Introduction
Ustekinumab, a monoclonal antibody that blocks interleukin-12 and interleukin-23, is a biological therapy used to treat moderate-to-severe psoriasis. Bullous pemphigoid (BP) induced by anti–tumor necrosis factor-alfa (TNF-α) agents has been described in the literature.1, 2, 3 No cases have been reported with ustekinumab. We report a case of BP occurring in a patient treated for 9 months with ustekinumab for severe psoriasis.
Case report
A 62-year-old man with a greater-than 20-year history of chronic plaque psoriasis presented with new-onset pruritic bullae. He had a history of hypertension and was treated with metformin for type 2 diabetes. There was no personal or family history of autoimmune disease. After unsuccessful systemic therapies (acitretin, methotrexate) and anti–TNF-α agents (etanercept, adalimumab), ustekinumab was introduced in September 2012. The patient received 5 subcutaneous injections: 45 mg at weeks 0, 4, 16 and 90 mg at weeks 28 and 40 (the dose was increased because the patient gained weight). The patient noticed the eruption of pruritic bullae in June 2013, 3 days after the fifth injection. Physical examination found tense bullae on erythematous patches and urticarial plaques predominantly on the upper thighs, lower neck, and upper trunk (Fig 1, Fig 2). There were no mucosal lesions and Nikolsky's sign was absent. Psoriatic plaques on the trunk and lower limbs were present. Histologic examination found a dermo-epidermal detachment with eosinophilic infiltration. The direct immunofluorescence highlighted deposits of IgG and C3 along the basal membrane (Fig 3). Cutaneous immunofluorescence basement membrane zone antibodies were present. These elements confirm the diagnosis of BP. Cessation of ustekinumab and the use of topical corticosteroids resulted in complete regression of the urticarial plaques and bullae within 3 weeks. The patient's psoriasis flared in December 2013, and he was started on infliximab with good results. No relapse of bullous disease was observed 18 months after withdrawal of ustekinumab and 14 months after stopping topical steroids.
Fig 1.
Tense bullae of the upper trunk.
Fig 2.
Tense bullae of the upper trunk.
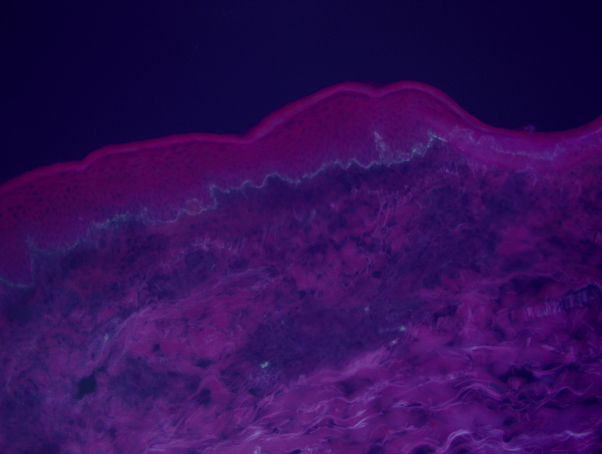
Fig 3.
Direct immunofluorescence: linear highlight in the basal membrane zone (deposits of IgG and C3 along the basal membrane).
Discussion
Many drugs may induce BP, including antibiotics (penicillin, fluoroquinolone, chloroquine, rifampicin), diuretics (furosemide, spironolactone), and angiotensin-converting enzyme inhibitors.4 Although an association between frequency of BP and psoriasis may exist,5 several cases of bullous pemphigoid were attributed to anti–TNF-α agents.1, 2, 3 To our knowledge, no case of BP has been described during ustekinumab use, but its mechanism of action, leading to down-regulation of TNF-α, makes it possibly accountable. Ustekinumab blocks the differentiation and clonal expression of Th1 and Th17 effector cells. It results in a reduced production of pro-inflammatory cytokines, including TNF-α agents.6 Although the mechanism is not yet understood, the modification of the immune response could cause the onset of BP. Other effects of inflammatory or immune skin disorders have also been reported with ustekinumab use, including cases of alopecia areata,7 linear IgA dermatosis,8 and eczema,9 suggesting the potential consequences of this cytokine imbalance. In our case, several factors argue in favor of an iatrogenic origin: the relatively early age of onset, acute and limited nature of the lesions, their rapid regression after stopping ustekinumab, and no recurrence after 18 months. Metformin's causation was less probable since the patient had been on this medication for many years and because no cases of BP with Metformin's use have been reported. Additionally, infliximab may have had an impact on this patient's BP, as this treatment was introduced a few months after cessation of ustekinumab to treat psoriasis. Some cases of BP have been treated successfully with anti–TNF-α agents.10, 11, 12 BP has also been treated successfully with ustekinumab in one report, which makes the whole question of causation and effect more difficult for the biologics.13 It suggests the involvement of other cytokinic pathways in our case, independent from TNF-α agents, in the occurrence of iatrogenic pemphigoid. To our knowledge, we report the first case of BP during ustekinumab therapy. With the increasing use of newly marketed biologics, new cutaneous side effects may occur in the future.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Bordignon M., Belloni-Fortina A., Pigozzi B., Tarantello M., Alaibac M. Bullous pemphigoid during long-term TNF-alpha blocker therapy. Dermatology. 2009;219:357–358. doi: 10.1159/000243805. [DOI] [PubMed] [Google Scholar]
- 2.Boussemart L., Jacobelli S., Batteux F. Autoimmune bullous skin diseases occurring under anti-tumor necrosis factor therapy: two case reports. Dermatology. 2010;221:201–205. doi: 10.1159/000318008. [DOI] [PubMed] [Google Scholar]
- 3.Stausbøl-Grøn B., Deleuran M., Sommer Hansen E., Kragballe K. Development of bullous pemphigoid during treatment of psoriasis with adalimumab. Clin Exp Dermatol. 2009;34:285–286. doi: 10.1111/j.1365-2230.2008.03204.x. [DOI] [PubMed] [Google Scholar]
- 4.Stavropoulos P.G., Soura E., Antoniou C. Drug-induced pemphigoid: a review of the literature. J Eur Acad Dermatol Venereol. 2014;28(9):1133–1140. doi: 10.1111/jdv.12366. [DOI] [PubMed] [Google Scholar]
- 5.Cusano F., Iannazzone S.S., Riccio G., Piccirillo F. Coexisting bullous pemphigoid and psoriasis successfully treated with etanercept. Eur J Dermatol. 2010;20:520. doi: 10.1684/ejd.2010.0970. [DOI] [PubMed] [Google Scholar]
- 6.Mease P.J. Inhibition of interleukin-17, interleukin-23 and the TH17 cell pathway in the treatment of psoriatic arthritis and psoriasis. Curr Opin Rheumatol. 2015;27(2):127–133. doi: 10.1097/BOR.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 7.Słowińsk M., Kardynal A., Warszawik O., Czuwara J., Rudnicka L. Alopecia areata developing paralell to improvement of psoriasis during ustekinumab therapy. J Dermatol Case Rep. 2010;4(1):15–17. doi: 10.3315/jdcr.2010.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Becker J. Development of linear IgA bullous dermatosis in a patient with psoriasis taking ustekinumab. J Am Acad Dermatol. 2012;67(4):150–151. doi: 10.1016/j.jaad.2011.11.955. [DOI] [PubMed] [Google Scholar]
- 9.Pernet C., Guillot B., Bessis D. Eczematous drug eruption after ustekinumab treatment. Arch Dermatol. 2012;148(8):959–960. doi: 10.1001/archdermatol.2012.586. [DOI] [PubMed] [Google Scholar]
- 10.Nin M., Tokunaga D., Ishii N., Komai A., Hashimoto T., Katoh N. Case of coexisting psoriatic arthritis and bullous pemphigoid improved by etanercept. J Dermatol. 2013;40:55–56. doi: 10.1111/j.1346-8138.2012.01659.x. [DOI] [PubMed] [Google Scholar]
- 11.Yamauchi P.S., Lowe N.J., Gindi V. Treatment of coexisting bullous pemphigoid and psoriasis with the tumor necrosis factor antagonist etanercept. J Am Acad Dermatol. 2006;54:121–122. doi: 10.1016/j.jaad.2005.10.055. [DOI] [PubMed] [Google Scholar]
- 12.Heffernan M.P., Bentley D.D. Successful treatment of Mucous Membrane Pemphigoid with Infliximab. Arch Dermatol. 2006;142(10):1268–1270. doi: 10.1001/archderm.142.10.1268. [DOI] [PubMed] [Google Scholar]
- 13.Majima Y., Yagi H., Tateishi C. A successful treatment with ustekinumab in a case of antilaminin-γ1 pemphigoid associated with psoriasis. Br J Dermatol. 2013;168(6):1367–1369. doi: 10.1111/bjd.12163. [DOI] [PubMed] [Google Scholar]