Abstract
Health-related behaviors are among the most significant determinants of health and quality of life. Improving health behavior is an effective way to enhance health outcomes and mitigate the escalating challenges arising from an increasingly aging population and the proliferation of chronic diseases. Although it has been difficult to obtain lasting improvements in health behaviors on a wide scale, advances at the intersection of technology and behavioral science may provide the tools to address this challenge. In this paper, we describe a vision and an approach to improve health behavior interventions using the tools of behavioral informatics, an emerging transdisciplinary research domain based on system-theoretic principles in combination with behavioral science and information technology. The field of behavioral informatics has the potential to optimize interventions through monitoring, assessing, and modeling behavior in support of providing tailored and timely interventions. We describe the components of a closed-loop system for health interventions. These components range from fine grain sensor characterizations to individual-based models of behavior change. We provide an example of a research health coaching platform that incorporates a closed-loop intervention based on these multiscale models. Using this early prototype, we illustrate how the optimized and personalized methodology and technology can support self-management and remote care. We note that despite the existing examples of research projects and our platform, significant future research is required to convert this vision to full-scale implementations.
Index Terms: Behavioral informatics, computational models, health behavior change, multiscale, self-management, wearable sensors
I. Introduction
The rapidly increasing cost and limited effectiveness of healthcare is one of the most important societal and global challenges. These circumstances have been exacerbated by an aging “boomer” population and the increasing prevalence of chronic diseases in younger demographics [1], [2]. In addition, there is increasing recognition that lifestyle behaviors account for a substantial portion of premature mortality (more than 40%) [3]–[5] and are responsible for the majority of functional health and quality-of-life outcomes [6]. These observations would suggest the need to focus resources on improving health-related behaviors. Traditionally, health behaviors have been defined as actions taken by a person to maintain, attain, or regain good health and prevent illness. Lifestyle and health-related behaviors include physical activity, such as exercise, nutrition, alcohol consumption, sleeping, socialization, and smoking. These may be overt (motor or verbal) and directly measurable, or covert (activities not viewable, e.g., physiological responses) and indirectly measurable. In essence, behaviors are physical events that occur in the body and are controlled by the brain [7], [8].
Unfortunately, poor health behaviors and habits appear to be easily acquired but difficult to eliminate. Perhaps even more challenging is the fact that once developed, good habits and behaviors are difficult to maintain long term. One possible way to address these issues is through personal face-to-face coaching, but this approach is costly and difficult to scale. Alternatively, recent advances in sensor and communication technology, in combination with data and computational modeling, can play a pivotal role in transforming health behavior change interventions [9]. Concurrent developments in sensor and communication technology and data science have now enabled the unprecedented quantification of behaviors in “the wild”—in real life and in real time [9]. These two factors, in combination with progress in computational modeling, have paved the way for the nascent field of behavioral informatics. Behavioral informatics is a scientific and engineering area comprising behavior monitoring, assessment, computational modeling, inference, and intervention. This field is poised to advance a set of technologies and computational approaches to facilitate successful interventions that are scalable, cost effective, and timely.
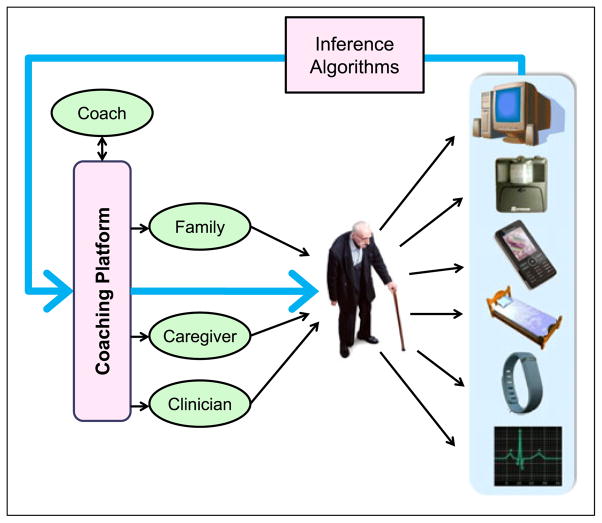
This paper describes an approach—currently in the evaluation stage—that provides an economically feasible method for helping people to improve and manage their health behaviors. The essence of this approach, shown in Fig. 1, is a coaching system composed of a number of components (or building blocks) that “closes the loop” between data acquisition and intervention. These components transform information from the physical world into data via a variety of sensors that can measure behaviors that are overt (motor or verbal) and directly measurable, or covert (activities that are not viewable, e.g., physiological responses) and indirectly measurable. The data collected are combined with subjective responses from the participants and processed by model-based assessment, predictive inference, and assessment algorithms that translate the data into useful information for a human coach, assisted by an artificial intelligence embedded into a coaching platform, in supporting individuals in improving health behaviors.
Fig. 1.
Individual sensors collect data from the home and environment. Inference algorithms generate estimates of behaviors, context, and important clinical states, which are used in health interventions. Tailored summaries and feedback are presented to the patient.
In this paper, we describe the structure of our prototype Health Coaching Platform and address aspects of the components necessary to supports its functions. One critical element to achieve this goal of closing the loop involves the development of multiscale computational models that capture aspects of behaviors at different scales, ranging from acquiring and processing raw sensor data, such as leg motion measurement or beat-to-beat heart rate (HR) monitoring, to quantify activities like eating, physical activity, and sleeping. These models provide predictions that generate prompts and cues to provoke and encourage behavior change in an optimal manner for each individual at the appropriate time. The combination of sensors with multiscale computational models allows us to observe and assess human behaviors unobtrusively, infer and predict individual health states and likely behaviors, and deliver optimal just-in-time interventions.
II. Closing the Loop With Intervention Protocols
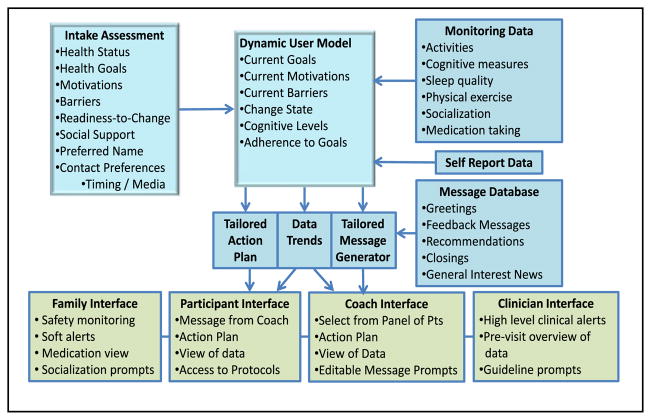
In healthcare and health psychology literature, there is considerable evidence that health interventions tailored to individuals are more effective than generic ones [10]–[12], and that timely feedback plays an important role in changing and sustaining behavior [13]. Coaching interventions that incorporate data from new sensor technologies and new methods for real-time communication with patients have the capability of enhancing the tailoring and timeliness of coaching feedback and encouragement. Computational models that provide an assessment of patient state, activities, and context (such as location or previous activities) can make health behavior interventions both more effective and scalable. As an example, our work on health coaching interventions for older adults in the home [14] uses a Health Coaching Platform with a data flow illustrated in Fig. 2. The blue boxes at the top of the diagram show how data from the initial interview, combined with monitoring data, builds and updates a dynamic user model which in turn determines the coaching actions. Based on this data flow, our work has explored methods for delivering tailored coaching using state-dependent active methods triggered by sensor data feedback and user input. This dynamic user model includes health behavior change variables, such as motivations, barriers, and readiness-to-change [15]. Fig. 2 illustrates that the inputs to the dynamic user model (both initial assessments and updates based on inferences from the sensor data) are used to select phrases from the message database for generating alerts and tailored coaching messages.
Fig. 2.
Framework for Northeastern University’s Health Coaching Platform includes a dynamic user model based on initial assessments and updated with sensor data. This user model drives the semiautomated tailored messaging for the health interventions.
The dynamic user model represents the current state of the patient and drives the semiautomated tailored messaging for the health interventions, as displayed in tailored interfaces for each stakeholder. This system was designed to facilitate a health coach, trained in health behavior change, in reaching a large panel of older adult participants in their home environment. The Health Coaching Platform includes modules for cognitive exercise [14], [16], physical exercise [17], sleep management [14], [18], medication management [19], and socialization [20].
As an additional source of information about a patient, coaching protocols that take advantage of the rapid uptake of new mobile communications technologies have given rise to techniques for ecological momentary assessment (EMA) [21]–[24] and just-in-time adaptive intervention (JITAI) [25]. Sensor feedback (usually from wearables or the user’s smart phone) can be used to trigger a quick assessment (EMA) or coaching message (JITAI) that is timely as well as context and location appropriate. In addition to being effective, these approaches are more scalable than traditional health behavior interventions [26].
To realize this goal, it is necessary to develop ways to monitor physical and physiological aspects of behaviors, convert the raw data into behavioral inferences, and then generate behavioral interventions. We demonstrate that this can be accomplished with a sequence of building blocks aided by computational models at each stage. Accordingly, there are three key areas that cover the different types of models needed to optimize the intervention.
Data science addressing acquisition of raw data.
Actions and activity recognition from raw data.
Models of health behavior change.
Although we have developed a Health Coaching Platform based on these principles with the previously described building blocks and subjected it to initial evaluation [14], [17], [19], [20], [27], [28], there are many remaining challenges that arise in the process of applying this approach to specific domains. The subsequent sections of this paper describe relevant aspects of data science followed by a multiscale modeling approach with examples converting raw data to usable knowledge enabling inferences and predictions. We then describe early approaches to computational modeling of behavior change—the most challenging and least developed area to date. Although we cover a number of existing realizations, we have also noted challenges that still need to be addressed where appropriate.
III. DATA SCIENCE IN SUPPORT OF BEHAVIOR MONITORING
Data quality assurance is critical in any sensing application, but particularly when using minimally obtrusive or unobtrusive heterogeneous sensors and data types. In fact, in behavioral informatics, the notion of a “sensor” needs to be interpreted broadly in that a sensor or sensor stream may represent any source of raw data related to behaviors as illustrated by the examples in Table I. This table lists a small subset of sensors that have been used in a variety of studies and applications in behavioral informatics. There are numerous examples where the understanding of underlying processes is necessary in order to assess and improve the generalizability of the analyzed results ranging from physical activities [29] to searching the Internet [30].
TABLE I.
Sample of Data Sources (E—Environment, M—Mobile, O—Other)
| Sensor | Phenomena | Type |
|---|---|---|
| PIR | Movement of a person | E |
| Contact Switches | Open/close doors | E |
| Bed sensors | Movements, HR, respiration | E |
| 3-D Cameras (Kinect) | Image & depth | E |
| Accelerometers | Physical activity | M |
| Gyroscopes | Orientation, gestures | M |
| Computer/keyboard | User interactions | E, M |
| RFID | Proximity to objects | E, M |
| Environmental sensors | Temperature, light, noise, etc. | E, M |
| Electrodes, optical sensor | HR | M |
| Mobile phone usage log, calendar | Social interactions, stress, | M |
| Credit card log | Diet, other behaviors | O |
| Questionnaires | Any behaviors and affective states | O |
Oftentimes, the context affecting the collected data is unknown and must be estimated; thus, limiting the interpretability of the observations. For example, in addition to subject-dependent variability, the data may be affected by location and environmental factors, resulting in apparent outliers. It might be necessary to have adaptive filtering or sampling based on the task or context (e.g., location, background activity). In our previous work, we have found that outlier measurements and missing data may frequently require understanding of the specific circumstances [31]. When monitoring health behaviors, missing data are often missing not at random, but rather are correlated with the activity or the state of the monitored individual. For example, patients may stop weighing themselves when they have been consuming high calorie foods or eating more than normal, yet be more likely to weigh themselves when adhering to their dietary goals. Knowledge and modeling of this bias is important when inferring the intervening weight measurements in a coaching intervention.
An additional process limiting data utility to be addressed by data science approaches is the censoring of data, where due to the measurement methodology, the value or observation is only partially known. Censoring may arise from a subject’s early withdrawal from a study or from limitations of a sensor or assessment instrument. For example, a sensor’s limited dynamic range or limits of response scales on questionnaires could censor the acquired data. Quite often, it is apparent that subjects “top out” or “bottom out” on assessment scales used in clinical trials. To mitigate these problems, we advocate improving the dynamic range of both sensors and clinical assessments and model the distortions due to these limits. For example, clinical assessments are improved by anchoring the scales, i.e., providing examples of minimum and maximum limits, and by modeling subjects’ ratings using scaling techniques such as the Item Response Theory [32]. In case of physical sensors, the effects of these aberrations can be reduced by modeling the distortions.
A useful approach to mitigate a variety of data issues is to combine data from multiple sensors, deploying a variety of fusion techniques. A specific example is the inference of smoking behavior from accelerometers and pulmonary plethysmography [33], [34]. Although there has been significant progress in a number of specific areas, there is a need for further research to address general context-dependent sensing.
IV. MODELS OF SENSING AND ACTIVITY RECOGNTION
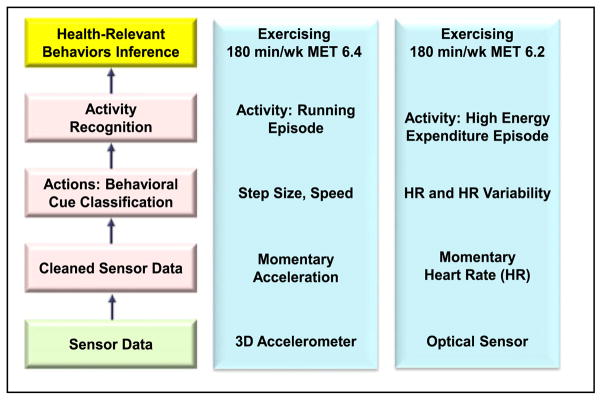
Considering the goal of optimizing JITAI as a control-theoretic problem, it is necessary to assess and predict behaviors continuously or at least sufficiently frequently. This requires continuous application of behavioral informatics, including sensing, assessment, and inference of behaviors. Since raw sensor data can typically only measure fine grain physical phenomena, it is necessary to make inferences about behaviors with computational multiscale models as illustrated in Fig. 3. Raw sensor data provide fine grain information about physical phenomena, such as instantaneous acceleration, that may need to be converted to elementary movements and actions that may in turn provide information about the activity and health-related behaviors, such as exercising. In the remainder of this section, we will describe the different building blocks for converting data to estimates of activity and patient states.
Fig. 3.
Example of a multiscale model used for an inference of exercising behaviors from two different sensors—accelerometers and an optical HR monitoring device.
Prior to the description of the multiscale modeling details, we note that the continuous monitoring of behaviors and physiological phenomena has the potential of revolutionizing not only behavioral interventions but also clinical assessments and therapy by providing information about subtle changes, trends, and variability assessments within individuals.
Diverse sensors and their resulting data streams represent the first stage in the quantification of behaviors. For example, a participant’s responses to questions, observations of caregivers, or clinicians as noted in the electronic health record, a participant’s telephone use history, purchasing history, or similar sources of behavior related data may all provide information used in computational models to estimate activities or patient state. These additional types of assessments can now be made more frequently using mobile phones for EMA [23], [24], where patient self report, such as aspects of health or psychological states that are not yet amenable to unobtrusive sensing, provide important inputs to a health behavior change model.
A. Models of Data Streams
The first step in the assessment of behaviors includes a transformation from raw sensor data to useful information. What makes this task particularly challenging is the need to quantify behaviors in real life and in natural environments with data acquisition methodologies that are as unobtrusive as possible. Our own work, as well as that of other researchers, suggests that any methodology that requires the participants to wear, operate, and maintain devices solely for monitoring can only be sustained for limited periods of time [35], [36]. To overcome this limitation, sensors need to be unobtrusively embedded in the environment or in devices used for other purposes, such as mobile telephones. Alternatively, they may be nested in motivating systems like step counting devices or safety alarms [37]. As a result of the unobtrusive nature of sensing, the data usually represent only surrogate markers of the phenomenon of interest, e.g., acceleration rather than energy expenditure. Consequently, raw data are subject to distortions, contamination with noise, and significant effects of the context of the measurement. Although these undesirable influences are common with almost any biomedical measurement, it is particularly significant in unobtrusive assessment of behaviors. For example, the assessment of older adults’ ability to perform activities of daily living (exercising, making a meal, taking a bath, getting dressed, etc.) must be inferred from an imperfect sensing of location, device interaction, and acceleration data. An effective way to mitigate these challenges is to develop computational models of sensors, which provide transformations from raw sensor data and actions, while incorporating context as much as possible. This usually involves a strategy of combining information from multiple sensors.
B. Computational Models of Sensors
Sensing can be interpreted as a measurement process that associates numerical elements to attributes of a class of objects or events. We formalize a measurement process as a transformation H that maps health and behavior-related events, objects, or states ψ̂ ∈ Ψ to elements in a numerical set Y [38]. The map H assigns a numerical value to aspects of events or actions, y (t) = H [ψ] (t). For example, using an accelerometer attached to the waist of an individual, the transformation H converts acceleration during walking or riding a car to sampled acceleration contaminated by the noise. It is also essential to recognize that a sensor transformation frequently depends on the context of the observation, namely y = H [ψ; C], where the vector C represents the context of the observation, with context defined as the set of environmental and situational aspects that affect the interpretation of the primary measurements and observations [39], [40]. For example, in the case of the accelerometry, it is important to distinguish data collected during running from those collected while riding in a car over rough but periodic terrain. Similarly, observing changes in HR and HR variability (HRV) to assess the rate of energy expenditure (power), the context may involve an activity such as running in contrast to watching an exciting film.
Although sensing the torso acceleration, the purpose of these measurements is to infer aspects of the actions and activities ψ. If H were known, invertible and noiseless, we could estimate the features of the actions by inverting the transformation H, namely ψ̂ = H−1 [y;C]. In most practical situations, however, H is unknown and must be approximated; in every case, it is important to incorporate as much as possible principled information about the transformation. In the case of accelerometry, energy expenditure is governed by Newton’s laws, combined with the effects of the location of the sensor. In many situations, the fundamental principles are difficult to incorporate, and the transformation is estimated using data-driven approaches. Even in these situations, it is useful to make assumptions that constrain the transformation. For example, if H can be approximated by a linear system and the uncertainties by Gaussian random variables, we could use the Kalman filter approach, or its various extensions, for state estimation. In general, knowledge of H or its approximations is useful in improving the estimates of the states that are not directly observable.
A simple example of a model-based approach involves the measurement of walking speed using passive infrared (PIR) motion sensors mounted on the ceiling of a hallway [41]. Each sensor event (firing) is an indication that a person is passing through its field of view; from these firing times, it is possible to estimate the speed of walking. However, Hagler et al.’s study [41] showed that even though the sensors were stationary, it was necessary to model each sensor’s errors in both time and space in order to obtain unbiased estimates of the speed of walking [41]. Thus, each firing of a PIR detector needed to be represented by a pair (xi − εx , ti − εt ), where xi is the location, ti is the time of the firing event of the ith sensor, and εx , εt are random variables representing the uncertainty associated with the corresponding dimensions. The reason for this type of representation is that the temporal uncertainty representation alone was not sufficient to account for the variability in the thermal signal generated by a moving human body, which depends on variables like body temperature and amount of clothing. As this example suggests, principle-based modeling of sensed data does not only involve the sensor processes but also aspects of the observed system, in this case, the participant’s actions.
Another example involves the assessment of sleep using a variety of force transducers and motion detectors. This approach involves strain gauge force sensors (load cells) installed at the four corners of a rectangular bed [42], [43]. This sensor setup can be used to infer movements in the bed, breathing, and even heartbeat. A biomechanical model of a breathing human was used to interpret the changes in the forces at the bed corners.
Perhaps the most information-rich sensors involve continuous video data streams (see the review by Aggarwal and Ryoo [44]) that covers a variety of the issues, including approaches to activity classification discussed in the next section. Although a video-based assessment raises concerns of privacy, these can frequently be alleviated by converting images to a greatly reduced numerical representation, eliminating the possibility of recovering the original images.
Although many implemented approaches to the interpretation of the sensor data exist, there are remaining challenges that need to be addressed. These include unobtrusive and adaptive calibration, sensor placement, and context invariance.
C. Modeling and Recognition of Activities
The ability to recognize people’s activities (exercising, gardening, etc.) is one of the pillars of behavior informatics, with applications ranging from healthcare to designing robots that interact with people. For behavior change interventions, knowledge of activities throughout the day provides useful information for generating optimal intervention strategies. In the case of caring for older adults, this information enables assistance when needed in their daily living activities [45]. Activity recognition also includes the detection of anomalies and adverse events, such as falls or deviant behaviors in security and surveillance applications.
In the most general terms, the problem of activity recognition amounts to inference of human dynamics typically involving movements or interactions with objects or other humans. Ideally, the inference problem involves classification of activities from estimates of movements and actions obtained from sensors as discussed in the previous section.
Although the framework for activity recognition is similar to that for sensor transformation, the domain of activity recognition is more general, involving estimation and classification based on the sensor inferences. Most of the approaches involve data-driven methods in combination with state transition models, context-free stochastic grammar, and space-time trajectories, although there have been approaches that incorporate “stick figure modeling” [46]–[48] which also incorporates biomechanical principles. Recent advances in 3-D image capture enable effective model-based inferences. These have been used to assess gait parameters and exercise performance [49]–[52]. One useful example deploys hybrid models of gait that combine continuous dynamical systems with discrete phase switching [50]. This biomechanical model has been particularly useful in the interactive exercise interventions and coaching intervention for older adults using the Microsoft Kinect camera [17].
Despite the advantages of video-based activity assessment, many existing studies monitoring older adults have used PIR motion detectors for activity monitoring and recognition because of cost, power, and privacy issues. The data from these sensors are sequences of firing events represented by sequences of pairs S = {(s1 , t1 ) , (s2 , t2 ) , . . . , (sn , tn )}, where si , ti represent the sensor identity and the time of firing, respectively. The goal of the inference process is to assign labels to the elements of S. This activity recognition processes must simultaneously determine the boundaries between activities (segmentation) and classifications. This is generally accomplished using a variety of modeling techniques for supervised and unsupervised training of clustering and recognition algorithms. As such, researchers attempted to use hidden Markov models (HMM). Using this type of approaches yielded reasonable activity recognition rates, ranging from 0.60 to 0.80 [53], [54]. These approaches, based on stationary sensors, can be complemented by mobile or wearable devices, especially when the monitored individuals are outside their homes [23], [55], [56].
Notwithstanding the advances in activity recognition, there are many remaining challenges. One of the major barriers to using existing approaches like machine learning for activity classification is the difficulty in obtaining labeled data. Another problem is testing the fundamental properties of activity models. For example, the Markov property is rarely tested, and when it is, rarely supported by the data.
D. Model-Based State Estimation From Physiological Sensors
There are a variety of wearable sensors for collecting physiological measurements in the home, workplace, or general environment. These include sensors that measure blood glucose, blood pressure, electrodermal activity, oxygen saturation, airway peak flows, and HR. Today, wearable sensors allow continuous long term beat-to-beat monitoring of HR and HRV, either based on electrocardiography or photoplethysmography. As an example of inferring patient state from physiological measures, we will consider HR and HRV to estimate patient stress and stress recovery. HR and HRV vary remarkably depending on physical activity, stress, and health, making HR and HRV interpretation complex. However, when combined with physiological and computational multiscale models, HRV may provide rich information about several health behaviors.
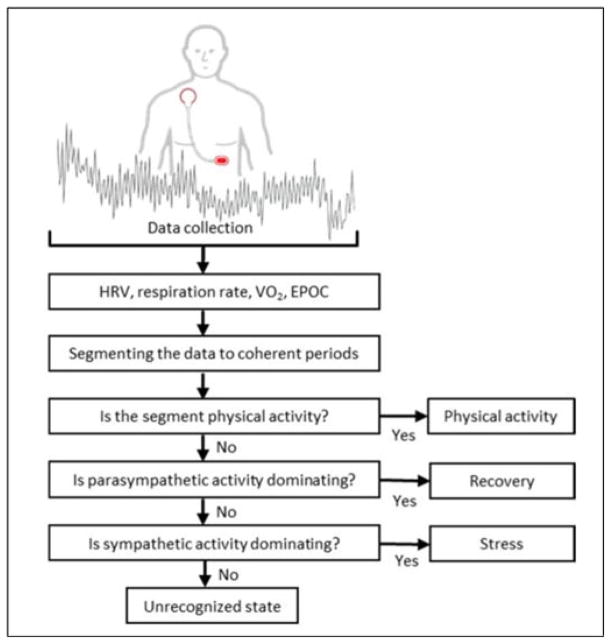
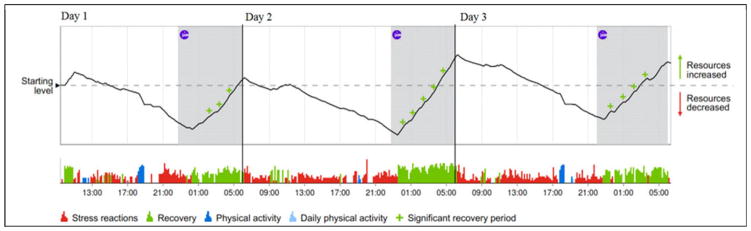
HR monitoring allows the assessment of the intensity of physical activity, as HR is almost linearly associated with oxygen consumption (VO2) at moderate to submaximal intensities in steady-state exercise [57]. However, the intensity of real-life physical activity usually changes repeatedly, and the relationship between HR and VO2 is curvilinear for very low-intensity physical activities and near-maximal exercise. A model based on HRV, age, gender, weight, height, and self-reported physical activity class was recently shown to provide accurate estimates of the intensity of the physical activity during real-life conditions [58]. Hence, HRV monitoring allows reliable continuous assessment of physical activity, exercising, and energy expenditure in real-life conditions. HRV is associated with functioning of the autonomous nervous system and, hence, is modified by stress and relaxation, physical activity, and health status [59]. However, HRV has high inter- and intraindividual variability, which complicates the interpretation and the use of HRV as a measure of stress. With a multiscale model-based approach, it is possible to transform the HRV signal into a quantification of an individual’s stress and recovery during daily life (see Fig. 4) [60], [61]. The HRV signal is first analyzed using a sliding window approach to quantify HRV, detect respiration rate (based on respiratory sinus arrhythmia), and estimate momentary oxygen consumption (VO2) and excess postexercise oxygen consumption [58]. This modeling step transforms raw sensor data into physiologically relevant parameters. The next step applies adaptive segmentation to divide the data into stationary and transient segments, which are further classified based on their physiological parameter values into the physiological states of physical activity, physiological recovery, stress, and other. This step transforms moment-by-moment physiological parameter vector data into physiologically and behaviorally meaningful states. Finally, the classified state data may be transformed to a more holistic representation of the individual’s physiological and behavioral status over the entire monitoring period, providing total energy expenditure, total amount of physical activity and exercise, and stress and recovery balance (see Fig. 5).
Fig. 4.
Model-based state classification based on beat-to-beat HR signal analysis.
Fig. 5.
Example of physiological and behavioral state classification based on a multiscale model of HRV. The line above describes cumulative autonomic nervous system stress and recovery index from 0 (stressed) to 100 (fully recovered). The lower graph shows minute-to-minute state classification (green—physiological recovery; red—physiological stress responses; blue—physical exercise; white—other state/nonclassified). Height of the bars represent strength of the physiological reaction (Source: Firstbeat Technologies, Jyväskylä, Finland).
V. Models of Behavior Change
The task of optimizing interventions can be interpreted as a control theory problem, where differences between observed behaviors and desired behaviors are used to generate the most effective input (intervention), as outlined in Fig. 1. An effective utilization of the control-theoretic framework, however, requires a quantitative characterization of the psychological state and corresponding dynamics as a function of time for each individual participant.
The characterization of health behaviors dynamics, as well as their change, requires multiple time scales. For example, the decision of whether or not to engage in a particular physical activity or consume a healthy snack occurs on a scale of seconds or minutes, but changing one’s lifestyle to accommodate regular visits to the gym may take days or weeks.
The multiscale dynamics must be reflected in monitoring and inference as well as in generation of interventions. For example, activity recognition may derive moment-to-moment information about an individual’s physical activity, exercise, and sleep, which may eventually accumulate into the quantification of behavioral patterns as compared to target behaviors, as illustrated in Fig. 3. Interventions, such as reminders, suggestions, and recommendations (e.g., for physical exercise or avoidance of unhealthy foods), might be most effective as a JITAI.
In contrast to the momentary interventions, recommendations for lifestyle changes influencing physical activity and exercise may deliver information about the target quantities on a daily or weekly level, and these targets should be dynamically adjusted to account for potential other factors such as acute illnesses. To optimize interventions, therefore, we need multiscale inference, modeling, and prediction of behaviors, which in turn requires a computational framework for behavior and behavior change.
A theoretical framework useful for predictive modeling in many domains is based on system theory, exploiting a state-space representation. A typical dynamical system is defined in terms of a state space Q (t) ∈ Ψ, an output vector V (t), and input vector A (t). To represent a behaving human, the inputs may include environmental, contextual, and social stimuli, as well as coaching events. The output vector comprises actions, as described above and shown in Fig. 3, that may include limb movements, speech acts, classified activities, or even responses to questionnaires (EMAs). Both inputs and outputs are typically random variables.
Although the system dynamics may be continuous, we assume that all the components are sampled at discrete times described by a sequence Tn = {t1 , t2 , . . . , tn } , and the sequences of unobservable states, coaching inputs, and measurable variables are given by Q (Tn ) , A (Tn ) , V (Tn ), respectively. To make predictions, we need to represent the state transition dynamics Q (tn + 1 ) = G [Q (Tn ) , A (Tn )] and the observation random sequences given by V (tn ) = R [Q (Tn )] .
Ideally, the state space and the state transition processes would be determined by psychological, empirical, and theoretical research. Unfortunately, with very few exceptions, most psychological theories of behaviors and behavior change have not been specified to characterize the dynamics at the different time scales to enable continuous quantitative assessment and predictions for individuals needed for the generation of optimal interventions. In the following sections, we present recent attempts to address this issue.
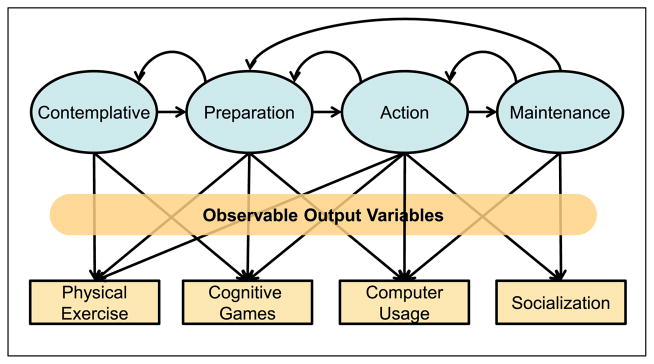
A. Discrete State-Space Representation
One starting point for this type of development was the Trans-theoretical Model (TTM) of Behavior Change [62]–[64] postulating discrete states for “readiness to change.” For example, in the TTM, a participant is assumed to progress through a small number of “readiness-of-change” states: precontemplation, contemplation, preparation, action, maintenance, and possibly termination [62].
Although as originally specified, the TTM has a number of issues [65], including limited predictive power, it can be reformulated in terms of a discrete state transition model as shown in Fig. 6. Adding several assumptions, some researchers proposed to characterize the behavior change process in terms of a hidden (latent) HMM [66]–[68]. Markov models [69], [70], and, in particular, HMM, have been effectively applied in many disciplines, ranging from learning theories [71], [72] in psychology and bioinformatics to automatic speech and image recognition in engineering, and have very well-developed techniques for training and inference (e.g., see Rabiner [73]). Although HMM-based approaches are intuitively appealing for the characterization of behavior change [74], they are based on a number of strong but questionable assumptions, such as the Markov property and its consequence—the exponential dwell time distribution. The Markov property may not hold because the prior participant’s history may change the probability of transitions. For example, the probability of a transition from the Preparation to the Action state may depend on whether the participant has previously been in the Action state or has arrived there from the Contemplation state. Similar issues arise when considering whether the dwell (time spent) in a given state of the Markov model is exponentially distributed; it is more likely that a participant would need some minimum time to spend in a given state before transitioning to the next state. An additional issue with using discrete state Markov models (see Fig. 6) relates to the fact that any intervention, such as coaching, would affect the transition probabilities and preclude the use of many computational tools for training and inference.
Fig. 6.
Example of a HMM for the TTM of behavior change. Only a subset of the states and transitions and output transformations are shown.
The discrete state Markov transition model could be modified to mitigate some of these issues, but its increased complexity would compromise its predictive power. For example, we could use a hidden semiMarkov model (HSMM) [70], [75] that can incorporate arbitrary dwell distributions. As a result of this generalization, the typical training of the HSMM is significantly more complex than the standard HMM. Incorporating the coaching effect would require modification of the transition probabilities that would likely reduce the predictive power of the discrete state Markov model.
B. Linear Dynamical System Representation
Rivera et al. developed a structural equation model (SEM) of health behavior change using linear dynamical control systems [15], [76]. The model is based on the psychological theory of planned behavior [77] that links perceived behavioral control, subjective norm, and attitude toward behaviors to the actual behaviors.
The linear dynamical system approach has been motivated by structural equations modeling [78] of the theory of planned behavior [77] that generated parameter estimates using population statistics and is itself based on the assumption of linear relationships and Gaussian distribution of errors. Although the SEM represents a static asymptotic state of the system, Rivera et al., explored the generalization of SEM to a dynamical system, assuming that the SEM parameters can be used as the coefficients of the differential equations representing the corresponding deterministic linear system [79].
Although this approach may eventually prove effective, it has currently a number of limitations. In particular, the present model has a large number of degrees of freedom (parameters), so the complexity of the system may approach, or even exceed, the degree of freedom in the data. As in the considerations of HMM, strong assumptions, e.g., linearity, need to be tested in order for this system to be used as an engine underlying interventions. We anticipate that a modified version of such a system, combined with certain nonlinear components, may be a potentially effective representation.
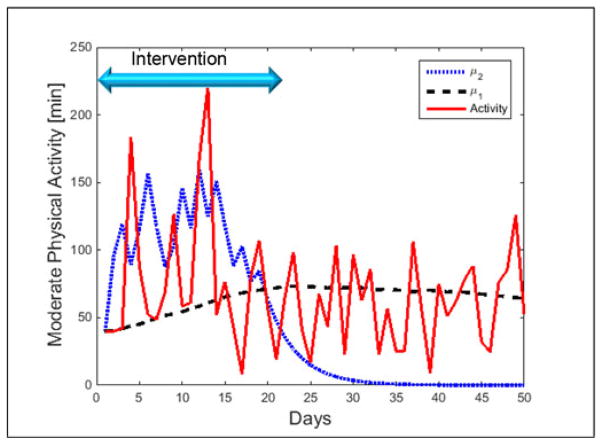
C. Dual-Process Representation
During the last couple of decades, behavioral researchers began considering a different class of models based on the dual-process theory [80], [81]. There is substantial evidence that human decisions are based on a combination of responses from two concurrent systems. Type 1 represents an automatic process, generating habitual responses/behaviors that are executed rapidly without conscious elaborations. A Type 2 process, such as cognitive decision making, is based on explicit problem-solving, and, therefore, slower than the Type 1 system. Thus, in cases where the systems compete, the faster Type 1 system may frequently “win,” and we take action based on our habitual response before we can apply reasoning. Because the habits that correspond to unhealthy responses are generally more prevalent, the Type 1 system’s short-term domination results in making poor health behavior choices unless we modify these habitual responses.
Another important difference between the two systems is the speed of learning. A change in automatic habitual responses of the Type 1 system occurs over a long time, requires a large number of trials, and extinguishes slowly [82]. The reasoning Type 2 system can learn rapidly through information, persuasion, and motivation, but can forget just as quickly.
A modeling approach based on the dual-process theory has a number of advantages in comparison to the two models described in previous sections. The computational modeling can take advantage of existing research in psychology on decision making and learning and may, therefore, be able to predict responses to stimuli in a variety of contexts. As such, it can incorporate mobile EMA and even trigger EMAs.
To provide an intuitive insight, we assume that each system responds concurrently to a stimulus, such as the logo of a fast food establishment. The system that responds faster will govern the response generation. In order for a participant to make a healthier choice, it is necessary to either train the Type 1 system to develop healthier habits or to coach the Type 2 system to anticipate and preempt the habitual responses.
To illustrate the ability of this model to reproduce the general characteristics of experimental data, we simulated the results of recently published experimental data from a study by Spring et al. [83] that was designed to examine the dynamics of an intervention to increase the duration of the participants’ physical activity per day. Each of the two types of systems was represented by a random variable that controlled each participant’s decision process regarding the activity level. A sample of simulation results based on this data is shown in Fig. 7. The red solid line represents the average daily activity in minutes, the black dashed line represents the Type 1 system, and the blue dotted line represents the Type 2 system. During the intervention, the Type 2 process quickly learns to adhere to the coach’s guidance, but it forgets to respond properly after the intervention is over. During the same time, the Type 1 process expertise is learning slowly, but takes over after the coaching ceases. This model can then be used to directly predict individual participants’ activity level as a function of time. The missing important ingredient of this model is how to quantify the coaches’ interventions to be able to predict the effect of these interventions and suggest the optimal ones.
Fig. 7.
Dynamics of a participant’s responses to coaching for increasing daily physical activity. Simulated data from Spring et al. [83].
VI. Integrating Monitoring and Modeling for Coaching Interventions
Our most recent evaluations of the Health Coaching Platform have tested the integration of data from sensors in the home: computational models that infer patient state, context, and adherence to goals; and intervention protocols to promote health behavior change. For our intervention protocols on cognitive training, sleep management, socialization, and physical exercise, we first use an in-home visit or Skype conferencing to assess current activity levels, health behavior goal selection, readiness to change, motivations, and barriers (when appropriate). For example, with our sleep intervention, we assessed sleep hygiene issues, anxiety, and circadian rhythm patterns before recommending changes to the environment or relaxation exercises. A tailored action plan was created and updated each week. A total of 33 elderly participants (average age 80.3 ± 9.4 years) have now been coached over a period of two years, with substudies on medication management [19], [84], socialization [20], and interactive video exercise using the Kinect camera [17].
As an example of monitoring various types of data from the home and providing feedback for a tailored health intervention, our socialization module for older adults in the home focuses on several proxy measures for inferring degree of socialization: time and contacts on email, time and contacts on the phone, time and contacts on Skype (all older participants and an enrolled remote family member use SkypeTM), and inferred time out of the home. To assess a baseline degree of socialization at the beginning of an intervention, we use the Ludden social network scale-revised [85] and the UCLA-R loneliness scale [85]. For coaching purposes, we also use motivational interviewing to assess motivations, barriers, and readiness-to-change for each selected activity. Table II shows our Level 1 selection of socialization activities for an older adult participant’s weekly action plan. The feedback and recording of their participation in the intervention is based on computer, phone, or motion sensor data from the home or self-report for the in-person activities.
TABLE II.
Activity Selections for the Level 1 Phase of the Socialization Coaching Intervention
| Technology | Activity | Freq |
|---|---|---|
| Computer | Make a Skype call to family member, friend, study participant, or coach | 1–3/wk |
| Computer | Participate in group Skype call | 1/wk |
| Computer | Send email to family member, friend, study participant, or coach | 1–3/wk |
| Computer | Participate in online support group or chat | 1/wk |
| Computer | Play online card or board game with others | 1/wk |
| Computer | Use Facebook—new interaction | 1/wk |
| Phone | Make a phone call to family member, friend, study participant, or coach | 1–3/wk |
| In Person | Visit with family or friends | 1–2/wk |
| In Person | Play a board or card game with someone | 1/wk |
| In Person | Participate in a community event | 1/wk |
| In Person | Participate in a volunteer activity | 1/wk |
| In Person | Walk in a public place (mall, park) for at least10 min | 1/wk |
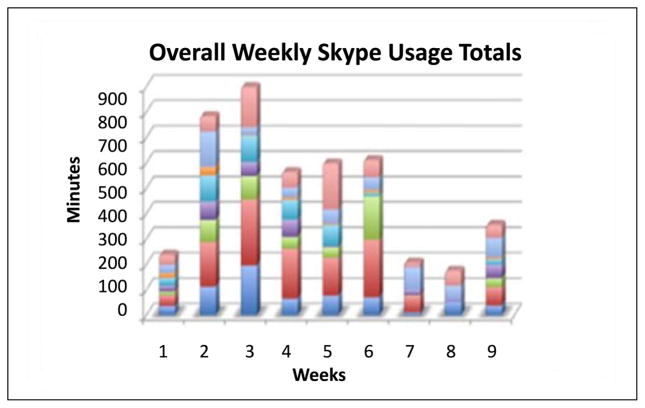
With the subset of our coaching participants that chose a socialization intervention (nine participants, 73.8 ± 6.7 years, 89% female), we found that we were able to maintain adherence to their selected socialization activities over a period of nine weeks. At baseline, only two-third of our participants was completely satisfied with their level of socialization. Our goal was to be able to provide a socialization intervention using Skype that could improve their social network and time interacting with people. Fig. 8 shows a graph of their overall Skype usage in minutes for each week of the intervention. Although the usage dropped off somewhat as time went on, most participants used Skype at least 1 h/week, communicating with an average of five people during the intervention. All participants studied improved their level of socialization and continued to see a benefit in the maintenance phase of coaching (after the nine weeks) from using Skype to communicate with remote family members and friends.
Fig. 8.
Weekly overall Skype usage (in minutes) by participants in the Socialization Intervention. The colors represent different participants.
One of the challenges demonstrated by this example lies in keeping adherence and motivation high throughout a lifestyle intervention. Coaching protocols must adapt to an individual’s change of state into a maintenance phase. Maintaining health behaviors is often harder to accomplish than a short-term change. One of our approaches has been to offer a menu of weekly activities for variety and challenge, as well as multiple intervention topics. The integration of estimates of patient state, context, and adherence to goals provides a valuable framework for providing tailored, timely, and potentially scalable health behavior change interventions.
VII. Limitations and Future Challenges
We have demonstrated the ability to integrate data science with models of sensors, activity, context, and behavior change into a coherent health coaching platform and deliver interventions in a way that keeps participants motivated and engaged. However, there are still many issues needing further attention. With special populations, such as older adults, ease-of-use and meaningfulness of messaging remains a top priority. Expanding use to minority and underserved populations will also need testing and design input. We currently have limited approaches to modeling privacy and data sharing preferences. The informed sharing of sensitive data requires insight that new participants often lack. We need to be able to estimate preferences, and do our best to share summarized data in a useful but privacy preserving manner.
At the outset, we described a vision of behavioral informatics in which unobtrusive sources of information are used to monitor, assess, infer, and intervene to help people improve and manage their behaviors, consequently improving their health and quality of life. Despite the advances in sensor technology, data science, computational modeling, inference, intervention optimization, and machine-assisted coaching platforms, there are many remaining challenges that need to be surmounted to implement this vision.
One of the outstanding problems stems from the variability across and within individuals in their health behaviors. Developing generalizable behavior inference algorithms that would not require a new training set for each new individual is inherently difficult. Although there have been some successes, there is a need to improve training approaches that would generalize across and within individuals without having a “ground truth.” Behaviors related to activity (exercising, sleeping, physical activity) are relatively observable and measurable by current sensor technologies; the challenges in using these sensors in long-term monitoring include technical concerns (such as battery life, user acceptance, and adherence to monitoring) and inter- and intraindividual variability of the behavioral patterns.
Several important health behaviors are still difficult to observe and quantify objectively and unobtrusively. These include diet, nutrition, and energy intake. Assessment of social and emotional aspects of behavior would also benefit from improved inference and assessment techniques.
Another important issue is false alarm fatigue. The generation of false alarms is a serious problem for behavioral informatics because of the continuous monitoring of low probability events. Under continuous or frequent monitoring, even well-performing detectors will likely generate a high proportion of false alarms. Consider, for example, a fall detector with sensitivity and specificity at 99%. For most detection tasks, this level of performance would be considered very good. However, since the prior probability of a fall in each hour is extremely low (<0.01), continuous monitoring may identify thousands of accelerometer or movement events to classify per hour; in this situation, a 99% specificity detector would generate about ten false alarms per hour. Despite the detector performance, false alarm fatigue needs to be addressed before these systems can be routinely used. One intriguing approach to mitigating this problem is to incorporate the utility of detecting an important event like a fall versus the disutility of a false alarm in the decision process.
A closely related issue is the cost-benefit tradeoff of an intervention and participant adherence. This is intimately tied to the problem of discounting future benefits relative to an immediate cost. For example, if a coaching intervention is not perceived to have immediate benefits, the participating individual may not adhere to the shared goals and activities agreed to with the coach. The challenge of preventive healthcare, in general, is to increase the value of future benefits and convert them to more immediate gains.
VIII. Conclusion
Future work in this area will generate a set of tools and methods that will help improve the well being of all, including older adults, underserved populations, and those residing in rural areas and is likely to have a significant societal impact. The proposed computational modeling-based approach to the assessment of behavioral, physical, cognitive, and affective states is expected to revolutionize healthcare delivery, including the provision of effective, timely, and targeted interventions. Further, the social benefits of behavioral informatics extend beyond healthcare, ranging from impacts in engineering disciplines, such as robotics, automation, and surveillance, to broad areas of education, economics, and scientific thrusts such as U.S. President Barack Obama’s Brain Initiative (connecting brain and behaviors). Additionally, work in this new area of behavioral informatics will inspire a new generation of students, who will be able to address problems at the intersection of computer science, engineering, and behavioral and social sciences.
The main tenant of this paper is the notion that multiscale computational models ranging from sensors to behavioral decisions is an important prerequisite for optimizing interventions aiding individuals in learning and adhering to better health behaviors. In conclusion, we would like to note that this paper only begins to scratch the surface of the problem of helping people to improve their health behaviors. Significant efforts in areas, such as sensor development, modeling, algorithm design, and clinical evaluations, are needed to address the complex issues in improving health behaviors.
Acknowledgments
This work was supported in part by the U.S. National Science Foundation under Grant 1111965, Grant 1407928, Tekes; FiDiPro, National Institutes of Nursing Research Grant P20NR015320.
The authors would like to thank S. Hagler, D. Austin, J. Kaye, T. Hayes, and many other colleagues at the Oregon Health and Science University and the Tampere University of Technology in Finland for contributions to this paper. They would also like to thank D. Spruijz-Metz and W. Nilsen for valuable discussions, and M. Wang and K. Nikita for shepherding this paper through the preparation process.
Biographies
Misha Pavel (S’67-M’75-LSM’11) received the Ph.D. degree in experimental psychology from New York University, New York, NY, USA, the M.S. degree in electrical engineering from Stanford University, Stanford, CA, USA, and the B.S. degree in electrical engineering from the Polytechnic Institute of Brooklyn, Brooklyn, New York.
He is currently a Professor of Practice jointly appointed between the College of Computer and Information Sciences and the Bouve College of Health Sciences at Northeastern University, Boston, MA, USA. He is also a Visiting Professor at the Technical University of Tampere, Tampere, Finland. He was the Chair of the Department of Biomedical Engineering (he founded in 2001) and as the Director of the Point of Care Laboratory, which focuses on unobtrusive monitoring, neurobehavioral assessment, and computational modeling in support of healthcare, with a particular focus on chronic disease and elder care. He came to Boston from a position of a Program Director of Smart and Connected Health on a leave from Oregon Health and Science University where he was a Professor at the Department of Biomedical Engineering, with a joint appointment in the Department of Medical Informatics and Clinical Epidemiology. In addition to his academic career, he was a Member of the technical staff at Bell Laboratories in early 1970s, where his research interests included network analysis and modeling, and later at AT&T Laboratories with focus on mobile and Internet-based technologies. His current fundamental research is at the intersection of multilevel computational modeling of complex behaviors of biological and cognitive systems, and augmented cognition. His most recent efforts are fundamental science and technology that would enable the transformation of healthcare to be proactive, distributed and patient-centered.

Holly Brugge Jimison (M’12) is a Professor in the College of Computer and Information Sciences and the College of Health Sciences at Northeastern University, Boston, MA, USA. Her research involves developing design principles for technology to enable patients to be more active and involved in their health care. She is currently the Director of Northeastern.s Consortium on Technology for Proactive Care focused on developing foundations as well as applications preventive and personalized healthcare. Among her key projects is tailoring health interventions based on feedback from in-home monitoring for diverse populations including older adults and those with neurological diseases. This research comprises computer modeling projects for assessing cognitive states using embedded metrics within adaptive computer games. She is recently a Technology Advisor and Health Scientist with the Office of Behavioral and Social Sciences Research at the National Institutes of Health. Her National Institutes of Health work focused on defining new research directions for shared medical decision making and on “big data” initiatives related to developing clinically relevant behavioral markers based on the monitoring of health behaviors in the home and environment.
Ilkka Kimmo Juhani Korhonen is a Ph.D. Adjunct Professor at Personal Health Informatics, Tampere University of Technology, Tampere, Finland, founding partner of PulseOn Oy. He was a Senior Manager in Wellness Business Program, Corporate Alliances and Business Development, Nokia Corporation, Espoo, Finland, and the Chief Research Scientist, Technology Manager, and Research Professor at ICT for Health, VTT Technical Research Center of Finland. His research interests include personal health informatics—making consumers as the primary user of their own health information; behavior informatics, use of technologies for behavioral tracking, computational modeling of behaviors, prediction of them, and eventually changing them for good; wearable health monitoring, especially monitoring and analysis of heart rate and physical activity; personal health systems, mHealth, eHealth, and ambient assisted living technologies and applications; especially wellness and chronic disease management technologies targeting consumer empowerment; biosignal interpretation methods and systems; especially for patient monitoring in critical care, home health care, to support independent living, for wellness management, and context sensitivity; critical care patient monitoring, adequacy of anaesthesia monitoring, level of analgesia monitoring; commercialization of personal and consumer health informatics and mHealth/eHealth, start-ups, business strategy, business models.
He became a Member of the IEEE Engineering in Medicine and Biology Society (IEEE/EMBS) and was elected as Europe representative of Administrative Committee Member, 1.1.2010–31.12.2012; IEEE/EMBS Member in 1999, Senior Member in 2011. He was an Associate Editor of IEEE Transactions on Information Technology in Biomedicine/IEEE Journal of Biomedical Health Informatics in 2002, became Editorial Board Member of Methods of Information in Medicine in 2003–2009. He has published more than 70 papers in international peer-reviewed journals, and more than 100 publications in scientific peer-reviewed conferences.

Christine M. Gordon received the M.P.H. degree in urban health and the B.A. degree in english language and literature from Northeastern University, Boston, MA, USA.
She is currently a Project Manager and Research Coordinator for the Consortium on Technology for Proactive Care at Northeastern University, an interdisciplinary program in the College of Computer and Information Science and Bouvé College of Health Sciences, Boston. The focus of her work is on evaluating wearable and unobtrusive monitoring devices for tailored intervention development and designing user interfaces that convey meaningful health information through the integration and visualization of multiple data streams. She has previously worked in research support with Brigham and Women.s Hospital, Health Resources in Action, and Northeastern University Colleges of Engineering, all in Boston.
Niilo Saranummi (SM’06–F’09) received the Dr.Tech. degree in biomedical engineering from the Tampere University of Technology, Tampere, Finland, in 1976.
He is currently a Research Professor at VTT Technical Research Centre of Finland, Espoo, Finland. His research interests include personal health systems and eHealth, and innovation, technology transfer and technology policy setting in health technologies. He was the President of the International Federation for Medical and Biological Engineering (IFMBE) from 1991 to 1994, an International Union for Physical and Engineering Sciences in medicine from 1994 to 1997, the Interim President of European Alliance for Medical and Biological Engineering and Science from 2003 to 2004, and the Chair of the International Academy of Medical and Biological Engineering from 2009 to 2012.
Dr. Saranummi was the Editor-in-Chief of IEEE Transactions of Information Technology in biomedicine from 2002 to 2007. He received the IFMBE.s Otto Schmitt Award in 2006. He is a Fellow of the International Academy of Medical and Biological Engineering, the American Institute of Medical and Biological Engineering and Health Level Seven.
Contributor Information
Misha Pavel, Email: m.pavel@neu.edu, Northeastern University, Boston, MA 02115 USA.
Holly B. Jimison, Northeastern University.
Ilkka Korhonen, Tampere University of Technology.
Christine M. Gordon, Northeastern University
Niilo Saranummi, VTT Technical Research Centre of Finland.
References
- 1.PCAST. Realizing the full potential of health information technology to improve healthcare for Americans: The path forward. President’s Council of Advisors on Science and Technology; Washington, DC, USA. 2010. [Google Scholar]
- 2.Center for Disease Control. Chronic Diseases, The Power to Prevent, The Call to Control: At A Glance. 2009 Dec 20; [Online]. Available: http://www.cdc.gov/chronicdisease/resources/publications/aag/pdf/chronic.pdf.
- 3.McGinnis JM, et al. The case for more active policy attention to health promotion. Health Affairs. 2002;21:78–93. doi: 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]
- 4.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270:2207–2212. [PubMed] [Google Scholar]
- 5.Schroeder SA. We can do better—Improving the health of the American people. N Engl J Med. 2007;357:1221–1228. doi: 10.1056/NEJMsa073350. [DOI] [PubMed] [Google Scholar]
- 6.Vincent GK, Velkoff VA. The Next Four Decades: The Older Population in the United States: 2010 to 2050. Washington, DC, USA: U.S. Dept. of Commerce, Economics and Statistics Administration, U.S. Census Bureau; 2010. [Google Scholar]
- 7.Michie S, Johnston M. Encyclopedia of Behavioral Medicine. New York, NY, USA: Springer; 2013. Behavior change techniques; pp. 182–187. [Google Scholar]
- 8.Spruijt-Metz D, et al. Building new computational models to support health behavior change and maintenance: New opportunities in behavioral research. Transl Behav Med. 2015;5:335–346. doi: 10.1007/s13142-015-0324-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wactlar H, et al. Can computer science save healthcare? IEEE Intell Syst. 2011 Sep-Oct;26(5):3–7. [Google Scholar]
- 10.Krebs P, et al. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51:214–221. doi: 10.1016/j.ypmed.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sohl SJ, Moyer A. Tailored interventions to promote mammography screening: A meta-analytic review. Prev Med. 2007;45:252–261. doi: 10.1016/j.ypmed.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Strecher VJ, et al. Moderators and mediators of a web-based computer-tailored smoking cessation program among nicotine patch users. Nicotine Tobacco Res. 2006;8:S95–S101. doi: 10.1080/14622200601039444. [DOI] [PubMed] [Google Scholar]
- 13.Ammerman LC, et al. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: A review of the evidence. Prev Med. 2002;35:25–41. doi: 10.1006/pmed.2002.1028. [DOI] [PubMed] [Google Scholar]
- 14.Jimison HB, Pavel M. Integrating computer-based health coaching into elder home care. Assistive Technol Res Ser. 2008;21:122–129. [Google Scholar]
- 15.Rivera DE, Jimison HB. Systems modeling of behavior change: Two illustrations from optimized interventions for improved health outcomes. IEEE Pulse. 2013 Nov;4(6):41–47. doi: 10.1109/MPUL.2013.2279621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hagler S, et al. Assessing executive function using a computer game: Computational modeling of cognitive processes. IEEE J Biomed Health Informat. 2014 Jul;18(4):1442–1452. doi: 10.1109/JBHI.2014.2299793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ofli F, et al. Design and evaluation of an interactive exercise coaching system for older adults: Lessons learned. IEEE J Biomed Health Informat. 2015 Jan 13; doi: 10.1109/JBHI.2015.2391671. to be published. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perez-Macias JM, et al. Comparative assessment of sleep quality estimates using home monitoring technology. Proc IEEE Conf Eng Med Biol Soc. 2014 Aug;2014:4979–82. doi: 10.1109/EMBC.2014.6944742. [DOI] [PubMed] [Google Scholar]
- 19.Pavel M, et al. Optimizing medication reminders using a decision-theoretic framework. Stud Health Technol Informat. 2010;160:791–795. [PubMed] [Google Scholar]
- 20.Jimison HB, et al. A socialization intervention in remote health coaching for older adults in the home. Proc IEEE 35th Annu Int Conf Eng Med Biol Soc. 2013:7025–7028. doi: 10.1109/EMBC.2013.6611175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavorial medicine. Ann Behav Med. 1994;16:199–202. [Google Scholar]
- 22.Shiffman S. Conceptualizing analyses of ecological momentary assessment data. Nicotine Tobacco Res. 2014;16:S76–S87. doi: 10.1093/ntr/ntt195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Intille SS. Technological innovations enabling automatic, context-sensitive ecological momentary assessment. In: Stone AA, Shiffman S, Atienza AA, Nebeling L, editors. The Science of Real-Time Data Capture: Self-Report in Health Research. London, U.K: Oxford Univ. Press; 2007. pp. 308–337. [Google Scholar]
- 24.Intille SS, et al. Just-in-time context-sensitive questioning for preventative health care. Proceedings of the AAAI 2002 Workshop on Automation as Caregiver: The Role of Intelligent Technology in Elder Care; Menlo Park, CA, USA: AAAI Press; 2002. [Google Scholar]
- 25.Nahum-Shani I, et al. Methodology Center, Tech Rep. University Park, PA: The Methodology Center, Penn State; 2014. Just in time adaptive interventions (JITAIs): An organizing framework for ongoing health behavior support; pp. 14–126. [Google Scholar]
- 26.Adams MA, et al. An adaptive physical activity intervention for overweight adults: A randomized controlled trial. PLoS One. 2013;8:e82901. doi: 10.1371/journal.pone.0082901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hagler S, et al. Quantification of human movement for assessment in automated exercise coaching. Proc IEEE 36th Annu Int Conf Eng Med Biol Soc. 2014:5836–5839. doi: 10.1109/EMBC.2014.6944955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perez-Macias JM, et al. Comparative assessment of sleep quality estimates using home monitoring technology. Proc IEEE 36th Annu Int Conf Eng Med Biol Soc. 2014:4979–4982. doi: 10.1109/EMBC.2014.6944742. [DOI] [PubMed] [Google Scholar]
- 29.Ali AA, et al. mPuff: automated detection of cigarette smoking puffs from respiration measurements. Proc11th Int Conf Inf Process Sens Netw. 2012:269–280. [Google Scholar]
- 30.Lazer DM, et al. The parable of Google Flu: Traps in big data analysis. Science. 2014;343:1203–1205. doi: 10.1126/science.1248506. [DOI] [PubMed] [Google Scholar]
- 31.Helander EE, et al. Are breaks in daily self-weighing associated with weight gain? PloS One. 2014;9:e113164. doi: 10.1371/journal.pone.0113164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Embretson SE, Reise SP. Item Response Theory. East Sussex, U.K: Psychology Press; 2013. [Google Scholar]
- 33.Ertin E, et al. AutoSense: Unobtrusively wearable sensor suite for inferring the onset, causality, and consequences of stress in the field. Proc 9th ACM Conf Embedded Netw Sens Syst. 2011:274–287. [Google Scholar]
- 34.Nazir S, et al. puffMarker: A multi-sensor approach for pinpointing the timing of first lapse in smoking cessation. Proc ACM Int Joint Conf Pervasive Ubiquitous Comput. 2015:999–1010. [PMC free article] [PubMed] [Google Scholar]
- 35.Ledger D, McCaffrey D. Inside Wearables: How the Science of Human Behavior Change Offers the Secret to Long-Term Engagement. Endeavour Partners; Cambridge, MA, USA: 2014. [Google Scholar]
- 36.Mitesh S, et al. Wearable devices as facilitators, not drivers, of health behavior change. JAMA. 2015;313:459–460. doi: 10.1001/jama.2014.14781. [DOI] [PubMed] [Google Scholar]
- 37.Sarela AK, et al. IST Vivago—An intelligent social and remote wellness monitoring system for the elderly. Proc. IEEE Annu. EMBS Spec. Topic Conf. Inf. Technol. Appl. Biomed; Birmingham, U.K. 2003. pp. 362–365. [Google Scholar]
- 38.Krantz D, et al. Foundations of Measurement, Vol I: Additive and Polynomial Representations. New York, NY, USA: Academic; 1971. [Google Scholar]
- 39.Jimison HB, Pavel M. Advances in Neural Information Processing Systems. Whistler, BC: 2010. A utility and context based framework for addressing the machine learning challenges of detecting rare but important clinical events; p. 44. http://media.nips.cc/Conferences/2010/NIPS-2010-Workshop-Book.pdf. [Google Scholar]
- 40.Thiemjarus S, Yang G-Z. Body Sensor Networks. New York, NY, USA: Springer; 2006. Context-aware sensing; pp. 287–331. [Google Scholar]
- 41.Hagler S, et al. Unobtrusive and ubiquitous in-home monitoring: A methodology for continuous assessment of gait velocity in elders. IEEE Trans Biomed Eng. 2010 Apr;57(4):813–20. doi: 10.1109/TBME.2009.2036732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Beattie ZT, et al. Classification of breathing events using load cells under the bed. Proc IEEE 31st Annu Int Conf Eng Med Biol Soc, Eng Future Biomed. 2009:3921–3924. doi: 10.1109/IEMBS.2009.5333548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Adami A, et al. Using load cells under the bed as a non-contact method for detecting periodic leg movements. IRBM. 2014;35:334–340. [Google Scholar]
- 44.Aggarwal JK, Ryoo MS. Human activity analysis: A review. ACM Comput Surv. 2011;43:1–43. [Google Scholar]
- 45.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Amer Geriatr Soc. 1983;31:721–727. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 46.Webb JA, Aggarwal JK. Structure from motion of rigid and jointed objects. Artif Intell. 1982;19:107–130. [Google Scholar]
- 47.Niyogi SA, Adelson EH. Analyzing gait with spatiotemporal surfaces. Proc IEEE Workshop Motion Non-Rigid Articulated Objects. 1994:64–69. [Google Scholar]
- 48.Campbell LW, Bobick AF. Recognition of human body motion using phase space constraints. Proc 5th Int Conf Comput Vis. 1995:624–630. [Google Scholar]
- 49.Banerjee T, et al. Detecting foreground disambiguation of depth images using fuzzy logic. Proc IEEE Int Conf Fuzzy Syst. 2013:1–7. [Google Scholar]
- 50.Ames AD, Vasudevan R, Bajcsy R. Human-data based cost of bipedal robotic walking. Proceedings of the 14th international conference on Hybrid systems: computation and control; 2011. pp. 153–162. [Google Scholar]
- 51.Stone E, Skubic M. Evaluation of an inexpensive depth camera for in-home gait assessment “. J Ambient Intell Smart Environ. 2011;3:349–361. [Google Scholar]
- 52.Stone E, Skubic M. Testing real-time in-home fall alerts with embedded depth video hyperlink. presented at the Int. Conf. Smart Homes Health Telematics; Denver, CO, USA. 2014. [Google Scholar]
- 53.Chen L, et al. Sensor-based activity recognition. IEEE Trans Syst, Man, Cybern C, Appl Rev. 2012 Nov;42(6):790–808. [Google Scholar]
- 54.Krishnan NC, Cook DJ. Activity recognition on streaming sensor data. Pervasive Mobile Comput. 2014;10:138–154. doi: 10.1016/j.pmcj.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Parkka J, et al. Activity classification using realistic data from wearable sensors. IEEE Trans Inf Technol Biomed. 2006 Jan;10(1):119–128. doi: 10.1109/titb.2005.856863. [DOI] [PubMed] [Google Scholar]
- 56.Choudhury T, et al. The mobile sensing platform: An embedded activity recognition system. IEEE Pervasive Comput. 2008 Apr;7(2):32–41. [Google Scholar]
- 57.Mutikainen S, et al. Objectively measured physical activity in Finnish employees: A cross-sectional study. BMJ Open. 2014;4(12):e005927. doi: 10.1136/bmjopen-2014-005927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Smolander J, et al. Estimating oxygen consumption from heart rate and heart rate variability without individual calibration. Clin Physiol Funct Imag. 2011;31:266–271. doi: 10.1111/j.1475-097X.2011.01011.x. [DOI] [PubMed] [Google Scholar]
- 59.Koolhaas J, et al. Stress revisited: A critical evaluation of the stress concept. Neurosci Biobehav Rev. 2011;35:1291–1301. doi: 10.1016/j.neubiorev.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 60.Dikecligil GN, Mujica-Parodi LR. Ambulatory and challenge-associated heart rate variability measures predict cardiac responses to real-world acute emotional stress. Biol Psych. 2010;67:1185–1190. doi: 10.1016/j.biopsych.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.FirstBeat. Stress and Recovery Analysis Method Based on 24-hour Heart Rate Variability. 2014 [Online]. Available: http://www.firstbeat.com/userData/firstbeat/research-publications/Stress-and-recovery_white-paper_2014.pdf.
- 62.Prochaska JO, et al. In search of how people change: Applications to addictive behaviors. Amer Psychol. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 63.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Amer J Health Promotion. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 64.Velicer WF, Prochaska JO. Stage and nonstage theories of behavior and behavior change: A comment on schwarzer. Appl Psychol. 2008;57:75–83. [Google Scholar]
- 65.Stoica P, Moses RL. Spectral Analysis of Signals. Upper Saddle River, NJ, USA: Prentice-Hall; 2005. [Google Scholar]
- 66.Böckenholt U. A latent Markov model for the analysis of longitudinal data collected in continuous time: states, durations, and transitions. Psychol Methods. 2005;10:65–83. doi: 10.1037/1082-989X.10.1.65. [DOI] [PubMed] [Google Scholar]
- 67.Seto E, Bajcsy R. Modeling physical activity behavior change. In: Sazonov E, Neuman MR, editors. Wearable Sensors: Fundamentals, Implementation and Applications. Amsterdam, The Netherlands: Elsevier; 2014. [Google Scholar]
- 68.Vermunt JK, et al. Handbook of Longitudinal Research: Design, Measurement, and Analysis. New York, NY, USA: Academic; 2008. Latent class models in longitudinal research; pp. 373–385. [Google Scholar]
- 69.Kemeny JG, Snell JL. Finite Markov Chains. Vol. 356. Princeton, NJ, USA: van Nostrand; 1960. [Google Scholar]
- 70.Feller W. An Introduction to Probability Theory and Its Applications. Vol. 2. New York, NY, USA: Wiley; 2008. [Google Scholar]
- 71.Norman MF. Markov Processes and Learning Models. Vol. 84. New York, NY, USA: Academic; 1972. [Google Scholar]
- 72.Visser I, et al. Fitting hidden Markov models to psychological data. Sci Program. 2002;10:185–199. [Google Scholar]
- 73.Rabiner L. A tutorial on hidden Markov models and selected applications in speech recognition. Proc IEEE. 1989 Feb;77(2):257–286. [Google Scholar]
- 74.Killeen PR. Markov model of smoking cessation. Proc Nat Acad Sci. 2011;108:15549–15556. doi: 10.1073/pnas.1011277108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pavel M, et al. The role of technology and engineering models in transforming healthcare. IEEE Rev Biomed Eng. 2013 Apr;6:156–177. doi: 10.1109/RBME.2012.2222636. [DOI] [PubMed] [Google Scholar]
- 76.Navarro-Barrientos JE, et al. A dynamical model for describing behavioural interventions for weight loss and body composition change. Math Comput Model Dyn Syst. 2011;17:183–203. doi: 10.1080/13873954.2010.520409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ajzen I. The theory of planned behavior. Org Behav Hum Decision Processes. 1991;50:179–211. [Google Scholar]
- 78.Bollen KA, Noble MD. Structural equation models and the quantification of behavior. Proc Nat Acad Sci. 2011;108:15639–15646. doi: 10.1073/pnas.1010661108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Martin C, et al. A dynamical systems model of social cognitive theory. Proc Amer Control Conf. 2014:2407–2412. [Google Scholar]
- 80.Hofmann W, et al. juImpulse and self-control from a dual-systems perspective. Perspectives Psychol Sci. 2009;4:162–176. doi: 10.1111/j.1745-6924.2009.01116.x. [DOI] [PubMed] [Google Scholar]
- 81.Kahneman D. Thinking, Fast and Slow. 1. New York, NY, USA: Farrar, Straus; 2011. [Google Scholar]
- 82.Shiffrin RM, Schneider W. Controlled and automatic human information processing: II. Perceptual learning, automatic attending and a general theory. Psycholo Rev. 1977;84:128–190. [Google Scholar]
- 83.Spring B, et al. Multiple behavior changes in diet and activity: A randomized controlled trial using mobile technology. Arch Internal Med. 2012;172:789–796. doi: 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Young D. Collaborative medication adherence for elderly adults in a home environment. Tech Rep. 2013 [Google Scholar]
- 85.Zunzunegui MV, et al. Social networks, social integration, and social engagement determine cognitive decline in community-dwelling Spanish older adults. J Gerontol B Psychol Sci Soc Sci. 2003 Mar;58:S93–S100. doi: 10.1093/geronb/58.2.s93. [DOI] [PMC free article] [PubMed] [Google Scholar]