Abstract
Compressive neuropathies of the upper extremity are common and can result in profound disability if left untreated. Nerve releases are frequently performed, but can be complicated by both iatrogenic events as well as progression of neuropathy. In this review, we will examine the management of post-operative complications following two common nerve compression release procedures: carpal tunnel release and cubital tunnel release.
Keywords: median nerve, ulnar nerve, carpal tunnel syndrome, carpal tunnel release, ulnar tunnel syndrome, cubital tunnel syndrome, complications
Carpal Tunnel Syndrome
Carpal tunnel syndrome (CTS) is the most common compressive neuropathy, affecting 1.6-7.8% individuals.4-6 Carpal tunnel release (CTR) is one of the most frequently performed outpatient procedures in the United States, and is typically considered to be a minor elective and routine procedure.7 Complications are rare, but can result in devastating loss of hand function.
Intraoperative complications
Normal anatomy of the carpal tunnel is detailed in Figure 1, which guides incision placement for open release. However, several anatomic variants exist, and can increase the risk of iatrogenic injury.8-10 (Figure 2) A solid understanding of the anatomic relationships of the proximal palm, carpal canal, and distal forearm can direct correct incision placement and prevent iatrogenic injury. 11-17 (Figure 3) Fortunately, injury to major neurovascular structures during carpal tunnel release is exceedingly low. Permanent nerve injury more commonly occurs to the branches of the median nerve, including the palmar cutaneous branch (0.03%), the deep motor branch of the median nerve (0.01%), or the common digital nerves (0.12%), compared with injury to the median nerve proper (0.06%).18 Injuries to adjacent structures, including the superficial palmar arch (0.1%), flexor tendons (0.1%) and the ulnar nerve (0.03%) have been also described. 18,19 Endoscopic techniques may result in a slightly higher rate of major nerve injury (0.13-0.3%) versus open techniques (0.10-0.2%).18,20 However, other studies have not demonstrated a difference in major complications by technique. It is likely that overall complication rates are more dependent on surgeon experience the specific technique.21-23
Figure 1. Incision design for open CTR.
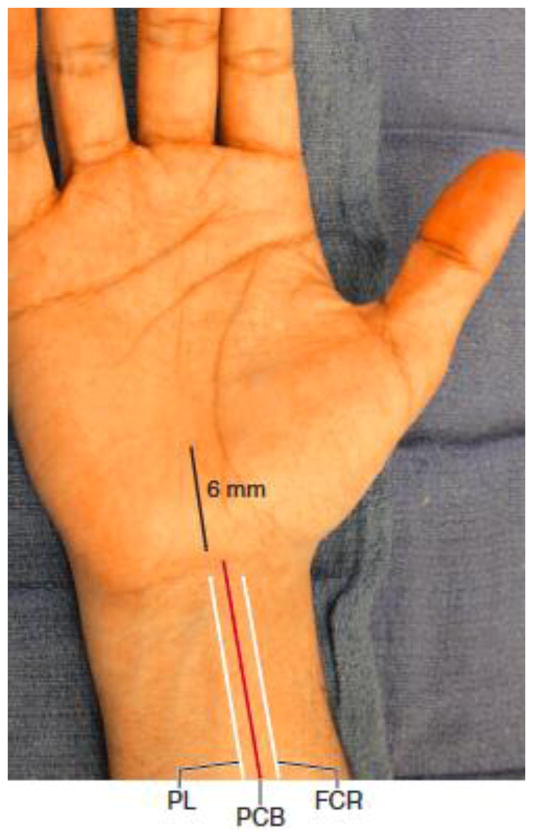
Iatrogenic injury to the palmar cutaneous branch of the median nerve can result in persistent paresthesias and painful neuromas, annadvertent division of the deep motor branch of the median nerve results loss of grip strength due to lack of palmar abduction and weakness with opposition. To prevent this, incisions for an open release should lie 5-6 mm ulnar to the thenar crease, in line with the ulnar border of the middle finger (Figure 3). However, overcorrecting in the ulnar direction can result in entry into the more superficial Guyon canal, with potential injury to the ulnar neurovascular bundle. Inadvertent entry into the Guyon canal can be recognized if the dissection is carried down through the skin to reveal hypothenar fat, with diminutive palmar fascia, and no visualization of the transverse fibers of the transverse carpal ligament. Because the hand naturally is slightly pronated when place on the hand table, entry into the Guyon canal can occur when the knife dissection is not perpendicular to the plane of the hand, but rather parallel to the transverse carpal ligament. From Sammer D. Open carpal tunnel release. In: Chung KC, editor. Operative techniques: hand and wrist surgery. vol. 2. Philadelphia: Elsevier Saunders; 2012; with permission
Figure 2. Topography of ulnar nerve and sites of ulnar nerve compression.
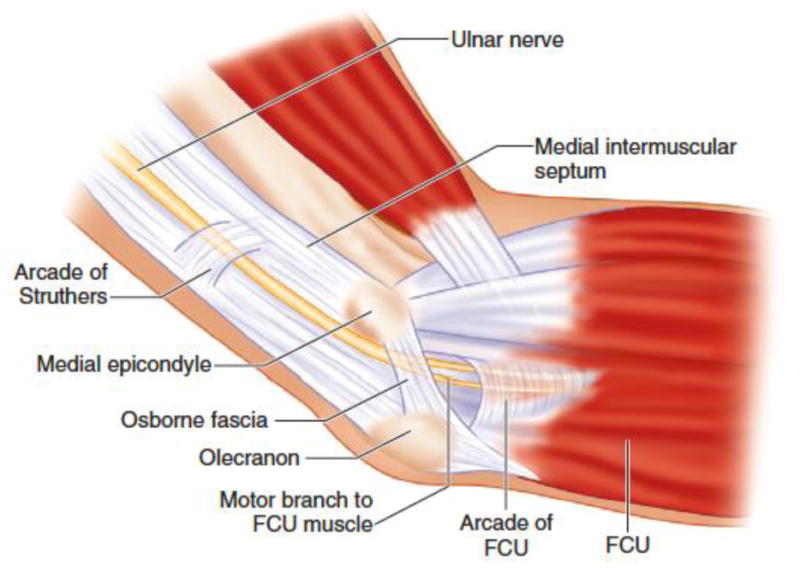
The ulnar nerve is derived from the ventral rami of cervical roots of C8 and T1 and becomes the terminal branch of the medial cord of the brachial plexus. The ulnar nerve then courses between the medial head of the triceps and the brachialis muscles. It travels posterior or medial to the brachial artery and posterior to the intramuscular septum. Approximately 8 cm from the medial epicondyle, the nerve is surrounded by the arcade of Struthers, which is a fascial band that connects the medial head of the triceps and the intramuscular septum. Here, it becomes superficial and pierces the medial intramuscular septum and enters the ulnar sulcus. It courses posterior to the medial condyle and medial to the olecranon and enters the cubital tunnel. The roof of the cubital tunnel is formed by Osborne's ligament. This is a thickened band between the humeral and ulnar head of the FCU. The medial collateral ligament of the elbow, elbow joint capsule and olecranon make up the floor of the tunnel. Once through the cubital tunnel, the ulnar nerve travels deep to the humeral and ulnar heads of the FCU in the forearm. It goes through the FCU to the deep flexor-pronator aponeurosis distally. From Lin PY, Sandeep SJ, Chung KC. In situ cubital tunnel decompression. In: Chung KC, editor. Operative techniques: hand and wrist surgery. vol.2. Philadelphia: Elsevier Saunders; 2012; with permission.
Figure 3. Topography of medial antecubital cutaneous (MABC) nerve.
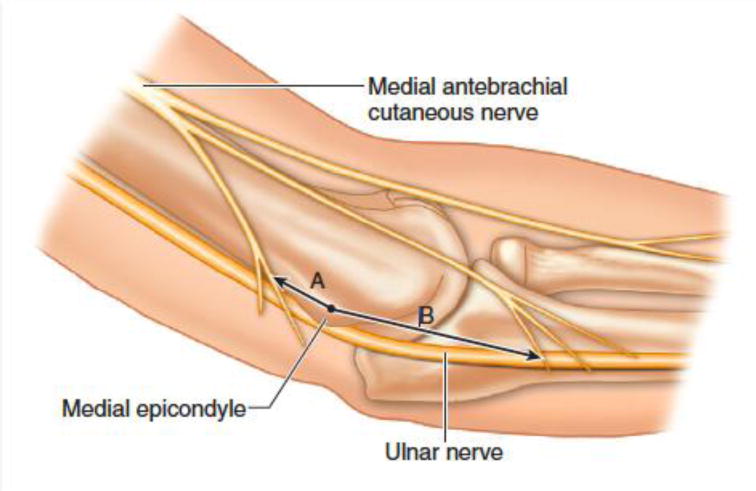
The proximal crossing branch is found approximately 1.8 cm proximal to the medial epicondyle while the distal crossing branch lies approximately 3.1 cm distal to the medial epicondyle. From Lin PY, Sandeep SJ, Chung KC. In situ cubital tunnel decompression. In: Chung KC, editor. Operative techniques: hand and wrist surgery. vol. 2. Philadelphia: Elsevier Saunders; 2012; with permission.)
Postoperative complications
A description of potential postoperative complications and etiologies of treatment failures are outlined in Table 1. Superficial and/or deep space infections are uncommon, and occur in only 0.4% of cases. Currently, perioperative antibiotic prophylaxis and operating room sterility is not indicated for CTR procedures, given the low rates of perioperative infection. 24,25 Symptomatic hypertrophic scarring and hypothenar “pillar” pain are more frequent, and have been correlated with perioperative mood disturbance. However, symptoms typically subside within 3 months, and can be managed by nonoperative techniques.26 The incidence of pathologic pain syndromes, including complex regional pain syndrome (CRPS), has been described in up to 8% of patients following CTR.27,28 Early recognition and referral to specialists experienced in the management of pathologic pain syndromes and CRPS is critical to prevent the propagation of symptoms and permanent disability. Less commonly, flexor tendon complications have been described following division of the transverse carpal ligament, including bowstringing, adhesions and triggering. 29,30 Finally, wrist instability and pisotriquetral arthrosis has been reported in approximately 2% of patients, which can often be managed successfully with splinting, anti-inflammatory agents, and steroid injections. For those patients who have failed nonoperative measures, pisiform excision can be considered. 31
Table 1. Complications of carpal tunnel release (CTR).
| Complication | Description |
|---|---|
| Injury to anatomic structures |
|
| Soft tissue complications |
|
| Pain |
|
| Other |
|
| Persistent symptoms |
|
Treatment Failure following CTR
Following carpal tunnel release, treatment failure can occur in up to 25% of patients, with approximately 12% of patients requiring secondary surgery. 1,32,33 Treatment failure refers to the presence of neuropathic symptoms, and can be considered in the following way: 1) persistent symptoms, 2) recurrent symptoms, or 3) the presence of an alternate diagnosis. 33 Persistent CTS refers to the presence of ongoing symptoms following CTR without improvement following release, and is more commonly encountered compared with recurrent symptoms. Persistent CTS following release is typically caused by an incomplete release of the flexor retinaculum distally or the antebrachial fascia proximally, and may be more common following endoscopic or limited incision techniques.33-36 However, other prospective, randomized controlled studies have failed to demonstrate a difference in the incidence of persistent symptoms following CTR by release technique. 37,38
Patients with recurrent CTS typically experience complete relief following primary release, but symptoms consistent with CTS recur after a period of at least 6 months or longer. The pathophysiology leading to recurrent CTS remains unclear, but is thought to be caused by scarring, fibrous proliferation, healing and reformation of the flexor retinaculum, or recurrent tenosynovitis.39 Extraneural scarring impairs epineural blood flow, impedes nerve gliding, and can result in recurrent compression on the nerve. Recurrent symptoms account for nearly 20% of all revision surgeries, and are more common among patients with hypertension and diabetes.39,40 It has been postulated that diabetes results in the glycosylation of connective tissues, increases collagen cross-linking, and causes stiffness and thickening of the transverse carpal ligament. Furthermore, microvascular disease associated with diabetes may render the median nerve more susceptible to injury by compression.41 Similarly, hypertension has been shown to be a risk factor for carpal tunnel syndrome. Although the physiologic mechanism by which hypertension leads to CTS remains unclear, it is thought to be related to the use of β-blockers and comorbid conditions associated with hypertension, such as diabetes and vascular disease. 40,42
Evaluation
Although adjunct diagnostic tests may be useful in the evaluation of patients with complications or treatment failure following CTR, a focused history and physical examination are the most important tools to guide the surgeon toward a treatment strategy. Patients who present with symptoms that are not congruent with prior symptoms of CTS should be evaluated for nerve injury or the presence of an alternative diagnosis. For example, patients with injury to the palmar cutaneous branch of the median nerve may present with localized numbness, hyperalgesia across the scar with a positive Tinel's sign along the course of the palmar cutaneous branch. Local anesthetic injection may help identify the lesion by temporary resolution of the discomfort.43 Conservative therapies such as desensitization, topical agents and Botulinum A injections may be initially helpful in suppressing symptoms.43,44 However, patients with persistent symptoms despite conservative measures should undergo neuroma resection of the affected palmar cutaneous branch and nerve transposition. Similarly, injury to the digital nerves may present with anesthesia of the affected digit, or neuroma formation in the palm. Treatment includes exploration and identification of the injury, with repair of the nerve or neuroma resection and nerve grafting as indicated. Progressive weakness with thenar atrophy may suggest injury to the recurrent motor branch of the median nerve. Hyperalgesia, trophic changes, edema and vasomotor asymmetries (i.e. temperature and skin changes) may suggest development of CRPS (complex regional pain syndrome).28
In addition to iatrogenic injury, the clinical examination can reveal alternate causes of symptoms. For example, the median nerve may be compressed more proximally in the forearm, such as at the ligament of Struthers (fibrous band between the medial epicondyle and supracondylar process), between the superficial and deep heads of the pronator teres, the arch of FDS, or the bicipital aponeurosis. Furthermore, vascular anomalies, tumors, Gantzer muscle (an accessory head of the flexor pollicis longus), palmaris profundus, or the presence of flexor carpi radialis brevis may all manifest with compressive symptoms.45 Additionally, spinal pathology, such as cervical radiculopathy, spinal cord lesions, and thoracic outlet syndrome may all mimic symptoms of carpal tunnel syndrome. Systemic diseases, such as diabetic neuropathy, thyroid conditions, and hemodialysis-dependent renal failure due to microglobulin amyloid deposits, related neurologic sequelae, may manifest with symptoms similar to that of CTS.46 Lesions resulting in a local mass effect at the carpal tunnel, such as ganglion cysts, arterial aneurysms, gouty tophi, amyloidosis, sarcoidosis, or fracture callus, may also results in diminished volume in the carpal canal and median nerve compression.
Among patients with no other competing diagnosis, it is critical to determine if the etiology of the treatment failure is due to the persistence or recurrence of symptoms following primary CTR. An interval of relief, followed by the recurrence of symptoms is suggestive of perineural fibrosis and scarring. Patients with persistent symptoms are more likely to have symptoms that mirror their symptoms prior to primary CTR, whereas patients with recurrence may be more likely to present with scar hypersensitivity and pain. 47,48 Standard provocative maneuvers, including carpal compression and wrist flexion testing may confirm the diagnosis of CTS, and provide information regarding the etiology of symptoms. (Table 2) 35,49,50 Although response to steroid injection has been shown to be well correlated with relief among patients with primary carpal tunnel syndrome, its utility among patients with recurrent or persistent symptoms is less clear.51 Recent evidence suggests that relief from steroid injection combined with positive provocative physical examination findings are predictive of relief for patients undergoing revision CTR for recurrent symptoms.50
Table 2. Diagnostic testing for carpal tunnel syndrome (CTS).
| Sensitivity (%) | Specificity (%) | |
|---|---|---|
| Hand diagram | 76 | 98 |
| Night pain | 96 | 100 |
| Phalen's | 75 | 95 |
| Tinel's | 64 | 99 |
| Durkan's | 89 | 91 |
| Semmes-Weinstein | 65 | 88 |
Data from Szabo, RM, Slater RR, Farver TB, et al. The value of diagnostic testing in carpal tunnel syndrome. J Hand Surg Am 1999;24(4):704-14.
Electrodiagnostic studies are useful to document the severity of compression, the presence of denervation of median nerve-innervated thenar musculature, and the presence of alternative locations of compression.1 Additionally, electrodiagnostic testing can provide an objective parameter for long-term follow-up. 35,52,53However, electrodiagnostic testing should not be taken in isolation, but rather in conjunction with the patient's clinical picture. For example, normal electrodiagnostic studies do not exclude the diagnosis of CTS, and electrodiagnostic studies can remain abnormal for a prolonged period of time following a successful surgical release.53,54 In this context, electrodiagnostic studies may not be helpful in diagnosing recurrent CTS given the persistence of electrical changes in nerve conduction and motor response even following successful release, but can provide information regarding prognosis, recovery, and the presence of additional areas of nerve compression or injury.50,55
Patients who have undergone prior CTR who present with persistent or recurrent symptoms should undergo plain radiographs to evaluate for the presence of fracture or dislocation contributing to compression on the median nerve. High-resolution ultrasonography may highlight the presence of space-occupying lesions contributing to median nerve compression, and can be further characterized with advanced imaging, such as MRI or CT, as indicated.56-58
Treatment options
In general, the decision to reoperate is based on signs and symptoms from the history and physical examination. For patients who present with clear signs of iatrogenic nerve injury (e.g. dense anesthesia, motor function loss), immediate nerve exploration is indicated. 43,59 A short course of conservative measures are helpful adjuncts for patients with persistent or recurrent symptoms following CTR, and include splinting, steroid injections, desensitization, and range of motion exercises to promote nerve and tendon gliding.35 However, the majority of patients with recalcitrant symptoms will surgical intervention.
Revision CTR is challenging, and robust evidence regarding the appropriate indications and timing is sparse. 50,60 The indications for reoperation include 1) persistent symptoms due to inadequate release of the flexor retinaculum or antebrachial fascia, 2) persistent symptoms due to more proximal nerve compression, 3) recurrent symptoms due to perineural scarring or reformation of the flexor retinaculum, and 4) suspected nerve injury. For patients who develop recurrent symptoms that at 1 year or longer following primary release, repeat carpal tunnel release is indicated. 35,59,61
Revision surgery begins with an extension of the previous incision both proximally and distally for adequate exposure and to identify the nerve in normal tissue planes away from the scar tissue. 33The incision should be extended proximally across the wrist crease, and created medially to the prior incision to enter the carpal canal along its ulnar aspect.62 The median nerve is identified proximally and distally. The dissection proceeds into the carpal canal, noting that the median nerve may be adherent to the underside of the flexor retinaculum.39,63 The transverse carpal ligament is explored, and released in its entirety.64 External neurolysis is performed to free the median nerve from surrounding scar, and internal neurolysis may also be required to visualize normal fascicular anatomy.33,35,39,59
Following nerve release and neurolysis, the surgeon should assess the favorability of the wound bed surrounding the median nerve. Substantial scarring and poor vascularity may impede nerve gliding and predispose patients toward recurrent symptoms. To augment soft tissue coverage, several local flaps have been described, including the hypothenar fat pad, synovial flap, abductor digiti minimi, or the palmaris brevis, and regional or free flaps, including radial forearm, omentum, and lateral arm flaps, which may promote neovascularization, decreasing scar reformation, and enhance nerve regeneration.65 Of these, the hypothenar fat pad is most commonly favored given its proximity to the wound bed, ease of dissection, and the robustness of the available tissue.66 Following neurolysis, dissection proceeds between the dermis of the hypothenar skin and underlying fat. After the ulnar neurovascular structures are identified, the fat pad is elevated and mobilized to a region between the median nerve and transverse carpal ligament. In 62 patients with recalcitrant CTS, 58 reported excellent results after undergoing carpal tunnel release, neurolysis, and hypothenar fat pad flap.65 In another study, 41 of 45 patients with recurrent CTS experienced resolution of pain following neurolysis and hypothenar fat pad flap.48 Recently, there has been growing enthusiasm for the use of vein grafts and synthetic substitutes to prevent scar formation following revision CTR and neurolysis. 67 Although these options may reduce operating room time and donor site morbidity, there is no evidence comparing the effectiveness of nerve wrapping with flap coverage, and synthetic options are substantially more expensive compared with autologous tissue coverage.64
Outcomes
Reported outcomes among patients with complications following carpal tunnel release vary widely. Some studies suggest that patients who are found to have an incomplete release of the transverse carpal ligament at reexploration have the most favorable prognosis, whereas patients with significant scarring and fibrosis fare much more poorly. 34,61 Similarly, patients who have undergone multiple revision procedures are less likely to experience relief, likely due to scarring and fibrosis in the wound bed.39 Furthermore, patient factors likely mediate outcomes. For example, Hulsizer et al. reported that only 18% of worker's compensation patients who underwent revision experienced improvement postoperatively, compared with 84% of patients with conventional insurance.34 Therefore, it is essential to counsel patients regarding the probability of achieving relief in order to appropriately set expectations following any revision surgery.
Cubital tunnel syndrome
Cubital tunnel syndrome (CuTS), or compression of the ulnar nerve at the elbow is the second most common compression neuropathy, and up to 75,000 decompression releases are performed in the United States yearly. (Figure 68,69 Although multiple strategies are described, no single technique has emerged as superior, and in situ decompression, and anterior transposition are most commonly performed.69,70 Nerve transpositions may be performed subcutaneously, intramuscularly (within the flexor-pronator mass) and submuscularly (beneath the flexor-pronator mass). Recently, endoscopic in situ releases have been described, with the possibility of similar effectiveness, and earlier return to work.71-74
Postoperative Complications
Outcomes following primary CuTR are generally favorable with good relief of symptoms in 80 to 90% of patients.2,3 Patient related risk factors such as pre-operative level of neuropathy, chronic neuropathy, older age (>50 years) and diabetes are associated with a poor prognosis following surgery. 3,52 For patients with severe, chronic ulnar nerve compression, persistent dysethesias and weakness are not uncommon and complete recovery is unlikely, which should be discussed among surgeons and patients to ensure realistic patient expectations following release.75 Therefore, discerning the best management for failed CuTR relies on appropriate diagnostic evaluation, patient counseling, careful operative approach, and discussion of the prognosis to address patient expectations. Table 3 provides an overview of complications described following CuTR.
Table 3. Complications of cubital tunnel release (CuTR).
| Prevention strategies | Treatment options | |
|---|---|---|
| Iatrogenic injury to MABC nerve | 1) Knowledge of anatomy: 1.8 cm proximal to medial epicondyle and 3.1 cm distal to medial epicondyle (FIGURE 2)2) Short 3-5 cm skin incisions |
|
| Nerve subluxation | 1) Secure ulnar nerve in its groove with subcutaneous tissue and feeding vessels2) Check thoroughly intra-op by moving arm in various ways |
|
| Recurrent symptoms | 1) Check for all possible sites of compression |
|
Nerve subluxation
Nerve subluxation is the most common cause of failed CuTR, reported in 2.4 to 20% of cases.76-78 To prevent subluxation during an in situ release, the ulnar nerve should remain within its groove, and circumferential dissection should be avoided to prevent disruption of the surrounding areolar tissue and feeding blood vessels. Only the compressive fascial bands are released without neurolysis to avoid destabilizing the ulnar nerve. Following release, the elbow should be manipulated to check for subluxation, and anterior transposition should be performed if subluxation is noted.13,69,76,78
Treatment failure
Neuropathic symptoms in the distribution of the ulnar nerve occur in up to 30% of patients following CuTR, primarily due to inadequate release, most commonly at the medial intermuscular septum, or perineural fibrosis.2,79,80 Pain radiating from the elbow scar to the small and ring fingers with numbness suggests recurrent compression, whereas patients who have persistent symptoms due to inadequate release do not experience any resolution in their symptoms. 81 In contrast, patients who may have recurrent symptoms due to perineural fibrosis may experience resolution of their symptoms initially, with symptom reappearance over time.
Iatrogenic Injury
Iatrogenic to the medial antebrachial cutaneous (MABC) nerve has been reported as the leading cause of pain following cubital tunnel release (CuTR). (Figure 5)81 In a study examining intraoperative findings in revision cubital tunnel releases, nearly 73 of 100 cases (had injury to the MABC nerve.82 Pain in the scar associated with numbness in the posterior and medial elbow region is indicative of a neuroma of the MABC. Patients with a painful neuroma also experience radiating pain along the MABC territory with light tapping on the painful spot and experience pain relief and improvement in elbow function following a small injection of local anesthetic.83 Initial management involves a six-month trial of conservative measures with local massage, physiotherapy and desensitization. If there is no significant improvement, the neuroma should be resected, and “cap” the ends of the nerve via electrocautery to prevent reformation of neuroma.81-83 Microsurgical repair of the nerve has also been described,78 although no studies have compared the effectiveness of repair versus resection.
Approach to revision cubital tunnel release
Failed release of the cubital tunnel is more frequent than carpal tunnel, and is also fraught with more challenges during revision surgery. Surgical options for failed cubital tunnel release include subcutaneous transposition, intramuscular transposition, submuscular transposition and medial epicondylectomy. Secondary procedures largely depend on the technique was used during the primary release (in situ release vs. transposition). Similar to the approach for revision carpal tunnel, the elbow incision should be extended proximally and distally to maximize visualization of the nerve, while protecting the posterior branches of the MABC nerve. Exploration should include examination of MABC branches to rule out neuroma, and evaluation for any evidence of nerve subluxation. If the primary procedure was an in situ decompression, the ulnar nerve may be scarred, entrapped proximally (intermuscular septum) or distally (flexor carpi ulnaris), or subluxing over the medial epicondyle. The nerve should be released in an extended fashion, and external neurolysis is performed. Following external neurolysis, a transposition procedure should be performed. Currently, there are no comparative studies examining the effectiveness of transposition techniques (subcutaneous, intramuscular, submuscular) among patients with recurrent cubital tunnel syndrome. 84 If the index procedure was a subcutaneous transposition, the nerve is usually found scarred along the medial epicondyle. After releasing the compression points, an intramuscular or submuscular transposition can be performed. Likewise, if a subcutaneous transposition was performed, the nerve should be dissected free prior to an intramuscular or submuscular transposition. Recently, there has been enthusiasm for creating a new soft tissue bed for the nerve by wrapping the ulnar nerve with vein or bioengineered synthetic devices to improve nerve gliding and minimize perineural fibrosis.69 Although these adjuncts have shown encouraging results, comparative studies are not yet available.85,86
Outcomes
Compared with revision procedures for carpal tunnel syndrome, the outcomes following revision CuTR are much less predictable. The reasons for this are likely multifactorial. For example, ulnar nerve compression at the elbow often presents much later compared with other nerve compression conditions, and patients are more likely to have advanced, irreversible neuropathic changes. Furthermore, previous submuscular transposition, older age, and severe pain are poor prognostic indicators.87 Although few patients experience complete relief, the majority of patients report some improvement in symptoms following revision procedures.88
Summary
Surgery for upper extremity compressive neuropathies is relatively common. In order to prevent iatrogenic injury, it is imperative for the surgeon to be aware of the structures associated with normal surgical anatomy and of those that are common variants. In addition, recurrent or persistent symptoms following a release are commonly associated with inadequate release, but can be associated with misdiagnosis. For either of these etiologies for failed decompression, it is crucial to perform a thorough history and physical examination with provocative testing. Advanced diagnostic testing such as EMG may be helpful for comparison if nerve injury is suspected, especially if a pre-operative study was conducted. Revision procedures can provide relief for many patients who present with recurrent or persistent symptoms, although the outcomes are less predictable compared with primary release.
Key Points.
Prevention of complications begins with a solid understanding of the normal anatomy and anatomical variations that may exist.
Carpal tunnel release (CTR) is among the most common hand surgical procedures performed, but complications occur in up to 25% of cases.1 Revision carpal tunnel surgery may be indicated in patients who present with recurrent, persistent, or new symptoms due to inadequate release, iatrogenic injury, recurrent symptoms, or perineural fibrosis.
Cubital tunnel syndrome (CuTS) is the second most common compressive neuropathy, but recurrence or failed decompression occurs in 25-35% of patients.2,3 Frequently reported complications include injury to the medial antebrachial cutaneous (MABC) nerve, ulnar nerve subluxation, and recurrent symptoms because of inadequate release or perineural fibrosis.
Acknowledgments
Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) to Dr. Kevin C. Chung.
Footnotes
Disclosures: None
References
- 1.Neuhaus V, Christoforou D, Cheriyan T, Mudgal CS. Evaluation and treatment of failed carpal tunnel release. The Orthopedic clinics of North America. 2012 Oct;43(4):439–447. doi: 10.1016/j.ocl.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Dellon AL. Review of treatment results for ulnar nerve entrapment at the elbow. J Hand Surg Am. 1989 Jul;14(4):688–700. doi: 10.1016/0363-5023(89)90192-5. [DOI] [PubMed] [Google Scholar]
- 3.Mowlavi A, Andrews K, Lille S, Verhulst S, Zook EG, Milner S. The management of cubital tunnel syndrome: a meta-analysis of clinical studies. Plast Reconstr Surg. 2000 Aug;106(2):327–334. doi: 10.1097/00006534-200008000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Shiri R. The prevalence and incidence of carpal tunnel syndrome in US working populations. Scandinavian journal of work, environment & health. 2014 Jan;40(1):101–102. doi: 10.5271/sjweh.3404. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka S, Wild DK, Seligman PJ, Behrens V, Cameron L, Putz-Anderson V. The US prevalence of self-reported carpal tunnel syndrome: 1988 National Health Interview Survey data. Am J Public Health. 1994 Nov;84(11):1846–1848. doi: 10.2105/ajph.84.11.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosen I. Prevalence of carpal tunnel syndrome in a general population. Jama. 1999 Jul 14;282(2):153–158. doi: 10.1001/jama.282.2.153. [DOI] [PubMed] [Google Scholar]
- 7.Leinberry CF, Rivlin M, Maltenfort M, et al. Treatment of carpal tunnel syndrome by members of the American Society for Surgery of the Hand: a 25-year perspective. J Hand Surg Am. 2012 Oct;37(10):1997–2003. doi: 10.1016/j.jhsa.2012.07.016. e1993. [DOI] [PubMed] [Google Scholar]
- 8.Lanz U. Anatomical variations of the median nerve in the carpal tunnel. J Hand Surg Am. 1977 Jan;2(1):44–53. doi: 10.1016/s0363-5023(77)80009-9. [DOI] [PubMed] [Google Scholar]
- 9.Mitchell R, Chesney A, Seal S, McKnight L, Thoma A. Anatomical variations of the carpal tunnel structures. The Canadian journal of plastic surgery = Journal canadien de chirurgie plastique. 2009 Fall;17(3):e3–7. [PMC free article] [PubMed] [Google Scholar]
- 10.Hurwitz PJ. Variations in the course of the thenar motor branch of the median nerve. J Hand Surg Br. 1996 Jun;21(3):344–346. doi: 10.1016/s0266-7681(05)80198-6. [DOI] [PubMed] [Google Scholar]
- 11.DaSilva MF, Moore DC, Weiss AP, Akelman E, Sikirica M. Anatomy of the palmar cutaneous branch of the median nerve: clinical significance. J Hand Surg Am. 1996 Jul;21(4):639–643. doi: 10.1016/S0363-5023(96)80018-9. [DOI] [PubMed] [Google Scholar]
- 12.Taleisnik J. The palmar cutaneous branch of the median nerve and the approach to the carpal tunnel. An anatomical study. J Bone Joint Surg Am. 1973 Sep;55(6):1212–1217. [PubMed] [Google Scholar]
- 13.Chung KC. Operative Techniques: Hand and Wrist Surgery. Vol. 2. Elsevier Saunders; 2012. [Google Scholar]
- 14.De Smet L, Fabry G. Transection of the motor branch of the ulnar nerve as a complication of two-portal endoscopic carpal tunnel release: a case report. J Hand Surg Am. 1995 Jan;20(1):18–19. doi: 10.1016/s0363-5023(05)80050-4. [DOI] [PubMed] [Google Scholar]
- 15.Luallin SR, Toby EB. Incidental Guyon's canal release during attempted endoscopic carpal tunnel release: an anatomical study and report of two cases. Arthroscopy. 1993;9(4):382–386. doi: 10.1016/s0749-8063(05)80311-1. discussion 381. [DOI] [PubMed] [Google Scholar]
- 16.Nath RK, Mackinnon SE, Weeks PM. Ulnar nerve transection as a complication of two-portal endoscopic carpal tunnel release: a case report. J Hand Surg Am. 1993 Sep;18(5):896–898. doi: 10.1016/0363-5023(93)90063-9. [DOI] [PubMed] [Google Scholar]
- 17.Terrono AL, Belsky MR, Feldon PG, Nalebuff EA. Injury to the deep motor branch of the ulnar nerve during carpal tunnel release. J Hand Surg Am. 1993 Nov;18(6):1038–1040. doi: 10.1016/0363-5023(93)90399-N. [DOI] [PubMed] [Google Scholar]
- 18.Boeckstyns ME, Sorensen AI. Does endoscopic carpal tunnel release have a higher rate of complications than open carpal tunnel release? An analysis of published series. J Hand Surg Br. 1999 Feb;24(1):9–15. doi: 10.1016/s0266-7681(99)90009-8. [DOI] [PubMed] [Google Scholar]
- 19.Shinya K, Lanzetta M, Conolly WB. Risk and complications in endoscopic carpal tunnel release. J Hand Surg Br. 1995 Apr;20(2):222–227. doi: 10.1016/s0266-7681(05)80056-7. [DOI] [PubMed] [Google Scholar]
- 20.Benson LS, Bare AA, Nagle DJ, Harder VS, Williams CS, Visotsky JL. Complications of endoscopic and open carpal tunnel release. Arthroscopy. 2006 Sep;22(9):919–924. 924 e911–912. doi: 10.1016/j.arthro.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 21.Michelotti B, Romanowsky D, Hauck RM, Prospective Randomized. Evaluation of Endoscopic Versus Open Carpal Tunnel Release in Bilateral Carpal Tunnel Syndrome: An Interim Analysis. Ann Plast Surg. 2014 Aug 28; doi: 10.1097/SAP.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 22.Larsen MB, Sorensen AI, Crone KL, Weis T, Boeckstyns ME. Carpal tunnel release: a randomized comparison of three surgical methods. J Hand Surg Eur Vol. 2013 Jul;38(6):646–650. doi: 10.1177/1753193412475247. [DOI] [PubMed] [Google Scholar]
- 23.Vasiliadis HS, Georgoulas P, Shrier I, Salanti G, Scholten RJ. Endoscopic release for carpal tunnel syndrome. Cochrane Database Syst Rev. 2014(1):CD008265. doi: 10.1002/14651858.CD008265.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leblanc MR, Lalonde DH, Thoma A, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y) 2011 Mar;6(1):60–63. doi: 10.1007/s11552-010-9301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harness NG, Inacio MC, Pfeil FF, Paxton LW. Rate of infection after carpal tunnel release surgery and effect of antibiotic prophylaxis. J Hand Surg Am. 2010 Feb;35(2):189–196. doi: 10.1016/j.jhsa.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 26.Kim JK, Kim YK. Predictors of scar pain after open carpal tunnel release. J Hand Surg Am. 2011 Jun;36(6):1042–1046. doi: 10.1016/j.jhsa.2011.03.036. [DOI] [PubMed] [Google Scholar]
- 27.da Costa VV, de Oliveira SB, Fernandes Mdo C, Saraiva RA. Incidence of regional pain syndrome after carpal tunnel release. Is there a correlation with the anesthetic technique? Revista brasileira de anestesiologia. Jul-Aug. 2011;61(4):425–433. doi: 10.1016/S0034-7094(11)70050-2. [DOI] [PubMed] [Google Scholar]
- 28.Carroll I, Curtin CM. Management of chronic pain following nerve injuries/CRPS type II. Hand Clin. 2013 Aug;29(3):401–408. doi: 10.1016/j.hcl.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 29.Netscher D, Dinh T, Cohen V, Thornby J. Division of the transverse carpal ligament and flexor tendon excursion: open and endoscopic carpal tunnel release. Plast Reconstr Surg. 1998 Sep;102(3):773–778. doi: 10.1097/00006534-199809030-00023. [DOI] [PubMed] [Google Scholar]
- 30.Lee SK, Bae KW, Choy WS. The relationship of trigger finger and flexor tendon volar migration after carpal tunnel release. J Hand Surg Eur Vol. 2014 Sep;39(7):694–698. doi: 10.1177/1753193413479506. [DOI] [PubMed] [Google Scholar]
- 31.Stahl S, Stahl S, Calif E. Latent pisotriquetral arthrosis unmasked following carpal tunnel release. Orthopedics. 2010 Sep;33(9):673. doi: 10.3928/01477447-20100722-06. [DOI] [PubMed] [Google Scholar]
- 32.Cobb TK, Amadio PC. Reoperation for carpal tunnel syndrome. Hand Clin. 1996 May;12(2):313–323. [PubMed] [Google Scholar]
- 33.Tung TH, Mackinnon SE. Secondary carpal tunnel surgery. Plast Reconstr Surg. 2001 Jun;107(7):1830–1843. doi: 10.1007/978-3-540-49008-1_40. quiz 1844,1933. [DOI] [PubMed] [Google Scholar]
- 34.Hulsizer DL, Staebler MP, Weiss AP, Akelman E. The results of revision carpal tunnel release following previous open versus endoscopic surgery. J Hand Surg Am. 1998 Sep;23(5):865–869. doi: 10.1016/S0363-5023(98)80164-0. [DOI] [PubMed] [Google Scholar]
- 35.Jones NF, Ahn HC, Eo S. Revision surgery for persistent and recurrent carpal tunnel syndrome and for failed carpal tunnel release. Plast Reconstr Surg. 2012 Mar;129(3):683–692. doi: 10.1097/PRS.0b013e3182402c37. [DOI] [PubMed] [Google Scholar]
- 36.Forman DL, Watson HK, Caulfield KA, Shenko J, Caputo AE, Ashmead D. Persistent or recurrent carpal tunnel syndrome following prior endoscopic carpal tunnel release. J Hand Surg Am. 1998 Nov;23(6):1010–1014. doi: 10.1016/s0363-5023(98)80008-7. [DOI] [PubMed] [Google Scholar]
- 37.Atroshi I, Hofer M, Larsson GU, Ornstein E, Johnsson R, Ranstam J. Open compared with 2-portal endoscopic carpal tunnel release: a 5-year follow-up of a randomized controlled trial. J Hand Surg Am. 2009 Feb;34(2):266–272. doi: 10.1016/j.jhsa.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 38.Chen L, Duan X, Huang X, Lv J, Peng K, Xiang Z. Effectiveness and safety of endoscopic versus open carpal tunnel decompression. Arch Orthop Trauma Surg. 2014 Apr;134(4):585–593. doi: 10.1007/s00402-013-1898-z. [DOI] [PubMed] [Google Scholar]
- 39.Zieske L, Ebersole GC, Davidge K, Fox I, Mackinnon SE. Revision carpal tunnel surgery: a 10-year review of intraoperative findings and outcomes. J Hand Surg Am. 2013 Aug;38(8):1530–1539. doi: 10.1016/j.jhsa.2013.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schreiber JE, Foran MP, Schreiber DJ, Wilgis EF. Common risk factors seen in secondary carpal tunnel surgery. Ann Plast Surg. 2005 Sep;55(3):262–265. doi: 10.1097/01.sap.0000174358.62299.1b. [DOI] [PubMed] [Google Scholar]
- 41.Fitzgibbons PG, Weiss AP. Hand manifestations of diabetes mellitus. J Hand Surg Am. 2008 May-Jun;33(5):771–775. doi: 10.1016/j.jhsa.2008.01.038. [DOI] [PubMed] [Google Scholar]
- 42.Emara MK, Saadah AM. The carpal tunnel syndrome in hypertensive patients treated with beta-blockers. Postgraduate medical journal. 1988 Mar;64(749):191–192. doi: 10.1136/pgmj.64.749.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Braun RM, Rechnic M, Fowler E. Complications related to carpal tunnel release. Hand Clin. 2002 May;18(2):347–357. doi: 10.1016/s0749-0712(01)00013-0. [DOI] [PubMed] [Google Scholar]
- 44.Ranoux D, Attal N, Morain F, Bouhassira D. Botulinum toxin type A induces direct analgesic effects in chronic neuropathic pain. Annals of neurology. 2008 Sep;64(3):274–283. doi: 10.1002/ana.21427. [DOI] [PubMed] [Google Scholar]
- 45.Mazurek MT, Shin AY. Upper extremity peripheral nerve anatomy: current concepts and applications. Clinical orthopaedics and related research. 2001 Feb;(383):7–20. doi: 10.1097/00003086-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Kwon HK, Pyun SB, Cho WY, Boo CS. Carpal tunnel syndrome and peripheral polyneuropathy in patients with end stage kidney disease. Journal of Korean medical science. 2011 Sep;26(9):1227–1230. doi: 10.3346/jkms.2011.26.9.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stutz N, Gohritz A, van Schoonhoven J, Lanz U. Revision surgery after carpal tunnel release--analysis of the pathology in 200 cases during a 2 year period. J Hand Surg Br. 2006 Feb;31(1):68–71. doi: 10.1016/j.jhsb.2005.09.022. [DOI] [PubMed] [Google Scholar]
- 48.Mathoulin C, Bahm J, Roukoz S. Pedicled hypothenar fat flap for median nerve coverage in recalcitrant carpal tunnel syndrome. Hand Surg. 2000 Jul;5(1):33–40. doi: 10.1142/s0218810400000120. [DOI] [PubMed] [Google Scholar]
- 49.De Smet L. Recurrent carpal tunnel syndrome. Clinical testing indicating incomplete section of the flexor retinaculum. J Hand Surg Br. 1993 Apr;18(2):189. doi: 10.1016/0266-7681(93)90105-o. [DOI] [PubMed] [Google Scholar]
- 50.Beck JD, Brothers JG, Maloney PJ, Deegan JH, Tang X, Klena JC. Predicting the outcome of revision carpal tunnel release. J Hand Surg Am. 2012 Feb;37(2):282–287. doi: 10.1016/j.jhsa.2011.10.040. [DOI] [PubMed] [Google Scholar]
- 51.Edgell SE, McCabe SJ, Breidenbach WC, LaJoie AS, Abell TD. Predicting the outcome of carpal tunnel release. J Hand Surg Am. 2003 Mar;28(2):255–261. doi: 10.1053/jhsu.2003.50031. [DOI] [PubMed] [Google Scholar]
- 52.Gellman H, Gelberman RH, Tan AM, Botte MJ. Carpal tunnel syndrome. An evaluation of the provocative diagnostic tests. J Bone Joint Surg Am. 1986 Jun;68(5):735–737. [PubMed] [Google Scholar]
- 53.Szabo RM, Slater RR, Jr, Farver TB, Stanton DB, Sharman WK. The value of diagnostic testing in carpal tunnel syndrome. J Hand Surg Am. 1999 Jul;24(4):704–714. doi: 10.1053/jhsu.1999.0704. [DOI] [PubMed] [Google Scholar]
- 54.Stutz NM, Gohritz A, Novotny A, Falkenberg U, Lanz U, van Schoonhoven J. Clinical and electrophysiological comparison of different methods of soft tissue coverage of the median nerve in recurrent carpal tunnel syndrome. Neurosurgery. 2008 Mar;62(3 Suppl 1):194–199. doi: 10.1227/01.neu.0000317393.06680.7d. discussion 199-200. [DOI] [PubMed] [Google Scholar]
- 55.Melvin JL, Johnson EW, Duran R. Electrodiagnosis after surgery for the carpal tunnel syndrome. Arch Phys Med Rehabil. 1968 Sep;49(9):502–507. [PubMed] [Google Scholar]
- 56.Campagna R, Pessis E, Feydy A, et al. MRI assessment of recurrent carpal tunnel syndrome after open surgical release of the median nerve. AJR American journal of roentgenology. 2009 Sep;193(3):644–650. doi: 10.2214/AJR.08.1433. [DOI] [PubMed] [Google Scholar]
- 57.Wu HT, Schweitzer ME, Culp RW. Potential MR signs of recurrent carpal tunnel syndrome: initial experience. Journal of computer assisted tomography. 2004 Nov-Dec;28(6):860–864. doi: 10.1097/00004728-200411000-00024. [DOI] [PubMed] [Google Scholar]
- 58.Pastare D, Therimadasamy AK, Lee E, Wilder-Smith EP. Sonography versus nerve conduction studies in patients referred with a clinical diagnosis of carpal tunnel syndrome. Journal of clinical ultrasound : JCU. 2009 Sep;37(7):389–393. doi: 10.1002/jcu.20601. [DOI] [PubMed] [Google Scholar]
- 59.Mosier BA, Hughes TB. Recurrent carpal tunnel syndrome. Hand Clin. 2013 Aug;29(3):427–434. doi: 10.1016/j.hcl.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 60.Amadio PC. Interventions for recurrent/persistent carpal tunnel syndrome after carpal tunnel release. J Hand Surg Am. 2009 Sep;34(7):1320–1322. doi: 10.1016/j.jhsa.2009.04.031. [DOI] [PubMed] [Google Scholar]
- 61.O'Malley MJ, Evanoff M, Terrono AL, Millender LH. Factors that determine reexploration treatment of carpal tunnel syndrome. J Hand Surg Am. 1992 Jul;17(4):638–641. doi: 10.1016/0363-5023(92)90307-b. [DOI] [PubMed] [Google Scholar]
- 62.Dellon AL, Chang BW. An alternative incision for approaching recurrent median nerve compression at the wrist. Plast Reconstr Surg. 1992 Mar;89(3):576–578. [PubMed] [Google Scholar]
- 63.Green DP, Wolfe SW. Green's operative hand surgery. 6th. Philadelphia: Elsevier/Churchill Livingstone; 2011. http://proxy.lib.umich.edu/login?url=https://www.clinicalkey.com/dura/browse/bookChapter/3-s2.0-C20091589800. [Google Scholar]
- 64.Abzug JM, Jacoby SM, Osterman AL. Surgical options for recalcitrant carpal tunnel syndrome with perineural fibrosis. Hand (N Y) 2012 Mar;7(1):23–29. doi: 10.1007/s11552-012-9391-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Strickland JW, Idler RS, Lourie GM, Plancher KD. The hypothenar fat pad flap for management of recalcitrant carpal tunnel syndrome. J Hand Surg Am. 1996 Sep;21(5):840–848. doi: 10.1016/S0363-5023(96)80201-2. [DOI] [PubMed] [Google Scholar]
- 66.Soltani AM, Allan BJ, Best MJ, Mir HS, Panthaki ZJ. A systematic review of the literature on the outcomes of treatment for recurrent and persistent carpal tunnel syndrome. Plast Reconstr Surg. 2013 Jul;132(1):114–121. doi: 10.1097/PRS.0b013e318290faba. [DOI] [PubMed] [Google Scholar]
- 67.Chou KH, Papadimitriou NG, Sarris I, Sotereanos DG. Neovascularization and other histopathologic findings in an autogenous saphenous vein wrap used for recalcitrant carpal tunnel syndrome: a case report. J Hand Surg Am. 2003 Mar;28(2):262–266. doi: 10.1053/jhsu.2003.50029. [DOI] [PubMed] [Google Scholar]
- 68.Fowler JR. Endoscopic Cubital Tunnel Release. J Hand Surg Am. 2014 Oct;39(10):2064–2066. doi: 10.1016/j.jhsa.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 69.Palmer BA, Hughes TB. Cubital tunnel syndrome. J Hand Surg Am. 2010 Jan;35(1):153–163. doi: 10.1016/j.jhsa.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 70.Zlowodzki M, Chan S, Bhandari M, Kalliainen L, Schubert W. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2007 Dec;89(12):2591–2598. doi: 10.2106/JBJS.G.00183. [DOI] [PubMed] [Google Scholar]
- 71.Tsai TM, Bonczar M, Tsuruta T, Syed SA. A new operative technique: cubital tunnel decompression with endoscopic assistance. Hand Clin. 1995 Feb;11(1):71–80. [PubMed] [Google Scholar]
- 72.Cobb TK, Walden AL, Merrell PT, Lemke JH. Setting expectations following endoscopic cubital tunnel release. Hand (N Y) 2014 Sep;9(3):356–363. doi: 10.1007/s11552-014-9629-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cobb TK, Sterbank PT, Lemke JH. Endoscopic cubital tunnel recurrence rates. Hand (N Y) 2010 Jun;5(2):179–183. doi: 10.1007/s11552-009-9227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hoffmann R, Siemionow M. The endoscopic management of cubital tunnel syndrome. J Hand Surg Br. 2006 Feb;31(1):23–29. doi: 10.1016/j.jhsb.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 75.Ruchelsman DE, Lee SK, Posner MA. Failed surgery for ulnar nerve compression at the elbow. Hand Clin. 2007 Aug;23(3):359–371. vi–vii. doi: 10.1016/j.hcl.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 76.Bartels RH, Menovsky T, Van Overbeeke JJ, Verhagen WI. Surgical management of ulnar nerve compression at the elbow: an analysis of the literature. Journal of neurosurgery. 1998 Nov;89(5):722–727. doi: 10.3171/jns.1998.89.5.0722. [DOI] [PubMed] [Google Scholar]
- 77.LeRoux PD, Ensign TD, Burchiel KJ. Surgical decompression without transposition for ulnar neuropathy: factors determining outcome. Neurosurgery. 1990 Nov;27(5):709–714. doi: 10.1097/00006123-199011000-00007. discussion 714. [DOI] [PubMed] [Google Scholar]
- 78.Nellans K, Tang P. Evaluation and treatment of failed ulnar nerve release at the elbow. The Orthopedic clinics of North America. 2012 Oct;43(4):487–494. doi: 10.1016/j.ocl.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 79.Holzner B, Kemmler G, Kopp M, et al. Preoperative expectations and postoperative quality of life in liver transplant survivors. Archives of Physical Medicine & Rehabilitation. 2001 Jan;82(1):73–79. doi: 10.1053/apmr.2001.19013. [DOI] [PubMed] [Google Scholar]
- 80.Hambleton RK, Swaminathan H, Rogers HJ. Fundamentals of Item Response Theory. Newbury Park, CA: SAGE Publications, Inc; 1991. [Google Scholar]
- 81.Dellon AL, MacKinnon SE. Injury to the medial antebrachial cutaneous nerve during cubital tunnel surgery. J Hand Surg Br. 1985 Feb;10(1):33–36. doi: 10.1016/s0266-7681(85)80011-5. [DOI] [PubMed] [Google Scholar]
- 82.Mackinnon SE, Novak CB. Operative findings in reoperation of patients with cubital tunnel syndrome. Hand (N Y) 2007 Sep;2(3):137–143. doi: 10.1007/s11552-007-9037-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stahl S, Rosenberg N. Surgical treatment of painful neuroma in medial antebrachial cutaneous nerve. Ann Plast Surg. 2002 Feb;48(2):154–158. doi: 10.1097/00000637-200202000-00007. discussion 158-160. [DOI] [PubMed] [Google Scholar]
- 84.Ehsan A, Hanel DP. Recurrent or persistent cubital tunnel syndrome. J Hand Surg Am. 2012 Sep;37(9):1910–1912. doi: 10.1016/j.jhsa.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 85.Varitimidis SE, Vardakas DG, Goebel F, Sotereanos DG. Treatment of recurrent compressive neuropathy of peripheral nerves in the upper extremity with an autologous vein insulator. J Hand Surg Am. 2001 Mar;26(2):296–302. doi: 10.1053/jhsu.2001.22528. [DOI] [PubMed] [Google Scholar]
- 86.Puckett BN, Gaston RG, Lourie GM. A novel technique for the treatment of recurrent cubital tunnel syndrome: ulnar nerve wrapping with a tissue engineered bioscaffold. J Hand Surg Eur Vol. 2011 Feb;36(2):130–134. doi: 10.1177/1753193410384690. [DOI] [PubMed] [Google Scholar]
- 87.Gabel GT, Amadio PC. Reoperation for failed decompression of the ulnar nerve in the region of the elbow. J Bone Joint Surg Am. 1990 Feb;72(2):213–219. [PubMed] [Google Scholar]
- 88.Aleem AW, Krogue JD, Calfee RP. Outcomes of revision surgery for cubital tunnel syndrome. J Hand Surg Am. 2014 Nov;39(11):2141–2149. doi: 10.1016/j.jhsa.2014.07.013. [DOI] [PubMed] [Google Scholar]


