Introduction
Basal cell carcinoma (BCC) is the most common type of skin cancer and is seen rarely on the nipple-areolar complex (NAC) in men and women. We present a case of a 47-year-old woman referred for Mohs micrographic surgery (MMS) for BCC on the nipple. Close examination of frozen section specimens during MMS and rebiopsy led to the correct diagnosis of invasive breast cancer. This case emphasizes the histologic importance of remaining vigilant when interpreting Mohs pathology and the importance of understanding immunohistochemical stains.
Case report
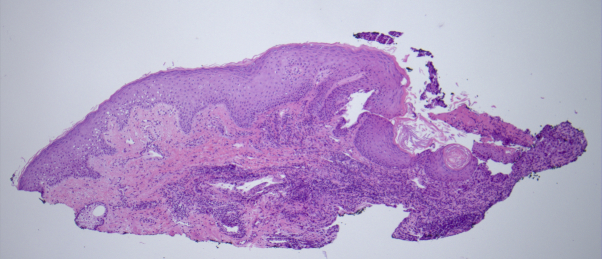
A 47-year-old woman was evaluated by her dermatologist for a persistent erosion of the right nipple. The patient suffered skin breakdown in this area, with intermittent, spontaneous, bloody discharge for the last year. No breast mass was identified on physical examination. Two mammograms, an ultrasound scan, and an MRI of the area were reported unremarkable. On examination, the patient had only superficial erosion involving the right nipple. A shallow shave biopsy found aggregates of atypical basaloid cells (Fig 1). These aggregates were stained with Ber-EP4, an immunomarker used to identify basal cell carcinoma.
Fig 1.
Original shave biopsy section shows basaloid islands.
A histologic diagnosis of BCC was rendered, and the patient was referred for MMS. At the time of presentation for surgery, there was a 7-mm erosion of the nipple without involvement of the areola (Fig 2). Frozen sections from the first stage of MMS revealed atypical cells that were evaluated as inconsistent with BCC (Fig 3) by the surgeon. Surgery was terminated and an excisional biopsy was performed.
Fig 2.
Clinical appearance at the time of presentation for Mohs surgery with a 7-mm erosion of the nipple.
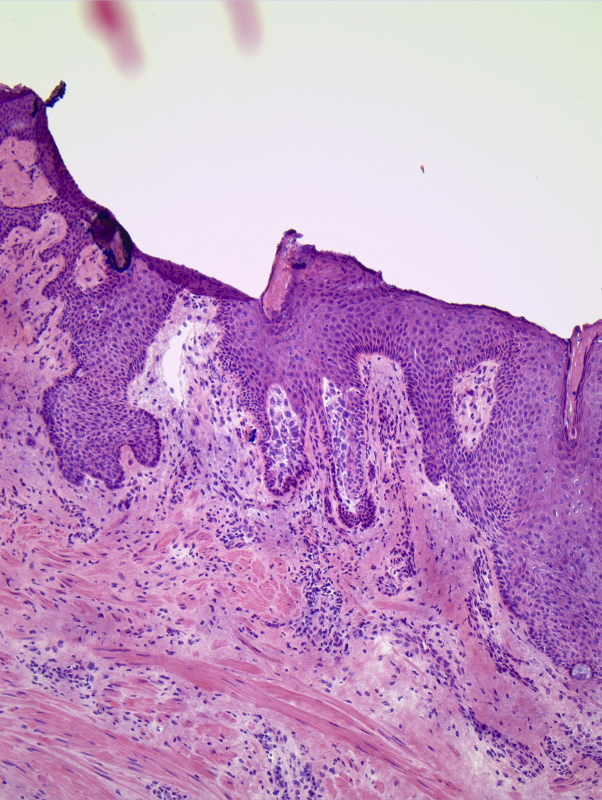
Fig 3.
Mohs frozen sections show atypical cells not consistent with the histologic appearance of BCC.
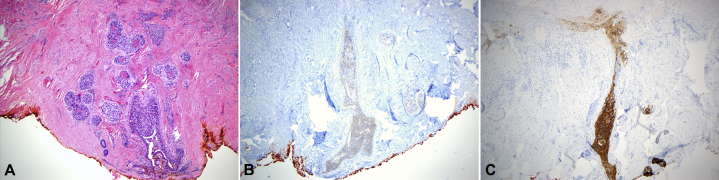
Histologic examination of the larger excisional specimen found a deeper proliferation of markedly atypical and pleomorphic cells that formed ductal structures, and an assessment of ductal breast carcinoma was rendered by a different dermatopathologist (W. H.) (Fig 4, A). Repeat immunostains showed expression of Ber-EP4 (Fig 4, B) but also expression of cytokeratin-7 and HER2-neu (Fig 4, C). There was also a markedly elevated proliferative index with Ki67 staining. The patient was then referred to an oncologist and breast surgeon for evaluation and management. Based on tumor size and a negative sentinel lymph node biopsy result, stage T1a breast cancer was diagnosed. Treatment consisted of a lumpectomy with nipple removal and adjuvant radiation.
Fig 4.
A, Hematoxylin-eosin stained section of re-excision specimen with invasive atypical ductal structures consistent with breast carcinoma. B, Ber-Ep4–stained section of re-excision specimen shows positive staining. C, HER2-neu–stained section of re-excision specimen shows positive staining.
Discussion
A broad differential diagnosis exists for dermatologic disease of the NAC. This differential diagnosis includes inflammatory conditions, such as dermatitis (nipple eczema) and lichen simplex chronicus; benign neoplasms, such as nipple adenoma; and malignant neoplasms, including nonmelanoma skin cancer, Paget's disease, breast carcinoma, and metastatic disease.
BCC of the NAC is a rare but increasingly common condition most often identified in men with excessive sun exposure of the trunk.1 The initial misdiagnosis of BCC may have been a result of the small size of the shave sampling and the choice of a shave rather than a punch biopsy. Although the expression of Ber-EP4 was thought to mitigate in favor of BCC, this monoclonal antibody actually marks a variety of neoplastic processes. In fact, the Ber-EP4 immunostain was developed from a breast cancer cell line, and the stain will mark not only BCC, but also other cutaneous malignancies, some breast carcinomas, and some gastrointestinal carcinomas.2
The presence of nipple discharge in this patient should likely have also brought the assessment of BCC into question. Although discharge has been reported in BCC of the nipple, it is not present in most cases.3 Nipple discharge with negative imaging findings poses a significant diagnostic problem for clinicians. Benign nipple discharge is most often bilateral, nonbloody, and nonspontaneous.4 On the contrary, pathologic nipple discharge, as seen in this patient, is most often unilateral, bloody, and spontaneous.4 Recent studies indicate that up to 25% of patients with pathologic nipple discharge will have underlying breast cancer. For patients with breast cancer presenting with only pathologic nipple discharge, mammography is of limited sensitivity (10% to 57%).5
When performing MMS, physicians must approach all histology specimens with a critical eye for the unexpected. Reviewing biopsy specimens before MMS resulted in an altered diagnosis in 2% of the cases in one study.6 Mohs surgeons treating cutaneous neoplasms of the NAC should be aware that breast carcinoma can mimic a BCC. In this case, careful histologic assessment of the frozen sections during MMS allowed for identification of potential misdiagnosis, for transition to an improved biopsy technique, and, ultimately, for timely and appropriate management of the patient's breast carcinoma.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Whitaker-Worth D.L., Carlone V., Susser W.S., Phelan N., Grant-Kels J.M. Dermatologic diseases of the breast and nipple. J Am Acad Dermatol. 2000;43(5 Pt 1):733–751. doi: 10.1067/mjd.2000.109303. [DOI] [PubMed] [Google Scholar]
- 2.Latza U., Niedobitek G., Schwarting R., Nekarda H., Stein H. Ber-EP4: new monoclonal antibody which distinguishes epithelia from mesothelial. J Clin Pathol. 1990;43(3):213–219. doi: 10.1136/jcp.43.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta C., Sheth D., Snower D.P. Primary basal cell carcinoma of the nipple. Arch Pathol Lab Med. 2004;128(7):792–793. doi: 10.5858/2004-128-792-PBCCOT. [DOI] [PubMed] [Google Scholar]
- 4.Yang L., Wu D., Fan Z.M. Retrospective analysis of pathologic nipple discharge. Genet Mol Res. 2015;14(1):1443–1449. doi: 10.4238/2015.February.13.23. [DOI] [PubMed] [Google Scholar]
- 5.Adepoju L.J., Chun J., El-Tamer M., Ditkoff B.A., Schnabel F. Joseph KA.The value of clinical characteristics and breast-imaging studies in predicting a histopathologic diagnosis of cancer or high-risk lesion in patients with spontaneous nipple discharge. Am J Surg. 2005;190(4):644–646. doi: 10.1016/j.amjsurg.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 6.Butler S.T., Youker S.R., Mandrell J., Flanagan K.H., Fosko S.W. The importance of reviewing pathology specimens before Mohs surgery. Dermatol Surg. 2009;35(3):407–411. doi: 10.1111/j.1524-4725.2008.01056.x. [DOI] [PubMed] [Google Scholar]