical Care Research Network (CPCCRN) embarked on an intensive prospective study of more than 10,000 admissions to its large academic PICUs with the primary aim to investigate the relationship of physiological instability to the development of morbidity and mortality.10 As part of this effort, we prospectively evaluated the incidence and outcomes of PICU CPR events to accurately determine the current overall incidence of CPR occurring in the PICU, the characteristics of children who received CPR in the PICU, their survival rates, and the neurologic and functional outcomes of the survivors. We also sought to determine if incidences and outcomes vary between cardiac and non-cardiac critically ill children. We hypothesized that CPR events would be more common among children with medical or surgical cardiac disease than those with medical or surgical non-cardiac disease, and that outcomes would be better for those cardiac patients.
METHODS
The current investigation was performed at the seven sites participating in the CPCCRN during the study period. These sites combined have approximately 17,000 PICU admissions per year. The details of patient selection and data collection have been previously published.10, 11 Patients ranging in ages from newborn to less than 18 years were randomly selected from both the General/Medical PICUs and the Cardiac/Cardiovascular PICUs. There were no separate general surgical or neurological PICUs. Only the first PICU admission was included, and patients were excluded if their vital signs were incompatible with life for at least the first 2 hours after PICU admission (i.e., moribund patients). Patients were enrolled from December 4, 2011 to April 7, 2013. The protocol was approved by the Institutional Review Boards at all participating institutions.
A CPR event was defined as chest compressions for ≥ 1 minute and/or defibrillation. The reasons for initiation of chest compressions were categorized as a pulseless cardiac arrest or poor perfusion with bradycardia and/or hypotension, as per American Heart Association Guidelines.12 Immediate outcomes from the CPR event were categorized as: return of spontaneous circulation (ROSC) for >20 minutes, return of circulation (ROC) by extracorporeal life support (ECLS), or no return of circulation.12,13 Survival to hospital discharge was reported for the index (or first) CPR event of each patient because a patient can only survive to discharge once per hospitalization.13
Diagnostic, demographic and functional status data, including Pediatric Cerebral Performance Category (PCPC) and Functional Status Scale (FSS) scores, were determined at PICU admission. The functional status evaluation included documentation of pre-illness baseline status (i.e., prior to the event that brought the child to the hospital), and later determination at PICU discharge and hospital discharge.10,11,13,14 Diagnoses were classified by the system of dysfunction accounting for the primary reason for PICU admission. Operative status included both operating room and interventional catheterization procedures, but not diagnostic catheterization procedures. Patients were classified as surgical or medical based on operative status prior to the CPR event, and then further classified into four sub-groups based on acute admission diagnoses and operative type: cardiac surgical, cardiac medical, non-cardiac surgical, non-cardiac medical. Physiological status was assessed with the Pediatric Risk of Mortality (PRISM) III score with a shortened observation time period.10 Investigators, research coordinators, and research assistants were trained in data collection with in-person training on multiple occasions; bi-weekly teleconference calls were also conducted.10, 11
Functional status was assessed by the Pediatric Cerebral Performance Category (PCPC) and Functional Status Scale (FSS) scores. The FSS was developed to provide assessment of functional status suitable for large studies. It is composed of 6 domains (mental status, sensory, communication, motor function, feeding, and respiratory) with domain scores ranging from 1 (normal) to 5 (very severe dysfunction). Therefore, total scores may range from 6 to 30 with lower scores indicating better function. The operational definitions and manual for the classifications have been published.14 The FSS validation consisted of comparison to the Adaptive Behavioral Assessment Scale II (ABAS II), a validated measure of pediatric adaptive behavior, and comparison to the Pediatric Cerebral Performance Category Scale (PCPC).10,14,15 A PCPC score of 1 describes children with normal age-appropriate neurodevelopmental functioning; 2 for mild cerebral disability; 3 for moderate disability; 4 for severe disability; 5 for coma/vegetative state; and 6 for brain death. As previously reported, favorable neurologic outcome was defined as a PCPC score of 1–3 at discharge or no increase compared to admission PCPC status.1,8,9,16,17 In addition, we categorized FSS scores of 6–7 as good, 8–9 as mildly abnormal, 10 – 15 as moderately abnormal, 16 – 21 as severely abnormal, and > 21 as very severely abnormal.10.11,14 These category ranges were chosen based on the dysfunction reflected in the score. This categorization was designed such that the equivalent FSS groups would approximately correspond to the PCPC categories.9,13,14 Newborns who had never achieved a stable baseline function were assigned an FSS = 6; this was operationalized by assigning a baseline FSS score of 6 to all admissions for infants 0–2 days of age and to transfers from another facility for infants 3–6 days of age.10,15 As previously reported, new morbidity was defined as an increase in the FSS total score ≥3.10
The primary study outcomes were the rate of CPR events and survival to hospital discharge with favorable neurologic outcomes. Secondary outcomes included return of circulation for >20 minutes, 24-hour survival, survival to hospital discharge, and survival without new morbidities.
All descriptive and inferential analyses are based on the index (i.e., first) qualifying CPR event. Categorical data are expressed as counts and percentages or rate per 100 admissions. Continuous data are expressed as median and interquartile range (IQR, 25th and 75th percentiles). Associations of patient and event characteristics with patient type were assessed using the Pearson chi-square or Fisher’s exact test for categorical variables and the Wilcoxon rank-sum test for continuous variables. Observed associations between duration of compressions and outcome were evaluated using the Cochran-Armitage trend test. Univariable associations of other key patient and event characteristics with outcome were evaluated using modified Poisson regression, a method that implements generalized estimating equations to facilitate direct estimation of rate ratios with robust variance estimates.18 Differences between cardiac and non-cardiac subgroups were further evaluated in a multivariable model. This model adjusted for patient age and whether compressions were started for poor perfusion or pulselessness, factors determined a priori to be potential covariates. Additionally, any variables with p < 0.15 in univariable analyses were included in the final model. Relative risks and associated 95% confidence intervals are reported. Analyses were performed in SAS® version 9.4 (SAS Institute, Cary, NC).
RESULTS
Enrollment at each of the seven CPCCRN sites varied from 1252 (12%) to 1617 (16%) of the 10,078 admissions in the overall study. The PICU mortality rate for these 10,078 admissions was 2.3% (227 PICU deaths) and overall hospital mortality rate was 2.7% (275 hospital deaths). A total of 139 (1.4%) received CPR for ≥ 1 minute and/or defibrillation within the initial PICU admission (Figure). Only 4 had defibrillation without chest compressions. Twenty-eight (20%) of these children received CPR on multiple occasions for a total of 182 CPR events (1.8 CPR events/100 admissions). Demographic and event data are displayed in Tables 1 and 2. The seven CPCCRN sites each contributed anywhere from 8 (6%) to 30 (22%) of the 139 children with CPR events. The incidence of index CPR events (i.e., number of index CPR events per 100 ICU admissions) ranged across sites from 0.6 to 2.3 per 100 admissions (p < 0.001). Among the 139 children with a CPR event, 31 (22%) failed to attain return of circulation during the initial CPR event, 91 (65%) attained return of spontaneous circulation for >20 minutes, and 17 (12%) attained return of circulation via ECLS instituted during CPR.
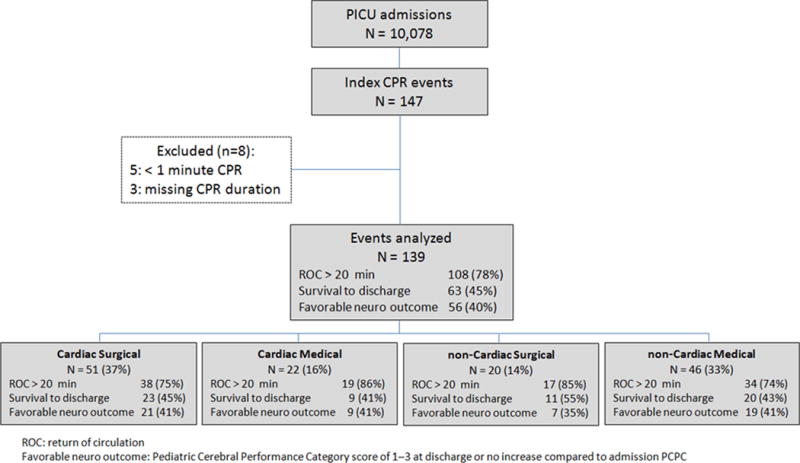
Flow diagram of patients evaluated, CPR events, overall outcomes, and outcomes among major sub-groups.
Table 1.
Patient characteristics
| Parameter | Overall N = 139 |
Cardiac N = 73 |
non-Cardiac N = 66 |
P-valuea |
|---|---|---|---|---|
| Female | 69 (50%) | 36 (49%) | 33 (50%) | 0.94 |
| Age at time of CPR event | < 0.001 | |||
| < 1 mo | 24 (17%) | 22 (30%) | 2 (3%) | |
| 1 mo – < 1 yr | 58 (42%) | 33 (45%) | 25 (38%) | |
| 1 yr – < 8 yrs | 36 (26%) | 10 (14%) | 26 (39%) | |
| 8 yrs – < 18 yrs | 21 (15%) | 8 (11%) | 13 (20%) | |
| Race | 0.49 | |||
| Black or African American | 34 (24%) | 15 (21%) | 19 (29%) | |
| White | 56 (40%) | 31 (42%) | 25 (38%) | |
| Other | 10 (7%) | 4 (5%) | 6 (9%) | |
| Unknown or Not Reported | 39 (28%) | 23 (32%) | 16 (24%) | |
| Ethnicity | 0.92 | |||
| Hispanic or Latino | 25 (18%) | 13 (18%) | 12 (18%) | |
| Not Hispanic or Latino | 76 (55%) | 39 (53%) | 37 (56%) | |
| Unknown or Not Reported | 38 (27%) | 21 (29%) | 17 (26%) | |
| Payer | 0.23 | |||
| Commercial | 47 (34%) | 24 (33%) | 23 (35%) | |
| Government | 79 (57%) | 39 (53%) | 40 (61%) | |
| Other | 5 (4%) | 3 (4%) | 2 (3%) | |
| Unknown | 8 (6%) | 7 (10%) | 1 (2%) | |
| Baseline FSS Score | 0.04 | |||
| Good (6–7) | 93 (67%) | 54 (74%) | 39 (59%) | |
| Mild (8–9) | 21 (15%) | 12 (16%) | 9 (14%) | |
| Moderate (10–15) | 20 (14%) | 6 (8%) | 14 (21%) | |
| Severe (16–21) | 2 (1%) | 1 (1%) | 1 (2%) | |
| Very Severe (>21) | 3 (2%) | 0 (0%) | 3 (5%) | |
| Baseline PCPC | 0.16 | |||
| 1 – Normal | 87 (63%) | 48 (66%) | 39 (59%) | |
| 2 – Mild disability | 30 (22%) | 17 (23%) | 13 (20%) | |
| 3 – Moderate disability | 12 (9%) | 3 (4%) | 9 (14%) | |
| 4 – Severe disability | 8 (6%) | 3 (4%) | 5 (8%) | |
| 5 – Coma/vegetative | 2 (1%) | 2 (3%) | 0 (0%) | |
| Primary Disorder for ICU Admission | <0.001b | |||
| Respiratory | 41 (29%) | 11 (15%) | 30 (45%) | |
| Cancer | 3 (2%) | 0 (0%) | 3 (5%) | |
| Cardiovascular Disease – Acquiredc | 21 (15%) | 9 (12%) | 12 (18%) | |
| Cardiovascular Disease – Congenital | 53 (38%) | 52 (71%) | 1 (2%) | |
| Gastrointestinal disorder | 5 (4%) | 0 (0%) | 5 (8%) | |
| Hematologic disorder | 1 (1%) | 0 (0%) | 1 (2%) | |
| Musculoskeletal Condition | 1 (1%) | 0 (0%) | 1 (2%) | |
| Neurologic | 8 (6%) | 0 (0%) | 8 (12%) | |
| Renal | 1 (1%) | 0 (0%) | 1 (2%) | |
| Miscellaneous | 5 (4%) | 1 (1%) | 4 (6%) | |
| PRISM-III, median (interquartile range) | 8 (3, 15) | 8 (3, 12) | 8 (3, 17) | 0.50 |
P-value reflects the Wilcoxon rank-sum test for association between PRISM-III and cardiac vs. non-cardiac patient type and the Chi-square or Fisher’s exact test for all other variables.
All primary disorders with overall count ≤ 5 were combined with Miscellaneous prior to p-value calculation.
Cardiovascular Disease – Acquired includes septic shock, systemic inflammatory response syndrome (SIRS) and post-cardiac arrest syndrome.
Table 2.
Event characteristics
| Parameter | Overall N = 139 |
Cardiac N = 73 |
non-Cardiac N = 66 |
P-valuea |
|---|---|---|---|---|
| CPR performed | 0.03 | |||
| Chest compressions only | 122 (88%) | 60 (82%) | 62 (94%) | |
| Defibrillation only | 4 (3%) | 2 (3%) | 2 (3%) | |
| Chest compressions and defibrillation | 13 (9%) | 11 (15%) | 2 (3%) | |
| Reason chest compressions started | 0.33 | |||
| Poor perfusion (i.e. bradycardia, hypotension) | 90 (67%) | 50 (70%) | 40 (63%) | |
| Pulselessness | 45 (33%) | 21 (30%) | 24 (38%) | |
| CPR performed open or closed chest | < 0.001 | |||
| Open chest | 21 (16%) | 20 (28%) | 1 (2%) | |
| Closed chest | 114 (84%) | 51 (72%) | 63 (98%) | |
| Chest compression duration (minutes) | 0.03 | |||
| 1–3 minutes | 44 (33%) | 18 (25%) | 26 (41%) | |
| 4–9 minutes | 26 (19%) | 12 (17%) | 14 (22%) | |
| 10–30 minutes | 33 (24%) | 17 (24%) | 16 (25%) | |
| >30 minutes | 32 (24%) | 24 (34%) | 8 (13%) | |
| Time from PICU admission to index CPR event | 0.25 | |||
| <1 hour | 9 (6%) | 4 (5%) | 5 (8%) | |
| 1 – <6 hours | 17 (12%) | 5 (7%) | 12 (18%) | |
| 6 – <24 hours | 21 (15%) | 11 (15%) | 10 (15%) | |
| 24 hours – <1 week | 50 (36%) | 27 (37%) | 23 (35%) | |
| 1 week or more | 42 (30%) | 26 (36%) | 16 (24%) |
P-value reflects the Wilcoxon rank-sum test for association between PRISM-III and cardiac vs. non-cardiac patient type and the Chi-square or Fisher’s exact test for all other variables.
Following their 139 index CPR events, 89 (64%) children survived for 24 hours, 64 (46%) survived to PICU discharge, 63 (45%) survived to hospital discharge, and 56 (40%) survived to hospital discharge with a favorable neurologic outcome (Table 3). Importantly, 56/63 (89%) of the survivors had favorable neurologic status at hospital discharge, and 48/63 (76%) had PCPC of 1 or no change from baseline. Notably, 35/63 (56%) had discharge PCPC of 1, 13 (21%) had a discharge PCPC of 2, and five (8%) had a PCPC of 3. Ten (16%) survivors were severely disabled or in a vegetative state at hospital discharge, but three of these had no change from the baseline PCPC. Only four (6%) of the survivors had a change in PCPC of 2 categories or more. Among the 63 who survived to hospital discharge, 46 (73%) had no new morbidities, as defined by an FSS increase ≥3,10 whereas 17 (27%) had an FSS increase ≥3. The median change in FSS scores was 1 (IQR 0, 3), and 26/63 (41%) had no change or slight improvement in FSS from baseline.
Table 3.
Outcomes
| Parameter | Overall N = 139 |
Cardiac N = 73 |
non-Cardiac N = 66 |
Relative risk (95% CI)a |
|---|---|---|---|---|
| Return of circulation achieved | 108 (78%) | 57 (78%) | 51 (77%) | 0.89 (0.74, 1.08) |
| Alive 24 hours following first event | 89 (64%) | 50 (68%) | 39 (59%) | 1.00 (0.76, 1.32) |
| Alive at the time of hospital discharge | 63 (45%) | 32 (44%) | 31 (47%) | 0.84 (0.57, 1.24) |
| Favorable neurologic outcome at hospital discharge (PCPC 1–3 or no change) | 56 (40%) | 30 (41%) | 26 (39%) | 0.91 (0.60, 1.38) |
Relative risk and 95% confidence interval (CI) based on modified Poisson regression model (n=135) with adjustment for patient age, PRISM-III score, time from PICU admission to index CPR event, and whether compressions started for poor perfusion or pulselessness. The four patients who had defibrillation without chest compressions were excluded from the relative risk model because of variables that are only applicable to patients with chest compressions.
Seventy three (53%) children with ICU CPR were cardiac patients (51 surgical/22 medical), and 66 (47%) were non-cardiac (20 surgical/46 medical). Twenty one had open-chest CPR, of whom 19 were cardiac surgical patients, one was a cardiac medical patient and one a non-cardiac surgical patient. Based on disease classification at PICU admission, the cardiac group had a higher incidence of index CPR events than the non-cardiac group (3.4% versus 0.8%, p<0.001). However, among those with a CPR event, there were no apparent differences in survival to hospital discharge or survival with a favorable neurologic outcome between the cardiac and non-cardiac groups (Table 3, Appendix Table 1).
The median duration of the initial CPR event was 9 minutes (IQR 3, 30) for the 135 CPR events with chest compressions ≥1 minute (range: 1–122 minutes). Among the 90 patients receiving CPR for poor perfusion with bradycardia and/or hypotension, the median duration of the initial CPR event was 8 minutes (IQR 3, 30); 17 (19%) did not attain return of circulation, 61 (68%) attained return of spontaneous circulation for >20 minutes, and 12 (13%) had return of circulation by ECLS during CPR. Among the 45 patients receiving CPR for pulselessness, the median duration of the initial CPR event was 14 minutes (IQR 3, 28); 14 (31%) did not attain return of circulation, 28 (62%) attained return of spontaneous circulation for >20 minutes, and 3 (7%) had return of circulation via ECLS during CPR.
Shorter duration CPR was associated with higher survival rates (Table 4). Among the 44 children with CPR for 1–3 minutes (12 cardiac surgical, 6 cardiac medical, 6 non-cardiac surgical, 20 non-cardiac medical), only one failed to attain ROC (because of withdrawal of technological support), 41 had ROSC, 2 had ROC via ECLS, and 29/44 (66%) survived to hospital discharge. In contrast, among 32 children with CPR >30 minutes, 14 (44%) failed to attain ROC, 9 (28%) had ROSC, 9 (28%) had ROC via ECLS, and only 9/32 (28%) survived to hospital discharge. However, the duration of CPR was not associated with favorable neurologic outcomes for children who survived to hospital discharge. Among the 29 survivors with 1–3 minutes of CPR, 26 (90%) had a favorable neurologic outcome. Similarly, 8/9 (89%) children who survived after >30 minutes of CPR had a favorable neurologic outcome.
Table 4.
Outcomes by duration of chest compressions
| Parameter | 1–3 minutes N = 44 |
4–9 minutes N = 26 |
10–30 minutes N = 33 |
>30 minutes N = 32 |
P-valuea |
|---|---|---|---|---|---|
| Return of circulation achieved | 43 (98%) | 23 (88%) | 20 (61%) | 18 (56%) | <0.001 |
| Alive 24 hours following first event | 39 (89%) | 19 (73%) | 14 (42%) | 14 (44%) | <0.001 |
| Alive at the time of hospital discharge | 29 (66%) | 12 (46%) | 11 (33%) | 9 (28%) | <0.001 |
| Favorable neurologic outcome at hospital discharge (PCPC 1–3 or no change) | 26 (59%) | 10 (38%) | 10 (30%) | 8 (25%) | 0.001 |
P-value reflects Cochran-Armitage trend test for differences in outcome relative to categorized length of CPR.
The four patients who had defibrillation without chest compressions could not be included in this Table.
Among the 139 children with a CPR event, six (4%) had a cardiac arrest prior to hospital admission and another four (3%) had an in-hospital cardiac arrest prior to PICU admission. Of these 10 patients with CPR events prior to the ICU admission, 4 (40%) survived to hospital discharge, and all four had favorable neurologic outcomes with PCPC 1 at discharge or no change from admission.
Seventy-six patients died prior to hospital discharge; 48 (63%) did not attain ROC during a resuscitation event (the initial resuscitation or a subsequent resuscitation), 23 (30%) had withdrawal of technological support, 3 (4%) had limitation of technological support, and 2 (3%) were declared dead by absence of brain function. Among the 23 patients with withdrawal of technological support, 17 (77%) had withdrawal of mechanical ventilation, 10 (45%) withdrawal of ECMO, 12 (55%) withdrawal of vasoactive medications, 3 (14%) withdrawal of renal replacement therapy, and 2 (9%) withdrawal of cardiac compressions during CPR.
Twenty eight children had multiple CPR events during their initial PICU admission; 20 with only one additional CPR event and 8 with more than one additional CPR event (Appendix Table 2). Of these 28 children, 13 (46%) attained ROC in a subsequent CPR event, and only 7 (25%) survived to hospital discharge (Appendix Table 3). Among the 7 survivors, 6 survived to hospital discharge with PCPC of 1 or no change from baseline and the other with PCPC 2. Subsequent CPR events were not more common after ROC from an initial CPR event >30 minutes versus ROC from an initial CPR event ≤30 minutes (5/18 [28%] versus 23/86 [27%], p=1.0).
DISCUSSION
In this prospective study of more than 10,000 pediatric admissions to these large academic PICUs, 139 children received one minute or more of chest compressions and/or defibrillation in the PICU, an incidence of 1.4%. Among these children, 78% attained return of circulation during their initial CPR event, 45% survived to hospital discharge, and 89% of the survivors had a favorable neurologic outcome; 73% survived without new morbidities. Consistent with previous single center studies,3–6 the relative incidence of CPR events in our multicenter study was higher for cardiac patients compared with non-cardiac patients (3.4% versus 0.8%). In contrast to previous single center study data and multi-center registry data,4–9 the survival and neurologic outcomes did not differ between the cardiac and non-cardiac patients. Although the likelihood of survival decreased with increased duration of CPR, there was no demonstrable difference in neurologic outcome or new morbidities among those who survived after longer durations of CPR.
Pediatric and adult studies suggest that rapid response teams have successfully decreased the number of cardiac arrests in wards and increased the proportion in ICUs.1,19 For example, over the last decade, more than 93% of pediatric ICU and ward CPR events in the United States occurred in a PICU.1 However, rapid increases in the size and number of PICUs over the last 2–3 decades might have resulted in a lower incidence of PICU CPR events.20 Nevertheless, the 1.4% incidence of PICU CPR events among PICU admissions in the current study is similar to the 1.8% incidence in 32 North American PICUs in the early1990s.3
Although our data suggest that the incidence of PICU CPR events has not changed much over the last 20 years, the outcomes are now substantially better. Only 13.7% of patients with an PICU CPR event survived to discharge in the early 1990s.3 In contrast, 45% of the contemporary CPCCRN patient cohort with PICU CPR events from 2011–2013 survived to hospital discharge, and 89% of the survivors had favorable neurological outcomes. The reasons for these improved outcomes are not certain. All of the CPCCRN PICU sites had 24/7 in-house call with critical care attendings and/or fellows in 2011–2013 in contrast to the rarity of attending and/or fellow in-house call in the early 1990s, and this higher level of in-hospital expertise has been associated with improved patient care.21 Perhaps a resurgence in focus on CPR quality, PICU CPR training, and CPR implementation science has translated into superior outcomes.1,7–9,12 All of these PICU sites participate in the multi-center Therapeutic Hypothermia After Pediatric Cardiac Arrest (THAPCA) trial.22 Therefore, it is plausible that the better outcomes are in part due to improvements in CPR and post-cardiac arrest care among providers who know that they are being monitored as part of that trial (the Hawthorne effect). Notably, Get With The Guidelines-Resuscitation registry data have also demonstrated that outcomes from pediatric in-hospital cardiac arrests (ICU plus non-ICU) have improved over the last decade.23
In this study, we defined favorable neurologic outcomes as PCPC scores at hospital discharge of 1–3 or no change compared with baseline, consistent with other pediatric cardiac arrest/CPR investigations.1,8,9,16,17 Favorable neurologic outcomes in most adult studies use adult Cerebral Performance Categories 1–2 which are identical to PCPC 1–3.24 Using this definition, 89% of survivors in our cohort had favorable neurologic outcomes. This contrasts markedly from the 37–65% rate of favorable neurologic outcomes among pediatric survivors following out-of-hospital cardiac arrest/CPR over the last decade.25–27 Perhaps a more important outcome is survival without new functional morbidities.10,11 Among the children surviving to hospital discharge following PICU CPR in our cohort, 73% had no new functional morbidities.
In single center studies, 3–6% of patients admitted to a pediatric cardiac ICU had cardiac arrests.4–6 Our data confirm this higher risk of PICU CPR events for cardiac versus non-cardiac patients (3.4% versus 0.8%). However, the absolute number of CPR events was similar among cardiac and non-cardiac PICU admissions because non-cardiac admissions were almost four-fold more common. In contrast to data from single center studies and an in-hospital cardiac arrest registry, rates of survival to discharge and survival with a favorable neurologic outcome were quite similar among cardiac and non-cardiac patients in our cohort (44% versus 47% and 41% versus 39%, respectively).4–9
Recent studies from the American Heart Association’s large multi-center Get With The Guidelines-Resuscitation in-hospital cardiac arrest registry have found that CPR durations >10 minutes are common among adults and children, and many patients survive after >30 minutes of CPR.9,28 However, the authors of those reports noted multiple limitations in the study designs including potential ascertainment biases, as well as absence of neurologic data for many of the survivors after >30 minutes of CPR.9,28 Consistent with the Get With The Guidelines-Resuscitation data, the likelihood of survival decreased with longer durations of CPR in our cohort. The median duration of CPR was 9 minutes (IQR 3, 30), and 67% of children survived to hospital discharge following 1–3 minutes of CPR compared with only 28% following >30 minutes of CPR. Surprisingly, favorable neurologic outcome was attained in 90% of survivors following 1–3 minutes of CPR compared with 89% following >30 minutes of CPR. These data suggest that ICU CPR efforts adequate for successful myocardial resuscitation may also be adequate for cerebral resuscitation. Neurologic outcomes appear much better for children with in-hospital CPR compared to pediatric out-of-hospital CPR where severe neurologic impairments have been reported to occur in 35–63% of cases.25–27 The differences can likely be explained by longer periods of untreated cardiac arrest with no cerebral blood flow during out-of-hospital cardiac arrests, and perhaps suboptimal basic and advanced life support in the challenging out-of-hospital setting. Additionally, difficulty in monitoring and treating post-cardiac arrest hypotension and myocardial dysfunction in the pre-hospital setting may contribute to the worse outcomes.
The findings in this multi-center study are limited because of the lack of data regarding CPR quality and post-cardiac arrest care.7,29 It is possible that the quality of CPR and post-cardiac arrest care are superior in these large, academic CPCCRN PICUs. If so, outcomes may not be generalizable to institutions with less effective CPR quality and/or post-cardiac arrest care. These data may differ from registry data or data from administrative databases because our research team reviewed the care of each patient in this PICU outcome study on a daily basis with a specific focus on collecting prospectively determined data from all children receiving CPR for >1 minute or defibrillation. Therefore, we are confident that all CPR events were documented in this study, avoiding ascertainment biases inherent in registry data and administrative databases. The neurologic outcome data does not include long-term outcomes, neurobehavioral outcomes, or detailed neuropsychological outcomes.30 Nevertheless, this study includes measures of both neurologic outcomes (PCPC) and functional outcomes (FSS) at the time of discharge for all surviving patients. Notably, adult data show that outcomes of individual patients improve over time, suggesting the long-term outcomes of these children may ultimately be superior to outcomes at discharge.31 Finally, the incidence of PICU CPR can be influenced by differences in the numerator (e.g., decreased by “do not attempt resuscitation” orders) and in the denominator (affected by admission criteria and illness severity of patients admitted to a specific PICU). Despite concerns that the incidence data might reflect increases in “do not attempt resuscitation” orders and increased admissions of children to PICUs with lower severity of illness, the incidence of PICU CPR has apparently not changed greatly over the last two decades.
Conclusions
Cardiopulmonary resuscitation is provided for many children admitted to the PICU despite close monitoring and many therapies intended to prevent cardiac arrest and the need for CPR. Fully 1.4% of children admitted to a large academic CPCCRN PICU received CPR and/or defibrillation. These data establish that contemporary PICU CPR, including long durations of CPR, results in high rates of survival to hospital discharge (45%), favorable neurologic outcome among survivors (89%), and survival without new morbidities (73%). Rates of survival to discharge and survival with favorable neurologic outcomes were similar among cardiac and non-cardiac patients. The rigorous prospective, observational study design avoided the limitations of missing data and potential selection biases inherent in registry and administrative data.
Acknowledgments
The Authors wish to acknowledge the important contributions of the following Research Coordinators and Data Coordinating Center staff: Teresa Liu, MPH, CCRP from University of Utah; Mary Ann DiLiberto, BS, RN, CCRC from The Children’s Hospital of Philadelphia; Carol Ann Twelves, BS, RN from The Children’s Hospital of Philadelphia; Jean Reardon, MA, BSN, RN from Children’s National Medical Center; Aimee Labell, MS, RN from Phoenix Children’s Hospital; Jeffrey Terry, MBA from Children’s Hospital Los Angeles; Rica Morzov, RN, BSN from Children’s Hospital Los Angeles; Margaret Villa, RN from Children’s Hospital Los Angeles and Mattel Children’s Hospital; Mary Ann Nyc, BS from UCLA Mattel Children’s Hospital; Jeni Kwok, JD from Children’s Hospital of Los Angeles; Ann Pawluszka, BSN, RN from Children’s Hospital of Michigan; Monica S. Weber, RN, BSN, CCRP from University of Michigan; Alan C. Abraham, BA, CCRC from University of Pittsburgh Medical Center; Jeri Burr, MS, RN-BC, CCRN from University of Utah.
Funding sources: This work was supported, in part, by cooperative agreements from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services: U10HD050096, U10HD049981, U10HD049983, U10HD050012, U10HD063108, U10HD063106, U10HD063114 and U01HD049934. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Copyright form disclosures: Dr. Berg received support for article research from the National Institutes of Health (NIH) and disclosed that this work was supported, in part, by cooperative agreements from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services: U10HD050096, U10HD049981, U10HD049983, U10HD050012, U10HD063108, U10HD063106, U10HD063114 and U01HD049934. His institution received funding from NICHD and support from cooperative agreements from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Department of Health and Human Services (U10HD050096, U10HD049981, U10HD049983, U10HD050012, U10HD063108, U10HD063106, U10HD063114 and U01HD049934). Dr. Clark received support for article research from the NIH. Her institution received funding from the NIH (NICHD). Dr. Moler received support for article research from the NIH. His institution received funding from the NIH/NICHD. Dr. Meert received support for article research from the NIH. Her institution received funding from the NIH. Dr. Harrison received support for article research from the NIH. His institution received funding from the NIH. Dr. Newth received support for article research from the NIH. His institution received funding from the NIH. Dr. Sutton received support for article research from the NIH and received funding from the Zoll Medical Corporation. His institution received funding from the National Institute of Child Health and Human Development. Dr. Wessel received support for article research from the NIH. His institution received funding from the NIH. Dr. Berger received support for article research from the NIH. His institution received funding from the NIH and the Association for Pediatric Pulmonary Hypertension. Dr. Carcillo received support for article research from the NIH. His institution received grant support from the NICHD. Dr. Dalton consulted for Innovtive ECMO Concepts, is employed by the Alaskan Native Tribal Health Center, lectured for Maquet Inc, received royalties from the SCCM (Rogers Text of Pediatric Critical Care), and received support for article research from the NIH. Her institution received grant support from the NIH. Dr. Heidemann received support for article research from the NIH. Her institution received funding (Dr. Heidemann’s salary is partially supported through the Collaborative Pediatric Critical Care Network grant sponsored by the NIH). Dr. Shanley received funding from University of MN, Case Western Reserve University, and Springer Publishers. He received support for article research from the NIH. His institution received funding from the NIH. Dr. Zuppa received support for article research from the NIH. Her institution received funding from NICHD and the NIH. Dr. Doctor received support for article research from the NIH. His institution received funding from the NIH and the Children’s Discovery Institute. Dr. Tamburro received support for article research from the NIH, disclosed government work, and disclosed other support (He has two potential financial conflicts, neither of which appear relevant to this manuscript submission. First, his institution received a grant from the US FDA Office of Orphan Product Development to study the use of exogenous surfactant in children with acute lung injury who had undergone a stem cell transplant or had leukemia / lymphoma. ONY supplied the medication for the trial. Also, he was an associate editor on a textbook and study guide and received royalties from Springer Publishers). Dr. Jenkins disclosed government work (She is a Federal Employee. Work was completed as part of official duties at the NIH. NIH funded the work through a cooperative agreement). Dr. Dean received support for article research from the NIH. His institution received funding from the NICHD. Dr. Holubkov received funding from St. Jude Medical, Inc. (Biostatistical Consulting – relationship terminated as of May 1, 2015); Pfizer Inc. (DSMB Membership); and Physicians Committee for Responsible Medicine (Biostatistical Consulting). He disclosed other support (He is a DSMB Member for the National Burn Association and for Fibrocell, Inc.) and he received support for article research from the NIH. His institution received funding from the NIH/NICHD. Dr. Pollack disclosed other support (occasional honoraria, occasional consultancy) and received support for article research from the NIH. His institution received funding from the NIH/NICHD under a U award.
Appendix Table 1.
Univariable associationsa with favorable neurologic outcome
| Parameter | Favorable outcome n (%) |
Relative risk (95% CI) | P-value |
|---|---|---|---|
| Sex | 0.68 | ||
| Female | 29 (42%) | 1.09 (0.73, 1.63) | |
| Male | 27 (39%) | Reference | |
| Age at time of CPR event | 0.46 | ||
| < 1 mo | 9 (38%) | Reference | |
| 1 mo – < 1 yr | 27 (47%) | 1.24 (0.69, 2.23) | |
| 1 yr – < 8 yrs | 11 (31%) | 0.81 (0.40, 1.66) | |
| 8 yrs – < 18 yrs | 9 (43%) | 1.14 (0.56, 2.34) | |
| Race | 0.35 | ||
| Black or African American | 10 (29%) | Reference | |
| White | 27 (48%) | 1.64 (0.91, 2.95) | |
| Other | 4 (40%) | 1.36 (0.54, 3.41) | |
| Unknown or Not Reported | 15 (38%) | 1.31 (0.68, 2.52) | |
| Ethnicity | 0.84 | ||
| Hispanic or Latino | 11 (44%) | Reference | |
| Not Hispanic or Latino | 31 (41%) | 0.93 (0.55, 1.56) | |
| Unknown or Not Reported | 14 (37%) | 0.84 (0.46, 1.54) | |
| Payer | 0.39 | ||
| Commercial | 20 (43%) | Reference | |
| Government | 29 (37%) | 0.86 (0.56, 1.34) | |
| Other | 4 (80%) | 1.88 (1.08, 3.26) | |
| Unknown | 3 (38%) | 0.88 (0.34, 2.29) | |
| Patient type | 0.84 | ||
| Cardiac | 30 (41%) | 1.04 (0.69, 1.57) | |
| Non-cardiac | 26 (39%) | Reference | |
| Baseline FSS Score | 0.90 | ||
| Good/Mild (6–9) | 45 (39%) | Reference | |
| Moderate (10–15) | 9 (45%) | 1.14 (0.67, 1.95) | |
| Severe/very severe (>16) | 2 (40%) | 1.01 (0.34, 3.04) | |
| Baseline PCPC | 0.52 | ||
| 1–3 (Normal, mild, moderate) | 53 (41%) | Reference | |
| 4–5 (Severe, coma/vegetative) | 3 (30%) | 0.73 (0.28, 1.92) | |
| Primary Disorder for ICU Admission | 0.34 | ||
| Respiratory | 19 (46%) | Reference | |
| Cardiovascular Disease – Acquired | 9 (43%) | 0.92 (0.51, 1.67) | |
| Cardiovascular Disease – Congenital | 22 (42%) | 0.90 (0.57, 1.42) | |
| Neurologic | 1 (13%) | 0.27 (0.04, 1.74) | |
| Miscellaneous | 5 (31%) | 0.67 (0.30, 1.50) | |
| PRISM-III, median (IQR) | 8 (3, 11) [vs. 8 (3, 16)] |
0.97 (0.95, 1.00)b | 0.046 |
| Time from PICU admission to index CPR event | 0.11 | ||
| <24 hours | 19 (40%) | Reference | |
| 24 hours – <1 week | 25 (50%) | 1.24 (0.79, 1.93) | |
| 1 week or more | 12 (29%) | 0.71 (0.39, 1.28) | |
| Defibrillation performed | 0.37 | ||
| Yes | 5 (29%) | 0.70 (0.33, 1.51) | |
| No | 51 (42%) | Reference | |
| Reason chest compressions started | 0.28 | ||
| Poor perfusion | 39 (43%) | 1.30 (0.81, 2.09) | |
| Pulselessness | 15 (33%) | Reference | |
| CPR performed open or closed chest | 0.85 | ||
| Open chest | 8 (38%) | 0.94 (0.52, 1.70) | |
| Closed chest | 46 (40%) | Reference |
Unadjusted relative risk, 95% confidence interval (CI), and p-value based on modified Poisson regression model.
Reflects relative risk of favorable outcome for one unit increase in total PRISM score.
Appendix Table 2.
Number of CPR events among patients
| Number of CPR events | n (%) patients |
|---|---|
| 1 | 111 (80%) |
| 2 | 20 (14%) |
| 3 | 4 (3%) |
| 4 | 1 (1%) |
| 5 | 3 (2%) |
Appendix Table 3.
Outcomes among patients with single versus multiple CPR events within the initial PICU admission
| Parameter | 1 CPR event N = 111 |
2 or more CPR events N = 28 |
|---|---|---|
| Return of circulation achieved for all events | 80 (72%) | 13 (46%)* |
| Alive at the time of hospital discharge | 56 (50%) | 7 (25%) |
| Favorable neurologic outcome at hospital discharge (PCPC 1–3 or no change) | 49 (44%) | 7 (25%)# |
15 (54%) failed to achieve ROC during a subsequent CPR event.
6 survived to discharge with PCPC of 1 or no change from baseline and the other with PCPC 2.
Footnotes
This investigation was performed at The Children’s Hospital of Phildelphia, University of Michigan, Children’s Hospital of Michigan, UCLA, Children’s Hospital Los Angeles, Children’s National Medical Center, Children’s Hospital of Pittsburgh, and Phoenix Children’s Hospital, Children.
Dr. Nadkarni disclosed that he does not have any potential conflicts of interest.
Disclosures: None
Contributor Information
Robert A. Berg, Department of Anesthesiology and Critical Care, The Children’s Hospital of Philadelphia and University of Pennsylvania Perelman School of Medicine, Philadelphia, PA.
Vinay M. Nadkarni, Department of Anesthesiology and Critical Care, The Children’s Hospital of Philadelphia and University of Pennsylvania Perelman School of Medicine, Philadelphia, PA.
Amy E. Clark, Department of Pediatrics, University of Utah School of Medicine, Salt Lake City, UT.
Frank Moler, Department of Pediatrics, University of Michigan, Ann Arbor, MI.
Kathleen Meert, Department of Pediatrics, Children’s Hospital of Michigan, Detroit, MI.
Rick E. Harrison, Department of Pediatrics, University of California at Los Angeles, Los Angeles, CA.
Christopher J. L. Newth, Department of Anesthesiology and Critical Care Medicine, Children’s Hospital Los Angeles, Los Angeles, CA.
Robert M. Sutton, Department of Anesthesiology and Critical Care, The Children’s Hospital of Philadelphia and University of Pennsylvania Perelman School of Medicine, Philadelphia, PA.
David L. Wessel, Department of Pediatrics, Children’s National Medical Center, Washington DC.
John T. Berger, Department of Pediatrics, Children’s National Medical Center, Washington DC.
Joseph Carcillo, Department of Critical Care Medicine, Children’s Hospital of Pittsburgh, Pittsburgh, PA.
Heidi Dalton, Department of Child Health, Phoenix Children’s Hospital and University of Arizona College of Medicine-Phoenix, Phoenix, AZ.
Sabrina Heidemann, Department of Pediatrics, Children’s Hospital of Michigan, Detroit, MI.
Thomas P. Shanley, Department of Pediatrics, University of Michigan, Ann Arbor, MI.
Athena F. Zuppa, Department of Anesthesiology and Critical Care, The Children’s Hospital of Philadelphia and University of Pennsylvania Perelman School of Medicine, Philadelphia, PA.
Allan Doctor, Departments of Pediatrics and Biochemistry, Washington University School of Medicine, St. Louis, MO.
Robert F. Tamburro, Eunice Kennedy Shriver National Institutes of Child Health and Human Development (NICHD), the National Institutes of Health (NIH), Bethesda, MD.
Tammara L. Jenkins, Eunice Kennedy Shriver National Institutes of Child Health and Human Development (NICHD), the National Institutes of Health (NIH), Bethesda, MD.
J. Michael Dean, Department of Pediatrics, University of Utah School of Medicine, Salt Lake City, UT.
Richard Holubkov, Department of Pediatrics, University of Utah School of Medicine, Salt Lake City, UT.
Murray M. Pollack, Children’s National Medical Center, Washington DC, Department of Pediatrics, George Washington University School of Medicine For the Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network.
References
- 1.Berg RA, Sutton RM, Holubkov R, Nicholson CE, Dean JM, Harrison R, Heidemann S, Meert K, Newth C, Moler F, Pollack M, Dalton H, Doctor A, Wessel D, Berger J, Shanley T, Carcillo J, Nadkarni VM, Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network and for the American Heart Association’s Get With the Guidelines-Resuscitation (formerly the National Registry of Cardiopulmonary Resuscitation) Investigators Ratio of PICU versus ward cardiopulmonary resuscitation events is increasing. Crit Care Med. 2013;41:2292–7. doi: 10.1097/CCM.0b013e31828cf0c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knudson JD, Neish SR, Cabrera AG, Lowry AW, Shamszad P, Morales DL, Graves DE, Williams EA, Rossano JW. Prevalence and outcomes of pediatric in-hospital cardiopulmonary resuscitation in the United States: an analysis of the Kids’ Inpatient Database. Crit Care Med. 2012;40:2940–4. doi: 10.1097/CCM.0b013e31825feb3f. [DOI] [PubMed] [Google Scholar]
- 3.Slonim AD, Patel KM, Ruttimann UE, Pollack MM. Cardiopulmonary resuscitation in pediatric intensive care units. Crit Care Med. 1997;25:1951–5. doi: 10.1097/00003246-199712000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Peddy SB, Hazinski MF, Laussen PC, Thiagarajan RR, Hoffman GM, Nadkarni V, Tabutt S. Cardiopulmonary resuscitation: special considerations for infants and children with cardiac disease. Cardiol Young. 2007;17:116–26. doi: 10.1017/S1047951107001229. [DOI] [PubMed] [Google Scholar]
- 5.Parra DA, Totapally BR, Zahn E, Jacobs J, Aldousany A, Burke RP, Chang AC. Outcome of cardiopulmonary resuscitation in a pediatric cardiac intensive care unit. Crit Care Med. 2000;28:3296–300. doi: 10.1097/00003246-200009000-00030. [DOI] [PubMed] [Google Scholar]
- 6.Rhodes JF, Blaufox AD, Seiden HS, Asnes JD, Gross RP, Rhodes JP, Griepp RB, Rossi AF. Cardiac Arrest in Infants After Congenital Heart Surgery. Circulation. 1999;100(Supplement 2):II-194–II-199. doi: 10.1161/01.cir.100.suppl_2.ii-194. [DOI] [PubMed] [Google Scholar]
- 7.Topjian AA, Berg RA, Nadkarni VM. Pediatric cardiopulmonary resuscitation: advances in science, techniques, and outcomes. Pediatrics. 2008;122:1086–98. doi: 10.1542/peds.2007-3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meaney PA, Nadkarni VM, Cook EF, Testa M, Helfaer M, Kaye W, Larkin GL, Berg RA. Higher survival rates among younger patients after pediatric intensive care unit cardiac arrests. Pediatrics. 2006;118:2424–33. doi: 10.1542/peds.2006-1724. [DOI] [PubMed] [Google Scholar]
- 9.Matos RI, Watson RS, Nadkarni VM, Huang HH, Berg RA, Meaney PA, Carroll CL, Berens RJ, Praestgaard A, Weissfeld L, Spinella PC. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation. 2013;127:442–51. doi: 10.1161/CIRCULATIONAHA.112.125625. [DOI] [PubMed] [Google Scholar]
- 10.Pollack MM, Holubkov R, Funai T, berger JT, Clark AE, Meert K, Berg RA, Carcillo J, Wessell DL, Moler F, Dalton H, Newth CJL, Shanley T, Harrison RE, Doctor A, Jenkins TL, Tamburro R, Dean JM, Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network Simultaneous Prediction of New Morbidity, Mortality, and Survival without New Morbidity from Pediatric Intensive Care: A New Paradigm for Outcomes Assessment. Crit Care Med. 2015 doi: 10.1097/CCM.0000000000001081. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pollack MM, Holubkov R, Funai T, Clark A, Berger JT, Meert K, Newth CJ, Shanley T, Moler F, Carcillo J, Berg RA, Dalton H, Wessel DL, Harrison RE, Doctor A, Dean JM, Jenkins TL, Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network Pediatric Intensive Care Outcomes: Development of New Morbidities During Pediatric Critical Care. Pediatr Crit Care Med. 2014;15:821–7. doi: 10.1097/PCC.0000000000000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berg MD, Schexnayder SM, Chameides L, Terry M, Donoghue A, Hickey RW, Berg RA, Sutton RM, Hazinski MF. Pediatric Basic Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S862–S875. doi: 10.1161/CIRCULATIONAHA.110.971085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L. Cardiac Arrest and Cardiopulmonary Resuscitation Outcome Reports: Update and Simplification of the Utstein Templates for Resuscitation Registries. Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 14.Pollack MM, Holubkov R, Glass P, Dean JM, Meert KL, Zimmerman J, Anand KJ, Carcillo J, Newth CJ, Harrison R, Willson DF, Nicholson C, Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network Functional Status Scale: new pediatric outcome measure. Pediatrics. 2009;124:e18–28. doi: 10.1542/peds.2008-1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pollack MMHR, Funai T, Clark A, Moler F, Shanley T, Meert K, Newth CJL, Carcillo J, Berger JT, Doctor A, Berg RA, Dalton H, Wessel DL, Harrison RE, Dean JM, Jenkins TL, Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network The Relationship between the Functional Status Scale and the Pediatric Overall and Cerebral Performance Categories. JAMA Pediatrics. 2014;168:671–6. doi: 10.1001/jamapediatrics.2013.5316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raymond TT, Cunningham CB, Thompson MT, Thomas JA, Dalton HJ, Nadkarnai VM. Outcomes among neonates, infants and children after extracorporeal cardiopulmonary resuscitation for refractory in-hospital pediatric cardiac arrest: a report from the National Registry of Cardiopulmonary Resuscitation. Pediatr Crit Care Med. 2010;11:362–371. doi: 10.1097/PCC.0b013e3181c0141b. [DOI] [PubMed] [Google Scholar]
- 17.Wolfe H, Zebuhr C, Topjian AA, Nishisaki A, Niles DE, Meaney PA, Boyle L, Giordano RT, Davis D, Priestley M, Apkon M, Berg RA, Nadkarni VM, Sutton RM. Interdisciplinary ICU Cardiac Arrest Debriefing Improves Survival Outcomes. Crit Care Med. 2014;42:1688–95. doi: 10.1097/CCM.0000000000000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case control studies. Am J Epidemiol. 2004;160:301–5. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- 19.Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid Response Teams: A Systematic Review and Meta-analysis. Arch Intern Med. 2010;170:18–26. doi: 10.1001/archinternmed.2009.424. [DOI] [PubMed] [Google Scholar]
- 20.Randolph AG, Gonzales CA, Cortellini L, Yeh TS. Growth of pediatric intensive care units in the United States from 1995 to 2001. J Pediatr. 2004;144:792–8. doi: 10.1016/j.jpeds.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 21.Nishisaki A, Pines JM, Lin RJ, Helfaer MA, Berg RA, TenHave T, Nadkarni VM. The Impact of 24-hour In-hospital Pediatric Critical Care Attending Physician Presence on Process of Care and Patient Outcomes. Critical Care Medicine. 2012;40:2190–5. doi: 10.1097/CCM.0b013e31824e1cda. [DOI] [PubMed] [Google Scholar]
- 22.Moler FW, Silverstein FS, Meert KL, Donaldson AE, Holubkov R, Browning B, Slomine BS, Christensen JR, Dean JM. Rationale, Timeline, Study Design and Protocol Overview of the Therapeutic Hypothermia After Pediatric Cardiac Arrest (THAPCA) Trials. Pediatr Crit Care Med. 2013;14:e304–15. doi: 10.1097/PCC.0b013e31828a863a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, Chan PS. American Heart Association Get With the Guidelines–Resuscitation Investigators. Survival trends in pediatric in-hospital cardiac arrests: an analysis from Get With the Guidelines-Resuscitation. Circ Cardiovasc Qual Outcomes. 2013;6:42–9. doi: 10.1161/CIRCOUTCOMES.112.967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Becker LB, Aufderheide TP, Geocadin RG, Callaway CW, Lazar RM, Donnino MW, Nadkarni VM, Abella BS, Adrie C, Berg RA, Merchant RM, O’Connor RE, Meltzer DO, Holm MB, Longstreth WT, Halperin HR. Primary Outcomes for Resuscitation Science Studies: A Consensus Statement from the American Heart Association. Circulation. 2011;124:2158–77. doi: 10.1161/CIR.0b013e3182340239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moler FW, Meert K, Donaldson AE, Nadkarni V, Brilli RJ, Dalton HJ, Clark RS, Shaffner DH, Schleien CL, Statler K, Tieves KS, Hackbarth R, Pretzlaff R, van der Jagt EW, Levy F, Hernan L, Silverstein FS, Dean JM, Pediatric Emergency Care Applied Research Network In-hospital versus out-of-hospital pediatric cardiac arrest: a multicenter cohort study. Crit Care Med. 2009;37:2259–67. doi: 10.1097/CCM.0b013e3181a00a6a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nitta M, Iwami T, Kitamura T, Nadkarni VM, Berg RA, Shimizu N, Ohta K, Nishiuchi T, Hayashi Y, Hiraide A, Tamai H, Kobayashi M, Morita H. Age-specific differences in outcomes after out-of-hospital cardiac arrests. Pediatrics. 2011;128:e812–20. doi: 10.1542/peds.2010-3886. [DOI] [PubMed] [Google Scholar]
- 27.Michiels EA, Dumas F, Quan L, Selby L, Copass M, Rea T. Long-term outcomes following pediatric out-of-hospital cardiac arrest. Pediatrs Crit Care Med. 2013;14:755–60. doi: 10.1097/PCC.0b013e31829763e2. [DOI] [PubMed] [Google Scholar]
- 28.Goldberger ZD, Chan PS, Berg RA, Kronick SL, Cooke CR, Lu M, Banerjee M, Hayward RA, Krumholz HM, Nallamothu BK. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380:1473–81. doi: 10.1016/S0140-6736(12)60862-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meaney PA, Bobrow BJ, Mancini ME, Christenson J, deCaen AR, Bhanji F, Abella BS, Kleinman ME, Edelson DP, Berg RA, Aufderheide TP, Menon V, Leary M. CPR Quality: Improving cardiac resuscitation outcomes both inside and outside the hospital: A consensus statement from the American Heart Association. Circulation. 2013;128:417–35. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 30.Holubkov R, Clark AE, Moler FW, Slomine BS, Christensen JR, Silverstein FS, Meert KL, Pollack MM, Dean JM. Efficacy outcome selection in the Therapeutic Hypothermia After Pediatric Cardiac Arrest (THAPCA) Trials. Pediatr Crit Care Med. 2015;16:1–10. doi: 10.1097/PCC.0000000000000272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sauvé MJ, Doolittle N, Walker JA, Paul SM, Scheinman MM. Factors associated with cognitive recovery after cardiopulmonary resuscitation. Am J Crit Care. 1996;5:127–39. [PubMed] [Google Scholar]


