Introduction
Approximately 16–18% of liver transplants in the United States were performed for the oncologic treatment of hepatocellular carcinoma (HCC).(1) Although Transarterial Chemoembolization (TACE) was the most common HCC bridging locoregional therapy while on the waitlist (75%), TACE rarely sterilizes HCC, especially in larger tumors.(1) Studies suggest that only 24% to 90% of patients were successfully down-staged from stage T3-4 tumors to within Milan criteria using TACE as a sole downstaging modality.(2) It is now appreciated that the utilization of more than one locoregional therapy may be most effective in successful HCC downstaging of beyond Milan criteria tumors prior to liver transplantation.
Radiation therapy is increasingly being used to treat large liver tumors where modern computer technology has overcome some of the historic drawbacks via accurate and targeted dose-delivery.(3) The stereotactic radiation therapy (SRT) technique delivers treatment typically over 3–5 treatments, compared to the standard duration of 20–25 treatments over a four to five week period. Accurate delivery of high doses to a small target over fewer treatments has been demonstrated to result in improved liver tumor control and reduced toxicities.(3) While TACE and SRT can be utilized independently, a combination of these therapies maximizes the strengths and reduces the limitations of these individual treatments.(4)
We previously reserved the combination of TACE and SRT to large inoperable HCC patients who were not eligible for liver transplantation.(4) After being impressed with the effectiveness of this treatment combination, we began to use this approach for downstaging beyond Milan criteria HCC patients in attempt to make them eligible for liver transplantation. The purpose of this study is to report a case-series of twelve HCC patients who were treated with TACE followed by SRT in attempt to successfully downstage for liver transplantation.
Methods
Treatment Approach
An a priori decision to utilize TACE followed by SRT to downstage HCC patients so they could be considered for liver transplantation was made at a multidisciplinary tumor board comprising of transplant surgeons, hepatologists, radiologists, interventional radiologists, nuclear medicine physicians, medical oncologists and radiation oncologists.
When SRT was planned to follow TACE, conventional transarterial chemoembolization with lipiodol and chemotherapy was utilized. Lipiodol is visible on fluoroscopy and non-contrast CT, which facilitates localization of the target for image-guided radiotherapy. Targeted super-selective TACE was performed initially in all patients. Briefly, a micro-catheter was advanced to the tumor-feeding artery or arteries. Non-tumor liver tissue was spared as much as possible. A mixture of 50 mg doxorubicin and lipiodol was delivered until the tumor is saturated. This is followed with 400 micron Embozene® microsphere particles (CeloNova BioSciences, TX) to achieve complete stasis. The lipiodol used during embolization typically remains in the tumor for several months when administered as described above. (Figure 1)
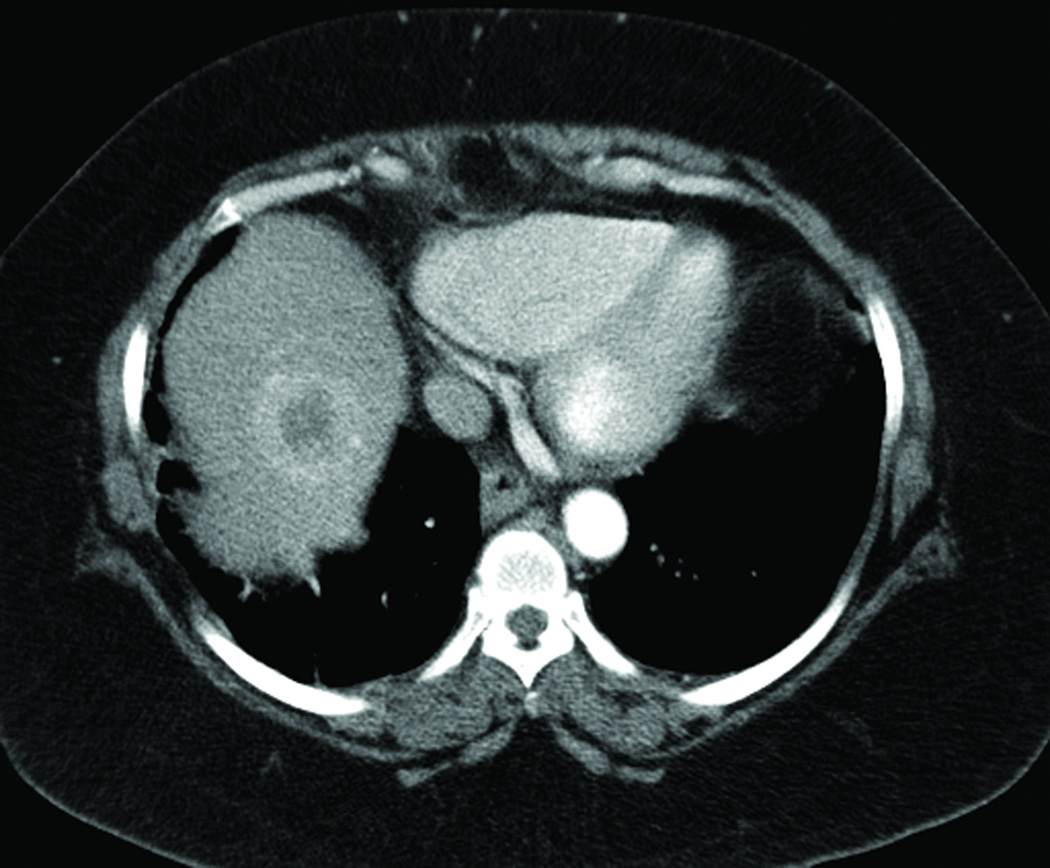
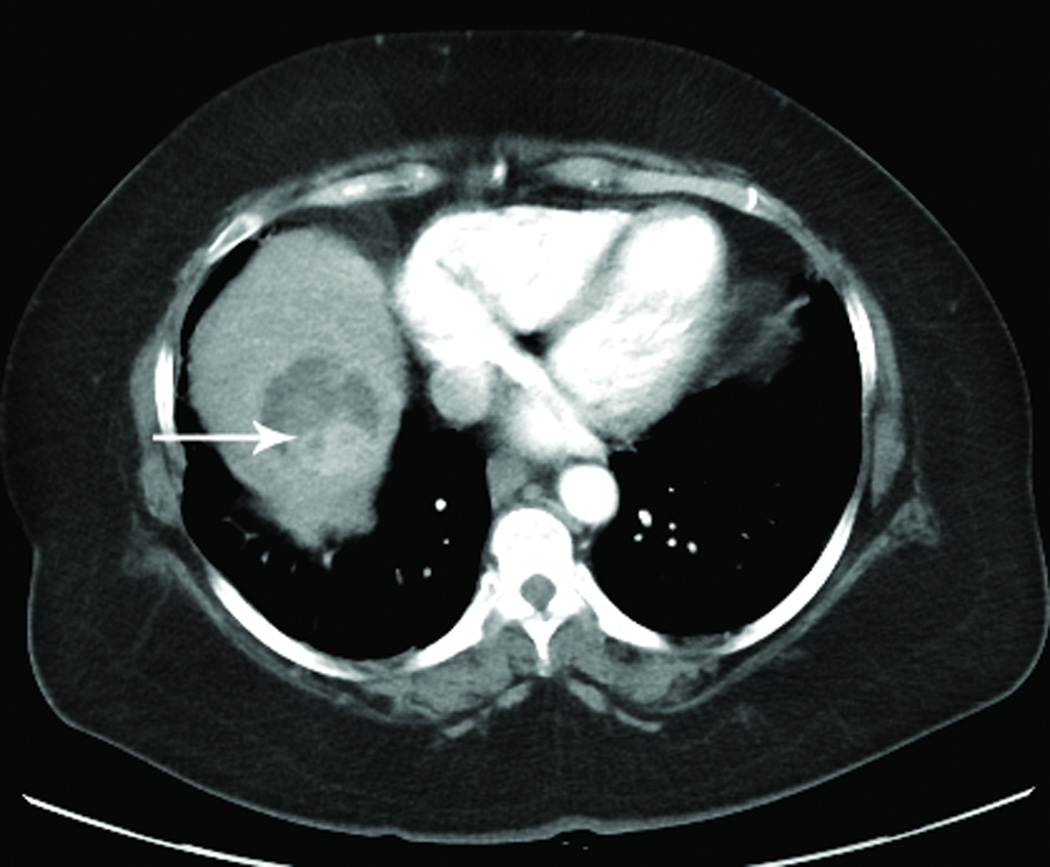
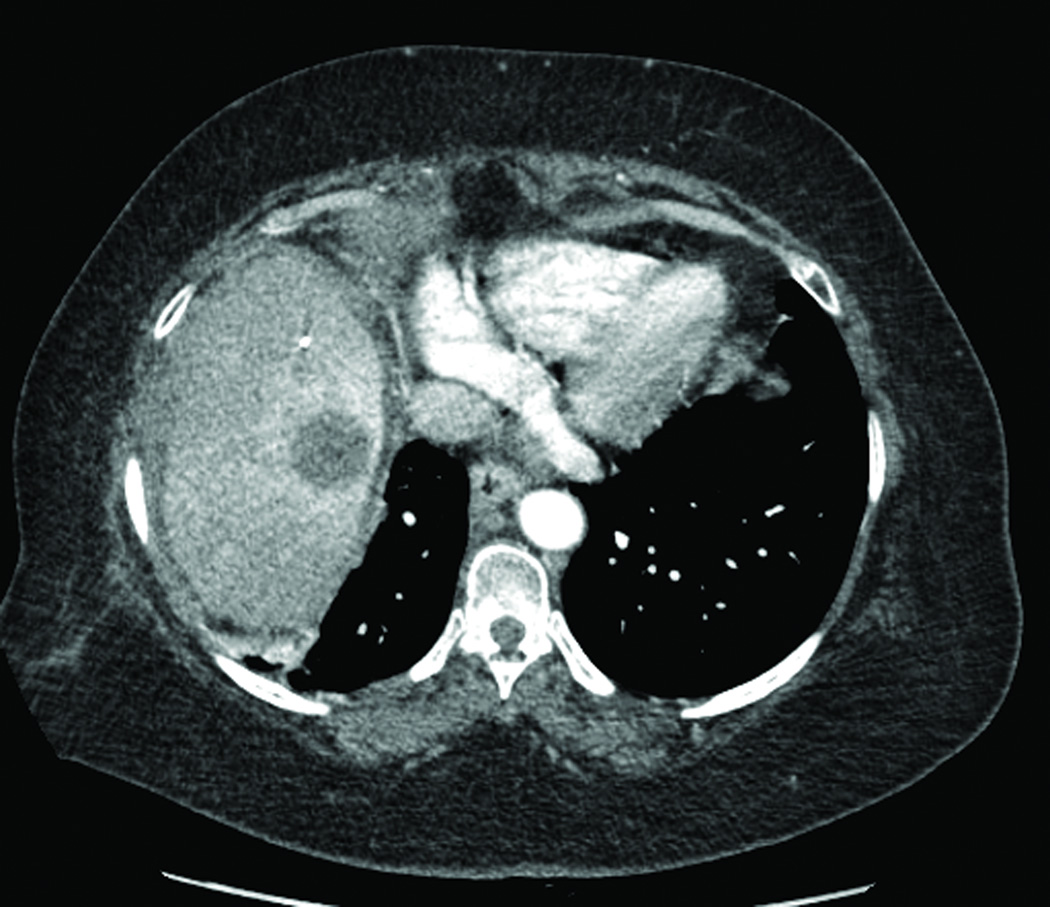
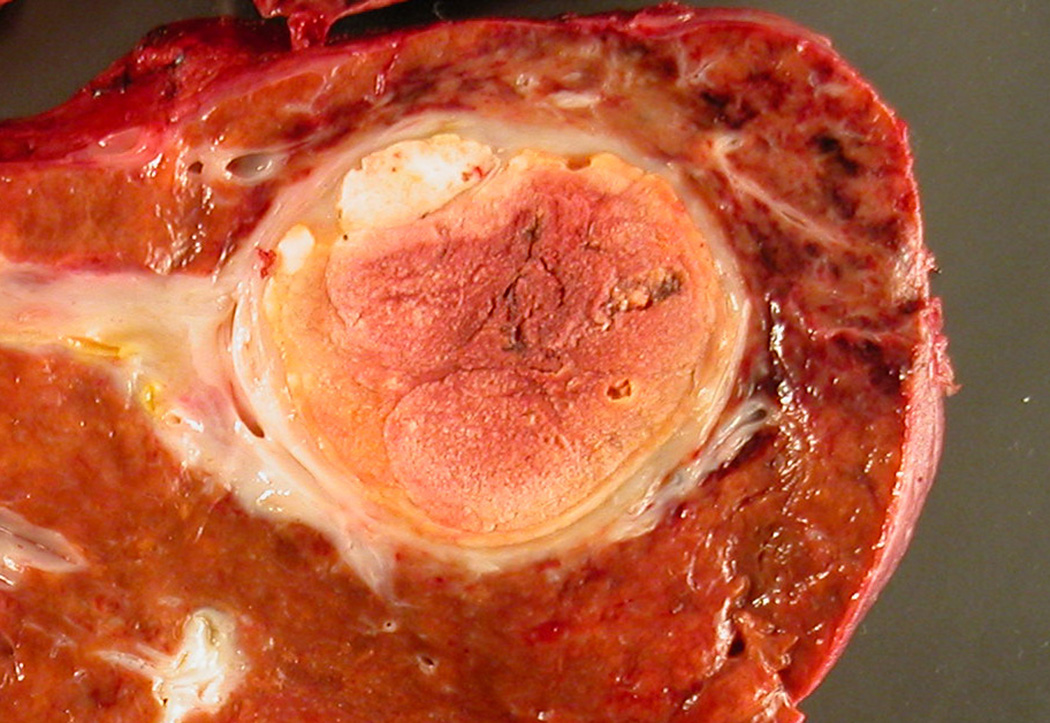
Figure 1.

Example of waitlisted patient with a beyond Milan criteria HCC treated with TACE followed by SRT. Initial CT imaging of HCC tumor (a), CT imaging of HCC tumor after TACE treatment demonstrating mRECIST partial tumor necrosis with arrow denoting persistent viable tumor (b), CT imaging illustrating SRT planning (c), CT imaging of HCC tumor post SRT treatment demonstrating mRECIST complete tumor necrosis (d), and gross explant pathology of the HCC tumor after treatment with TACE followed by SRT therapy with no viable tumor detected microscopically (e).
If the tumor-lipiodol was not well visualized following TACE, patients underwent CT-guided placement of liver fiducials (Civco Polymark 1 mm × 3 mm fiducials; Civco Medical Solutions; Orange City, IA) to facilitate image registration and tumor targeting at the time of radiation treatment.
SRT for HCC was typically performed using a three-fraction schedule for a total of 45 Gy, delivered over 10 calendar days. Clinically accepted practices were followed including custom immobilization, treatment planning, respiratory correction, and image guided treatment delivery. (4). Fixed-field intensity-modulated radiation therapy (IMRT) or dynamic arc plans were utilized for treatment delivery on a linear accelerator. At least 800 cc of normal liver parenchyma volume was spared to receive less than 15 Gy during SRT. Changes in SRT dosing were made only when 800cc of uninvolved liver could not be spared, or dose-tolerance limits to adjacent critical organs could not be met.
Case Series
There were twelve patients who were treated with TACE-SRT combination, with a mean follow-up of 29 months (range 6–48). (Table 1) These patients (8 male, 4 female) were not initially transplant candidates because their tumors exceeded the Milan criteria. The mean age of the patient group was 58.6 years (range 42 – 70 years). The MELD score ranged from 6–14 and no patients had clinically evident hepatic decompensation symptoms. HCC diagnosis was made based upon Organ Procurement and Transplant Network (OPTN) Criteria: one 5b tumor (6 patients), two 5b tumors (5 patients), one 5b and one 5a tumors (1 patient). In addition to meeting imaging criteria, four of the patients had an alpha feto-protein level over 100 and the four patients had biopsy-proven HCC. The underlying liver disease was hepatitis B (n=3), hepatitis C (n=4–6), alcohol (n=1), alpha-1 anti-trypsin (n=1), and non-alcoholic steato-hepatitis (n=1). A total of 18 tumors were treated in these twelve patients, sizes ranging from 1.7 to 7.6 cm (mean 4.2 cm). A single TACE procedure was performed in 7 patients while the remaining 5 patients had 2 TACE procedures performed to completely embolize the HCC prior to SRT. Though thermal ablation was typically used at our institution to treat HCC < 3 cm, five patients had lesions <3 cm that were too close to major blood vessels or biliary tree and thus were treated with SRT. The mean time from diagnosis to first TACE was 7.8 weeks (range 3 to 24), and from TACE to SRT was 13 weeks (range 6 to 18). The mean biological equivalent dose of radiation delivered using SRT was 255Gy3 (180–270 Gy3). The mean time from SRT to liver transplantation was 7.8 months.
Table 1.
Patient Demographics, Tumor Characteristics, and Hepatocellular Carcinoma Treatment Properties
| Age/ gender |
MELD/ CPS |
Baseline decompensation |
Tumor size (cm) |
Segment location |
Decompensation after TACE-SRT |
TACE procedures |
SRT localization |
SRT Doses |
Transplant Status |
|
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 63 M |
MELD12 CPS-C |
MC-HE, V | 3.6; 2.2 | 5; 8 | MC-HE, V | 2 | Lipiodol | 15 Gy 3 doses |
Transplanted |
| 2 | 60 F |
MELD7 CPS-A |
None | 3.9; 2.2 | 6; 5 | MC-HE, MC-A | 2 | Lipiodol | 15 Gy 3 doses |
Transplanted |
| 3 | 42 M |
MELD6 CPS-A |
None | 4.5, 3.0 | 6/7; 5 | None | 1 | Lipiodol | 15 Gy 3 doses |
Transplanted |
| 4 | 70 M |
MELD6 CPS-A |
None | 6.0 | 8 | None | 1 | Lipiodol | 15 Gy 2 doses |
Transplanted |
| 5 | 53 F |
MELD8 CPS-B |
V | 4.7,1.7 | 7; 8 | V | 2 | Fiducials | 15 Gy 3 doses |
Transplanted |
| 6 | 66 M |
MELD7 CPS-A |
None | 5.5 | 4/5/8 | None | 1 | Lipiodol | 15 Gy 3 doses |
Transplanted |
| 7 | 57 M |
MELD6 CPS-A |
None | 4.7 | 5/8 | None | 1 | Fiducials | 15 Gy 3 doses |
Active on Waitlist |
| 8 | 58 M |
MELD9 CPS-B |
V | 5.7 | 5/6 | MC-HE, MC-PE, renal failure |
1 | Lipiodol | 15 Gy 3 doses |
Died of sepsis 2mo after SRT |
| 9 | 60 F |
MELD13 CPS-B |
None | 7.6 | 7 | None | 2 | Lipiodol | 15 Gy 3 doses |
POD outside of SRT field |
| 10 | 61 M |
MELD9 CPS-B |
PE | 4.5, 2.0 | Central Rt Lobe 5/6/7/8 |
MC-A | 1 | Fiducials | 13.5 Gy 2 doses* |
POD outside of SRT field |
| 11 | 55 M |
MELD14 CPS-C |
Jaundiced | 6.0 | 5/6/7 | A | 1 | Lipidol | 7.5 Gy 6 doses** |
POD outside of SRT field |
| 12 | 58 M |
MELD10 CPS-A |
None | 5.2, 2.4 | 5/8 | V, A | 2 | Lipiodol | 15 Gy 3 doses |
POD at edge of SRT field |
F Female; M Male; CPS Child-Pugh Score; MC Medically Controlled; HE Hepatic Encephalopathy; V Varices; A Ascites; PE Pleural Effusion; Gy Gray; SRT Stereotactic RadioTherapy; POD Progression Of Disease;
chosen due to a smaller than average total liver volume;
chosen due to concern for acute toxicity in setting of poor LFTs
Six patients have undergone liver transplantation. The liver transplant operations were straightforward with 3/6 recipients receiving no blood products (mean red blood cell transfusion 3.2u). There were no complications with the hepatic artery reconstruction. Two of the six patients developed biliary strictures post-transplant managed endoscopically. One patient developed acute cellular rejection within 90 days of transplantation managed with pulse steroid therapy. Explant pathology demonstrated pathological complete response, with no viable tumor detected in the 10 treated HCC sites in the six case series patients (100% necrosis). However, there was viable HCC tumor present in two patients in areas of the liver that were not treated with either TACE or SRT. In one patient there was evidence of small diameter (<1cm) multifocal HCC involving both lobes, while in another patient there was a single focus of additional HCC (1.4cm) away from the treated site, not apparent on the diagnostic imaging. One patient died without evidence of tumor-recurrence at 29 weeks following liver transplantation due to medication noncompliance. Five patients are alive and without signs of tumor recurrence at the time of reporting.
Six patients did not undergo transplantation. (Table 1) One patient is active on the transplant waitlist. One patient died of sepsis 2 months after SRT. Three patients developed new HCC tumors outside the SRT treatment field while on the waitlist and were delisted. In each of these three cases, the TACE +SRT treated HCC tumors demonstrated a complete radiographic response based upon mRECIST criteria. One patient developed progressive tumor growth at the margin of the SRT treatment field and also was delisted.
Discussion
This limited case-series demonstrates the effectiveness of TACE followed by SRT in downstaging beyond Milan Criteria HCC. TACE followed by SRT was completed in all twelve patients. Six patients underwent liver transplantation after downstaging, and perhaps most compelling, no viable tumor was detected on explant pathology in the treated HCCs. Furthermore, the SRT-treated tumors demonstrated a complete radiographic response in the 3/4 patients delisted (for tumor progression elsewhere in the liver). Only one patient demonstrated tumor progression at the margin of the SRT treatment field. While TACE and SRT can be utilized independently, a combination of these therapies is complimentary and has a number of potential advantages. TACE-related treatment failures are expected to occur at the periphery of the treated tumor, which often has supplemental vascular supply whereas SRT-related treatment failures typically occur at the center, where the tumor is most hypoxic.(4) Initial TACE treatment typically results in tumor involution and can help reduce radiation fields thus sparing uninvolved hepatic parenchyma. In addition, cytotoxic agents used in TACE can exert a local radio-sensitization effect, and TACE-SRT combination may be synergistic.
Perhaps the pragmatic clinical debate is whether or not it is necessary to utilize SRT as HCC downstaging adjunct to TACE. There are no randomized clinical trials to inform clinical decision-making. In this limited case series, only one patient died following TACE + SRT. Low complication rates have been reported among studies of SRT(5, 6) thus the treatment regimen appears safe even in the setting of cirrhosis and liver decompensation. A transplant center’s approach is based upon their philosophy as to whether it is acceptable to simply shrink a HCC tumor while on the waitlist, or aim for complete tumor necrosis. The tumor response rate following TACE +SRT was significantly higher than similar studies using SRT alone as a bridge to transplant.(5, 6) Furthermore, the non-transplant HCC literature demonstrates a survival advantage to treating the periphery of TACE-treated HCC tumors with an additional locoregional therapy. For small HCC tumors, ablation has been demonstrated to result in increased HCC necrosis and improved survival. However, technical failure with HCC tumors ≥3 cm or centrally located lesions are common. Our center utilizes SRT following TACE treatment of HCC tumors greater than 3.0 cm.(4) SRT dosage may need to be modified for peripheral tumors adjacent to the heart or hollow viscus. A recent meta-analysis which studied 17 clinical trials treating over 1476 patients using either TACE or a combination of TACE with conventional radiation therapy demonstrated a significant improvement in overall survival with the use of the combined therapy compared to TACE alone.(7) These studies demonstrate improved survival in non-transplant patients although the role of SRT as a bridge to transplant remains unclear.
In conclusion, this limited case series suggests that TACE followed by SRT may be an effective downstaging approach for select patients with HCC tumors >3 cm that exceed the Milan criteria HCC.
Acknowledgments
This research was funded by National Institutes of Health grant numbers 1 K23 DK091514 (DD) and 1 R03 DK106432 (DD).
Abbreviations
- HCC
Hepatocellular Carcinoma
- TACE
Trans-Arterial Chemoembolization
- SRT
Stereotactic Radiation
- SRTR
Scientific Registry of Transplant Recipients
- IMRT
Intensity-Modulated Radiation Therapy
- CT
Computed Tomography
- Gy
Gray
- AFP
Alpha Feto-Protein
Footnotes
Disclosure
The authors of this manuscript have no conflicts of interest to disclose as described by the journal Liver Transplantation.
References
- 1.Freeman RB, Jr, Steffick DE, Guidinger MK, Farmer DG, Berg CL, Merion RM. Liver and intestine transplantation in the United States, 1997–2006. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2008;8(4 Pt 2):958–976. doi: 10.1111/j.1600-6143.2008.02174.x. [DOI] [PubMed] [Google Scholar]
- 2.De Luna W, Sze DY, Ahmed A, Ha BY, Ayoub W, Keeffe EB, et al. Transarterial chemoinfusion for hepatocellular carcinoma as downstaging therapy and a bridge toward liver transplantation. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2009;9(5):1158–1168. doi: 10.1111/j.1600-6143.2009.02576.x. [DOI] [PubMed] [Google Scholar]
- 3.Hawkins MA, Dawson LA. Radiation therapy for hepatocellular carcinoma: from palliation to cure. Cancer. 2006;106(8):1653–1663. doi: 10.1002/cncr.21811. [DOI] [PubMed] [Google Scholar]
- 4.Jacob R, Turley F, Redden DT, Saddekni S, Aal AK, Keene K, et al. Adjuvant stereotactic body radiotherapy following transarterial chemoembolization in patients with non-resectable hepatocellular carcinoma tumours of >/= 3 cm. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2015;17(2):140–149. doi: 10.1111/hpb.12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Facciuto ME, Singh MK, Rochon C, Sharma J, Gimenez C, Katta U, et al. Stereotactic body radiation therapy in hepatocellular carcinoma and cirrhosis: evaluation of radiological and pathological response. Journal of surgical oncology. 2012;105(7):692–698. doi: 10.1002/jso.22104. [DOI] [PubMed] [Google Scholar]
- 6.Dewas S, Mirabel X, Kramar A, Jarraya H, Lacornerie T, Dewas-Vautravers C, et al. [Stereotactic body radiation therapy for liver primary and metastases: the Lille experience] Cancer radiotherapie : journal de la Societe francaise de radiotherapie oncologique. 2012;16(1):58–69. doi: 10.1016/j.canrad.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Meng MB, Cui YL, Lu Y, She B, Chen Y, Guan YS, et al. Transcatheter arterial chemoembolization in combination with radiotherapy for unresectable hepatocellular carcinoma: a systematic review and meta-analysis. Radiotherapy and oncology : journal of the European Society for Therapeutic Radiology and Oncology. 2009;92(2):184–194. doi: 10.1016/j.radonc.2008.11.002. [DOI] [PubMed] [Google Scholar]