Abstract
Open-wedge high tibial osteotomy for medial unicompartmental arthritis of the knee joint is a successful treatment option but is associated with potential intraoperative complications such as tibial plateau fracture, dislocation of the osteotomy hinge, under- or over-correction of the posterior slope, and neurovascular injury. Therefore we devised a protective cutting system and describe our method for the prevention of these complications. The potential advantages of this system are protection of the posterior neurovascular structures using a curved protector, bone cutting along the natural tibial slope using a superior surface aligning with the natural tibial slope, and complete 1-plane sawing of the posterior wall before the lateral hinge.
Open-wedge high tibial osteotomy (OWHTO) for medial unicompartmental arthritis of the knee joint is a successful treatment option but is associated with potential intraoperative complications. During surgical procedures, the possible major problems that could jeopardize the final clinical outcomes are tibial plateau fracture,1 dislocation of the osteotomy hinge,2, 3, 4, 5, 6 under- or over-correction of the posterior slope,7, 8, 9 and neurovascular injury.1, 10
An irregular cutting surface and breakage of the medial cortex that is especially important in block-type fixation also occur, and this means that the plane of the osteotomy could be changed during the procedure. These phenomena may originate for the following reasons: Sawing is usually performed with a freehand technique, and most of the osteotomy is performed with an osteotome because of the fear of causing neurovascular injuries except when addressing the medial cortex. From this reason, an incomplete osteotomy could be performed at the posterior cortex, and this could be a major factor that increases the posterior slope and the incidence of tibial plateau fractures.
To prevent the aforementioned problems, we thought that some surgical advancements were required and we devised a protective cutting system (PCS; Tradimedics, Seongnam, Republic of Korea). The potential advantages of this system are protection of the posterior neurovascular structures using a curved protector, bone cutting along the natural tibial slope using a superior surface aligning with the natural tibial slope, and complete 1-plane sawing of the posterior wall before the lateral hinge. The overall aim of this report is to contribute to the prevention of intraoperative complications and to offer some solutions.
Surgical Technique
This technical note describes our technique of biplanar OWHTO using the PCS (Video 1). The details are summarized in Table 1, Table 2.
Table 1.
Tips and Pearls
| Appropriate exposure of the posteromedial cortex is mandatory. |
| The MCL should be released from the anterior side. |
| The PCS should be inserted with contact with the posterior cortex. |
| The tip of the PCS should be hooked at the fovea of the fibular head. |
| Sawing should be directed to the tip of the PCS. |
| The anterior portion of the cortex should be preserved for a biplanar osteotomy. |
MCL, medial collateral ligament; PCS, protective cutting system.
Table 2.
Pitfalls and Risks
| Exposure of the posterior compartment is necessary. |
| Hematoma can occur at the posterior compartment. |
| Calf massage and compression are necessary for the prevention of compartment syndrome. |
| Blunt hooking should be performed at the fovea of the proximal tibiofibular joint. |
| Surgeons still have to be careful to ensure that the saw or osteotome does not penetrate the vessels posteriorly. |
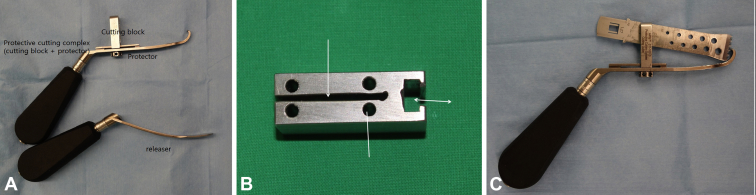
Composition of PCS
The PCS is composed of a releaser and a protective cutting complex (Fig 1). The releaser is used for obtaining easy access to the lateral cortex of the proximal tibia from the posteromedial corner through the posterior wall of the proximal tibia. The most important point regarding the releaser is that the release should be performed with contact with the posterior wall of the proximal tibia because this guarantees the safety of the posterior neurovascular structures by displacing them posteriorly. The body of the releaser is mildly curved to prevent movement to the posterior side and to allow easy contact with the posterior wall of the proximal tibia. In addition, the curved nature of the releaser is helpful in inserting the protective cutting complex and checking the space with an arthroscope at the interval between the posterior wall of the proximal tibia and the anterior side of the releaser. The end portion of the releaser is bluntly designed to prevent direct injury to the posterior neurovascular structures.
Fig 1.
(A) The protective cutting system is composed of a releaser and a protective cutting complex. (B) The protective cutting complex is composed of a separate cutting block and a protector. The cutting block has a slot for the saw (single-headed arrow), holes for fixing the cutting block to the anteromedial cortex (line), and a slot for connecting the cutting block to the protector (double-headed arrow). (C) The saw blade is inserted through the slot of the cutting block, and it is directed to the tip of the protector.
The protective cutting complex is the main instrument in the system. This complex is composed of a separate cutting block and protector (Fig 1). The proximal body of the protector contains the portion for the attachment of the cutting block, and the cutting block is movable for achieving contact with the posteromedial corner of the proximal tibia. The distal body of the protector is curved, similar to the releaser. The tip of the protector is reversely bent, and this enables the device to stopping sawing; this function is important for preservation of the lateral hinge. Therefore the saw can access the area just above the proximal tibiofibular joint. The cutting block has a central cutting slot and holes for guide pin insertion. By use of the superior surface of the cutting block, bone cutting along the natural tibial slope is possible with the help of a lateral C-arm image. The open anterior slot enables the surgeon to perform a uniplanar or biplanar osteotomy by controlling the amount of sawing at the anterior portion of the medial cortex.
Surgical Procedure Focused on PCS
Step 1: Approach
An incision measuring about 5 cm is longitudinally made at the anteromedial portion of the proximal tibia. The interval behind the patellar tendon is now freed, and the insertion area of the tendon is protected using a retractor. The superior border of the pes anserinus is incised, the medial collateral ligament is mobilized from the tibia, and the release is performed by inserting a common periosteal elevator.
Step 2: Release of Posteromedial Aspect
For the release of the posteromedial cortex, the releaser is inserted through the aforementioned interval and a further release is performed by pushing the releaser with contact at the posterior cortex. During this procedure, this interval can be checked using a dry arthroscope to ensure the safety of the posterior neurovascular structures.
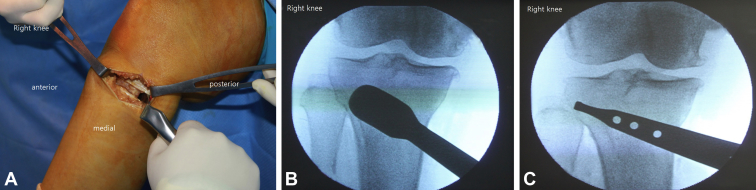
Step 3: Setting of PCS
If the tip portion of the releaser accesses the fibular head area, the protector is inserted at the interval between the posterior cortex and the releaser, and the releaser is removed. With the help of an anteroposterior C-arm image, the tip portion of the protector is hooked to the target portion of the hinge that is located in the area just above the proximal tibiofibular joint (Fig 2) and the cutting block is attached to the protector and pushed to the posteromedial cortex of the tibia.
Fig 2.
(A) The releaser is inserted through the released interval, and further release is performed by pushing the releaser with contact at the posterior cortex. (B) If the tip portion of the releaser accesses the fibular head area, the protector is inserted at the interval between the posterior cortex and the releaser, and the releaser is removed. (C) The tip portion of the protector is hooked to the target portion of the hinge that is located at the lateral cortex of the proximal tibia.
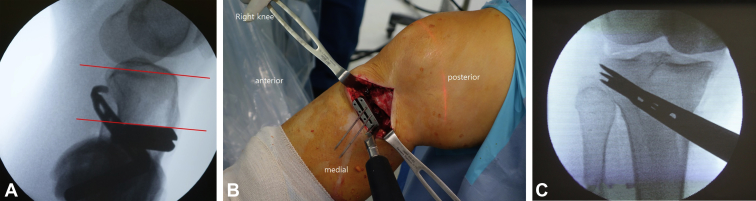
If the contact is completed, the cutting block is tightened to the protector. For the proper configuration of the proximal wedge, the angle of the cutting surface is checked using a lateral C-arm image and the superior surface of the cutting block is adjusted to the natural slope by controlling the protector's handle. If the cutting slope is acceptable, guide pins are inserted in the holes of the cutting block (Fig 3). These guide pins prevent advancement of the saw in an unexpected direction, although the saw progresses along the central line of the protector in the original design. In addition, this procedure causes the cutting block to be securely fixed to the medial cortex.
Fig 3.
(A) The superior surface of the cutting block is placed parallel to the natural slope (red lines) by controlling the protector's handle. (B) If the cutting slope is acceptable, guide pins are inserted in the holes of the cutting block. (C) Final C-arm image for sawing.
Step 4: Osteotomy
Sawing is finally performed, and the main goal of our system is safe and complete sawing of the posterior cortex. The amount of sawing at the anterior cortex is adjusted based on the type of osteotomy (uniplanar or biplanar). The sawing is stopped if we feel contact with the metal that is at the tip portion of the protector. After removal of the protective cutting complex, the C-arm images are checked with insertion of a thin osteotome, and final additional osteotomy or distraction is performed. The amount of distraction or control of the tibial slope is adjusted according to the preoperative planning.
Discussion
High tibial osteotomy is an attractive option for medial unicompartmental osteoarthritis because the knee joint is preserved and the technique results in excellent pain relief and functional improvement.11, 12 OWHTO offers numerous advantages over lateral closing-wedge procedures and is gaining popularity.11, 13, 14 Despite these advantages, OWHTO is associated with potential intraoperative complications: tibial plateau fracture,1 unwanted increase in the posterior tibial slope, under- or over-correction,7, 8, 9 and dislocation of the osteotomy hinge,3 leading to unpredictable correction.15 In addition, an irregular and incomplete osteotomy and cortical breakage could cause early mechanical failure.2, 3, 15, 16
The rate of tibial plateau fracture has been reported to be up to 11%.1 This complication can originate from an incomplete osteotomy and can be avoided by choosing the hinge of the osteotomy at the lateral cortex of the proximal tibia and by carrying out the osteotomy almost completely and not in a subtotal manner, as is often recommended.1, 8, 12 With our devised system, a complete osteotomy is not difficult because posterior neurovascular injuries can be avoided by the protector.
The tibial slope is usually increased after OWHTO, and this is also related to an incomplete osteotomy of the posterolateral cortex.7, 8, 9 If an incomplete osteotomy is performed on the posterolateral side, the opening gap is dominantly increased on the anterior side and this causes an unwanted increase in the posterior slope. Our system enables the surgeon to perform a complete osteotomy and can control the tibial slope.
Some authors recommend a partial osteotomy to prevent fracture and dislocation of the lateral hinge.8, 9 However, a partial osteotomy also causes tibial plateau fracture. Han et al.2 reported that this complication was related to the position of the osteotomy and suggested a safe zone. On the basis of these reports, lateral hinge dislocation is related to the extent and level of the osteotomy. We can control the level of the osteotomy using the described system and guide pins.
Most surgeons try to perform an osteotomy with alignment of the natural tibial slope, although there are some controversies. However, there are few methods for assessing the tibial slope during OWHTO. Using the PCS, the superior surface of the cutting block can be used as a guide aligning the natural tibial slope. By use of lateral images, the surface can be adjusted by rotating the protector's handle, and it can be maintained by fixing the cutting block to the anteromedial cortex.
During sawing, the saw should be directed to the tip portion of the protector for sawing of the posterior cortex. During this procedure, the posterior neurovascular structures can be protected by the protector. However, the saw can also be blocked by the protector. Therefore, sawing could be performed with a little posterior direction for the proper sawing of the posterior cortex. Sawing directed too anteriorly could create a complete osteotomy of the lateral hinge, and this could cause instability of the proximal fragment.
The described PCS provides a technical advancement for the accuracy of an osteotomy and avoidance of intraoperative complications, and we hope our system will be helpful to other surgeons. However, this is only a technical advancement and only short-term follow-up has been performed. Long-term follow-up series are needed.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Surgical technique of biplanar open-wedge high tibial osteotomy using protective cutting system (PCS).
References
- 1.Spahn G. Complications in high tibial (medial opening wedge) osteotomy. Arch Orthop Trauma Surg. 2004;124:649–653. doi: 10.1007/s00402-003-0588-7. [DOI] [PubMed] [Google Scholar]
- 2.Han S.B., Lee D.H., Shetty G.M., Chae D.J., Song J.G., Nha K.W. A “safe zone” in medial open-wedge high tibia osteotomy to prevent lateral cortex fracture. Knee Surg Sports Traumatol Arthrosc. 2013;21:90–95. doi: 10.1007/s00167-011-1706-7. [DOI] [PubMed] [Google Scholar]
- 3.Miller B.S., Downie B., McDonough E.B., Wojtys E.M. Complications after medial opening wedge high tibial osteotomy. Arthroscopy. 2009;25:639–646. doi: 10.1016/j.arthro.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 4.Giuseffi S.A., Replogle W.H., Shelton W.R. Opening-wedge high tibial osteotomy: Review of 100 consecutive cases. Arthroscopy. 2015;31:2128–2137. doi: 10.1016/j.arthro.2015.04.097. [DOI] [PubMed] [Google Scholar]
- 5.Schroter S., Freude T., Kopp M.M. Smoking and unstable hinge fractures cause delayed gap filling irrespective of early weight bearing after open wedge osteotomy. Arthroscopy. 2015;31:254–265. doi: 10.1016/j.arthro.2014.08.028. [DOI] [PubMed] [Google Scholar]
- 6.Takeuchi R., Ishikawa H., Kumagai K. Fractures around the lateral cortical hinge after a medial opening-wedge high tibial osteotomy: A new classification of lateral hinge fracture. Arthroscopy. 2012;28:85–94. doi: 10.1016/j.arthro.2011.06.034. [DOI] [PubMed] [Google Scholar]
- 7.Marti C.B., Gautier E., Wachtl S.W., Jakob R.P. Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy. 2004;20:366–372. doi: 10.1016/j.arthro.2004.01.024. [DOI] [PubMed] [Google Scholar]
- 8.Noyes F.R., Goebel S.X., West J. Opening wedge tibial osteotomy: The 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med. 2005;33:378–387. doi: 10.1177/0363546504269034. [DOI] [PubMed] [Google Scholar]
- 9.Song E.K., Seon J.K., Park S.J. How to avoid unintended increase of posterior slope in navigation-assisted open-wedge high tibial osteotomy. Orthopedics. 2007;30:S127–S131. [PubMed] [Google Scholar]
- 10.Song E.K., Seon J.K., Park S.J., Jeong M.S. The complications of high tibial osteotomy: Closing- versus opening-wedge methods. J Bone Joint Surg Br. 2010;92:1245–1252. doi: 10.1302/0301-620X.92B9.23660. [DOI] [PubMed] [Google Scholar]
- 11.El-Azab H., Halawa A., Anetzberger H., Imhoff A.B., Hinterwimmer S. The effect of closed- and open-wedge high tibial osteotomy on tibial slope: A retrospective radiological review of 120 cases. J Bone Joint Surg Br. 2008;90:1193–1197. doi: 10.1302/0301-620X.90B9.20688. [DOI] [PubMed] [Google Scholar]
- 12.Staubli A.E., De Simoni C., Babst R., Lobenhoffer P. TomoFix: A new LCP-concept for open wedge osteotomy of the medial proximal tibia—Early results in 92 cases. Injury. 2003;34(suppl 2):B55–B62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 13.Asada S., Akagi M., Mori S., Matsushita T., Hashimoto K., Hamanishi C. Increase in posterior tibial slope would result in correction loss in frontal plane after medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2012;20:571–578. doi: 10.1007/s00167-011-1610-1. [DOI] [PubMed] [Google Scholar]
- 14.Brouwer R.W., Bierma-Zeinstra S.M., van Koeveringe A.J., Verhaar J.A. Patellar height and the inclination of the tibial plateau after high tibial osteotomy. The open versus the closed-wedge technique. J Bone Joint Surg Br. 2005;87:1227–1232. doi: 10.1302/0301-620X.87B9.15972. [DOI] [PubMed] [Google Scholar]
- 15.Jacobi M., Wahl P., Jakob R.P. Avoiding intraoperative complications in open-wedge high tibial valgus osteotomy: Technical advancement. Knee Surg Sports Traumatol Arthrosc. 2010;18:200–203. doi: 10.1007/s00167-009-0928-4. [DOI] [PubMed] [Google Scholar]
- 16.Agneskirchner J.D., Freiling D., Hurschler C., Lobenhoffer P. Primary stability of four different implants for opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2006;14:291–300. doi: 10.1007/s00167-005-0690-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique of biplanar open-wedge high tibial osteotomy using protective cutting system (PCS).