Abstract
Purpose
To classify the self-identified goals of individuals post-stroke with chronic upper extremity (UE) paresis, and determine if age, UE functional capacity, and pre-stroke hand dominance influence overall goal selection.
Method
Sixty five subjects participated. Using the Canadian Occupational Performance Measure (COPM) to establish treatment goals, the top five goals were categorized using the Occupational Therapy Practice Framework into five categories: activities of daily living (ADL), instrumental activities of daily living (IADL), leisure, work, and general UE movement. A chi-square analysis determined if age, UE functional capacity (measured by the Action Research Arm Test), and UE hand dominance influenced individual goal selection.
Results
The majority of goals were in the ADL (37%) and IADL (40%) categories. A small percentage (12%) was related to general UE movement. Individuals with moderate UE functional capacity identified more ADL goals than those with higher UE functional capacity. There was not a difference between age and UE dominance across all five goal areas.
Conclusions
Individuals with chronic UE paresis had specific goals that were not influenced by age or hand dominance, but partially influenced by severity. General UE movement goals were identified less than goals related to specific activities.
After a stroke, an individual’s capacity to participate in activities that are personally meaningful is often compromised. On average, individuals post-stroke discontinue 57% of their activities [1]. Decreased participation is often a result of many stroke-related deficits, the primary one being upper extremity (UE) paresis. At 6 months post-stroke, 65% of survivors cannot incorporate their affected hand into routine activity [2]. Given the vital role of both upper extremities in daily activities [3], deficits in participation following a stroke can be attributed, in part, to UE paresis and its resulting loss of function.
An essential component of rehabilitation is generating goals [4], wherein clinicians establish discipline-specific goals that guide interventions to address stroke-related deficits. Currently, goals may be established from a variety of sources. Goals may come from pre-established template created by the Institution where an individual receives rehabilitation services or they may be generated out of clinical experience and the clinician’s interpretation about the individual’s level of function. In addition to guiding clinical interventions, rehabilitation goals are ultimately established to increase participation in meaningful activities. Individuals with an inability to participate in meaningful activities can experience psychosocial consequences such as depression [5], feelings of helplessness [5], and a loss of individual role, both for self and also within a family unit [6]. If the overall goal of rehabilitation is to increase participation in meaningful activity, then rehabilitation efforts should be individualized. This is often inconsistently accomplished through collaborative goal setting between the client and the clinician [7].
Current research indicates that individuals after stroke experienced little control over their rehabilitation goals and their involvement in goal setting is generally passive [8]. This is despite the fact that involving patients in the goal setting process is empowering and generates a personal sense of ownership [9] and motivation [10]. Further, involving patients in goal setting affords therapists an opportunity to provide individualized rehabilitation interventions [10]. Previous studies have identified general goals of individuals with stroke, such as improving self-care and home management [11] in addition to shopping and meal preparation [1]. What is less understood is what activities individuals with UE dysfunction identify as goals while receiving rehabilitation services. It is possible that self-identified goals may be influenced by different characteristics, such as age, UE functional capacity, and hand dominance. For example, as individuals age, their interests and activities may evolve which could potentially influence or re-direct goals. Additionally, both UE functional capacity and UE dominance are likely to influence goal selection simply due to the nature of activities (i.e. activities that require a higher degree of coordination and function and those more dominant-oriented).
The purpose of this study was to first evaluate the self-identified goals of people with chronic stroke and upper extremity paresis and then determine if these self-identified goals were influenced by age, UE functional capacity, and/or pre-stroke hand dominance. This study will provide an in-depth understanding of the goals of individuals living with chronic paresis and improve overall efforts to customize the rehabilitation process to each person.
Methods
This descriptive analysis was completed on data acquired at the baseline assessment as part of an ongoing randomized control trial studying the dose of task specific practice on UE function following stroke (NCT #01146379). The study was approved by the Human Research Protection Office at Washington University, St. Louis, MO. Informed consent was obtained from all participants.
We used available data from 65 participants. Inclusion criteria for the clinical trial were: (1) diagnosis of an ischemic or hemorrhagic stroke; (2) sufficient cognitive skills to actively participate in a high-repetition, task-specific intervention for the UE, defined as a score of 0–1 on items 1b and 1c of the National Institute of Health Stroke Scale (NIHSS); (3) unilateral upper extremity weakness defined by a score of 1–3 on the arm item of the NIHSS; (4) Action Research Arm Test score of the affected limb ≥ 10 points; and (5) ability to provide informed consent. Individuals were excluded from this study if they were: (1) unable to follow a 2-step command; (2) unavailable for two-month follow-up testing; (3) pre-existing psychiatric diagnoses or other neurological diagnoses; (4) currently receiving other stroke treatment (e.g. Botox); and/or (5) pregnant.
Prior to receiving the task-specific intervention for the paretic UE, each individual identified personal goals using the Canadian Occupational Performance Measure [12]. The Canadian Occupational Performance Measure is a widely-used assessment of client outcomes related to the domains of self-care, productivity, and leisure using a semi-structured interview format [12]. This measure is designed for use with a variety of populations and clinical diagnoses, and has strong psychometric properties [13,14]. Because the clinical trial intervention is targeting upper extremity function, participants identified goals that primarily related to UE function as opposed to other stroke-related deficits (e.g. walking). Additionally, the Canadian Occupational Performance Measure is often utilized as a goal setting tool for individuals receiving rehabilitation services [15,16]. When completing this measure, individuals typically identify multiple problems/deficits related to three domains (self-care, productivity, leisure) and then conclude with selecting five primary goals. These five goals are specific to each individual. Primary goals may be selected due to high personal value for a particular activity and/or a strong need to be able to perform a particular action. The final goals may span all three domains or be targeted toward just one or two domains, depending on the individual.
The final five primary goals were used for this analysis. First, identified goals were grouped according to areas of occupation using the Occupational Therapy Practice Framework [17]. The practice framework was used because it provides the most comprehensive structure to classifying occupations according to current practice standards. Goals from the Canadian Occupational Performance Measure were categorized as follows: activities of daily living (ADLs), instrumental activities of daily living (IADLs), work, and leisure. Additionally, we added a category not included in the Occupational Therapy Practice Framework labeled general UE movement to capture more abstract UE goals such as “reach better” or “manipulate small items.” Activities of daily living refer to an individual’s capacity to care for oneself and enable basic well-being [18]. This includes tasks such as dressing, grooming, or bathing. Instrumental activities of daily living support participation in the home and community but often require a more complex skill level; examples are meal preparation, yard work, or driving [17]. Work related activities are specific to job performance and often include some form of financial compensation [17]. Finally, leisure tasks are non-obligatory activities that are self-initiated and intrinsically motivating [17]. Because leisure activity can occur in a variety of settings and intensities, we further classified leisure goals as indoor and sedentary, outdoor and light physical activity, outdoor and moderate physical activity, or outdoor and strenuous using an established scale [19]. The first author reviewed each category of goals a minimum of five times to ensure consistency. Given the level of detail provided for each domain of the Occupational Therapy Practice Framework, discrepancy between goal categories was rarely encountered. Where categorization was unclear, the research team reviewed at length and reached a consensus for final assignment to a category.
After categorizing each goal from each person, we then examined how subject characteristics might influence goal choice. We chose the characteristics of age, UE functional capacity, and pre-stroke hand dominance because these characteristics have strong potential to influence the type of goals participants identify for rehabilitation. Age was dichotomized into those who were younger than 65 years and those who were 65 years or older. UE functional capacity was defined by baseline score of the affected UE on the Action Research Arm Test (ARAT). The ARAT is a criterion-rated, 19-item, activity based assessment of the UE and is a widely-used measure of upper extremity functional capacity following a stroke [20]. The psychometric properties of the ARAT have been well-established [21–23]. Using ordinal scoring, individuals are scored on four sub-tests assessing grasp, grip, pinch, and gross motor on a scale of 0 (unable to complete) to 3 (completes with normal movement). A maximum score of 57 is possible, indicating normal movement. The scale was divided approximately into thirds, such that individuals with scores between 10 and ≤ 20 points were considered to have low functional capacity; scores between 21 and 39 points were considered to have moderate functional capacity; and scores of ≥ 40 were considered to have high functional capacity. Hand dominance was established via self-report, referring to pre-stroke function. This information was then used to determine if the dominant or nondominant UE was affected by the stroke.
Statistical Analyses
Statistical analyses were completed with SPSS version 20 (IBM Corporation; Armonk, New York). We visually inspected the data, once goals were categorized according to the Occupational Therapy Practice Framework. Chi-Square analyses were run to determine if subject characteristics of age, UE functional capacity, and hand dominance influenced the frequency of goal selection. Each goal domain was tested separately and a Pearson chi-square analysis was completed for 3x2 tables and a Fisher’s exact test was completed for 2x2 tables. If the 3x2 analyses showed a significant difference, additional pairwise (2x2) analyses were done to determine which pairs were different. The criterion for significance was set at P < 0.05.
Results
The final five goals identified on the COPM from 65 participants were used for this study. General characteristics of all participants are provided in Table 1. Overall, participants presented with high to moderate UE functional capacity based on ARAT scores. Most were independent with ADLs and living with at least one other adult.
Table 1.
Participant characteristics collected at the baseline assessment.
| Demographic | Total Samplea (n=65) |
|---|---|
|
| |
| Age (yrs) | 59 ± 10.2 |
|
| |
| Months since stroke | 24 ± 33.9 |
|
| |
| % Male | 63% |
|
| |
| % Dominant side affected | 55% |
|
| |
| % Type of stroke | |
| Ischemic | 74% |
| Hemorrhagic | 12% |
| Unknown | 14% |
|
| |
| % Living status | |
| Living alone, independent with ADL | 25% |
| Living alone, requires assist with ADL | 5% |
| Living with others, independent with ADL | 56% |
| Living with others, requires assist with ADL | 14% |
|
| |
| % Working prior to stroke | 58% |
|
| |
| % Working presently | |
| Not working | 89% |
| < 20 hrs/week | 5% |
| Part-time (>20 hrs/week) | 5% |
| Full-time | 1% |
|
| |
| Baseline ARAT scoreb | 32 ± 11.4 |
Values reported for age, months since stroke, and baseline ARAT as means with standard deviation; remaining values reported as percentage of total sample
ARAT: Action Research Arm Test, 0–57 point scale, higher numbers indicate more UE function.
A total of 319 goals were identified. Table 2 includes examples of goals within each category.
Table 2.
Examples of participant goals across goal categories
| ADL | IADL | Work | Leisure | General UE Movement |
|---|---|---|---|---|
| Fastening buttons | Baking cookies | Painting a wall | Playing the piano | Picking up small items |
| Cutting food with knife | Mowing the yard | Using large metal scissors to cut | Sewing | Stabilizing item with affected hand |
| Tying a neck tie | Unlocking a door | Using screwdriver | Restoring car | Carry heavy objects |
| Using a curling iron | Typing on computer | Stabilizing electrical box against wall | Playing cards | Reaching overhead |
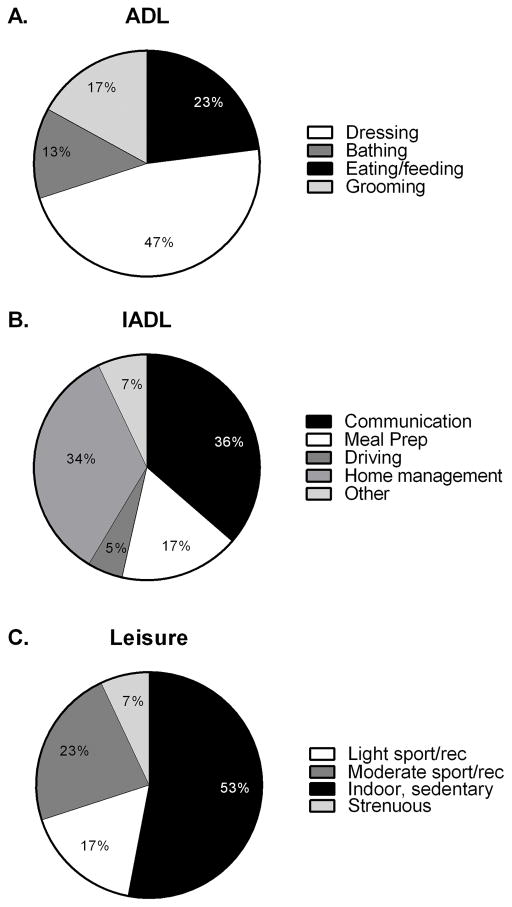
Because the IADL domain of the Practice Framework is large, goals ranged from meal preparation, managing doors and locks around the home, and also outdoor maintenance activities. Work related activities were specific to two participants, both employed in positions requiring a substantial amount of manual labor. After categorizing goals, there were 117 goals in the ADL domain (37% of total) and 129 in the IADL domain (40% of total). A total of 6 goals were identified related to work and productivity (2% of total) and 30 goals were in the leisure activity domain (9% of total). The final category of general UE movement included 37 goals (12% of total). Figure 1 reflects the goal distribution within the ADL, IADL, and leisure domains. The majority of goals within the ADL category (Figure 1A) were for dressing, with smaller percentages distributed across bathing, eating/feeding, and grooming. More than a third of the goals in the IADL category (Figure 1B) were related to communication (e.g. handwriting and/or typing), with another third related to home management activities (e.g. laundry). Within the leisure category (Figure 1C), more than half of goals were indoor, sedentary activities. Due to the limited number of goals in the work/productivity and general UE movement categories, these were not further divided into subcategories.
Figure 1.
Table 3 presents a comparison of the frequency of goals for each participant by the three characteristics of age, UE functional capacity, and hand dominance. Only one of the three characteristics identified influenced overall goal selection. No significant difference was found between the five goal categories when stratified by age. We found a small but significant difference between UE functional capacity and ADL goals (p= 0.04). Additional chi-square analyses comparing each pair showed that those with moderate functional capacity had more ADL goals than those with high functional capacity (p= 0.02). There were no differences between the low functional capacity group and the other two groups. Overall UE functional capacity did not influence the frequencies of the remaining goal categories. There was not a significant difference in all five goal areas between individuals whose dominant UE was affected versus individuals whose non-dominant UE was affected.
Table 3.
Percentage of participants identifying goals within each category relative to the three characteristics (age, UE functional capacity, dominance).
| Group | ADL | p | IADL | p | Work | p | Leisure | p | Non-specific | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | <65 | 90% | .11 | 92% | .56 | 10% | >.99 | 33% | .57 | 44% | .17 |
| ≥ 65 | 71% | 100% | 6% | 41% | 65% | ||||||
| Functional Capacitya | Low | 83% | .04* | 100% | .55 | 14% | .76 | 29% | .47 | 43% | .4 |
| Moderate | 92% | 92% | 8% | 33% | 46% | ||||||
| High | 64% | 92% | 8% | 50% | 67% | ||||||
| Dominance | Dominant affected | 83% | >.99 | 92% | .62 | 11% | .68 | 36% | >.99 | 53% | .62 |
| Non- Dominant affected | 86% | 97% | 7% | 35% | 45% |
: Stratified by ARAT (Action Research Arm Test) score: low functional capacity, ≤ 20 points; moderate functional capacity, 21–39 points; high functional capacity, ≥ 40 points
significant at p= 0.05
Discussion
To our knowledge, this study is the first of its kind to complete an in-depth analysis on the goals of chronic stroke survivors relative to their UE functional capacity. Previously published research is available on general goals of individuals post-stroke [11,24–26]. Given the prevalence of UE paresis, it is necessary to better understand the rehabilitation priorities of this population. The majority of goals spanned the IADL and ADL domains, as is expected given the breadth of these categories.
Our results indicate that only a small portion of goals were related to general UE movement, and not focused on accomplishing specific functional activities. Of the 319 total goals, only 12% were in the general UE movement category. The goals in this category might be considered more impairment-focused than activity-focused. The small percentage of impairment-focused goals is not consistent with the observation that impairment-focused therapeutic exercises, such as shoulder flexion exercises for increasing shoulder strength, or finger and wrist stretching exercises for increasing finger extension range of motion, are the most commonly observed UE rehabilitation interventions [27]. Our data suggest that general movement goals are a lower priority for individuals with UE dysfunction. Thus, in order to address the activity-focused goals of clients, therapists could consider more activity-based and fewer impairment-based UE interventions. Alternatively, self-identified general UE movement goals may have been a way for clients to describe difficulty with UE use across a variety of goal domains. Clinicians may want to consider this option and further inquire about how general goals link to problems performing functional activities in order to ensure individualized interventions.
The three characteristics of age, UE functional capacity, and pre-stroke hand dominance, had surprisingly little influence on goal selection across the five categories. We found that age, dichotomized as <65 years and ≥ 65 years, did not influence the self-identified goals across all 5 categories. UE functional capacity had only a small influence on the frequency of reported goals, such that there were more ADL goals identified by people with moderate functional capacity compared to high functional capacity, but no differences with the low functional capacity group. Within the subcategories of ADLs, there were no obvious differences, (based on visual inspection of goal lists) between the groups. Collectively, the data illustrate that people with UE paresis have specific goals that they want to be able to accomplish, and ADL vs. non-ADL goals should not be imposed by treating clinicians based on severity. Many goals identified for this study are activities that require the use of both upper extremities, regardless of which UE was affected by the stroke. This finding challenges clinicians to not assume goals relative to UE dominance but rather to each individual’s priorities and meaningful activities.
The results of this analysis reinforce the premise in stroke rehabilitation that every individual presents with a unique set of needs and goals and individualized rehabilitation is imperative. Because age, UE functional capacity, and hand dominance had little influence on selected goals, it would not be appropriate for clinicians to set goals based on these characteristics. For example, an individual whose nondominant UE was affected may still identify brushing teeth as a therapy goal because parts of the task such as prepping a toothbrush and managing a toothpaste container are typically a bilateral activity. To take this point further, handwriting is often regarded as an activity completed with the dominant UE. Someone may identify handwriting as a goal when the nondominant UE is affected in order to stabilize the paper during writing. Thus, our data provide support for the importance of patient/client input in the goal setting process [9,10].
Several limitations need to be considered when interpreting these data. First, we used the COPM to generate goals, where the structured interview inquires about the ability to do activities. Thus, the tool used may have led to over-identification of specific activities as goals and an under-identification of more general movement goals. Second, there were several instances in the chi-square analyses where we had insufficient numbers in a cell (i.e. <5). It most often occurred when examining the category of work goals, as there were not many identified. This means that differences might truly exist between groups, but we were unpowered to detect them. Third, individuals were cued to identify goals related to UE function because this was a clinical trial investigating the dose-response relationship on UE function. It is likely that, in the clinic, individual goals may cover a broader range of deficits, including cognitive and attentional dysfunction. While all deficits merit attention, this study aimed to provide a more comprehensive understanding of individual goals relative to the UE, given that over 70% of individuals experience hemiparesis after a stroke [28,29]. Finally, age was treated as a dichotomous variable when it is actually a continuous one. The split point at age 65 was chosen because that is a common retirement age in the United States. It is possible, though unlikely, that this split point caused us to miss a hidden relationship between self-identified goals and age.
In summary, self-identified goals of individuals with chronic UE dysfunction were specific to an activity, and less often included general movement (e.g. reach further or build strength). Age, UE functional capacity, and pre-stroke UE dominance do not significantly influence goal selection. Our data encourage clinicians not to assume that certain activities (e.g. typing on a computer when dexterity has been severely affected) may not be a priority to an individual following stroke. Given the bilateral nature of many activities, dominance is not a reliable determinant of individual goals. The same is true for both functional capacity and age. Future studies are now needed to determine how best to capitalize on individualized goals in order to optimize client-centered interventions and outcomes after stroke.
Implications for Rehabilitation.
Considering the specificity of individual goals following stroke, it is recommended that clinicians regularly utilize a goal setting tool to help establish client goals.
It is recommended that clinicians further inquire about general goals in order to link upper extremity deficits to functional activity limitations.
Age, upper extremity functional capacity, and hand dominance have little influence on the rehabilitation goals for individuals with chronic paresis after stroke.
Footnotes
Declaration of Interest
This study was funded by NIH R01HD068290. All authors contributed to data acquisition, processing, and manuscript preparation. The authors have no conflicts of interest to disclose.
References
- 1.Hartman-Maeir A, Soroker N, Ring H, Avni N, Katz N. Activities, participation and satisfaction one-year post stroke. Disabil Rehabil. 2007;29:559–566. doi: 10.1080/09638280600924996. [DOI] [PubMed] [Google Scholar]
- 2.Dobkin BH. Clinical practice. Rehabilitation after stroke. N Engl J Med. 2005;352:1677–1684. doi: 10.1056/NEJMcp043511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bailey RR, Lang CE. Upper-limb activity in adults: referent values using accelerometry. J Rehabil Res Dev. 2013;50:1213–1222. doi: 10.1682/JRRD.2012.12.0222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown M, Levack W, McPherson KM, Dean SG, Reed K, Weatherall M, Taylor WJ. Survival, momentum, and things that make me "me": patients' perceptions of goal setting after stroke. Disabil Rehabil. 2013 doi: 10.3109/09638288.2013.825653. [DOI] [PubMed] [Google Scholar]
- 5.Wood JP, Connelly DM, Maly MR. 'Getting back to real living': A qualitative study of the process of community reintegration after stroke. Clin Rehabil. 2010;24:1045–1056. doi: 10.1177/0269215510375901. [DOI] [PubMed] [Google Scholar]
- 6.Pound P, Gompertz P, Ebrahim S. A patient-centred study of the consequences of stroke. Clin Rehabil. 1998;12:338–347. doi: 10.1191/026921598677661555. [DOI] [PubMed] [Google Scholar]
- 7.Maitra KK, Erway F. Perception of client-centered practice in occupational therapists and their clients. Am J Occup Ther. 2006;60:298–310. doi: 10.5014/ajot.60.3.298. [DOI] [PubMed] [Google Scholar]
- 8.Rosewilliam S, Roskell CA, Pandyan AD. A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal setting in stroke rehabilitation. Clin Rehabil. 2011;25:501–514. doi: 10.1177/0269215510394467. [DOI] [PubMed] [Google Scholar]
- 9.Laver K, Halbert J, Stewart M, Crotty M. Patient readiness and ability to set recovery goals during the first 6 months after stroke. J Allied Health. 2010;39:e149–154. [PubMed] [Google Scholar]
- 10.Maclean N, Pound P, Wolfe C, Rudd A. Qualitative analysis of stroke patients' motivation for rehabilitation. Bmj. 2000;321:1051–1054. doi: 10.1136/bmj.321.7268.1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Phipps S, Richardson P. Occupational therapy outcomes for clients with traumatic brain injury and stroke using the Canadian Occupational Performance Measure. Am J Occup Ther. 2007;61:328–334. doi: 10.5014/ajot.61.3.328. [DOI] [PubMed] [Google Scholar]
- 12.Law M, Baptiste S, McColl M, Opzoomer A, Polatajko H, Pollock N. The Canadian occupational performance measure: an outcome measure for occupational therapy. Can J Occup Ther. 1990;57:82–87. doi: 10.1177/000841749005700207. [DOI] [PubMed] [Google Scholar]
- 13.McColl MA, Paterson M, Davies D, Doubt L, Law M. Validity and community utility of the Canadian Occupational Performance Measure. Can J Occup Ther. 2000;67:22–30. doi: 10.1177/000841740006700105. [DOI] [PubMed] [Google Scholar]
- 14.Cup EH, Scholte op Reimer WJ, Thijssen MC, van Kuyk-Minis MA. Reliability and validity of the Canadian Occupational Performance Measure in stroke patients. Clin Rehabil. 2003;17:402–409. doi: 10.1191/0269215503cr635oa. [DOI] [PubMed] [Google Scholar]
- 15.Wressle E, Lindstrand J, Neher M, Marcusson J, Henriksson C. The Canadian Occupational Performance Measure as an outcome measure and team tool in a day treatment programme. Disabil Rehabil. 2003;25:497–506. doi: 10.1080/0963828031000090560. [DOI] [PubMed] [Google Scholar]
- 16.Birkenmeier RL, Prager EM, Lang CE. Translating animal doses of task-specific training to people with chronic stroke in 1-hour therapy sessions: a proof-of-concept study. Neurorehabil Neural Repair. 2010;24:620–635. doi: 10.1177/1545968310361957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Association AOT. Occupational Therapy Practice Framework: Domain & Process. 3. American Journal of Occupational Therapy; 2014. p. 68. [Google Scholar]
- 18.Christiansen CH, Hammecker CL. Self-Care. In: Bonder BR, Wagner MB, editors. Functional Performance in older adults. F.A. Davis; 2001. pp. 155–175. [Google Scholar]
- 19.Washburn RA, Zhu W, McAuley E, Frogley M, Figoni SF. The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil. 2002;83:193–200. doi: 10.1053/apmr.2002.27467. [DOI] [PubMed] [Google Scholar]
- 20.Lang CE, Wagner JM, Dromerick AW, Edwards DF. Measurement of upper-extremity function early after stroke: properties of the action research arm test. Arch Phys Med Rehabil. 2006;87:1605–1610. doi: 10.1016/j.apmr.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Platz T, Pinkowski C, van Wijck F, Kim IH, di Bella P, Johnson G. Reliability and validity of arm function assessment with standardized guidelines for the Fugl-Meyer Test, Action Research Arm Test and Box and Block Test: a multicentre study. Clin Rehabil. 2005;19:404–411. doi: 10.1191/0269215505cr832oa. [DOI] [PubMed] [Google Scholar]
- 22.Van der Lee JH, De Groot V, Beckerman H, Wagenaar RC, Lankhorst GJ, Bouter LM. The intra- and interrater reliability of the action research arm test: a practical test of upper extremity function in patients with stroke. Arch Phys Med Rehabil. 2001;82:14–19. doi: 10.1053/apmr.2001.18668. [DOI] [PubMed] [Google Scholar]
- 23.Lin JH, Hsu MJ, Sheu CF, Wu TS, Lin RT, Chen CH, Hsieh CL. Psychometric comparisons of 4 measures for assessing upper-extremity function in people with stroke. Phys Ther. 2009;89:840–850. doi: 10.2522/ptj.20080285. [DOI] [PubMed] [Google Scholar]
- 24.Polatajko HJ, McEwen SE, Ryan JD, Baum CM. Pilot Randomized Controlled Trial Investigating Cognitive Strategy Use to Improve Goal Performance After Stroke. American Journal of Occupational Therapy. 2011;66:104–109. doi: 10.5014/ajot.2012.001784. [DOI] [PubMed] [Google Scholar]
- 25.Lawrence M, Kinn S. Determining the needs, priorities, and desired rehabilitation outcomes of young adults who have had a stroke. Rehabil Res Pract. 2012;2012:963978. doi: 10.1155/2012/963978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Skidmore ER, Holm MB, Whyte EM, Dew MA, Dawson D, Becker JT. The feasibility of meta-cognitive strategy training in acute inpatient stroke rehabilitation: case report. Neuropsychol Rehabil. 2011;21:208–223. doi: 10.1080/09602011.2011.552559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lang CE, Macdonald JR, Reisman DS, Boyd L, Jacobson Kimberley T, Schindler-Ivens SM, Hornby TG, Ross SA, Scheets PL. Observation of amounts of movement practice provided during stroke rehabilitation. Arch Phys Med Rehabil. 2009;90:1692–1698. doi: 10.1016/j.apmr.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris JE, Eng JJ, Miller WC, Dawson AS. A self-administered Graded Repetitive Arm Supplementary Program (GRASP) improves arm function during inpatient stroke rehabilitation: a multi-site randomized controlled trial. Stroke. 2009;40:2123–2128. doi: 10.1161/STROKEAHA.108.544585. [DOI] [PubMed] [Google Scholar]
- 29.Duncan PW, Goldstein LB, Horner RD, Landsman PB, Samsa GP, Matchar DB. Similar motor recovery of upper and lower extremities after stroke. Stroke. 1994;25:1181–1188. doi: 10.1161/01.str.25.6.1181. [DOI] [PubMed] [Google Scholar]