Abstract
Abductor tendon tears typically develop insidiously in middle-aged women and can lead to debilitating lateral hip pain and a Trendelenburg limp. The gluteus medius tendon is most commonly torn and may show fatty degeneration over time, similar to the rotator cuff muscles of the shoulder. Endoscopic repair offers a therapeutic alternative to traditional open techniques. This article describes the workup, examination, and endoscopic repair of a full-thickness gluteus medius tear presenting as lateral hip pain and weakness. The surgical repair for this case used a single-row suture anchor technique. In addition, the indications and technique for a double-row repair will be discussed.
Abductor tendon tears have been diagnosed with increasing frequency over the past 2 decades.1, 2 More frequent diagnosis can be attributed in part to the increased use of magnetic resonance imaging (MRI), as well as an increased awareness within the orthopaedic community. Tears of the gluteus medius and minimus were first described in the 1990s as “rotator cuff tears of the hip”3, 4 and follow the same patterns of retraction, fatty atrophy, and occasional calcification as seen in the shoulder.
Most hip abductor tears involve the gluteus medius tendon.5 The gluteus medius is a large fan-shaped muscle originating from the outer edge of the iliac crest, extending from the anterior superior iliac spine to the posterior superior iliac spine. The anterior and middle muscular fibers are vertically oriented. The posterior fibers are horizontally oriented, running parallel to the femoral neck and the fibers of the gluteus minimus inserting anterior to it. The gluteus medius inserts onto the superoposterior and lateral facets of the greater trochanter. There is an intervening “bald spot” situated between its insertion and that of the gluteus minimus onto the anterior facet.5 Midsubstance tears have been described,6 but most commonly, the gluteus medius ruptures from its lateral facet footprint.7 As with any degenerative tendon tear, gluteal tendon pathology can progress through a process of bursitis, tendinopathy, partial-thickness tears, full-thickness tears, and massive tears with associated fatty infiltration and atrophy.
Clinical Evaluation
Abductor tendon tears occur up to 4 times more frequently in women than in men, possibly because of the wider female pelvis.1, 3, 5 Some evidence suggests that tears occur in 25% of middle-aged women and 10% of middle-aged men.5 Lachiewicz8 has described 3 classic presentations. The most common presentation involves the atraumatic insidious onset of lateral-sided hip pain. These tears are often degenerative in nature and are associated with a higher degree of fatty atrophy. Tears may also be discovered as an incidental finding at the time of open hip surgery, such as femoral neck fracture fixation or joint arthroplasty. The third scenario presented by Lachiewicz involves an iatrogenic abductor tendon avulsion after a direct Hardinge lateral approach to the hip. This approach splits the gluteus medius and may create a defect at the tendon footprint if not adequately repaired.
Physical assessment of a patient complaining of lateral hip pain should begin with an evaluation of gait. A Trendelenburg gait, in which the pelvis drops toward the contralateral side during a single-limb stance, signals abductor weakness. Patients may have tenderness over the greater trochanter and weakness with resisted hip abduction. Trochanteric bursitis similarly presents in middle-aged women, but unlike abductor tendon tears, bursitis is characterized by tenderness to palpation without associated abductor weakness. External coxa saltans, or snapping hip syndrome, can also cause lateral hip pain. This condition typically afflicts younger women in their second or third decade of life and is characterized by a palpable, or even audible, snap of the iliotibial band over the greater trochanter. External snapping may be reproduced by flexing and extending the hip with the patient in the lateral decubitus position. Other less common diagnostic considerations include an occult fracture of the proximal femur, lumbar spondylosis or spinal stenosis, and neuropathy of the superior gluteal nerve, which may be associated with diabetes mellitus and rheumatoid arthritis.8
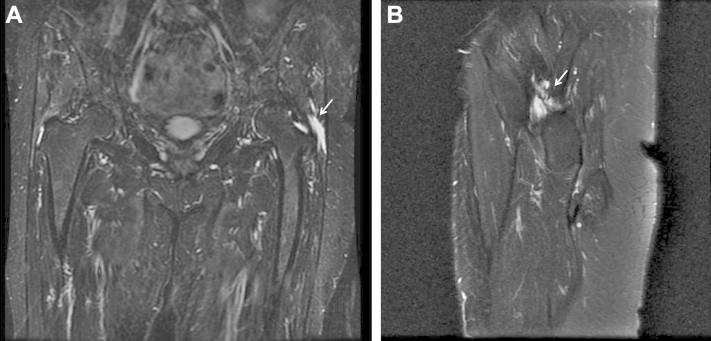
Initial treatment should consist of a trial of conservative management including nonsteroidal anti-inflammatory drugs and physical therapy focusing on range of motion and abductor strengthening. Pain that is recalcitrant to corticosteroid injections and other nonoperative treatment may be further evaluated with advanced imaging. Ultrasound may identify thickening or fluid signals with 79% sensitivity and a nearly 100% positive predictive value,9 but it is highly user dependent. MRI allows differentiation between partial- and full-thickness tears and may also be used to characterize the degree of tendon calcification and fatty atrophy. Partial or complete defects are best visualized as a hyperintense signal on T2-weighted MRI (Fig 1), whereas T1-weighted sequences are best for identifying the degree of fatty degeneration (Fig 2). When a tear is visible on MRI, surgical repair should be considered early to impede gradual degeneration.8
Fig 1.
(A) T2-weighted coronal magnetic resonance image of the pelvis showing a full-thickness gluteus medius tear (arrow) of the left hip. (B) T2-weighted sagittal series may be used to estimate the amount of tendon retraction (arrow).
Fig 2.
A T1-weighted coronal magnetic resonance image may be used to estimate the extent of fatty degeneration (arrow) of the gluteus medius of the left hip.
Surgical Technique
The patient is positioned supine on a standard traction table with an attached hip distraction system, well-padded boots, and a perineal post (Advanced Supine Hip Positioning System; Smith & Nephew, Memphis, TN). After the induction of general anesthesia, the patient is shifted toward the foot of the bed so that the post is abutting the perineum. The pelvis is slightly translated toward the contralateral hip, and gentle distraction is applied to the contralateral limb.
First, a diagnostic arthroscopy is performed to rule out concomitant sources of pain. Traction is applied to the operative limb using gentle oscillations to alleviate muscular tension as the limb is slowly extended and adducted. The joint may distract up to 10 mm with this maneuver, and an audible pop may be heard, indicating disruption of the hip chondrolabral suction seal. After sterile preparation and draping, the greater trochanter is marked by palpation. An anterolateral (AL) portal is established first, 1 cm proximal and 1 cm anterior to the AL tip of the greater trochanter. The surgeon may err proximally for better visualization of the gluteus medius insertion onto the superoposterior facet of the greater trochanter. Under fluoroscopic guidance, standard cannulation (8.5 × 110 mm; Smith & Nephew) into the joint is performed 1 to 2 mm above the femoral head and below the labrum. A 70° arthroscope (Smith & Nephew) is placed through the AL portal. Next, the midanterior portal (MAP) is made 4 to 5 cm medial and 1 cm inferior to the AL portal over the vastus ridge. If indicated, any necessary chondrolabral, osseous, or capsular work may be performed.
Attention is then turned to the gluteus medius repair (Video 1, Table 1). Traction is released, and the hip is abducted 15° to 20° to relieve gluteal tension. The peritrochanteric space is then entered with use of a 5.0-mm metal cannula (Smith & Nephew) through the MAP; the cannula is directed between the iliotibial band and the lateral aspect of the greater trochanter and is then swept from proximal to distal, opening the potential space. A 70° arthroscope is placed through the cannula and is used to visualize the distal aspect of the peritrochanteric space by aiming the arthroscope and light source distally.
Table 1.
Pearls and Pitfalls of Endoscopic Single-Row Gluteus Medius Repair
| Pearls | Pitfalls |
|---|---|
| Use a midanterior viewing portal to enable working portals anterolaterally and posterolaterally. | Do not neglect to release traction and abduct the hip 15°-20° to relieve gluteal tension. |
| Use a 4.5-mm shaver or thermal ablation (or both) to resect tenuous bands of bursal tissue. | Do not perform incomplete bursectomy; the surgeon should be able to visualize the undersurface of the gluteus maximus and the longitudinal fibers of the vastus lateralis medially. |
| Decorticate the tendon footprint to create a bleeding surface for healing. | Do not establish a separate portal for suture anchor placement; suture anchors may be placed percutaneously to limit soft-tissue morbidity. |
| Establish a posterolateral working portal to facilitate suture passage through the anterior leaflet of the tear. | Do not ignore the gluteus minimus tendon; it must be evaluated and, if injured, repaired with an additional suture anchor. |
With use of a Wissinger rod through the AL portal, another 5.0-mm metal cannula is positioned between the tip of the greater trochanter and the iliotibial band. A 4.5-mm shaver (Stryker, Kalamazoo, MI) is introduced and used to resect tenuous bands of bursal tissue. The bursectomy is continued until the gluteus maximus insertion is identified distally, the iliotibial band laterally, the undersurface of the gluteus maximus proximally, and the longitudinal fibers of the vastus lateralis medially. The gluteus medius typically has a thick tendinous insertion onto the posterosuperior facet and a thinner, muscular attachment onto the lateral facet.5, 10, 11 The surgeon should now be able to locate the gluteus medius along the lateral footprint of the greater trochanter and the gluteus minimus inserting anteriorly. A probe may be used to explore the bursal side of the tendon. Partial-thickness tears are commonly articular sided—and thus difficult to see directly—but they can be indirectly evaluated with dynamic examination.
With use of a grasper (Arthrex, Naples, FL), the excursion of the gluteus medius tendon is evaluated in relation to its footprint along the superoposterior and lateral facets (Fig 3). A repairable tendon tear can be pulled laterally to the footprint without significant tension. Depending on the chronicity and retraction of the tear, adhesions may need to be released with a thermal ablator (Smith & Nephew) to improve the tendon’s excursion. The footprint is then decorticated with an arthroscopic burr (Stryker) to create a bleeding surface for healing. A spinal needle may be placed to determine the appropriate trajectory for suture anchor placement at the lateral footprint of the greater trochanter. One 5.5-mm triple-loaded suture anchor (Biosteon; Stryker) is placed percutaneously (Fig 4). A posterolateral (PL) portal is then established 1 cm proximal and posterior to the PL corner of the greater trochanter. One of the sutures is retrieved with a tissue-penetrating device (Slingshot; Stryker Sports Medicine, Greenwood Village, CO) through the PL portal and passed through the anterior edge of the tendinous tissue 1 to 2 cm from its distal edge. The second limb is passed a few millimeters directly distal to create a horizontal mattress configuration. These steps are repeated for the second suture of the anchor. All 4 suture limbs are retrieved through the PL portal. The third suture is passed in a horizontal mattress configuration through the posterior leaflet using an InJector II (Stryker Sports Medicine) through the PL portal (Fig 5). For tears involving the gluteus minimus, another anchor can be placed in the gluteus minimus footprint using spinal needle localization. The posterior suture is tied with reverse half-hitches and alternating posts through the PL portal. The camera is switched to the AL portal for improved visualization of the anterior leaflet as the final 2 sutures are tied. For single-row fixation, the suture limbs are cut, and the hip is gently adducted and abducted to assess the tension of the repair.
Fig 3.
Endoscopic image of a left hip viewed from the midanterior portal with a grasper through the anterolateral portal. The grasper is pulling the posterior leaflet of a full-thickness gluteus medius tear (PL), with the footprint to the left of the image. (AL, anterior leaflet of gluteus medius tear.)
Fig 4.

Endoscopic image of a left hip viewed from the midanterior portal depicting 3 sutures from a triple-loaded suture anchor. The anchor has been placed in the center of the gluteus medius tendon footprint between the anterior leaflet (AL) and posterior leaflet (PL) of the gluteus medius tear.
Fig 5.

Endoscopic image of a left hip viewed from the midanterior portal with an InJector II being used through the posterolateral portal to pass suture through the posterior leaflet of the gluteus medius tear (PL).
Double-row fixation may be considered for particularly massive tears that are retracted or have diffuse fatty degeneration requiring extensive debridement. For double-row fixation, the suture limbs from the proximal row are used to create a suture bridge construct over the surface of the tendon (Fig 6). The posterior limbs are fed through a knotless anchor (SwiveLock; Arthrex), which is placed in line with the most posterior proximal anchor. Full tension is maintained on the suture limbs before impacting the anchor into bone. This same process is repeated for the anterior suture limbs and anterior knotless anchor.
Fig 6.

Endoscopic image of a right hip viewed from the anterolateral portal depicting a double-row suture bridge construct. If the tear is large and retracted, a lateral row can be used to increase the stiffness of the repair construct.
Postoperatively, the patient is placed into an abduction pillow (Ossur, Foothill Ranch, CA), which should be worn at night. In the recovery unit, patients are fitted for a hip abduction orthosis (Ossur) that limits flexion to 0° to 90°. Patients are instructed to use crutches with 20-lb flat-foot weight-bearing restrictions for 6 weeks. They are encouraged to use continuous passive motion and a stationary bicycle for the first 3 weeks. Early strengthening is focused on core and proximal neuromotor control. Progressive abductor strengthening is started after 12 weeks.
Discussion
Surgery for abductor tendon tears has classically involved an open repair, but recent innovations have enabled endoscopic repair. The purpose of this article is to describe our repair technique for full-thickness tears of the gluteus medius tendon.
Most of the basic science literature on single- or double-row tendon repairs has focused on the rotator cuff. Biomechanical data have shown double-row repairs of the rotator cuff to have a higher load to failure, smaller gap formation, higher tensile load, and enhanced healing rate (in a sheep model) when compared with single-row constructs.12, 13, 14 These results, however, have not yet translated to a difference in clinical outcomes, so single-row repair is still widely used. Many surgeons reserve double-row fixation for massive or severely retracted rotator cuff tears. The biomechanical literature on gluteal repairs is sparse. Dishkin-Paset et al.15 used a cadaveric model to compare different double-row suture configurations, but no studies to date have evaluated the biomechanical strength of single-row techniques in the hip.
Clinical outcome literature on gluteal tendon repairs consists entirely of Level IV evidence case series with no more than 72 patients reported in a single study.16, 17 The first open repair technique was described in 1997 by Weber and Berry,18 who reported suture repairs in 9 patients with abductor avulsions after primary total hip arthroplasty. Open techniques have evolved to suture anchors and even more complex models, such as the Ligament Augment and Reconstruction System (LARS, Arc sur Tille, France)19, 20 and biologic patch augmentation.21, 22, 23 Voos et al.7, 24 described the first endoscopic technique using suture anchors in 2007 and reported no pain or complications in all 10 patients at a mean follow-up of 25 months. More recent reports have confirmed excellent patient-reported outcomes at similar time points after endoscopic repair.25, 26 In 2013 Domb et al.25 reported good to excellent patient satisfaction in 14 of 15 patients and significant improvements in modified Harris Hip, Hip Outcome, and Non-Arthritic Hip Scores. In addition, a trochanteric microfracture technique has recently been reported to address gluteus medius tendinopathy without evidence of a discrete tear.27 No patients in endoscopic case series to date have required a revision repair.16
In conclusion, endoscopic single-row suture repair is an effective technique for addressing isolated full-thickness tears of the gluteus medius tendon. The single-row technique can be performed through just 3 endoscopic portals (AL portal, MAP, and PL portal), thus minimizing soft-tissue morbidity. Larger tears with more extensive retraction or fatty atrophy may require a double-row or open technique. With proper patient selection and early surgical intervention, however, the single-row technique can be used to successfully repair most full-thickness gluteal tendon tears.
Footnotes
The authors report the following potential conflict of interest or source of funding: C.A.B.-J. receives support from American Journal of Sports Medicine. S.J.N. receives support from Journal of Bone and Joint Surgery, Stryker, Ossur, Allosource, Arthrex, Athletico, DJ Orthopaedics, Linvatec, Miomed, and Smith & Nephew.
Supplementary Data
The technique for gluteus medius tendon repair with a single-row construct is shown. A repair of a left hip gluteus medius tear, mostly through a midanterior viewing portal, is shown, except when otherwise noted.
References
- 1.Strauss E.J., Nho S.J., Kelly B.T. Greater trochanteric pain syndrome. Sports Med Arthrosc. 2010;18:113–119. doi: 10.1097/JSA.0b013e3181e0b2ff. [DOI] [PubMed] [Google Scholar]
- 2.Bird P.A., Oakley S.P., Shnier R., Kirkham B.W. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis Rheum. 2001;44:2138–2145. doi: 10.1002/1529-0131(200109)44:9<2138::AID-ART367>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 3.Bunker T.D., Esler C.N., Leach W.J. Rotator-cuff tear of the hip. J Bone Joint Surg Br. 1997;79:618–620. doi: 10.1302/0301-620x.79b4.7033. [DOI] [PubMed] [Google Scholar]
- 4.Kagan A. Rotator cuff tears of the hip. Clin Orthop Relat Res. 1999;368:135–140. [PubMed] [Google Scholar]
- 5.Robertson W.J., Gardner M.J., Barker J.U., Boraiah S., Lorich D.G., Kelly B.T. Anatomy and dimensions of the gluteus medius tendon insertion. Arthroscopy. 2008;24:130–136. doi: 10.1016/j.arthro.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Yanke A.B., Hart M.A., McCormick F., Nho S.J. Endoscopic repair of a gluteus medius tear at the musculotendinous junction. Arthrosc Tech. 2013;2:e69–e72. doi: 10.1016/j.eats.2012.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Voos J.E., Rudzki J.R., Shindle M.K., Martin H., Kelly B.T. Arthroscopic anatomy and surgical techniques for peritrochanteric space disorders in the hip. Arthroscopy. 2007;23:1246.e1–1246.e5. doi: 10.1016/j.arthro.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 8.Lachiewicz P.F. Abductor tendon tears of the hip: Evaluation and management. J Am Acad Orthop Surg. 2011;19:385–391. doi: 10.5435/00124635-201107000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Westacott D.J., Minns J.I., Foguet P. The diagnostic accuracy of magnetic resonance imaging and ultrasonography in gluteal tendon tears—A systematic review. Hip Int. 2011;21:637–645. doi: 10.5301/HIP.2011.8759. [DOI] [PubMed] [Google Scholar]
- 10.Domb B.G., Nasser R.M., Botser I.B. Partial-thickness tears of the gluteus medius: Rationale and technique for trans-tendinous endoscopic repair. Arthroscopy. 2010;26:1697–1705. doi: 10.1016/j.arthro.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Dwek J., Pfirrmann C., Stanley A., Pathria M., Chung C.B. MR imaging of the hip abductors: Normal anatomy and commonly encountered pathology at the greater trochanter. Magn Reson Imaging Clin N Am. 2005;13:691–704. doi: 10.1016/j.mric.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Lorbach O., Bachelier F., Vees J., Kohn D., Pape D. Cyclic loading of rotator cuff reconstructions: Single-row repair with modified suture configurations versus double-row repair. Am J Sports Med. 2008;36:1504–1510. doi: 10.1177/0363546508314424. [DOI] [PubMed] [Google Scholar]
- 13.Baums M.H., Spahn G., Buchhorn G.H., Schultz W., Hofmann L., Klinger H.-M. Biomechanical and magnetic resonance imaging evaluation of a single- and double-row rotator cuff repair in an in vivo sheep model. Arthroscopy. 2012;28:769–777. doi: 10.1016/j.arthro.2011.11.019. [DOI] [PubMed] [Google Scholar]
- 14.Ma C.B., Comerford L., Wilson J., Puttlitz C.M. Biomechanical evaluation of arthroscopic rotator cuff repairs: Double-row compared with single-row fixation. J Bone Joint Surg Am. 2006;88:403–410. doi: 10.2106/JBJS.D.02887. [DOI] [PubMed] [Google Scholar]
- 15.Dishkin-Paset J.G., Salata M.J., Gross C.E. A biomechanical comparison of repair techniques for complete gluteus medius tears. Arthroscopy. 2012;28:1410–1416. doi: 10.1016/j.arthro.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Ebert J.R., Bucher T.A., Ball S.V., Janes G.C. A review of surgical repair methods and patient outcomes for gluteal tendon tears. Hip Int. 2015;25:15–23. doi: 10.5301/hipint.5000183. [DOI] [PubMed] [Google Scholar]
- 17.Walsh M.J., Walton J.R., Walsh N.A. Surgical repair of the gluteal tendons: A report of 72 cases. J Arthroplasty. 2011;26:1514–1519. doi: 10.1016/j.arth.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Weber M., Berry D.J. Abductor avulsion after primary total hip arthroplasty. Results of repair. J Arthroplasty. 1997;12:202–206. doi: 10.1016/s0883-5403(97)90067-x. [DOI] [PubMed] [Google Scholar]
- 19.Bajwa A.S., Campbell D.G., Comely A.S., Lewis P.L. Gluteal tendon reconstruction in association with hip arthroplasty. Hip Int. 2011;21:288–292. doi: 10.5301/HIP.2011.8414. [DOI] [PubMed] [Google Scholar]
- 20.Bucher T.A., Darcy P., Ebert J.R., Smith A., Janes G. Gluteal tendon repair augmented with a synthetic ligament: Surgical technique and a case series. Hip Int. 2014;24:187–193. doi: 10.5301/hipint.5000093. [DOI] [PubMed] [Google Scholar]
- 21.Fisher D.A., Almand J.D., Watts M.R. Operative repair of bilateral spontaneous gluteus medius and minimus tendon ruptures. A case report. J Bone Joint Surg Am. 2007;89:1103–1107. doi: 10.2106/JBJS.F.01201. [DOI] [PubMed] [Google Scholar]
- 22.Fink B. Repair of chronic ruptures of the gluteus medius muscle using a nonresorbable patch. Oper Orthop Traumatol. 2012;24:23–29. doi: 10.1007/s00064-011-0073-3. [in German] [DOI] [PubMed] [Google Scholar]
- 23.Rao B.M., Kamal T.T., Vafaye J., Taylor L. Surgical repair of hip abductors. A new technique using Graft Jacket allograft acellular human dermal matrix. Int Orthop. 2012;36:2049–2053. doi: 10.1007/s00264-012-1630-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Voos J.E., Shindle M.K., Pruett A., Asnis P.D., Kelly B.T. Endoscopic repair of gluteus medius tendon tears of the hip. Am J Sports Med. 2009;37:743–747. doi: 10.1177/0363546508328412. [DOI] [PubMed] [Google Scholar]
- 25.Domb B.G., Botser I., Giordano B.D. Outcomes of endoscopic gluteus medius repair with minimum 2-year follow-up. Am J Sports Med. 2013;41:988–997. doi: 10.1177/0363546513481575. [DOI] [PubMed] [Google Scholar]
- 26.McCormick F., Alpaugh K., Nwachukwu B.U., Yanke A.B., Martin S.D. Endoscopic repair of full-thickness abductor tendon tears: Surgical technique and outcome at minimum of 1-year follow-up. Arthroscopy. 2013;29:1941–1947. doi: 10.1016/j.arthro.2013.08.024. [DOI] [PubMed] [Google Scholar]
- 27.Redmond J.M., Cregar W.M., Gupta A., Hammarstedt J.E., Martin T.J., Domb B.G. Trochanteric micropuncture: Treatment for gluteus medius tendinopathy. Arthrosc Tech. 2015;4:e87–e90. doi: 10.1016/j.eats.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The technique for gluteus medius tendon repair with a single-row construct is shown. A repair of a left hip gluteus medius tear, mostly through a midanterior viewing portal, is shown, except when otherwise noted.