Abstract
The kindling hypothesis for depression predicts that with more recurrences, the interval between successive recurrences decreases. Studies with unipolar and bipolar samples generally have been consistent with this premise. However, previous research is subject to a statistical artifact. Slater’s fallacy maintains that these intermorbid intervals appear to decrease because highly recurrent individuals with consistently shorter intervals become a larger proportion of the remaining sample with each recurrence. Correcting for this bias, research on bipolar disorder no longer evidences such an effect. We predicted similar results for unipolar depression when correcting for this bias, and proposed an alternative model: individuals who are highly recurrent have consistently shorter intermorbid periods, even following the very first lifetime episode. As predicted, correcting for Slater’s fallacy removed the appearance of decreasing intermorbid intervals. Further, highly recurrent individuals exhibited shorter intermorbid intervals in general, and for the very first interval, supporting the alternative model.
Keywords: UNIPOLAR DEPRESSION, KINDLING, LIFE EVENTS, LIFE STRESS, CYCLE ACCELERATION
Major depression is a debilitating condition, made even more formidable through its often recurrent and chronic nature. Estimates of how many first-time depressed individuals will have future episodes range from 40 to 60 percent (Monroe & Harkness, 2011). Those with a more recurrent course also are likely to develop other serious problems, including functional brain impairment, health difficulties, hospital stays, and suicide attempts (Ferguson, Boden, & Horwood, 2007; Greden, 2001; Sheline, Wang, Gado, Csernansky, & Vannier, 1996).
Two general models have been advanced to account for the recurrent nature of major depression (Monroe & Harkness, 2005). First, a ‘stable liability’ model holds that vulnerability factors existing prior to the first lifetime depressive episode remain following recovery, signifying an ongoing heightened biological predisposition to future episodes (e.g., Burcusa & Iacono, 2007). In contrast, a second ‘acquired susceptibility’ model revolves around the premise of an increasing susceptibility to future recurrences that derives from the stress and experiences associated with each new depressive episode. The kindling model typically is presented as a version of the acquired susceptibility model (Post, 1992).
The kindling model for depression draws upon research on the onset and progression of epileptic seizures (see Post, 1992). The general notion of kindling is that responses become triggered more easily after repeated presentation of a stimulus (Post, Rubinow, & Ballenger, 1986). As extended to mood disorders, the model was intended to explain a series of common observations regarding the lifetime course of these conditions. The first and most widely-recognized observation was that, although the initial lifetime episode often was preceded by a stressful life event, the association between major stress and episode onset lessened with successive recurrences (e.g., Ezquiaga, Guitierrez, & Lopez, 1987; Ghaziuddin, Ghaziuddin, & Stein, 1990). It was inferred that the decreasing association between major life events and depression onset was indicative of less significant forms of stress acquiring the capability of triggering depression onset in the absence of major life stress (i.e., stress sensitization).
In additional investigations, another aspect of kindling was proposed: the amount of well time between successive recurrences (from here on, “intermorbid interval”) was reported to become progressively shorter over successive episodes (Angst & Presig, 1995; Angst et al., 1973; Kessing & Andersen, 1999; Kessing, Hansen, Andersen, & Angst, 2004). This “cycle acceleration” feature of kindling is thought to be manifested as another attribute of stress sensitization, wherein progressively less severe and more common life events become capable of triggering recurrences, and thus progressively shorter intermorbid intervals result (Monroe & Anderson, 2015; Oepen, Baldessarini, & Salvatore, 2004; Ormel, Oldehinkel, & Brilman, 2001; Post, 1992). Cycle acceleration was originally noted by Kraepelin (1921), who observed an apparent tendency for later episodes to be separated by shorter intervals than early episodes. This decreasing intermorbid interval length is believed to be “modal across a majority of studies” (Post, 1992, p. 999). A series of studies reported findings consistent with cycle acceleration for bipolar and unipolar samples (e.g., Angst & Presig, 1995; Angst et al., 1973; Ehnvall & Agren, 2002; Kessing & Andersen, 1999; Kessing, Hansen, Andersen, & Angst, 2004).
However, research on cycle acceleration is subject to a potentially serious problem. First noted by Elliot Slater (1938) in research with bipolar patients, Slater’s fallacy is a statistical artifact that also raises intriguing theoretical possibilities (Haghighat, 1996; Oepen et al., 2004). When data from all depressed individuals are pooled together in the analyses, intermorbid intervals may appear to be shortening as the number of recurrences increases. But this effect may be solely attributable to a subgroup of individuals who have many recurrences with consistently shorter intermorbid intervals. These highly recurrent individuals become a larger proportion of the remaining sample with each recurrence, giving rise to the illusion of progressively shorter intermorbid intervals (Oepen et al., 2004; Slater, 1938). In statistical terms, previous studies did not separate between-person from within-person effects, or their efforts to do so may have been well-intended but insufficient (Hoffman & Stawski, 2009).
Most importantly in theoretical terms, this means that prior research has inadvertently overlooked the possibility that two subtypes exist within the general population of people who suffer recurrences. Some of these individuals may be highly recurrence-prone and have numerous depressive episodes over the life course, whereas others may be less recurrence-prone and have a few sporadic, if any, additional episodes. Individuals who are highly recurrence-prone may be characterized by consistently shorter intermorbid intervals throughout their lifetime course, whereas those who are not highly recurrence-prone may have longer, or more variable, intervals. Instead of pooling all depressed persons together, who potentially possess varying degrees of liability to recurrences, studies should directly investigate a model wherein highly recurrent persons are hypothesized to exhibit consistently shorter intermorbid intervals over successive recurrences. Perhaps most illuminating would be to demonstrate that – even for the very first recurrence – highly recurrent individuals exhibit a shorter intermorbid interval compared to the less recurrent individuals. Detection of valid differences in recurrence-proneness could transform research on depression and its recurrences, by delimiting heterogeneity and focusing attention on early indicators of biological, cognitive, and social risk for recurrences (Monroe & Harkness, 2011; Monroe & Anderson, in press).
To address Slater’s fallacy, three recommendations have been made. First, Slater (1938) suggested matching individuals by specific episode count. For example, the researcher could examine successive intermorbid intervals for individuals with, say, four (or five, or six, etc.) lifetime episodes of depression. This more homogeneous grouping of persons would be less likely to yield results biased by individuals with characteristically longer intermorbid intervals, but would be less powerful due to restricting the sample.
Second, survival analyses take into account individual liability (frailty) toward recurrence (Kessing et al., 2004). Results analyzed in this way have had mixed outcomes. For example, Kessing, Olsen, and Andersen (1999) found evidence for a cycle acceleration in unipolar depression for women, but not for men. In contrast, a study combining unipolar and bipolar patients evidenced cycle acceleration for both genders (Kessing et al., 2004). Finally, yet another study did not detect cycle acceleration for patients with unipolar depression (Solomon et al., 2000). Survival analytic techniques may help to correct bias from individuals with a high liability to recurrence, but it is important to be aware that they are not designed to permit direct and more powerful analysis of changes in intermorbid interval length over successive episodes.
Third, multilevel modeling procedures are well suited for correcting biases associated with Slater’s fallacy. These approaches first model each individual’s own slope and intercept separately, then combine them in an analysis sensitive to the non-independent data structure inherent in within-person longitudinal designs (e.g., Gelman & Hill, 2007). Importantly, these procedures allow for discussing within-person change in intermorbid interval length in directly interpretable units of time. Further, between-person and within-person effects can be directly compared in a single model. When correcting for Slater’s fallacy, research on bipolar disorder has rejected the hypothesis of a progressive shortening of intermorbid intervals (Baldessarini et al., 2012; Oepen et al., 2004). However, it is not yet known whether Slater’s fallacy may be operating with respect to unipolar depression.
Several specific predictions follow from evaluating kindling’s predictions in light of Slater’s fallacy. First, a fundamental prerequisite is to initially demonstrate the purported shortening of the intermorbid interval with successive recurrences for the entire pooled sample. We hypothesized that there would be a significant effect consistent with cycle acceleration when pooling data from all participants. Second, assuming successful replication of this prerequisite finding, we predicted that correcting for Slater’s fallacy would reveal that the apparent cycle acceleration effect would no longer be significant. Third, to demonstrate the predicted between-person differences in intermorbid interval length overall (i.e., those with more episodes have shorter average intervals), we hypothesized a significant difference in the average intermorbid interval between those with fewer versus many recurrences. Fourth, the most novel and persuasive evidence for a subtype distinction would be to demonstrate that highly recurrent cases (≥ 4 lifetime episodes) differ from less recurrent cases (2–3 lifetime episodes) at the time of their very first recurrence with regard to their initial intermorbid interval.1
Finally, if when correcting for Slater’s fallacy cycle acceleration becomes nonsignificant, it still could be argued by proponents that the kindling pattern characterizes the lifetime course for some individuals. To be conservative and probe this modified version of kindling theory, we investigated inter-individual variability in trajectories for length of intermorbid intervals over time (which would allow for detection of such possible effects).
Method
A community-based longitudinal project that assessed and followed individuals from mid-adolescence to age 30, the Oregon Adolescent Depression Project (OADP; see Lewinsohn et al., 2003), provided the foundation for addressing our predictions. Participants were predominantly white (89%), with African American (1%), Hispanic (3%), American Indian (3%), Asian (3%), and “other” (2%) making up the rest of the sample. The sample was 52.1% female at the initial assessment. The modal household income was between $20,000 and $30,000, consistent with the national average at that time (U.S. Census Bureau, 2013). Written informed consent from participants and family members (and guardians for those under 18) was obtained prior to each round of data collection.
Participants and Procedure
Three cohorts of participants were randomly selected from urban and rural high schools in western Oregon. Data were collected on four occasions. (A full description of OADP methodology can be found elsewhere; Lewinsohn et al., 2003; Rohde et al., 2007). About 61 percent of those initially selected (N = 1709 adolescents) completed the initial interviews and questionnaires (T1) between 1987 and 1989. Ages at T1 ranged from 14–19 (M = 16.6, SD = 1.2). A second round of questionnaires and interviews (T2) was conducted a year later. About 88% of T1 participants were re-evaluated at T2 (N = 1507). A third round of data collection (T3) was completed around participants’ 24th birthday, between 1994 and 1999. Participants recruited for wave T3 included all individuals with a history of psychopathology (N = 644) and a random sample of those with no such history (N = 457). A total of 941 participants (85% of those recruited) were assessed at T3, including 555 individuals with prior history (315 with a depression history) and 386 without. Finally, a fourth assessment was conducted around participants’ 30th birthday. A total of 816 participants (87% of the T3 group) were evaluated at T4. A total of 480 participants (59%) assessed at T4 were women. About 33 percent of this sample had a history of depression (N = 271), 24 percent had other psychopathology histories (N = 199), and 43 percent reported no psychopathology up to T3 (N = 346).
For the first three hypotheses addressing Slater’s fallacy, we necessarily used data for individuals who had at least 2 episodes of major depression (N = 304). This subset of participants was also used for the test of the random slope variance. For the analysis comparing participants with few versus many lifetime episodes, however, we needed to take added precautions that our division of the sample into recurrence groups (high versus low) is reasonably stable (i.e., additional recurrences wouldn’t alter the outcome). Consequently, we used data from 281 unipolar depressives who all have at least 5 years of follow-up time subsequent to their initial depressive episode from which to observe recurrences.2
Measures
Participant diagnostic interviews
At T1, T2, and T3, participants were interviewed with the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Orvaschel, Puig-Antich, Chambers, Tabrizi, & Johnson, 1982), based on DSM-III-R criteria. The Longitudinal Interview Follow-Up Examination (LIFE; Keller et al., 1987) was used to assess the presence and course of disorders between interviews. At T4, participants were interviewed with the Structured Clinical Interview for Axis I DSM-IV Disorders-Non-Patient Edition (SCID-NP; First, Spitzer, Gibbon, & Williams, 1995). All interviewers had advanced degrees in a mental health field and completed a 70-hour diagnostic interviewing course in the LIFE and SCID-NP. Prior to interviewing participants, interviewers were required to attain a minimum kappa of 0.80 across all symptoms for at least two consecutive training interviews as well as a videotaped interview with evidence of psychopathology.
MDD recurrence
Recurrent MDD episodes between T1 and T4 were each represented with a dichotomous variable. Recurrence was specified as a new episode of MDD after full recovery of at least 8 consecutive weeks with no more than 1–2 mild depressive symptoms.
Intermorbid interval length
Length of time between episodes was measured through the diagnostic interview measures. This was operationalized as the period of time between meeting full recovery criteria and meeting full episode criteria. Episode onset and offset were recorded in months. Intermorbid interval length was converted to years to better reflect the sample distribution of this variable (M = 5.36 years).
Data Analysis
A priori power analysis
For our linear mixed effect models, 261 participants were needed to display a percent change in slope of 30%, a conservative estimate of what kindling would be expected to evidence (R package longpower). Regarding the t-test comparing individuals’ first intermorbid interval length, because we had a set number of individuals in our samples, as well as unequal sample sizes between the recurrent and less recurrent groups, we calculated that we would have 80% power to detect an effect size of d = .37 with our current group sizes.
Analyses
To isolate purely within-person changes in intermorbid interval lengths, the number of recurrences should be centered with respect to each individual’s own mean number of recurrences (person mean-centering; Hoffman & Stawski, 2009; Wang & Maxwell, 2015), rather than with respect to the overall mean of the sample. But first, to reveal the expected and prerequisite kindling prediction for the intermorbid interval, we fit a linear mixed effect model necessarily restricting the sample to individuals with two or more lifetime episodes. This subsample essentially maintained the overall ethnic distribution, but was 75% female, consistent with the gender difference in depression. We regressed length of intermorbid interval on number of recurrences, which was centered around the grand mean of all individuals. Following recommendations by Barr, Levy, Scheepers, and Tily (2013), we included a by-participant random intercept and slope. In accord with this first hypothesis, we predicted that recurrences would be significantly related to intermorbid interval length, with a negative slope.
As discussed above, however, this analysis confounds between-person and within-person effects. Correcting for Slater’s bias, we performed a second analysis to isolate the purely within-person effect. We fit a linear mixed effect model, regressing length of intermorbid interval on number of recurrences, this time centered around each individual’s own mean. Centering around individual means effectively removes the between-subject effect variation, which is the statistical basis for Slater’s fallacy. For this second hypothesis, we predicted that with this correction, recurrences would have a nonsignificant relation with intermorbid interval length (i.e., cycle acceleration would no longer be apparent).
To evaluate differences in intermorbid intervals on average, we also included a person-mean variable as a predictor, so that we could isolate the purely within-person and between-person effects in one analysis (per recommendations by Wang & Maxwell, 2015). In keeping with this hypothesis, the regression coefficient associated with this variable indicates differences in average intermorbid interval length between persons with more versus fewer recurrences. Package lme4 in R was used for all of these statistical analyses.
For our final prediction evaluating between-person differences in the very first intermorbid interval, an independent samples two-tailed t-test compared the length of the first intermorbid interval for those with high (≥ 4 episodes) versus low (2–3 episodes) number of recurrences. Age of first-onset was added as a covariate to control for its relation with recurrence (e.g. Lewinsohn, Clarke, Seeley, & Rohde, 1994; for a review, see Burcusa & Iacono, 2007).3
Finally, to examine conservatively whether some individuals might show a trajectory in keeping with cycle acceleration, we assessed the random effects variance of the slope, which addresses differences in how the lengths of individuals’ intermorbid interval change as they have more recurrences.4 When allowing variance parameters to be freely estimated, however, the model did not converge, so variance parameters were constrained to be nonnegative. Constrained estimation is recommended due to better control of the Type I error rate, larger empirical power, and ease of interpretability (Ke & Wang, 2014). The covariance between the intercept and slope was freely estimated.
As this latter issue has rarely been assessed previously, we did not have a specific hypothesis. A random slope significantly greater than zero would indicate that individuals differ in their intermorbid interval trajectories (i.e., some individuals could show a pattern of shortening intermorbid intervals, consistent with cycle acceleration and kindling, while others could show different patterns of intermorbid interval length change as they have additional recurrences). In contrast, a nonsignificant random slope would indicate that there is negligible variation in trajectories (beyond what would be expected from random noise in the sample estimates). We tested these different outcomes with a generalized likelihood ratio test, comparing a model containing a random intercept, slope, and their covariance to a model constraining the slope and associated covariance to be zero. Generalized likelihood ratio tests are preferable over specific Wald tests due to their power advantage and robustness in terms of Type I error rates (Hertzog, von Oertzen, Ghisletta, & Lindenberger, 2008; Ke & Wang, 2014). The χ2 value of this model comparison was compared to a .05 critical value from a 50–50 mixture distribution, recommended in cases of constrained estimation (Ke & Wang, 2014).
Results
Descriptive statistics and a breakdown of the recurrence distribution are presented in Table 1.
Table 1.
Descriptive Statistics and Recurrence Distribution
| Variable | M | SD | Min | Max | Skew | Kurtosis | |||
|---|---|---|---|---|---|---|---|---|---|
| Age of First Onset | 17.18 | 4.10 | 5 | 26 | −0.18 | −0.04 | |||
| Number of Episodes | 2.23 | 1.44 | 1 | 10 | 1.61 | 3.41 | |||
| Intermorbid Interval Length | 5.36 | 3.44 | 0.25 | 18.58 | 1.33 | 1.99 | |||
| Recurrence Distribution in Sample of Individuals with at Least One MDD Recurrence | |||||||||
| Number of episodes | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Number of participants | 153 | 69 | 51 | 16 | 7 | 3 | 4 | 0 | 1 |
| Percentage of sample | 50 | 23 | 17 | 5 | 2 | 1 | 1 | 0 | <1 |
Note. The top portion of the table contains descriptives for the entire sample of depressed individuals (N=629). The bottom portion is restricted to those with at least one recurrence (N=304).
Primary Analyses
When analyzing cycle acceleration with the traditional approach, results indicated the prerequisite progressive shortening of intermorbid intervals consistent with existing research on cycle acceleration. Specifically, for every additional recurrence, the length tended to decrease by 0.90 years, 95% confidence interval (CI) [−1.14, −0.67], t(82.947) = −7.48, p < .0001.
However, the interpretation of this first finding is altered strikingly due to our second hypothesis also being supported. When correcting for Slater’s fallacy by centering with respect to each individual’s own mean number of recurrences, the results no longer evidence a significant cycle acceleration effect, b = −0.15 years, 95% CI [−0.43, 0.13], t(25.898) = −1.16, p = .309.
Further, when isolating the purely between-person effect from the purely within-person effect, we found a significant between-person effect, such that individuals with more recurrences on average had shorter intermorbid intervals than those with fewer episodes, b = −1.39 years, 95% CI [−1.69, −1.10], t(58.973) = −9.344, p < .0001.
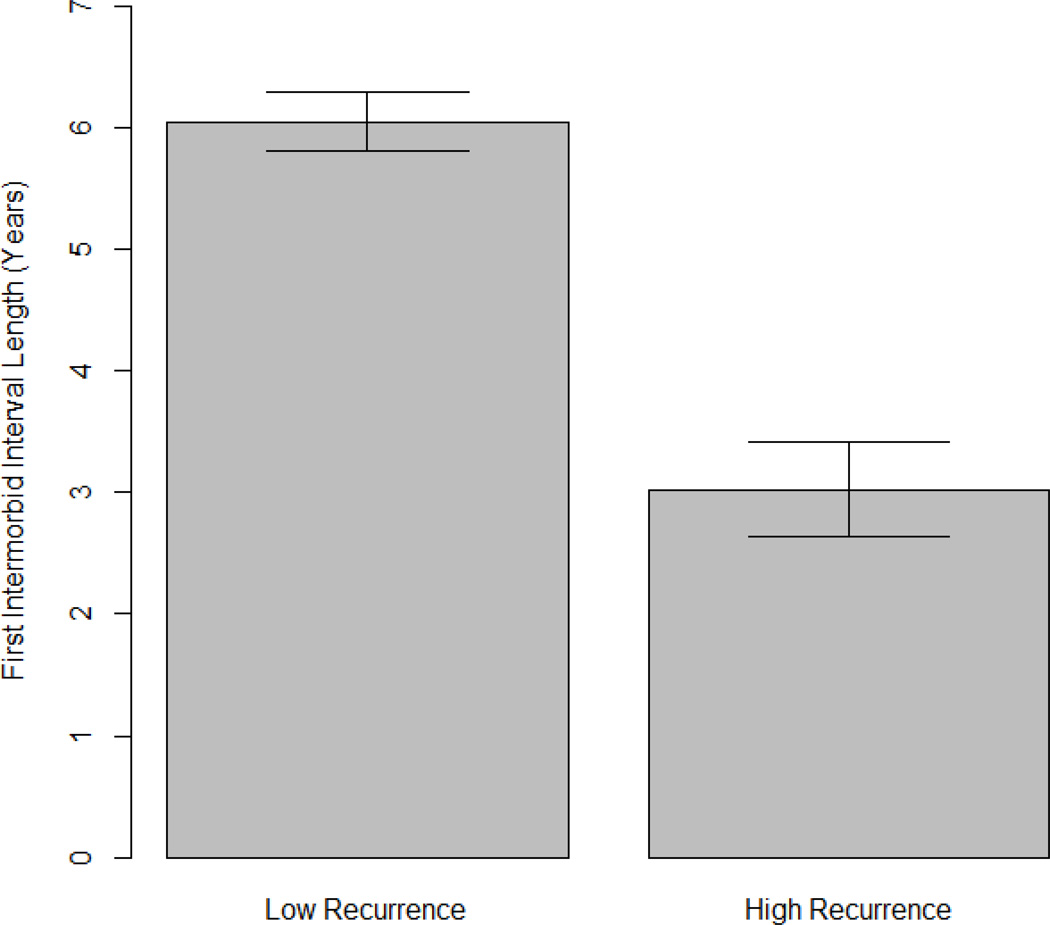
Finally, our alternative model also was strongly supported. Highly recurrent individuals (≥ 4 episodes; n = 81) had a significantly shorter first intermorbid interval by 3 years (M = 3.24 years, SD = 2.85) than less recurrent individuals (2–3 episodes; n = 200, M = 6.26 years, SD = 3.96), b = −3.02, 95% CI [−3.93, −2.12], t(278) = −6.55, p < .001, Cohen’s d = 0.87 (controlling for age of first-onset). This result is graphed in Figure 1.
Figure 1.
Mean length of the first intermorbid interval, grouped by recurrence subgroup. Low recurrence (less highly recurrent): 2–3 episodes. High recurrence (highly recurrent): ≥ 4 episodes. Error bars represent ± 1 SE.
A further analysis tested the variance of the random slope, allowing for individuals to vary in their linear rates of change in intermorbid interval length over time.5 The random slope variance was essentially 0.00, χ2(2) < 1, p = .99.6 The zero variance reflects that there is no systematic variation in individual slopes expressing change in intermorbid interval length, after removing variance that would be expected from random sample noise. Overall, this means that the random slope variance is not statistically significant. Thus, it is plausible that the nonsignificant relation between recurrences and intermorbid interval length is the same for all individuals, which provides assurances that kindling is not likely to be operative, even for some individuals in our sample.
Discussion
The present study demonstrated that the presumed cycle acceleration observation over repeated recurrences of major depression is due to a statistical artifact. As hypothesized, intermorbid intervals seemed to decrease over time when pooling data across all individuals, but this effect became nonsignificant after correcting for Slater’s fallacy. Further, individuals were found to differ in their overall tendency to have longer or shorter intermorbid intervals, with highly-recurrent individuals having on average shorter intermorbid intervals, and even having a shorter interval at the time of the very first recurrence. Most intriguingly, these results call into question an important tenet of the kindling premise, and by extension raise alternative ways of conceptualizing the nature of recurrence in unipolar depression.
We first replicated the predicted evidence for cycle acceleration using traditional methods of analyzing recurrence data. These initial findings yielded the appearance of cycle acceleration: the length of the intermorbid interval decreased over successive recurrences (i.e., the estimated change for the intermorbid interval was both negative and statistically significant). This prerequisite finding set the stage for addressing our second prediction.
As we have pointed out, the traditional approach confounds both between-individual and within-individual variation. Slater’s fallacy suggests that the average differences in intermorbid interval length between individuals with many and few recurrences biases this estimate, resulting in an illusion of decreasing intermorbid intervals. We found that the effect of the apparent decreasing intermorbid intervals indeed was entirely attributable to the between-person effect in our analysis, not to the decreasing intermorbid intervals within persons over successive recurrences. There was no evidence of change within-individuals, providing no indication for cycle acceleration, or for any significant change in intermorbid interval length in either direction across time. These results reinforce the fact that the research question demands the inclusion of analyses that directly assess changes in intermorbid interval length over time purely within-individuals.
With regard to theorizing about the nature of recurrence, we must explain why the findings are no longer significant when controlling for Slater’s fallacy. We reasoned that if cycle acceleration is an artifact, the most plausible explanation would be based upon differences between individuals. To this end, we evaluated the average duration of intermorbid intervals as a function of prior history of depression. The results were in keeping with this prediction, substantiating that individuals who were more recurrent had, on average, consistently briefer periods of well time between episodes than less recurrent individuals. These between-individual results are consonant with the premise that there are distinct subtypes of individuals who populate the recurrence pool: those who are highly recurrent (with shorter intermorbid intervals) and those who are less recurrent (with longer intermorbid intervals). We then went one step further to propose that these subgroups could be identifiable even at the time of their first recurrence. As our findings confirm, we found strong evidence for this prediction: the first intermorbid interval difference between the highly recurrent and less-highly recurrent groups was, on average, three years.
That the individuals who eventually became highly recurrent cases differed at this critical initial clinical juncture of a first lifetime episode suggests that they also differ along other lines that could distinguish them as a distinct subtype of depressed persons who are highly likely to have many recurrences over the life course (i.e., recurrence-prone; Burcusa & Iacono, 2007; Monroe & Anderson, 2015). The theoretical and clinical significance of detecting proneness or liability to recurrence early in the lifetime course would be of tremendous value, allowing for more detailed studies of the genetic, neural systems, neuroendocrine, psychological, and social factors that could also distinguish the highly recurrence-prone (Monroe & Harkness, 2011).
To ensure we were not overlooking the possibility that cycle acceleration characterized a portion of the sample, we evaluated whether the nonsignificant change in intermorbid length over time was general to everyone, or whether some individuals exhibited changes with increasing recurrences (e.g., increasing, decreasing, or flat trajectories). Based on our analysis of the random slope variance, it became clear that individuals did not vary from one another in systematic ways with respect to changes in intermorbid interval length with increasing recurrences (beyond what would be expected from random variability). This means that our focal finding of a nonsignificant cycle acceleration effect is not moderated by other factors, such as genetic predisposition, family history, or gender (i.e., between-person predictors), because there is no significant amount of between-individual variation in trajectories for the moderator to account for (Singer & Willet, 2003, p. 100). We conclude that the current study does not provide evidence for classes or types of intermorbid interval trajectories (e.g., an increasing trajectory, a cycle acceleration trajectory, a flat trajectory). Although it is worth reiterating the study does provide evidence for subgroups that vary in their tendency to have short or long intermorbid intervals overall.
This study was not without limitations. Although ideally we would have full lifetime data on participants, practical considerations inevitably render the timing and duration of any study rather arbitrary within the broader life context (Monroe & Harkness, 2011). Owing to these constraints, the critic could contend that the finding of shorter intermorbid intervals on average for the highly recurrent cases also may be an artifact, for to have many recurrences over the study period, these cases would have to display shorter intermorbid intervals. The primary rejoinder to this observation is the direct comparison of the very first intermorbid interval for those individuals who subsequently became highly versus not highly recurrent. This is essentially an ex post facto, yet prospective, research design. If persons who are destined to suffer repeated recurrences over later stretches of time differ at the very beginning of the life course clinical trajectory in terms of a shorter intermorbid interval, then it strongly argues against the concern about the shorter average intermorbid interval being a misleading consequence of the restricted time frame available over which recurrences can be experienced.
Additionally, although using community participants has many advantages, our sample was generally not composed of inpatients who may evidence depression in its more severe forms. Individuals in our study were predominantly young, white, middle-class Americans. Thus, the results cannot easily generalize to recurrence trajectories for other races and cultural groups. However, our community sample represented a range in number of lifetime depressive episodes (e.g., up to 10). Finally, although the kindling model rests heavily on cycle acceleration, this investigation was not designed to assess other features of kindling, including the stress sensitization or the development of refractoriness to treatment (Post, 2007).
The present study does, however, raise a key question about a core tenet of stress sensitization: that less severe forms of life stress acquire the capability of triggering a depressive episode. This central premise represents the proposed mechanism for explaining the observation that major life stress becomes less common prior to depression onset with each successive episode. As the depressed person becomes increasingly susceptible to stress, it is assumed that progressively lower levels of stress become more and more capable of triggering future episodes. Thus relieved of the primary etiologic responsibility for triggering depression initially, the lower-frequency major life events are increasingly replaced by higher-frequency – but lower severity – life events as the causal mechanism expediting recurrences (Monroe & Harkness, 2005; Ormel et al., 2001; Post, 1992).
Could it be that the changing role of major life stress with successive recurrences also is an illusion, based on the same fallacy, an artifact attributable to not distinguishing within- versus between-person effects? In other words, the association between major life stress and successive recurrences also may only appear to diminish? Much like we have explained the apparent episode acceleration by subgroup differences, perhaps the apparent changes in major life stress prior to episode onset also can be explained by similar reasoning. For example, highly recurrent individuals, who become more prevalent in the sample as lifetime episodes rise, simply may become depressed without significant life stress prior to episode onset (i.e., major stress is not of causal relevance for highly recurrence-prone cases; Monroe & Reid, 2009; Monroe & Anderson, 2015). Discovering such group differences in the causal significance of major life stress would have far-reaching implications, and represents a high priority agenda for recurrence research.
To focus on immediate needs for advancing this research agenda, we suggest initially targeting first-onset cases of major depression, with special attention devoted to the distinction between these incident cases with and without major life stress prior to depression onset. This strategy provides the foundation for making competing predictions derived from the stress sensitization and subtype models of recurrence. The general objective is to evaluate life-course trajectories of the two stress groups with regard recurrences, timing of recurrences, and the role of major life stress in recurrences. For instance, based on stress sensitization, first lifetime depressed persons with major life stress would have a high likelihood of recurrence, and early in the lifetime trajectory of recurrences major life events will cease to be prominent prior to onset. In direct contrast, based on the subtype explanation, first lifetime depressed persons with major life stress will have a lower likelihood of recurrences (compared to first lifetime depressed persons without major life stress), and when these cases do have recurrences, they will do so solely subsequent to major life stress. The key practical challenges facing researchers will be to obtain a sufficient sample of first onset cases, carefully assessed for major life stress, and for whom an adequate amount of time will available following the initial episode to depict differing recurrence trajectories (Monroe, 2008; Monroe & Harkness, 2005, 2011).7
Acknowledgments
This research was supported in part by NIMH grants MH40501, MH50522, and NIDA grant DA12951, awarded to Dr. Peter Lewinsohn, and the John Simon Guggenheim Fellowship, awarded to Dr. Scott Monroe. The authors wish to thank Scott Maxwell and Anne Simons for helpful comments on an earlier draft of this manuscript.
Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Institute of Mental Health or National Institute on Drug Abuse.
Footnotes
The specific split between 2–3 episodes and ≥ 4 episodes was chosen to maintain a large enough sample in the highly recurrent group while remaining consistent with the nature of the constructs of highly and less highly recurrent. An analysis comparing those with 2 episodes versus more than 2 episodes had highly similar results, suggesting that the effect is robust.
This allowed ample time to detect a recurrence within the study period, as increasing the follow-up interval to 7 years tends caught only a negligible number [9 cases] of new first recurrences in our data.)
Models comparing highly recurrent and less highly recurrent individuals on their first intermorbid interval length were also conducted without age of onset as a control and additionally without excluding individuals with less than 5 years of follow-up time after their initial episode of depression. Results were highly similar in both cases. The means reported represent the group means adjusted for the age covariate.
The linear mixed effect model used for this analysis is similar to that used in our other analyses, but omits the person-mean variable that specifies the purely between-person effect. The purely between-person “person mean” variable completely accounted for inter-individual differences in individuals’ intermorbid interval length, leading to a random intercept of 0.00 when included in the model. This is completely consistent with, and reinforces, the highly significant between-person differences in average intermorbid interval length. However, in order to accurately estimate the random effects coefficients, it was important to fit a model without the purely between-person component.
The random intercept variance = 3.69. Comparison with a model constraining the random intercept variance to be zero yielded χ2(2) = 19.08, p < .05, indicating a distribution wherein 68% of individuals have an intercept (person-mean centered) ranging between 1.92 years above and below the mean interval length of 4.87 years. We do not discuss this result, as it is consistent with, and highly redundant with, our results for purely between-person differences in average intermorbid interval length, indicating significant differences between individuals in overall tendency to have shorter versus longer intermorbid intervals.
More precisely, the variance of the random slope = 9.64×10−6, indicating a distribution wherein 68% of individuals have a slope ranging between .003 above and below the mean value of −0.15. The covariance between the random intercept and slope = −0.08. Had we been able to freely estimate the variance components, these estimates would likely be negative, which is still indicative of no additional between-individual variation in trajectories beyond random error.
It is interesting to note that the stress sensitization model is restricted in its ability to fully explain all onsets of depression, for there are no firmly specified principles accounting for first onsets of depression without major life events.
Author Contributions
S.F.A. and S.M.M. developed the study concept. Data collection was performed by P.R. and P.L. S.F.A. performed the data analysis. S.F.A. and S.M.M interpreted the analyses. S.F.A. drafted the paper, and S.M.M., P.R., and P.L. provided critical revisions. All authors approved the final version of the paper for submission.
Contributor Information
Samantha F. Anderson, University of Notre Dame
Scott M. Monroe, University of Notre Dame
Paul Rohde, Oregon Research Institute.
Peter M. Lewinsohn, Oregon Research Institute
References
- Angst J, Baastrup P, Grof P, Hippius H, Poeldinger W, Weis P. The course of monopolar depression and bipolar psychoses. Psychiatria Neurologia Neurochirurgia. 1973;76:489–500. [PubMed] [Google Scholar]
- Angst J, Presig M. Course of a clinical cohort of unipolar, bipolar, and schizoaffective patients: Results of a prospective study from 1959 to 1985. Schweizer Archivfur Neurologie und Psychiatrie. 1995;146:5–18. [PubMed] [Google Scholar]
- Baldessarini RJ, Salvatore P, Khalsa HMK, Imaz-Etxeberria H, Gonzalez-Pinto A, Tohen M. Episode cycles with increasing recurrences in first episode bipolar-I disorder patients. Journal of Affective Disorders. 2012;136:149–154. doi: 10.1016/j.jad.2011.08.037. [DOI] [PubMed] [Google Scholar]
- Barr DJ, Levy R, Scheepers C, Tily HJ. Random effects structure for confirmatory hypothesis testing: Keep it maximal. Journal of Memory and Language. 2013;68:255–278. doi: 10.1016/j.jml.2012.11.001. doi: http://dx.doi.org/10.1016/j.jml.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burcusa SL, Iacono WG. Risk for recurrence in depression. Clinical Psychology Review. 2007;27:959–985. doi: 10.1016/j.cpr.2007.02.005. doi: http://dx.doi.org/10.1016/j.cpr.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehnvall A, Agren H. Patterns of sensitisation in the course of affective illness: A life-charting study of treatment-refractory depressed patients. Journal of Affective Disorders. 70:67–75. doi: 10.1016/s0165-0327(01)00328-7. [DOI] [PubMed] [Google Scholar]
- Ezquiaga E, Gutierrez JLA, Lopez AG. Psychosocial factors and episode number in depression. Journal of Affective Disorder. 1987;12:135–138. doi: 10.1016/0165-0327(87)90005-x. [DOI] [PubMed] [Google Scholar]
- Ferguson DM, Boden JM, Horwood LJ. Recurrence of major depression in adolescence and early adulthood, and later mental health, educational and economic outcomes. The British Journal of Psychiatry. 2007;191:335–342. doi: 10.1192/bjp.bp.107.036079. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM–IV Axis I Disorders–Non-Patient Edition (SCID-I/NP, Version 2.0) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- Gelman A, Hill J. Data Analysis Using Regression and Multilevel/Hierarchical Models. New York, NY: Cambridge University Press; 2007. [Google Scholar]
- Ghaziuddin M, Ghaziuddin N, Stein GS. Life events and the recurrence of depression. Canadian Journal of Psychiatry. 1990;35:239–242. doi: 10.1177/070674379003500307. [DOI] [PubMed] [Google Scholar]
- Greden JF. The burden of recurrent depression: Causes, consequences, and future prospects. Journal of Clinical Psychiatry. 2001;62:5–9. [PubMed] [Google Scholar]
- Haghighat R. Lifelong development of risk of recurrence in depressive disorders. Journal of Affective Disorders. 1996;41:141–147. doi: 10.1016/s0165-0327(96)00082-1. [DOI] [PubMed] [Google Scholar]
- Hertzog C, von Oertzen T, Ghisletta P, Lindenberger U. Evaluating the power of latent growth curve models to detect individual differences in change. Structural Equation Modeling. 2008;15:541–563. [Google Scholar]
- Hoffman L, Stawski RS. Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development. 2009;6:97–120. doi: http://dx.doi.org/10.1080/15427600902911189. [Google Scholar]
- Ke Z, Wang L. Detecting individual differences in change: Methods and comparisons. Structural Equation Modeling. 2014 Advance online publication. [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kessing LV, Andersen PK. The effect of episodes on recurrence in affective disorder: A case register study. Journal of Affective Disorders. 1999;53:225–231. doi: 10.1016/s0165-0327(98)00125-6. [DOI] [PubMed] [Google Scholar]
- Kessing LV, Hansen MG, Andersen PK, Angst J. The predictive effect of episodes on the risk of recurrence in depressive and bipolar disorders--A life-long perspective. Acta Psychiatrica Scandinavica. 2004;109:339–344. doi: 10.1046/j.1600-0447.2003.00266.x. doi: http://dx.doi.org/10.1046/j.1600-0447.2003.00266.x. [DOI] [PubMed] [Google Scholar]
- Kraepelin E. Manic-depressive Insanity and Paranoia. Edinburgh: Livingstone; 1921. [Google Scholar]
- Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: Age at onset, episode duration, and time to recurrence. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:809–818. doi: 10.1097/00004583-199407000-00006. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH. Psychosocial functioning of young adults who have experienced and recovered from major depressive disorder during adolescence. Journal of Abnormal Psychology. 2003;112:353–363. doi: 10.1037/0021-843x.112.3.353. [DOI] [PubMed] [Google Scholar]
- Monroe SM. Annual Review of Clinical Psychology. Vol. 4. Palo Alto, CA: Annual Reviews; 2008. Modern approaches to conceptualizing and measuring life stress; pp. 33–52. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Anderson SF. The changing association of major life stress with recurrences of major depression. 2015 Manuscript submitted for publication. [Google Scholar]
- Monroe SM, Anderson SF. Depression: The shroud of heterogeneity. Current Directions in Psychological Science. in press [Google Scholar]
- Monroe SM, Harkness KL. Life stress, the “kindling” hypothesis, and the recurrence of depression: Considerations from a life stress perspective. Psychological Review. 2005;112:417–445. doi: 10.1037/0033-295X.112.2.417. doi: http://dx.doi.org/10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Harkness KL. Recurrence in major depression: A conceptual analysis. Psychological Review. 2011;118:655–674. doi: 10.1037/a0025190. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Reid MW. Life stress and major depression. Current Directions in Psychological Science. 2009;18:68–72. [Google Scholar]
- Oepen G, Baldessarini RJ, Salvatore P. On the periodicity of manic-depressive insanity, by Elliot Slater (1938): Translated excerpts and commentary. Journal of Affective Disorders. 2004;78:1–9. doi: 10.1016/s0165-0327(02)00359-2. [DOI] [PubMed] [Google Scholar]
- Ormel J, Oldehinkel AJ, Brilman EI. The interplay and ecological continuity of neuroticism, difficulties, and life events in the etiology of major and subsyndromal, first and recurrent depressive episodes in later life. American Journal of Psychiatry. 2001;158:885–891. doi: 10.1176/appi.ajp.158.6.885. [DOI] [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J, Chambers W, Tabrizi MA, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-Sads-E. Journal of the American Academy of Child and Adolescent Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. American Journal of Psychiatry. 1992;149:999–1010. doi: 10.1176/ajp.149.8.999. [DOI] [PubMed] [Google Scholar]
- Post RM. Kindling and sensitization as models for affective episode recurrence, cyclicity, and tolerance phenomena. Neuroscience and Biobehavioral Reviews. 2007;31:858–873. doi: 10.1016/j.neubiorev.2007.04.003. doi: http://dx.doi.org/10.1016/j.neubiorev.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Post RM, Rubinow DR, Ballenger JC. Conditioning and sensitization in the longitudinal course of affective illness. British Journal of Psychiatry. 1986;149:191–201. doi: 10.1192/bjp.149.2.191. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR, Klein DN, Andrews JA, Small JW. Psychosocial functioning of adults who experienced substance use disorders as adolescents. Psychology of Addictive Behaviors. 2007;21:155–164. doi: 10.1037/0893-164X.21.2.155. doi: http://dx.doi.org/10.1037/0893-164X.21.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheline YI, Wang PW, Gado MH, Csernansky JG, Vannier MW. Hippocampal atrophy in recurrent major depression. Proceedings of the National Academy of Sciences. 1996;93:3908–391. doi: 10.1073/pnas.93.9.3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, Willet JB. Longitudinal Data Analysis. New York: Oxford University Press; 2003. [Google Scholar]
- Slater E. Zu periodic des manisch-depressiven irreseins. Z. Gesamte Neurologie Psychiatrie. 1938;162:794–801. [Google Scholar]
- Solomon DA, Keller MB, Leon AC, Mueller TI, Lavori PW, Shea M, T…Endicott J. Multiple recurrences of major depressive disorder. American Journal of Psychiatry. 2000;157:229–233. doi: 10.1176/appi.ajp.157.2.229. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Income, poverty, and health insurance coverage in the United States: 2012. 2013 Retrieved from http://www.census.gov/prod/2013pubs/p60-245.pdf.
- Wang P, Maxwell SE. On disaggregating between-person and within-person effects with longitudinal data using multilevel models. Psychological Methods. 2015;20:63–83. doi: 10.1037/met0000030. [DOI] [PubMed] [Google Scholar]