Lobular capillary hemangiomas, also known as pyogenic granulomas, are common, benign, vascular proliferations of the cutaneous or mucous surfaces that grow rapidly and are prone to ulceration and bleeding.1, 2 Recurrence of lobular capillary hemangiomas in the same location after treatment is common with rates ranging from 3.7% to 43.5%.3 Well-known causes of lobular capillary hemangiomas are trauma, infection, medication, chronic irritation, viral oncogenes, increased levels of female sex hormones, and microscopic arteriovenous anastomoses.1 Patients commonly seek treatment because of associated pain or discomfort from ulceration, bleeding, or both. Surgical excision and cryotherapy show best therapeutic outcomes for lobular capillary hemangiomas, although electrodessication, shave excision, imiquimod cream, topical timolol, and sclerotherapy are also used.3, 4
We report a case of frequent lobular capillary hemangioma development in the setting of von Hippel-Lindau syndrome (VHL) and neurofibromatosis type 1 (NF1), requiring multiple treatment modalities.
Case report
A 34-year-old man with a history of VHL and NF1 was referred to dermatology for evaluation and management of multiple bleeding papules. The papules were tender, and the bleeding caused his pillowcases to be soaked in blood. He reported many similar papules previously in various anatomical locations. Removal of prior lesions was successful and did not cause satellitosis. New papules would appear gradually over years, and at the time of the visit, 6 papules were bothersome because of intermittent bleeding.
The patient was given the diagnosis of NF1 based on clinical findings that were first noted in childhood including multiple café au lait macules, axillary freckling, and Lisch nodules. VHL was suspected after magnetic resonance imaging showed hemangioblastoma of the left cerebellum during evaluation of sensorineural hearing loss. VHL was subsequently confirmed by mutation analysis (P81S mutation). Central nervous system hemangioblastoma is the most common tumor in VHL and was present in the patient. He did not have any additional tumors or cysts in the central nervous system or visceral organs that are common in VHL, which include retinal hemangioblastomas, renal cell carcinoma and cysts, pheochromocytomas, and pancreatic tumors and cysts.5 The patient did not have family history of NF1 or VHL. Medications included dextroamphetamine for attention deficit disorder.
On physical examination, the lesions of concern were exophytic, red, vascular papules located on the right jawline, front of the right shoulder, left lower aspect of the back, and right lower aspect of the back, consistent with lobular capillary hemangiomas (Fig 1). These were painful with slight pressure. Several other similar, although smaller, papules were noted on the trunk. On the face, trunk, and extremities there were at least 20 scattered well-defined, ovoid, light-brown macules. Involving the chest, abdomen, and back were multiple discrete 4- to 8-mm subcutaneous rubbery-soft nodules (Fig 2). Axillary freckling was noted on both axilla and the groin. The patient returned to the dermatology clinic 4 months later with new growing and bleeding vascular papules in new locations; they were similar to those removed at the initial visit and consistent with lobular capillary hemangiomas.
Fig 1.
Two vascular papules on the right jawline and front of the right shoulder. Asymptomatic ill-defined soft nodule on the right upper lip.
Fig 2.
Multiple café au lait macules, axillary freckling, and neurofibromas on the torso and abdomen.
There are many options for treatment of lobular capillary hemangiomas. In our patient, these lesions were treated by shave excision with electrodessication and samples were sent for histologic evaluation (Fig 3). At the follow-up visit 4 months later, 5 additional lesions were destroyed with the same approach. Neither recurrence nor satellitosis was noted at sites of prior treatment.
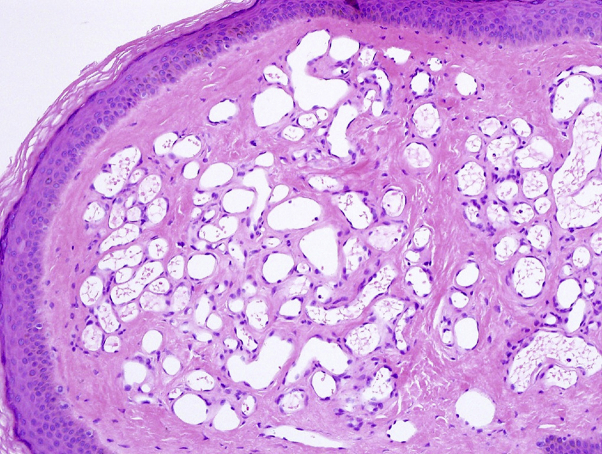
Fig 3.
Proliferating capillaries grouped into lobules by dense fibrous bands, clutched by an epithelial collarette. (Hematoxylin-eosin stain; original magnification: ×20.)
Discussion
NF1 and VHL are both autosomal dominant syndromes caused by mutations of tumor suppressor genes with prevalences of 1:3,000 and 1:36,000 respectively.5, 6 The presence of 2 independent genetic syndromes in the same individual is extremely rare, and this case represents a chance event rate of 1 in 108,000,000 (based on the combined prevalence of VHL 1:36,000 and NF1 1:3000).5, 6 NF1 occurs as a result of mutation of the NF1 tumor suppressor gene (chromosome 17), leading to neurofibromas, café au lait macules, central nervous system gliomas, and bony abnormalities.6 VHL occurs as a result of a mutation in the VHL tumor suppressor gene (chromosome 3), which leads to unregulated growth of vascular tumors in multiple tissues. Common VHL tumors include hemangioblastomas of the retina, brain, and viscera along with renal cell carcinoma and pheochromocytoma.5, 7 In VHL, angiogenesis is likely the result of increased levels of glucose transporter 1, vascular endothelial growth factor, and platelet-derived growth factor.5 Unlike in NF1, VHL does not exhibit cutaneous findings.8 Interestingly, lobular capillary hemangiomas have not been described in association with either NF1 or VHL.
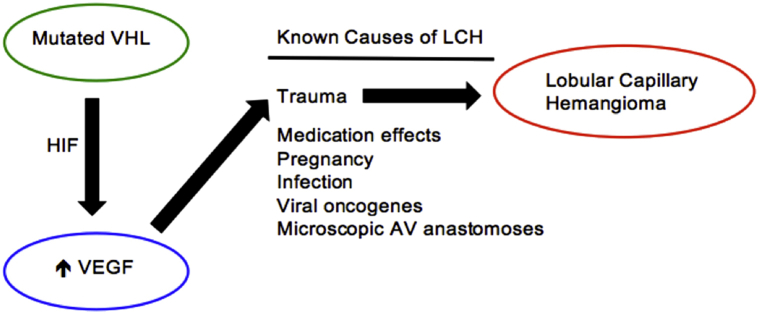
This patient shows an uncommon growth pattern of lobular capillary hemangiomas with numerous lesions in new locations that require periodic treatment for symptom relief rather than the typical recurrent lobular capillary hemangioma in the same location. Based on known predisposing factors of lobular capillary hemangiomas and based on the pathophysiology of this patient's genetic diseases, we hypothesize that increased vascular endothelial growth factor in addition to minor trauma contributed to this presentation (Fig 4).
Fig 4.
Potential pathway for recurrent lobular capillary hemangiomas (LCH) in this patient. There are several well-known causes for lobular capillary hemangiomas.1 In the setting of von Hippel-Lindau syndrome (VHL), there is increased vascular endothelial growth factor (VEGF),5 which we hypothesize predisposes our patient to more frequent development of lobular capillary hemangiomas in the setting of minor trauma.9AV, Arteriovenous; HIF, hypoxia inducible factor.
We present a case of a patient with VHL and NF1, and very frequent development of lobular capillary hemangiomas. We hypothesize that this phenomenon is related to the angiogenesis pathways induced by VHL. Further studies are needed to examine a connection between VHL and/or NF1 and lobular capillary hemangiomas.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Lin R.L., Janniger C.K. Pyogenic granuloma. Cutis. 2004;74(4):229–233. [PubMed] [Google Scholar]
- 2.Harris M.N., Desai R., Chuang T.Y., Hood A.F., Mirowski G.W. Lobular capillary hemangiomas: an epidemiologic report, with emphasis on cutaneous lesions. J Am Acad Dermatol. 2000;42(6):1012–1016. [PubMed] [Google Scholar]
- 3.Lee J., Sinno H., Tahiri Y., Gilardino M.S. Treatment options for cutaneous pyogenic granulomas: a review. J Plast Reconstr Aesthet Surg. 2011;64(9):1216–1220. doi: 10.1016/j.bjps.2010.12.021. [DOI] [PubMed] [Google Scholar]
- 4.Khorsand K., Maier M., Brandling-Bennett H.A. Pyogenic granuloma in a 5-month-old treated with topical timolol. Pediatr Dermatol. 2015;32(1):150–151. doi: 10.1111/pde.12297. [DOI] [PubMed] [Google Scholar]
- 5.Lonser R.R., Glenn G.M., Walther M. von Hippel-Lindau disease. Lancet. 2003;361(9374):2059–2067. doi: 10.1016/S0140-6736(03)13643-4. [DOI] [PubMed] [Google Scholar]
- 6.Lu-Emerson C., Plotkin S.R. The neurofibromatoses. Part 1: NF1. Rev Neurol Dis. 2009;6(2):E47–E53. [PubMed] [Google Scholar]
- 7.Maher E.R., Neumann H.P., Richard S. von Hippel-Lindau disease: a clinical and scientific review. Eur J Hum Genet. 2011;19(6):617–623. doi: 10.1038/ejhg.2010.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quigg M., Rust R.S., Miller J.Q. Clinical findings of the phakomatoses: von Hippel-Lindau disease. Neurology. 2006;66(9):E33–34. doi: 10.1212/01.wnl.0000210491.21411.25. [DOI] [PubMed] [Google Scholar]
- 9.Abe M., Misago N., Tanaka S., Masuoka J., Tabuchi K. Capillary hemangioma of the central nervous system: a comparative study with lobular capillary hemangioma of the skin. Acta Neuropathol. 2005;109(2):151–158. doi: 10.1007/s00401-004-0921-4. [DOI] [PubMed] [Google Scholar]