Abstract
Labral repair has been shown to be an effective treatment option with excellent early outcomes; however, in cases of severe labral damage or when the labral tissue is too large or diminutive, labral repair may be less effective. The purpose of this article is to present a modified technique for hip labral reconstruction using iliotibial band allograft tissue and a front-to-back fixation technique. The described technique is modified from the original report of a technique for arthroscopic labral reconstruction. The front-to-back technique allows the surgeon to make a graft that is longer than necessary and cut excess graft after front-to-back fixation, resulting in the correct graft size and a reproducible procedure. Allograft tissue offers several advantages, including the ability to control graft thickness and length, as well as the ability to eliminate donor-site morbidity. This procedure adds to the available techniques for treatment of labral pathology by providing a labral reconstruction technique using allograft tissue.
The labrum is a key structure in the hip. Previous research has suggested that it is crucial to maintaining fluid pressurization and the hip seal, stabilizing the joint to distraction forces, and controlling contact pressure.1, 2 Unfortunately, labral pathology is a common finding among patients who present for treatment of hip pain. Previous reports have suggested that the prevalence of labral pathology among clinical populations ranges from 22% to 55%.3, 4, 5
Given the importance of a functional labrum and the high prevalence of labral dysfunction, it is imperative that surgical techniques are developed and used to restore the native labrum in cases of injury or degeneration. The original arthroscopic techniques that involved resection and debridement have largely fallen out of favor because of the growing emphasis on establishing and improving proper hip anatomy. Labral repair has been shown to be an effective treatment option that leads to greater improvement in pain, function, and return to activity when compared with resection or debridement.6 However, in cases of severe labral damage or when the labral tissue is too large or diminutive, labral repair may be less effective and labral reconstruction may be indicated (Table 1).
Table 1.
Indications and Contraindications for Arthroscopic Hip Labral Reconstruction in Patients With Labral Pathology
| Clinical indications |
| Labral tear that is considered irreparable7 |
| Intrasubstance labral degeneration |
| Diminutive labral tissue (<2-3 mm) or large labral tissue (>8 mm)8 |
| Previous labral treatment8, 9 |
| Rim ossification7 |
| Severe pincer lesion with lateral center-edge angle >45° |
| Potential contraindications |
| Older age (>60 yr)10 |
| Significant loss of rotational arc (>50%) |
| Joint space <50% of contralateral joint space10 |
The described technique broadens the orthopaedic surgeon's arsenal by providing an alternative to autograft labral reconstruction. The changes in technique and graft source may allow for use and integration of longer grafts, larger reconstructions, and reduced operative time. The purpose of this report is to present a modified technique for hip labral reconstruction using iliotibial band allograft tissue and a front-to-back approach.
Surgical Technique
The patient was placed in the supine position on a fracture table. Anesthesia used for the procedure was spinal anesthesia combined with a general anesthetic. In patients younger than 20 years, an epidural anesthetic was used. A heavy paralytic agent, rocuronium, was used at a loading dose of 1.5 mg per 1 kg. Traction was used intermittently throughout the procedure; the total time did not exceed 90 minutes (in intervals of 45 minutes or less).
Three portals were used for this procedure. The anterolateral portal was placed slightly anterior to the superior tip of the greater trochanter. The midanterior portal was placed under direct visualization and was located 6 cm medial to the anterolateral portal and roughly 1 cm distal. The third, accessory portal (distal anterolateral accessory [DALA] portal) was placed roughly 4 to 5 cm distal and 2 to 3 cm posterior to the anteromedial portal. The use of 3 portals was absolutely necessary to maintain appropriate graft tension throughout the procedure as the graft was fixed in position from the anterior aspect to the posterior aspect of the acetabular rim. Occasionally, a fourth portal (DALA 2 portal) was placed approximately 1 cm posterior to the DALA portal and was used if the angles for anchor insertion or suture tying were not perfect from the DALA 1 portal.
Femoral osteoplasty was performed when indicated to return the femoral neck to an anatomic shape and provide an excellent bleeding environment for graft incorporation (Fig 1, Video 1). After femoral osteoplasty, torn and damaged labral tissue (Fig 2, Video 1) was fully excised from the origin of the anterior transverse acetabular ligament posteriorly to the point of stable tissue. This is typically from the low anterior portion of the acetabulum at the origin of the transverse acetabular ligament (7:30 clock-face position in left hip and 4:30 clock-face position in right hip) to the posterior aspect of the acetabulum (3-o'clock position in left hip and 9-o'clock position in right hip). A round burr (4.0-mm Abrader Burr [Smith & Nephew, London, England] or 4.5-mm Prebent Spherical Burr [ConMed Linvatec, Utica, NY]) was used to reshape the acetabular rim. The goal was to establish an improved anatomic shape; remove the pincer lesion; and expose a flat, congruent bleeding surface on the acetabular rim for graft incorporation (Fig 3).
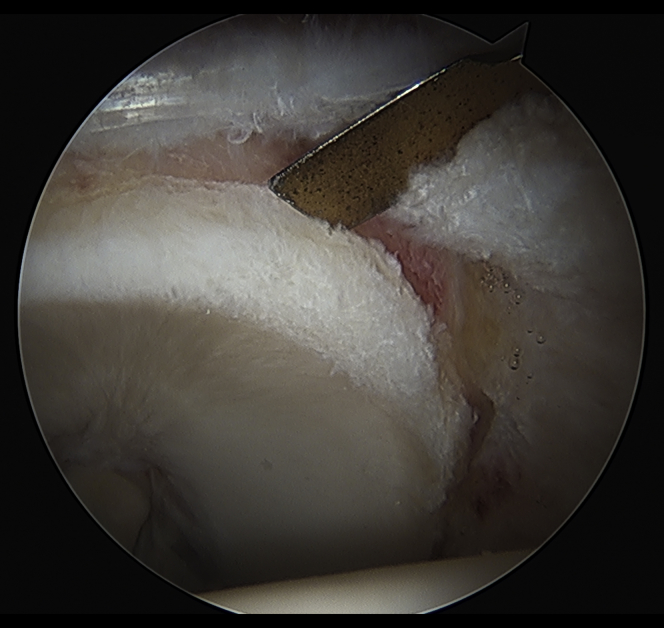
Fig 1.
From the anterolateral portal, we visualize the final femoral osteoplasty of a right hip undergoing arthroscopic allograft labral reconstruction using the front-to-back technique.
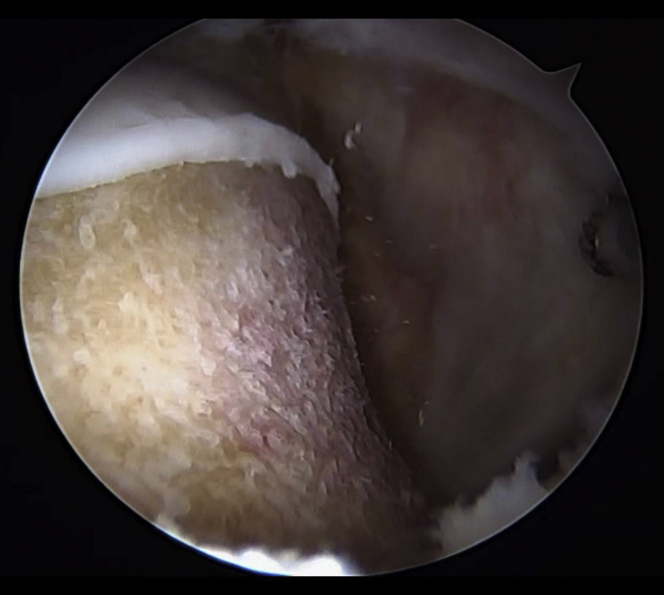
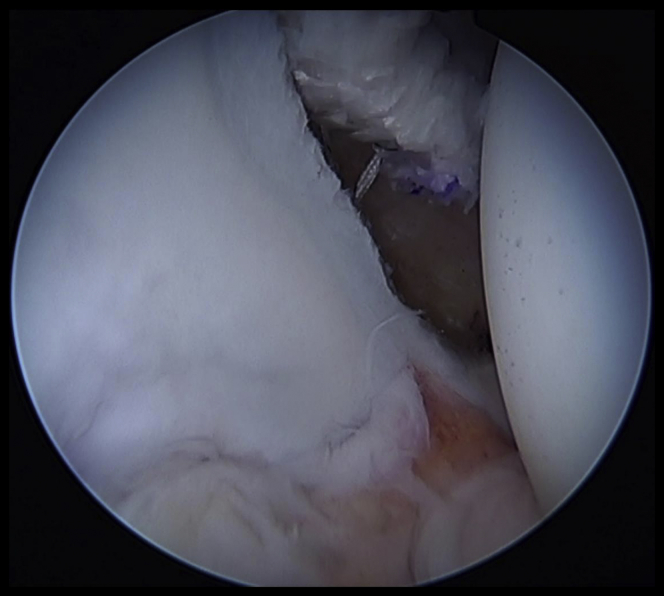
Fig 2.
A torn, irreparable labrum in a right hip viewed from the anterolateral portal.
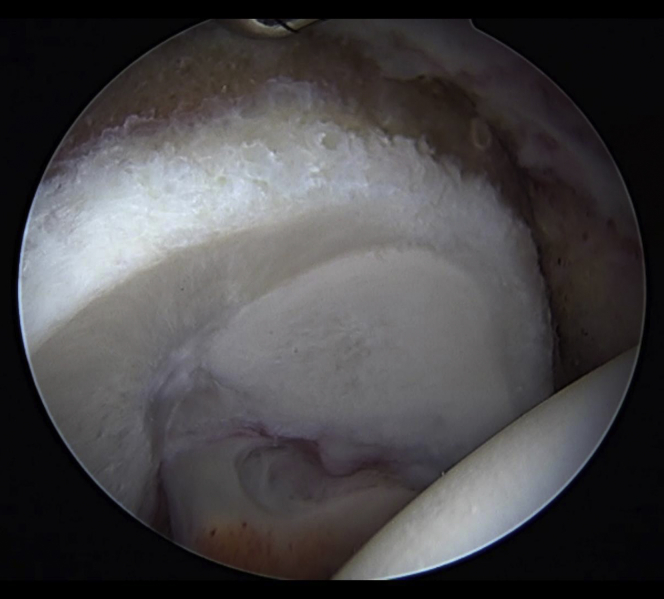
Fig 3.
The final prepared acetabular rim with the labrum resected between the 9-o'clock position and 4:30 clock-face position (origin of anterior transverse acetabular ligament) in a right hip. The pincer lesion has been resected, and the cartilage has been stabilized.
The extent of the labral defect was measured to determine the graft length (Fig 4). The graft length was overestimated to avoid the graft being too short. This can be 2 cm or more for large labral defects. The most anteroinferior anchor was placed adjacent to the origin of the anterior transverse acetabular ligament (Fig 5). Anchors were placed roughly 11 to 14 mm apart from the distal accessory portal into the acetabular rim (Fig 6, Video 1). They were placed as close to the acetabular edge as possible without breaching the joint. This is critical because, ultimately, the graft, when fixed, will be centered on the anchor. If the anchor is placed too far from the joint edge, it can be difficult to obtain a seal between the final labral reconstruction and the femoral head in this location. The anchors used depend on the thickness of the acetabular rim in each location and the bone quality. PEEK (polyether ether ketone) is the preferred anchor used when necessary (PressFT 2.1-mm PEEK/1.8-mm double-loaded Y-Knot all suture anchor [ConMed Linvatec]; 2.3-mm PEEK BioRaptor [Smith & Nephew]; or Biomet Juggerknot [Zimmer Biomet, Warsaw, IN]). Suture shuttling was performed through the anteromedial portal for anterior sutures and through the anterolateral portal for posterior sutures to allow for graft fixation and knot tying from the distal accessory portal (DALA 1 or 2 portal depending on the angle needed) (Fig 7).
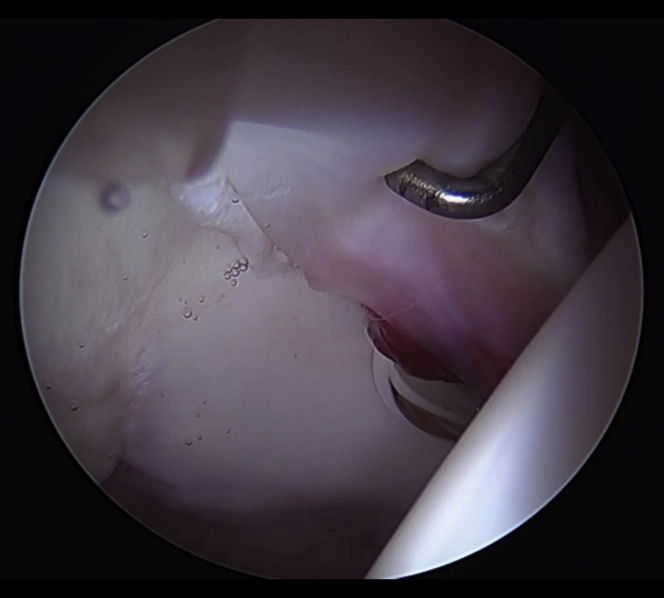
Fig 4.
Viewing from the anterolateral portal, a 4-mm-wide elevator inserted from the distal anterolateral accessory portal is used to measure the length of the labral defect from the front to the back in a right hip. This is used to estimate the final graft length. Typically, 15 to 20 mm is added to the final measurement to ensure that the graft is not too short.
Fig 5.
Viewing from the anterolateral portal, the first anchor in this right hip has been placed at the origin of the anterior transverse acetabular ligament and a drill guide is being placed to insert the second anchor in the iliopsoas fossa. All anchors are placed from the distal anterolateral accessory 1 and 2 portals.
Fig 6.
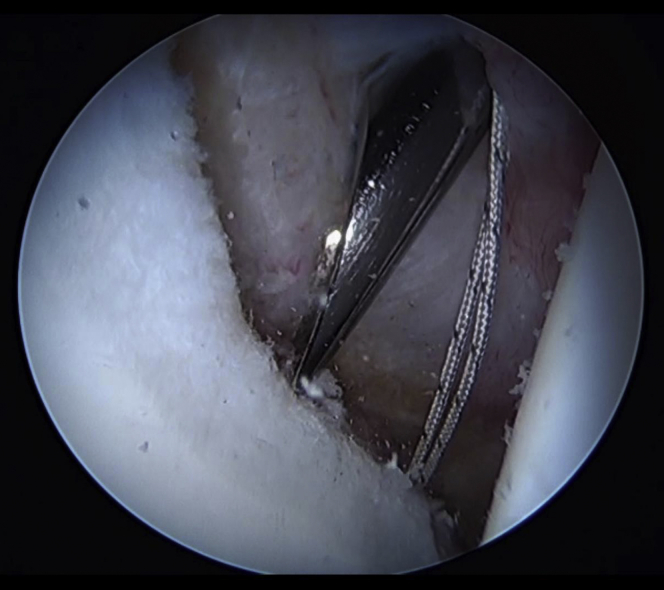
Viewing from the anterolateral portal, (A) anterior anchors and (B) posterior anchors are placed roughly 12 mm apart for this labral reconstruction in a right hip.
Fig 7.
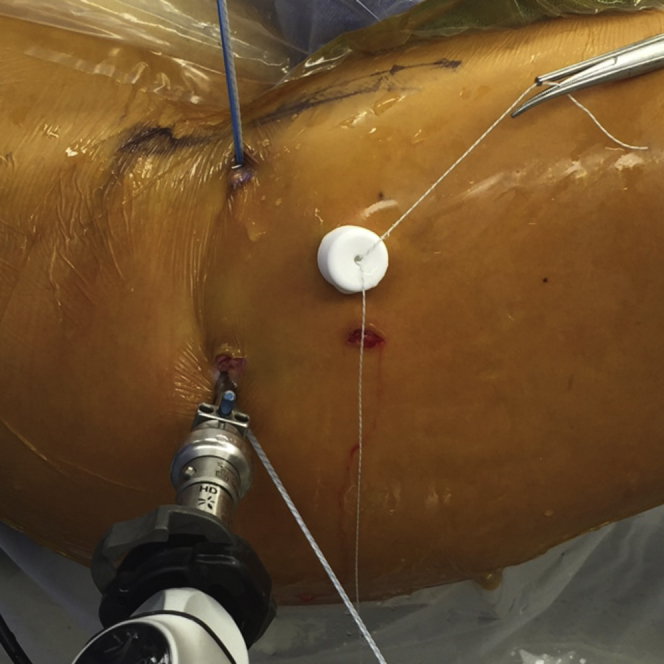
Suture shuttling is performed through the anteromedial portal for anterior anchors and through the anterolateral portal for posterior anchors in a right hip. The camera is in the anterolateral portal. The cannula is in the distal anterolateral 1 portal, and the distal anterolateral 2 portal is about 1 cm posterior to this.
The graft was prepared on the back table. Iliotibial band allograft (AlloSource, Centennial, CO, or MTF Sports Medicine, Edison, NJ), freeze dried or frozen, was soaked in solution comprising 250 mL of saline and 80 mg of gentamicin. Once thawed, the graft was measured and then rolled to create a final tubularized graft measuring roughly 5 to 6 mm in diameter to have adequate tissue to obtain a seal with the femoral head. The graft was folded into thirds, and a No. 2-0 Vicryl suture (Ethicon, Somerville, NJ) was placed at either end of the graft (Fig 8). An accordion-type suture technique was used in which several small bites were taken across the end of the graft; when tied, the tension bunched the graft and began the tubularization process (Fig 9). Each suture was secured in the Graftmaster (Smith & Nephew), and another No. 2-0 absorbable Vicryl suture was run up and down the length of the graft to tubularize the graft9 (Fig 10). The graft should be meticulously prepared so that it is tight and somewhat rigid. This will ensure that it is highly workable during the fixation process and that it does not significantly swell or fray.
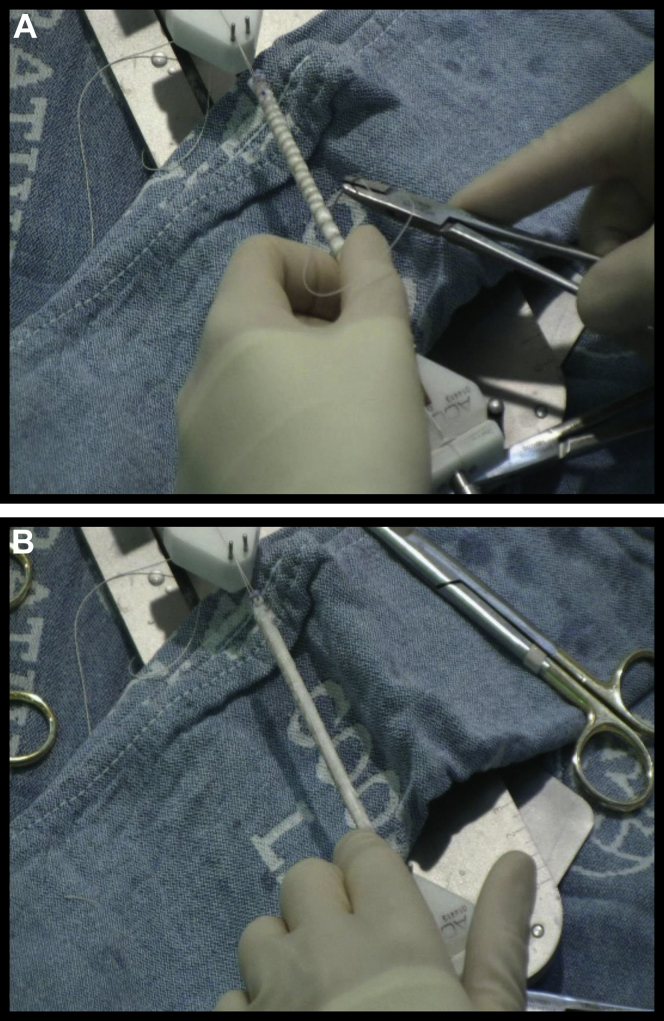
Fig 8.
The frozen fascia lata allograft for labral reconstruction has been measured and cut; at this point, it will be folded into thirds to begin the tubularization process.
Fig 9.
Small bites with No. 2-0 Vicryl on a small half (SH) needle are taken across each end of the prepared allograft to “accordion” them together and to provide a holding suture for the Graftmaster.
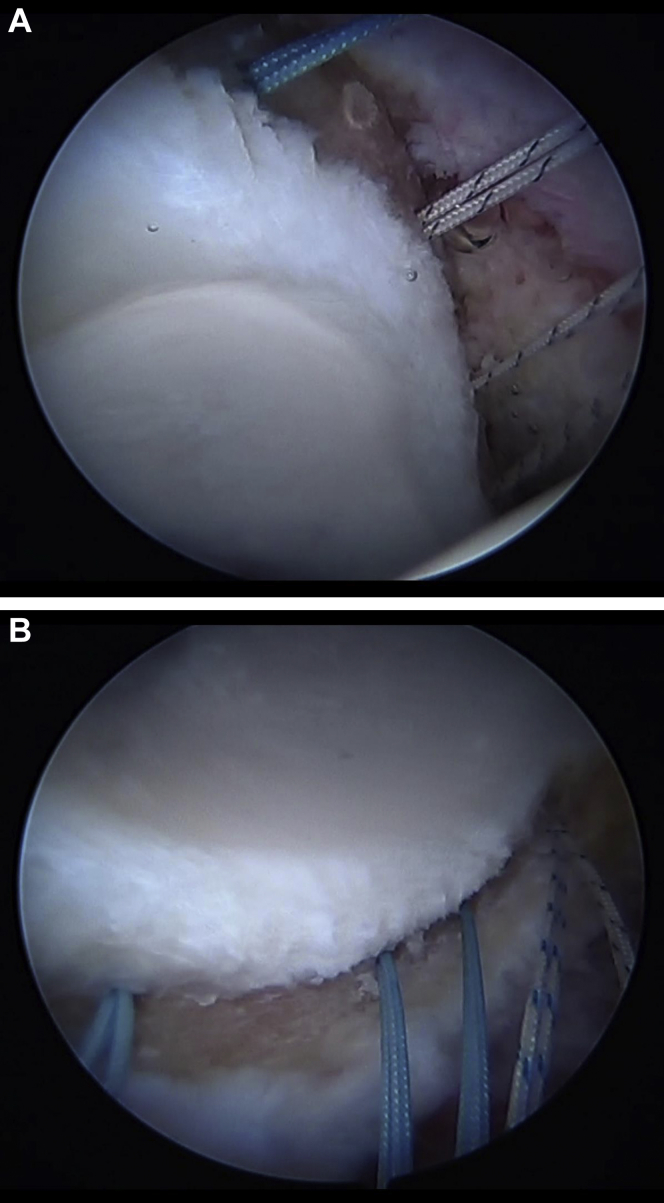
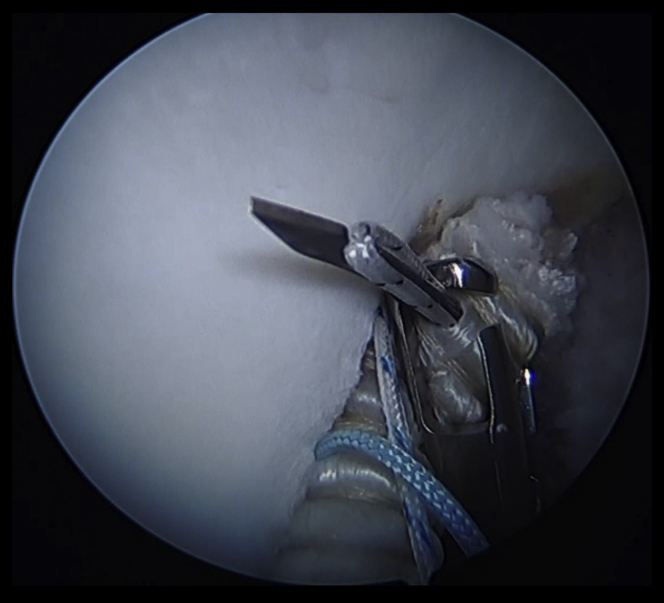
Fig 10.
(A) A running, non-locking No. 2-0 Vicryl suture is run up and back on the allograft to form a suitable, tight cylinder roughly 5 to 6 mm in diameter. (B) Meticulous preparation is critical to achieve a highly workable final graft that does not swell or fray.
A cannula (Clear-Trac Complete Threaded Hip Cannula, 8.5 mm × 110 mm; Smith & Nephew) was placed from the distal accessory portal through the intact anteroinferior capsule, aligning with the most anteroinferior suture. One end of this suture was made long and passed through the end of the graft. A simple knot was tied around and through the graft, ultimately fixing the graft to the suture (Fig 11). The shortened end of the suture (post suture) was pulled, bringing the anterior portion of the graft into the joint (Fig 12). The remainder of the graft was pushed through the cannula and into the joint (Fig 13). The graft was provisionally placed in an appropriate position along the acetabular rim (Fig 14). The first suture was secured with alternating half-hitch sutures, with the first 2 knots thrown in the same direction (Fig 15). Circumferential sutures were tied from the distal accessory portal (DALA 1 or 2), with the surgeon working from anterior to posterior (Video 1). The second-to-last suture was passed but not tied to allow for mobility at the end of the graft (Fig 16). With greater experience with this technique, occasionally, more anchors are passed and not tied so that the graft can be tensioned around the anterior aspect of the acetabulum to ensure that there is a perfect, tight seal between the graft and the femoral head with final fixation. The length of the graft was assessed (Fig 17). Excess graft was removed by cutting with a beaver blade (Procision USA S-6400; Havel's, Cincinnati, OH) from the anterolateral portal while maintaining tension from the distal accessory portal (Fig 18, Video 1). The most posterior suture was passed through the end of the graft with an ElitePass (Smith & Nephew) (Fig 19). This suture from the 1.8-mm double-loaded Y-Knot all-suture anchor (ConMed Linvatec) was then tied down. The other suture for this anchor was passed on the inside of this knot and tied circumferentially around the graft. This ultimately created a Mason-Allen type of suture construct, which allowed for compression of the graft and prevented this suture from slipping off of the end of the graft as it was tied (Fig 20). The remaining sutures were tied and secured from the DALA portals (Fig 21). Traction was taken down, and the graft was inspected in the peripheral compartment to ensure that there was a complete, continuous seal between the graft and the femoral head (Fig 22).11 Dynamic testing of the joint was performed, and the anterior portion of the capsule was closed (Video 1).
Fig 11.
The post suture of the first or most anteroinferior anchor is shortened, and the non–post suture is passed through the end of the graft. A simple knot is tied, and the suture is then passed through the graft to end up on the opposite side of the knot. Held in this fashion, the holding sutures and graft form a cross with the anchor suture. The holding sutures are ultimately cut.
Fig 12.
Pulling the post suture pulls the graft into the 8.5-mm × 110-mm Clear-Trac cannula and into the right hip joint.
Fig 13.
The graft is pushed through the cannula and into the right hip joint.
Fig 14.
Viewing from the anterolateral portal in a right hip, an arthroscopic probe is used from the anteromedial portal to position the graft into provisional position on the acetabular rim. Frequently, the camera and probe are switched between the anterolateral and anteromedial portals to achieve this.
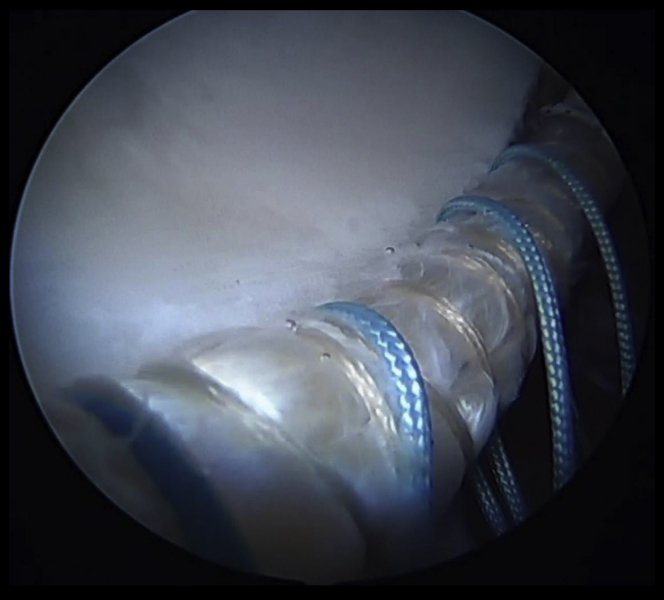
Fig 15.
Viewing from the anterolateral portal in a right hip, pulling on the post suture pulls the graft into final position so that it ultimately can be secured with arthroscopic knots.
Fig 16.
Viewing upside down from the anteromedial portal in a right hip, sutures are passed to be later tied once the graft has been tensioned, cut, and fixed posteriorly.
Fig 17.
Viewing upside down from the anteromedial portal in a right hip, a closed-ended grasper is used to hold the tensioned graft to assess where the graft should be cut to achieve the perfect length.
Fig 18.
Viewing upside down from the anteromedial portal in a right hip, a closed-ended grasper holds the excess end of the tensioned graft from the distal anterolateral 1 portal while a beaver blade (Procision) is used from the anterolateral portal to cut the graft.
Fig 19.
Viewing upside down from the anteromedial portal in a right hip, the ElitePass passes 1 suture (black tiger stripe) from the double-loaded 1.8-mm Y-Knot through the graft, which is then tied.
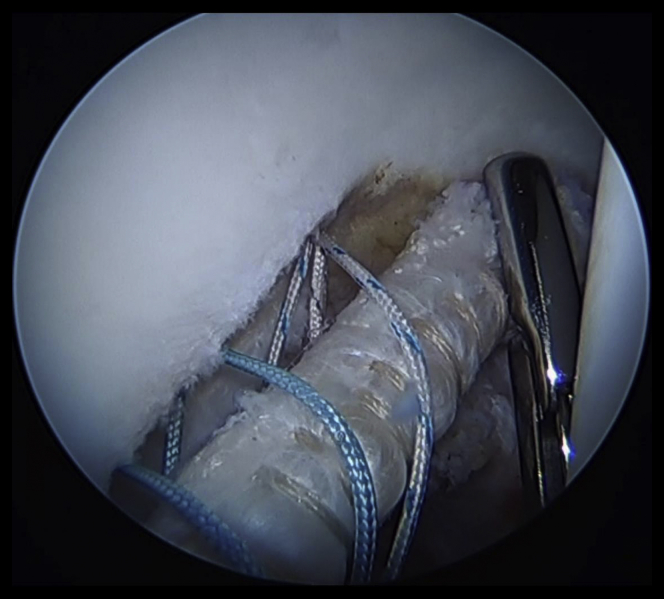
Fig 20.
Viewing upside down from the anteromedial portal in a right hip, the blue tiger stripe suture from the double-loaded Y-Knot is passed circumferentially above the previously tied black tiger suture. This Mason-Allen type of construct allows suitable compression of the graft end and prevents the circumferential suture from slipping off the end of the graft as it is tied.
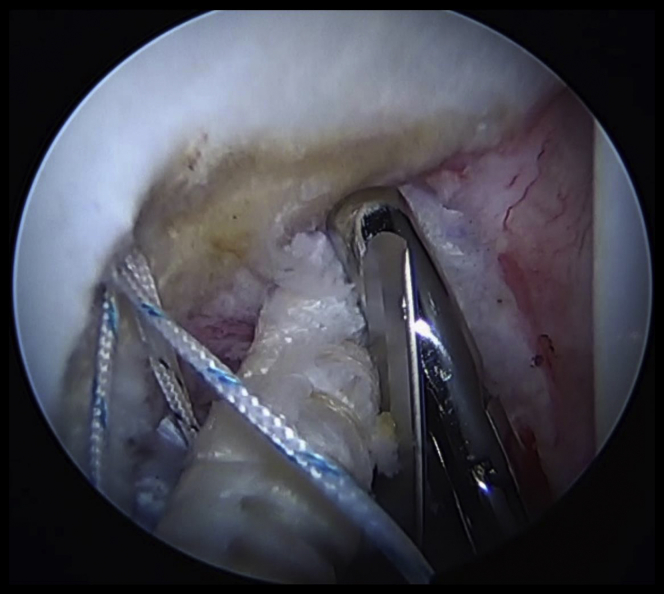
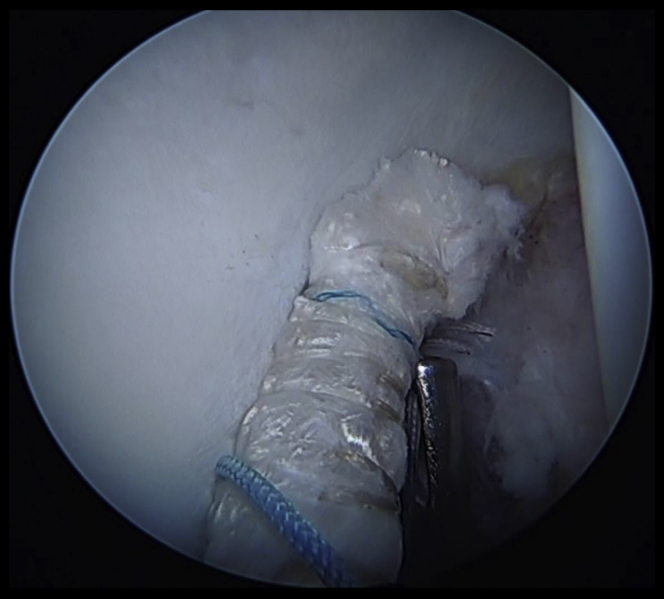
Fig 21.
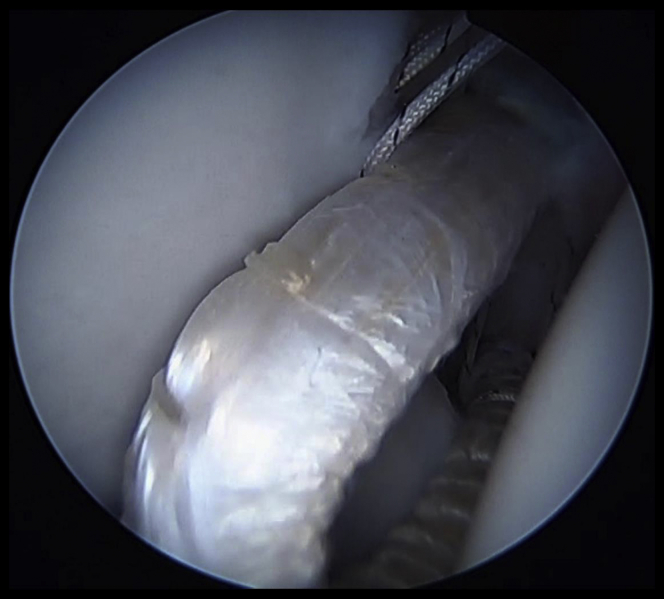
Viewing from the anterolateral portal in a right hip, (A) the graft is appropriately tensioned and (B) the final knot is tied through a cannula from the distal anterolateral accessory portal.
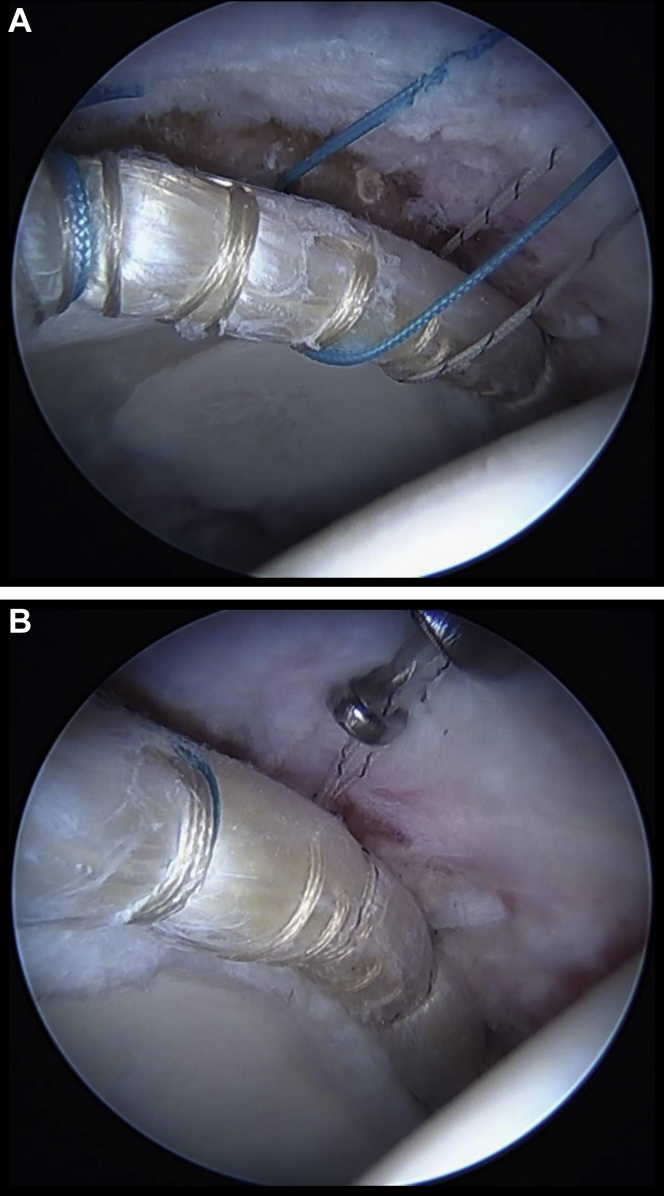
Fig 22.
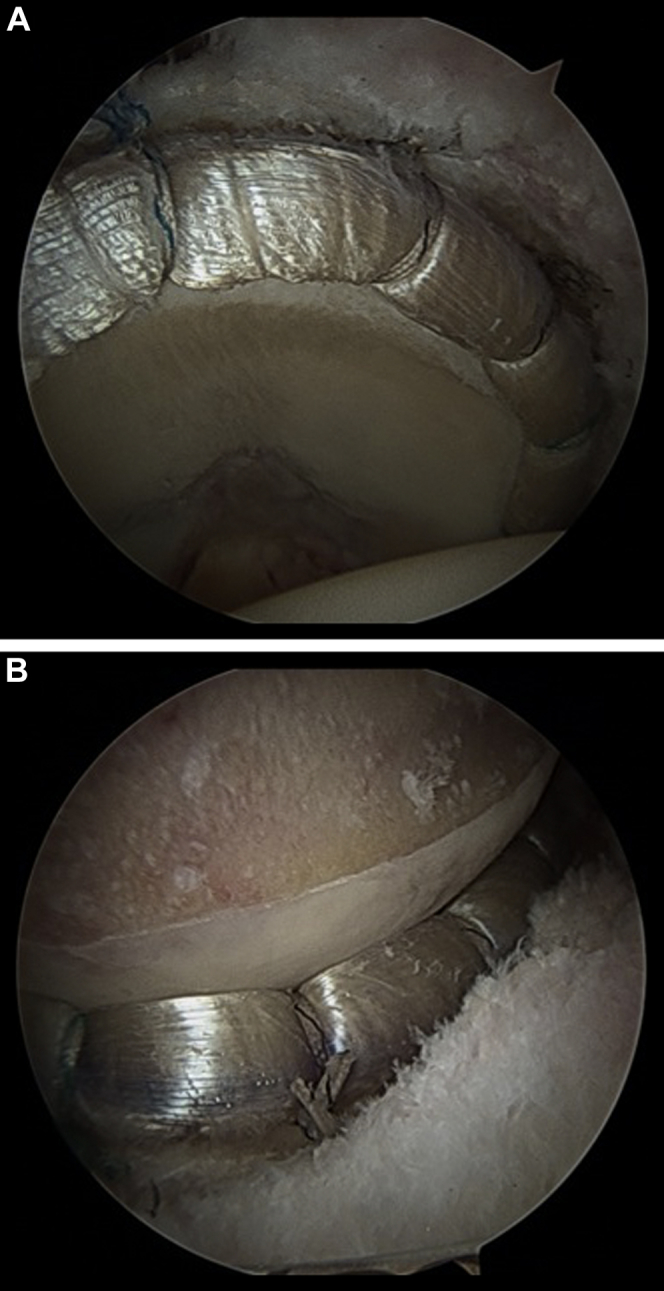
Final view of an 8-cm acetabular labral reconstruction from frozen fascia lata allograft in a right hip (A) fixed with 7 anchors viewed in traction and (B) with the joint reduced, showing a perfect seal between the labral reconstruction and the femoral head.
Reprinted with permission.11
Discussion
This technical note on our labral reconstruction technique is one of the first to report the use of allograft tissue for reconstruction. Labral reconstructions using iliotibial band autograft have been previously reported. The use of allograft tissue offers several advantages. First, allograft tissue gives an opportunity to create a more uniform, consistent graft because the most ideal section of the tissue can be used. This offers the best potential to create a final graft with a tubularized diameter of 5 to 6 mm. In addition, using longer grafts is possible because the graft length is not limited by the availability of host tissue. Allograft tissue is also more workable in the joint and less prone to swelling and fraying than tendinous grafts; however, allograft tissue does require meticulous preparation to make a graft that is easy to work with in the joint and does not swell. The longer graft also allows for complete replacement of the damaged labrum, especially the anteroinferior labrum, which may be prone to tearing in the future and become a late pain generator. Although the longer graft may be more technically demanding to work with, it gives the opportunity to create a more complete reconstruction and re-creation of normal anatomy. Achieving the perfect graft diameter requires a delicate balance: A graft that is too small is easy to incorporate but presents a challenge to obtaining a seal, whereas a graft that is too large in diameter makes it easy to obtain a seal but may be more difficult to incorporate. The most obvious and significant benefits of allograft are that it eliminates the potential for donor-site morbidity to the patient and reduces operative time.
The described technique for labral reconstruction is slightly modified from a previously reported technique.9 The variation from the original technique, which required first securing the graft anteriorly and posteriorly and then fixating at points in between,9 was used to avoid any discrepancy between the graft length and the size of the graft that is needed to fill the defect. With the previously described technique, if the graft was too long, bunching along the rim occurred. If it was too short, the graft either had to be stretched too tightly or was unable to span the entire graft site. Either situation could compromise the ultimate goal of establishing an effective seal between the labral graft and the femoral head. With the front-to-back technique, the initial graft is made approximately 1 cm longer than the intraoperative graft measurement. As the graft is fixed from front to back, the excess graft material is removed before the most posterior fixation. This technique eliminates any mismatch between the graft length and the labral defect and allows for the more consistent creation of the appropriate graft size. The technique allows for creation of the appropriate graft length that is reproducible and has accurate tension to create the appropriate seal. A potential disadvantage is the need for a third portal; however, we believe that the benefits outweigh this disadvantage.
The primary concern when using any labral reconstruction procedure is the technical demand. It is recommended that surgeons have been adequately trained in hip arthroscopy and have adequately practiced before attempting a large labral reconstruction because it is technically demanding. Surgeons should be very comfortable with and efficient in performing a thorough femoral osteoplasty and acetabular rim trimming and should be able to repair large labral tears before embarking on a labral reconstruction.12 The pearls and pitfalls of our technique are listed in Table 2.
Table 2.
Pearls and Pitfalls for Arthroscopic Labral Reconstruction of Hip Using Front-to-Back Fixation Technique and Iliotibial Allograft
| Pearls |
| Normal traction is used. |
| The use of 3 portals is necessary to maintain graft tension. |
| The anterolateral portal is used to visualize the anterior acetabulum. |
| The anteromedial portal is used to visualize the posterior acetabulum. |
| The peripheral compartment should be used to access the anteroinferior joint out of traction. |
| The distal portal (DALA portal) should be used to place anchors. |
| The graft should be shuttled in traction through the DALA portal through the intact anteroinferior capsule. |
| Pitfalls |
| Use of excess traction |
| Loss of anterior capsule integrity |
| Inability to access entire acetabulum |
| Lack of meticulous graft preparation |
| Inadequate anchor placement with anchors not placed as close to edge of acetabulum as possible without penetrating subchondral bone |
DALA, distal anterolateral accessory.
The described procedure adds to the available techniques for treatment of labral pathology by providing a labral reconstruction technique using allograft tissue. The benefits of allograft tissue and the front-to-back fixation technique should be considered when one is choosing a technique for labral reconstruction.
Acknowledgment
The authors thank Chris Pizzo and Joint Media Solutions for providing Video 1.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.J.W. receives support from ConMed, Linvatec, Smith & Nephew, Biomet, and ConMed Linvatec.
Supplementary Data
A right hip with an irreparable labral tear is shown, viewed arthroscopically from the anterolateral portal for viewing of the anterior portion of the acetabulum and from the anteromedial portal for an upside-down view of the posterior acetabulum. The key steps for the front-to-back technique for arthroscopic labral reconstruction with fascia lata allograft are presented. The key steps begin with a thorough femoral osteoplasty and preparation of the acetabular rim to both create an appropriate healing environment for the graft and stabilize the cartilage. Access to the most anterior aspect of the acetabulum is then established through an intact anteroinferior capsule from the distal accessory portal. Anchors are placed and separated by roughly 11 to 13 mm through the zone of reconstruction (9-o'clock position to 4:30 clock-face position) because exposure is best before graft insertion. The graft is fixed to the non–post suture of the most anterior anchor and pulled into the joint by the post suture. The graft is progressively tensioned and fixed with circumferential anchors from anterior to posterior. Posterior excess graft is cut to ensure the perfect graft length. Once complete, the femoral head is reduced and the graft is assessed to ensure that there is a perfect, secure seal between the graft and the femoral head. The anterior portion of the graft is then closed.
References
- 1.Philippon M.J., Nepple J.J., Campbell K.J. The hip fluid seal—Part I: The effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22:722–729. doi: 10.1007/s00167-014-2874-z. [DOI] [PubMed] [Google Scholar]
- 2.Nepple J.J., Philippon M.J., Campbell K.J. The hip fluid seal—Part II: The effect of an acetabular labral tear, repair, resection, and reconstruction on hip stability to distraction. Knee Surg Sports Traumatol Arthrosc. 2014;22:730–736. doi: 10.1007/s00167-014-2875-y. [DOI] [PubMed] [Google Scholar]
- 3.Reiman M.P., Goode A.P., Cook C.E., Holmich P., Thorborg K. Diagnostic accuracy of clinical tests for the diagnosis of hip femoroacetabular impingement/labral tear: A systematic review with meta-analysis. Br J Sports Med. 2015;49:811. doi: 10.1136/bjsports-2014-094302. [DOI] [PubMed] [Google Scholar]
- 4.McCarthy J.C., Noble P.C., Schuck M.R., Wright J., Lee J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001:25–37. doi: 10.1097/00003086-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Narvani A.A., Tsiridis E., Kendall S., Chaudhuri R., Thomas P. A preliminary report on prevalence of acetabular labrum tears in sports patients with groin pain. Knee Surg Sports Traumatol Arthrosc. 2003;11:403–408. doi: 10.1007/s00167-003-0390-7. [DOI] [PubMed] [Google Scholar]
- 6.Larson C.M., Giveans M.R. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369–376. doi: 10.1016/j.arthro.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 7.Ayeni O.R., Alradwan H., de Sa D., Philippon M.J. The hip labrum reconstruction: Indications and outcomes—A systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22:737–743. doi: 10.1007/s00167-013-2804-5. [DOI] [PubMed] [Google Scholar]
- 8.Ejnisman L., Philippon M.J., Lertwanich P. Acetabular labral tears: Diagnosis, repair, and a method for labral reconstruction. Clin Sports Med. 2011;30:317–329. doi: 10.1016/j.csm.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Philippon M.J., Briggs K.K., Hay C.J., Kuppersmith D.A., Dewing C.B., Huang M.J. Arthroscopic labral reconstruction in the hip using iliotibial band autograft: Technique and early outcomes. Arthroscopy. 2010;26:750–756. doi: 10.1016/j.arthro.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 10.Geyer M.R., Philippon M.J., Fagrelius T.S., Briggs K.K. Acetabular labral reconstruction with an iliotibial band autograft: Outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med. 2013;41:1750–1756. doi: 10.1177/0363546513487311. [DOI] [PubMed] [Google Scholar]
- 11.White B.J., Stapleford A.B., Hawkes T.K., Finger M.J., Herzog M.M. Allograft use in arthroscopic labral reconstruction of the hip: Minimum 2-year follow-up with front-to-back fixation technique. Arthroscopy. 2016;32:26–32. doi: 10.1016/j.arthro.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 12.McCarthy J.C., Lee J. Hip arthroscopy: Indications and technical pearls. Clin Orthop Relat Res. 2005;441:180–187. doi: 10.1097/01.blo.0000195057.27653.93. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A right hip with an irreparable labral tear is shown, viewed arthroscopically from the anterolateral portal for viewing of the anterior portion of the acetabulum and from the anteromedial portal for an upside-down view of the posterior acetabulum. The key steps for the front-to-back technique for arthroscopic labral reconstruction with fascia lata allograft are presented. The key steps begin with a thorough femoral osteoplasty and preparation of the acetabular rim to both create an appropriate healing environment for the graft and stabilize the cartilage. Access to the most anterior aspect of the acetabulum is then established through an intact anteroinferior capsule from the distal accessory portal. Anchors are placed and separated by roughly 11 to 13 mm through the zone of reconstruction (9-o'clock position to 4:30 clock-face position) because exposure is best before graft insertion. The graft is fixed to the non–post suture of the most anterior anchor and pulled into the joint by the post suture. The graft is progressively tensioned and fixed with circumferential anchors from anterior to posterior. Posterior excess graft is cut to ensure the perfect graft length. Once complete, the femoral head is reduced and the graft is assessed to ensure that there is a perfect, secure seal between the graft and the femoral head. The anterior portion of the graft is then closed.