Introduction
Angiolymphoid hyperplasia with eosinophilia (ALHE) is an uncommon, benign disorder that presents as solitary or multiple papulonodules, located predominantly in the head and neck region. The pathogenesis of ALHE remains controversial. It has occurred following various forms of trauma or infection. The disorder is commonly regarded as an angioproliferative process accompanied by an inflammatory infiltrate that is thought to be a reactive component. ALHE may represent a T-cell lymphoproliferative disorder of a benign or low-grade malignant nature.1 Other reported cases have shown damaged arteries and veins at the base of the lesion, suggesting that an underlying arteriovenous malformation may play a role in the pathogenesis.2 Additionally, some evidence suggests that ALHE may be related to traumatic pseudoaneurysm, supporting a vascular origin.3 Multiple treatments are proposed in the dermatologic literature for ALHE. We report a case of multiple lesions on the neck treated with low-dose methotrexate.
Case report
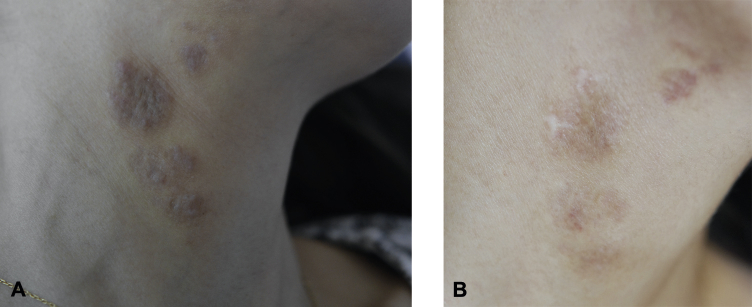
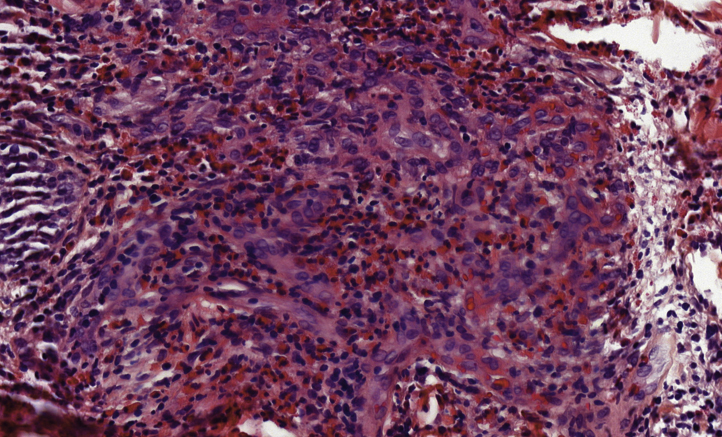
A 31-year-old woman presented in 2006 with a single erythematous nodule with overlying fine scales located on the right side of the neck. Three months later, she returned to the clinic with additional new lesions on the same side of the neck. Ultrasound scan and cutaneous magnetic resonance imaging showed proliferation of subcutaneous blood vessels without arteriovenous malformation. The histopathology findings showed vascular hyperplasia lined by enlarged endothelial cells that have ovoid nuclei and intracytoplasmic vacuoles accompanied by mixed inflammatory infiltrate of lymphocytes and eosinophils (Fig 1).2 Peripheral hypereosinophilia (900 g/L) was also seen. The patient was treated initially with oral prednisone, 30 mg daily for 1 month, resulting in complete regression of the lesions. She gained 6 kg during the treatment period but showed no other adverse effects. However, despite slowly tapering the prednisone, the lesions recurred 48 hours after stopping treatment. Remarkable long-lasting improvement was observed after initiation of pulsed dye laser therapy. A total of 6 complete sessions at a rate of one session per month led to resolution of symptoms for 6 years. After 6 years, she had another relapse that was resistant to 4 sessions of pulsed dye laser therapy (Fig 2, A). The patient refused to take systemic steroids because of their adverse side effects. While reviewing the dermatologic literature, we found a case of orbital ALHE resistant to corticosteroid therapy in which the patient was treated successfully with low-dose methotrexate and remained symptom free 1 year after discontinuation of the treatment.4 After an extensive discussion of the different treatment modalities and their potential risks and benefits with our patient, we opted for the initiation of methotrexate. The patient was started on methotrexate, 15 mg/wk for 12 months, after which we observed that the lesions were significantly improved (Fig 2, B). The dose was subsequently reduced to 10 mg/wk for 7 months and then to 5 mg/wk for 3 months, after which methotrexate was stopped. The patient remained free of recurrence with a 4-month follow-up.
Fig 1.
Histopathologic features of ALHE. Vascular hyperplasia lined by enlarged endothelial cells, inflammatory infiltrate with lymphocytes and eosinophils. (Hematoxylin-eosin stain; original magnification: ×200.)
Fig 2.
Multiple well-infiltrated, brown-violaceous plaques and nodules on the neck before initiation of the methotrexate (A). Twelve months after treatment with methotrexate, the lesions regressed dramatically. There remains scars of the initial biopsies with postinflammatory hyperpigmentation and some minimally inflamed macular lesions (B).
Discussion
Treatment is usually required for ALHE, as spontaneous regression is rare. Many treatments are proposed in the dermatologic literature. Complete surgical excision is the preferred choice, but recurrence may happen if excision is incomplete. Other alternative treatments have been reported with variable levels of success. These treatments include laser therapy (pulsed dye, CO2, copper vapor),5, 6 systemic or intralesional corticosteroid injection,7 cryotherapy, imiquimod, tacrolimus, isotretinoin, radiotherapy, interferon alfa 2a, anti–interleukin-5 antibody, photodynamic therapy, and methotrexate.4
The surgical excision was not applicable in our case because of the multiplicity and the infiltrative nature of the lesions. This infiltrative nature could also explain the inefficacy of laser therapy at this stage.
Methotrexate is a potent competitive antagonist of the enzyme dihydrofolate reductase that is essential in DNA synthesis process. Methotrexate has anti-inflammatory, immunosuppressive, and antiproliferative effects and has been used successfully in the treatment of various skin diseases either with or without a vascular component. Examples of these cutaneous lesions with vascular components include various vasculitides such as polyarteritis nodosa, Takayasu arteritis, and Wegener granulomatosis.8 The advantages of methotrexate include the once-weekly administration, the well-established side-effect profile, and the low cost.
The treatment regimen was well tolerated in our case, and the patient had a positive response. This response can be attributed to methotrexate's dual mechanism of action: anti-inflammatory and antiangiogenic. The patient underwent periodic check-ups with no adverse effects observed either clinically or from laboratory markers that included complete blood count with differentiation, creatinine, and liver transaminases. We continue following up with her and observing the efficacy of the treatment. Although there are no studies to confirm the most effective management regimen, we believe that methotrexate could have a promising role in the treatment of ALHE.
Footnotes
Funding sources: none.
Conflicts of interest: None declared.
References
- 1.Kempf W., Haeffner A.C., Zepter K. Angiolymphoid hyperplasia with eosinophilia: evidence for a T-cell lymphoproliferative origin. Hum Pathol. 2002;33:1023–1029. doi: 10.1053/hupa.2002.128247. [DOI] [PubMed] [Google Scholar]
- 2.Olsen T.G., Helwig E.B. Angiolymphoid Hyperplasia with Eosinophilia: A clinicopathologic study of 116 patients. J Am Acad Dermatol. 1985;12:781–796. doi: 10.1016/s0190-9622(85)70098-9. [DOI] [PubMed] [Google Scholar]
- 3.Vadlamudi G., Schinella R. Traumatic pseudoaneurysm: a possible early lesion in the spectrum of epithelioid hemangioma/angiolymphoid hyperplasia with eosinophilia. Am J Dermatopathol. 1998;20(2):113–117. doi: 10.1097/00000372-199804000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Baker M.S., Avery R.B., Johnson C.R., Allen R.C. Methotrexate as an Alternative Treatment for Orbital Angiolymphoid Hyperplasia with Eosinophilia. Orbit. 2012;31:324–326. doi: 10.3109/01676830.2011.584932. [DOI] [PubMed] [Google Scholar]
- 5.Ozcanli H., Ozenci A.M., Ozcanli C., Ibis S., Gurer I.E. Angiolymphoid hyperplasia: a case of a rare arterial involvement and successful recurrence treatment with laser therapy. J Eur Acad Dermatol Venereol. 2007;21:1106–1107. doi: 10.1111/j.1468-3083.2006.02094.x. [DOI] [PubMed] [Google Scholar]
- 6.Abrahamson T.G., Davis D.A. Angiolymphoid hyperplasia with eosinophilia responsive to pulsed dye laser. J Am Acad Dermatol. 2003;49:S195–S196. doi: 10.1067/mjd.2003.314. [DOI] [PubMed] [Google Scholar]
- 7.Lembo S., Balato A., Cirillo T., Balato N. A long-term follow-up of angiolymphoid hyperplasia with eosinophilia treated by corticosteroids: when a traditional therapy is still up-to-date. Case Rep Dermatol. 2011;3:64–67. doi: 10.1159/000323182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schartz N.E., Alaoui S., Vignon-Pennamen M.D. Successful treatment in two cases of steroid-dependent cutaneous polyarteritis nodosa with low-dose methotrexate. Dermatology. 2001;203(4):336–338. doi: 10.1159/000051785. [DOI] [PubMed] [Google Scholar]