Abstract
Purpose
Despite advances in therapies, disparities in outcomes have been documented for rheumatoid arthritis (RA) patients for both ethnicity and English-language proficiency. The goals of these analyses were to compare differences in RA patient-reported outcomes, by both self-identification of ethnicity and English language proficiency, and to identify factors that might explain differences among groups
Methods
Data collected through structured telephone interviews of a longitudinal cohort with physician-diagnosed rheumatoid arthritis (n=438); only women were included (n=335). Three groups were defined based on self-reported ethnicity and English proficiency: (white/English, n=219), (Hispanic/English, n=39), and (Hispanic/Spanish, n=77). Outcomes examined were patient-reported physical functioning, pain, and presence of moderate or severe fatigue. Multivariate regression analyses compared outcomes among groups adjusting for sociodemographic characteristics, health and disease factors, and depression.
Results
Hispanic/Spanish women had worse function, pain, and fatigue than either English-proficient group. Depression was associated with all outcomes (p<0.0001), and accounted for greater differentials in scores than ethnicity/language proficiency. In interaction analyses, differences between women who were and were not depressed were greater for Hispanic/English than for Hispanic/Spanish. Non-depressed Hispanic/Spanish scores were significantly worse than non-depressed Hispanic/English; i.e., the impact of depression was less for Hispanic/Spanish because both depressed and non-depressed women in this group reported worse outcomes. After adjustment for sociodemographic factors and depression, language remained significantly associated with outcomes.
Conclusions
Disparities in patient-reported outcomes may be driven less by ethnicity than by sociodemographic or psychological factors. Measurement instruments that are not culturally appropriate and equivalent may also hamper meaningful analyses of disparities.
Background
Over the past decade, health outcomes for persons with rheumatoid arthritis (RA) have improved significantly in large part due to advances in therapies and treatment strategy. However, improvements in outcomes have not been universal for all persons with RA, particularly vulnerable populations defined by race and ethnicity, level of English language proficiency, immigrant status, and extent of education1–5. As a result, disparities in outcomes such as pain, disease activity, and function have been documented5–7. For example, a study of nearly 500 ethnically diverse RA patients revealed significantly worse disease activity and function scores among African Americans and non-US born Hispanics8 as well as patients with low English language proficiency.9,10 Similar effects have been demonstrated in other chronic conditions such as diabetes and asthma11–13.
The “Hispanic paradox,” in which Hispanics exhibit greater severity in clinical manifestations and have lower SES but have decreased risk of mortality, has been observed in RA14. However, several studies have noted that Hispanics rate their health worse than other groups, in spite of the “Hispanic paradox” in mortality15,16, and differences in self-rated health between Spanish-speaking and English-speaking Hispanics have also been noted17. Data from the CORRONA registry (Consortium of Rheumatology Researchers of North America) also shows that Hispanics had significantly higher disease activity and worse functional status compared to whites, but were not less likely to achieve low disease activity or remission18.
Despite the differences in outcomes documented according to both ethnicity and English language proficiency8,14,18, few studies have conducted a nuanced examination of those differences by performing an analysis that includes both variables. The goals of these analyses were to compare differences in RA outcomes, using both self-identification of ethnicity and English language proficiency, and to identify factors that might explain differences among groups.
Methods
Subjects
Subjects were participants in the UCSF Rheumatoid Arthritis Outcomes Study (RA-OS), for which data are obtained through annual structured telephone interviews. All RA-OS participants were recruited from rheumatology practices and clinics, and all had physician-diagnosed RA. Interviews were conducted in English or Spanish, according to the preference of the participant, and collected information about RA symptoms and medications, other health conditions, functioning, psychological status, and sociodemographic characteristics. Annual re-interview rates have averaged 93% over the history of the RA-OS. The current manuscript uses data collected in 2012–2013. All procedures were approved by the UCSF Committee on Human Research, and participants provided verbal consent.
Ethnicity was self-reported in response to the question, “Are you Latino or of Hispanic origin or descent?” Race was also self-reported, with options of white, black or African-American, Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaska Native, or other. Individuals could indicate more than one category.
438 individuals responded to interviews, 387 women and 51 men. Given that function and symptom reports have been found to differ by sex and that there were too few men to conduct analyses by ethnic and language proficiency groups (4 English-speaking Hispanic men, and 6 Spanish-speaking Hispanic men), only women were included in analyses. Further, an additional 52 women were excluded from analysis because they self-identified their race/ethnicity as other than Caucasian or Hispanic, leaving a total of 335 women in the analysis.
English language proficiency was assessed with the question, “Is English your preferred language?” English language proficiency was also inferred from the language in which the interview was conducted. For 98% (n=328) of the women, the interview was conducted in their stated preferred language. Primary analyses therefore used the language in which the interview was conducted to define English language proficiency, defining three ethnicity/English-language-proficency groups: English-language proficient non- Hispanic whites (white/English, n = 219), English-language-proficient Hispanics (Hispanic/English, n = 39), and non-English-language-proficient Hispanics (Hispanic/Spanish n = 77). To assess the sensitivity of findings to the definition of English language proficiency, analyses were repeated after deleting responses of individuals for whom the interview was not conducted in their stated preferred language (n = 7).
Patient-reported RA outcomes
Two measures of function were examined, disability in valued life activities (VLAs) and functional limitations. VLA disability was measured with the Short Valued Life Activities scale (S-VLA)19, which consists of 14 items covering three domains of functioning: obligatory activities (required for independence), committed activities (represent major life roles such as family care and paid work), and discretionary activities (includes social, leisure, and recreational activities). For the VLA, individuals rate the amount of difficulty experienced in each activity on a 0 – 3 (no difficulty – unable) scale. Activities that are considered by the individual to be unimportant or that the individual does not perform for non-health-related reasons are not rated and not included in scoring. A score is calculated as the mean of all rated items, ranging from 0 – 3. Functional limitations were measured with the Health Assessment Questionnaire (HAQ)20. The HAQ is the most commonly used measure of functioning in RA. Scores range from 0 – 3, using the same response scale as the S-VLA.
Pain and fatigue self-reports were also examined. Current pain was rated on 0 – 100 scale (no pain – worse pain imaginable)20. Fatigue over the past two weeks was rated no fatigue, very mild, mild, moderate, severe, or very severe. For analyses, responses were dichotomized as moderate, severe, or very severe fatigue vs. none, very mild, or mild.
Other variables
Sociodemographic variables included age, income, and education. Low income was defined as a family income ≤125% of the federal poverty level based on household size. Education was categorized as high school education or less vs. greater. Health insurance was coded as none, Medicaid, or other. Health literacy was estimated with three questions developed by Chew21, and was categorized as limited or not limited.
Depressive symptoms were assessed with the Patient Health Questionnaire, and a score ≥10 was used to indicate at least minor depression22. Comorbid conditions were presented as a list, and the total number tallied. For analysis, the number of comorbid conditions was categorized as 0 or 1 vs. 2 or more.
Duration of RA was based on self-reported year of diagnosis or self-reported age at diagnosis. Current use of specific RA medications was queried and responses categorized as current use of biologic therapy, non-biologic DMARD, and prednisone.
Analysis
Differences among the three ethnicity/language groups (white/English, Hispanic/English, Hispanic/Spanish) were first assessed using chi square analyses and analyses of variance (ANOVA) with post-hoc means comparisons. Sequential multivariate linear and logistic regression analyses were then used to compare outcomes among the groups after adjustment for (1) sociodemographic characteristics (age, low income, low education, health insurance source, limited health literacy), (2) health and disease factors (comorbid conditions, RA duration, current use of DMARDS, current use of biologic therapy, and current dose of prednisone), and (3) depression. Because we were particularly interested in potential differences in the relationships between depression and outcomes by language group, we tested for language×depression interactions in models that included the Hispanic participants only.
Results
Subject characteristics
There were significant differences among the groups in all demographic variables examined (Table 1). However, except for age, the differences were predominantly noted between the Hispanic/Spanish group and the two English-speaking groups. Whites were older and more likely to be retired. Spanish-speaking Hispanics were more likely to have low education and low income, less likely to have been born in the United States, more likely to have no health insurance or insurance through Medicaid, and more likely to have limited health literacy. Depression was more prevalent in the Spanish-speaking group.
Table 1.
Participant characteristics
| White, English interview (n = 219) |
Hispanic, English interview (n = 39) |
Hispanic, Spanish interview (n = 77) |
p* | |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Age, years | 63.5 ± 12.4 | 56.3 ± 13.8 | 56.9 ± 13.8 | <.0001 |
| Education ≤ HS | 16.9 (37) | 28.2 (11) | 93.5 (72) | <.0001 |
| Low income | 9.6 (21) | 10.3 (4) | 39.0 (30) | <.0001 |
| Working | 37.9 (83) | 41.0 (16) | 52.6 (40) | .08 |
| Retired | 46.6 (102) | 30.8 (12) | 18.4 (14) | <.0001 |
| Born in US | 87.2 (191) | 84.6 (33) | 2.6 (2) | <.0001 |
| If not born in US, time in US (years) | 43.7 ± 13.4 | 48.7 ± 10.9 | 23.5 ± 12.9 | <.0001 |
| n = 27 | n = 6 | n = 75 | ||
| Limited health literacy | 18.3 (40) | 10.3 (4) | 61.0 (47) | <.0001 |
| Health insurance | ||||
| No insurance | 0.9 (2) | 2.6 (1) | 9.1 (7) | .001 |
| Medicaid | 2.7 (6) | 5.1 (2) | 62.3 (77) | <.0001 |
| Health and RA characteristics | ||||
| PHQ score | 4.4 ± 4.3 | 4.4 ± 5.0 | 8.3 ± 5.1 | <.0001 |
| Depression, PHQ ≥10 | 15.1 (33) | 15.4 (6) | 33.8 (26) | .001 |
| Comorbid conditions, ≥2 | 16.0 (35) | 18.0 (7) | 22.1 (17) | .48 |
| RA duration, years | 25.6 ± 12.) | 24.0 ± 11.3 | 16.2 ± 12.4 | <.0001 |
| RA medications | ||||
| Current use, DMARD | 68.0 (149) | 64.1 (25) | 81.8 (63) | .05 |
| Current use, biologic | 45.7 (100) | 66.7 (26) | 45.5 (35) | .05 |
| Current use, prednisone | 42.9 (94) | 41.0 (16) | 62.3 (48) | .01 |
| RA outcomes | ||||
| Fatigue, moderate or sevee | 51.1 (112) | 48.7 (19) | 79.2 (61) | <.0001 |
| Pain rating | 29.8 ± 27.3 | 31.2 ± 31.9 | 47.6 ± 28.6 | <.0001 |
| HAQ | 1.125 ± 0.69 | 1.125 ± 0.87 | 1.33 ± 0.79 | .10 |
| VLA difficulty | 0.75 ± 0.60 | 0.63 ± 0.63 | 1.12 ± 0.79 | <.0001 |
| Self-rated health (excellent, very good, good) | 58.0 (127) | 61.5 (24) | 23.4 (18) | <.0001 |
| Global rating | 68.3 ± 26.3 | 72.6 ± 24.3 | 50.0 ± 26.8 | <.0001 |
p-value from ANOVA or chi-square analysis. Values presented as % (n) or mean ± standard deviation
Differences in patient-reported outcome measures across ethnic/language groups
The Hispanic/Spanish group had worse function, higher levels of pain, and was more likely to have moderate to severe fatigue than either English-proficient group. There were no significant differences in these outcomes between English-proficient Hispanics and whites.
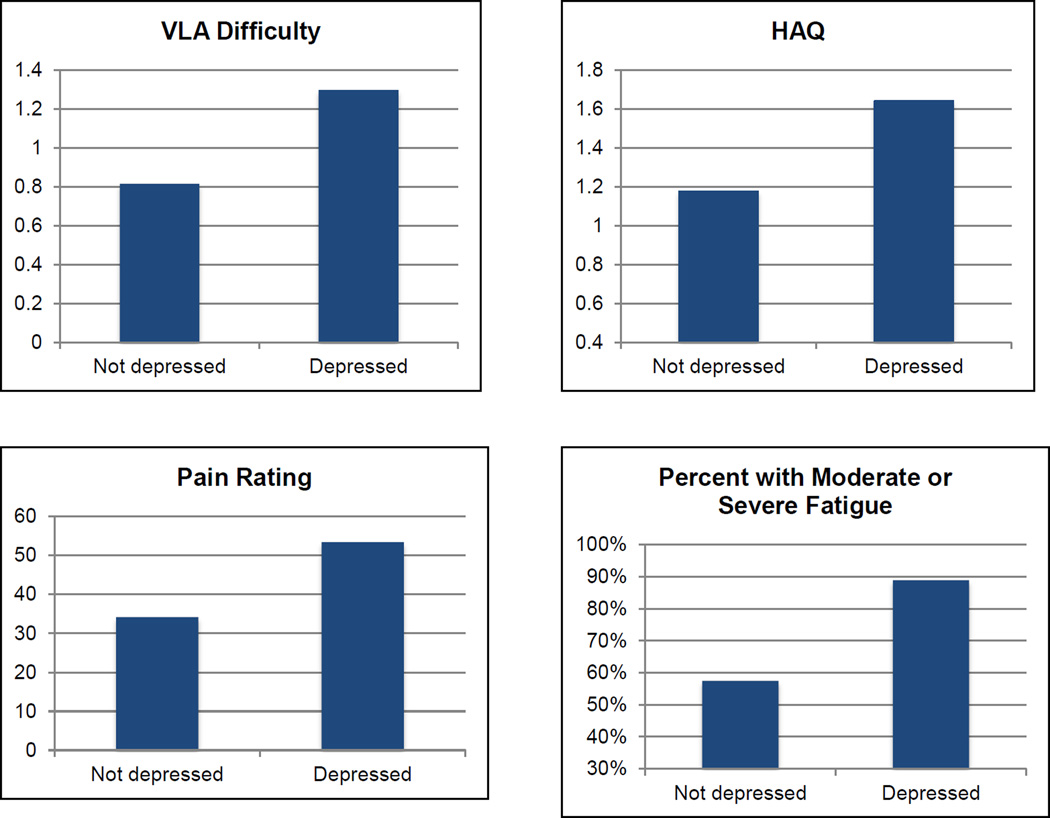
In the multivariate analyses, after accounting for sociodemographic characteristics, health and disease factors, and depression, a significant difference in VLA disability between the Hispanic/Spanish and white/English groups still existed (Table 2). Depression was strongly associated with greater VLA disability (Figure 1), and accounted for a greater differential in scores than ethnicity/language proficiency. Increasing age and disease duration and prednisone use were also significantly associated with VLA disability.
Table 2.
Unadjusted and adjusted mean scores on patient-reported outcomes for English-language proficient non-Hispanic whites (white/English), English-language-proficient Hispanics (Hispanic/English), and non-English-language-proficient Hispanics (Hispanic/Spanish)
| White, English interview (reference group) |
Hispanic, English interview |
Hispanic, Spanish interview |
|
|---|---|---|---|
| VLA disability score | |||
| Unadjusted | 0.77 | 0.63 | 1.12*** |
| Multivariable model 1 | 0.80 | 0.74 | 1.10* |
| Multivariable model 2 | 0.78 | 0.72 | 1.02* |
| Multivariable model 3 | 0.77 | 0.72 | 1.06* |
| Health Assessment Questionnaire | |||
| Unadjusted | 1.12 | 1.13 | 1.41** |
| Multivariable model 1 | 1.12 | 1.20 | 1.38^ |
| Multivariable model 2 | 1.13 | 1.22 | 1.34 |
| Multivariable model 3 | 1.12 | 1.22 | 1.37^ |
| Pain rating | |||
| Unadjusted | 31.1 | 31.2 | 47.6**** |
| Multivariable model 1 | 32.7 | 33.5 | 40.1 |
| Multivariable model 2 | 33.0 | 34.6 | 38.4 |
| Multivariable model 3 | 32.7 | 34.5 | 39.7 |
| Percent with moderate/severe fatigue | |||
| Unadjusted | 53.0 | 48.7 | 80.3*** |
| Multivariable model 1 | 51.0 | 55.1 | 70.8^ |
| Multivariable model 2 | 56.8 | 51.4 | 69.3 |
| Multivariable model 3 | 55.3 | 50.2 | 70.5^ |
Multivariable model 1: Adjusted for sociodemographic characteristicss (age, income, education, health insurance, health literacy)
Multivariable model 2: Model 1 + additional health and disease characteristics (comorbid conditions, RA duration, medication use)
Multivariable model 3: Model 2 + depression (PHQ score)
P-values represent differences from white/English group.
p<.10
p<.05
p<.01
p<.001
p<.0001
Figure 1. Impact of depression on patient-reported outcomes.
Note: All differences between not depressed and depressed significant at p<.0001.
From multiple regression analyses adjusting for ethnicity, language, other sociodemographic characteristics (age, income, education, health insurance, health literacy), and additional health and disease characteristics (comorbid conditions, RA duration, medication use).
After accounting for sociodemographic characteristics, the difference between the Hispanic/Spanish and white/English groups in HAQ scores was no longer significant (Table 2). As with VLA disability, depression was strongly associated with higher HAQ scores, and increasing age and disease duration and prednisone use were also significantly associated with HAQ.
For pain and fatigue ratings, after accounting for sociodemographic characteristics, the differences between the Hispanic/Spanish and white/English groups were no longer significant (Table 2). Depression was significant associated with both pain and fatigue ratings.
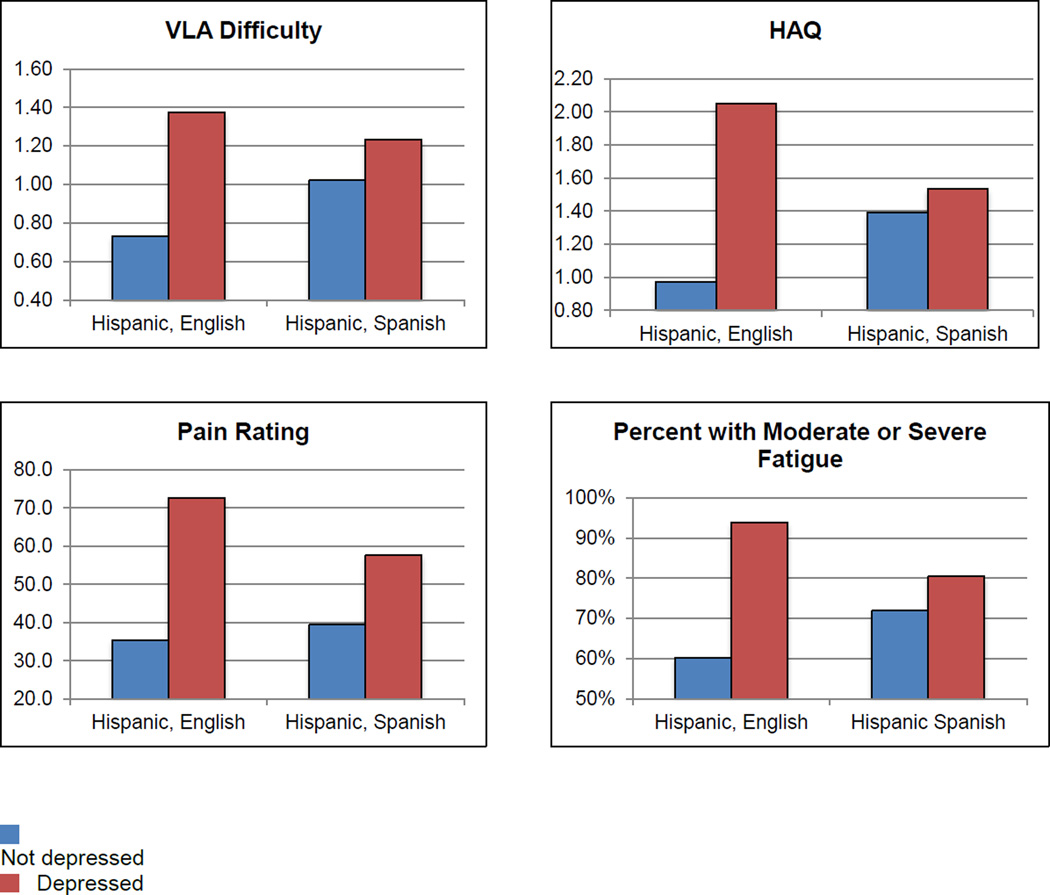
Examination of means for the depressed and non-depressed women in each ethnicity/language group suggested that an interaction might exist between depression and language, such that depression had a larger effect on outcomes in the Hispanic/English group. We therefore tested for language by depression interactions only among the Hispanic participants. Interactions were noted between depression and ethnicity/language for all outcome measures (p<.10). Adjusted means were calculated based on fully adjusted multiple regression models, and Figure 2 shows adjusted mean scores for the English- and Spanish-speaking Hispanics. In each case, the difference between women who were and were not depressed was greater for the English-speaking group than for the Spanish-speaking group. Further, for all measures, the non-depressed Spanish-speaking group’s score was significantly worse than the non-depressed English-speaking group. In other words, the impact of depression was less for Spanish-speaking Hispanics because both depressed and non-depressed women in the latter group reported worse outcomes. In each of these models, the main effect for language remained significant (p<.05).
Figure 2. Adjusted mean scores for RA outcomes for English-speaking and Spanish-speaking Hispanic women: Illustration of interactions.
Note: From multiple regression analyses adjusting for ethnicity, language, other sociodemographic characteristics (age, income, health insurance, health literacy), and additional health and disease characteristics (comorbid conditions, RA duration, medication use).
Discussion
This analysis found statistically and clinically significant decrements in patient-reported RA outcomes of function, pain, and fatigue for Hispanic women with limited English-language proficiency compared to English-proficient women regardless of ethnicity. In contrast, there were no substantive differences between outcomes of English-proficient whites and English-proficient Hispanics.
Sociodemographic differences clearly played a significant role in explaining disparities in patient-reported outcomes. There were large differences in sociodemographic characteristics of the Hispanic/Spanish group compared to both English-proficient groups – they had lower education levels, were more likely to have low incomes, low health literacy, and have no health insurance or Medicaid, and less likely to have been born in the US. Low education and low income have each consistently been linked to poor health outcomes, and these characteristics did account for some of the differences between the Spanish- and English-speaking groups.
Depression also played an important role in explaining disparities in outcomes. Depression was significantly more prevalent among the Hispanic/Spanish group, and was the variable most strongly related to all outcomes in multivariate analyses. Other research has noted high rates of depression among Hispanics in the general population and among Spanish-speaking RA patients, in particular, and has found a strong association of depression with patient-reported outcomes7,23. Depression is generally reported to be present in 15–40% of persons with RA; Hispanic patients appear to have rates at the high end of this range.
The high prevalence of depression and its impact on RA symptoms suggests that Spanish-speaking RA patients are in particular need of effective treatments for depression. However, cultural barriers to appropriate and effective depression treatment may exist for Spanish-speaking Hispanics. A recent qualitative study reported that 89% of Spanish-speaking RA patients said they would not disclose depression, and 80% said they would not be willing to take medication for depression24. While 80% said they would be willing to try psychotherapy for depression, this avenue of treatment is not routinely available in public or safety-net settings, where many Spanish-speaking Hispanics in the US receive their care25. Because depression is associated with RA patient global assessments26, which are an integral part of most RA disease activity scores, there is also a potential for comorbid depression to affect decisions regarding treatment for RA and to impact the results of clinical research and trials.
Notably, however, even though depression was significantly higher among the Spanish-speaking Hispanic group and depression was strongly associated with each outcome, depression did not explain the difference in outcomes between the two Hispanic groups. The non-depressed Spanish-speaking Hispanics had worse outcomes than the English-speaking Hispanics, even after accounting for socioeconomic, health, and disease characteristics.
Are the disparities we noted due to differences in disease status, to reporting bias, to measurement issues, or to other factors? It is difficult to separate assessment of disease status from patient-reports of pain or function from global assessments, because these are often inputs to the assessment of disease status. There is some evidence that Hispanics may have lower pain threshold in experimental settings compared to non-Hispanic whites. However, effect sizes in these studies were small27,28, and could not explain the large differences we found.
Our finding that English-proficient Hispanics and whites had similar outcomes suggests that factors related to acculturation may play an important role, although the mechanism by which this occurs is unclear. Some have noted that extremely positive ratings of health may be viewed culturally by Hispanics as boasting, and thus be unacceptable15. However, a systematic problem with the measurement of patient-reported outcomes in different languages may also exist. Sudano found substantial differences in mean scores of the SF-36 v2 for Spanish-speaking Hispanics vs Caucasians and English-speaking Hispanics29 and suggested that the lack of linguistic equivalence for the response options was at least partially responsible. Bzostek and colleagues noted that the language of interview was a critical measure of acculturation, and that translation issues may account for some of the differences observed15. While many of the outcome measures used in rheumatology have been translated, few have undergone testing for cultural equivalency or differential scale performance. Psychometric experts have concluded that more attention is needed to resolve measurement issues in vulnerable populations, specifically to evaluate the transferability of health outcomes measures to diverse population groups30.
This study does have limitations. In our sample, the number of English-speaking Hispanics was relative small; a larger sample may have yielded more variation in responses. The majority of the Spanish-speaking participants were recruited from a public hospital rheumatology clinic, and based on the general characteristics of patients in that hospital, were primarily from Mexico and Central America, which may limit generalizability. In addition, in our sample, language, sociodemographic characteristics, and literacy were clustered, so the ability to separate the effects of one of these factors may have been limited. The S-VLA has undergone a standard translation – back-translation process, but has not undergone a test of cultural equivalence. However, standard Spanish translations of the HAQ and the pain rating were used. We lacked clinical measures of disease activity or severity or radiographic damage, so differences in patient-reported outcomes could represent actual differences in disease status. However,, it is important to note that patient-reported components are included in many of the standard disease activity measures (such as Disease Activity Scale with 28-Joint Counts (DAS-28), so these measures may be affected by the same reporting disparities that we found.
The disparities we noted exist in the context of growing acceptance of the importance of measuring patient-reported outcomes and of shifts in the US population toward larger numbers of individuals of Hispanic ethnicity, many of whom have limited English-language proficiency. The development of the vast majority of patient-reported outcomes measures has been conducted within “majority” populations; i.e., English-speaking, well educated non-Hispanic whites. While the methods of translating measures for use in non-English-speaking populations have improved, very few of these efforts have included examinations of cultural or conceptual equivalence or understandability of language. PROs need to be measured and tracked over time because they provide important information about patients’ functioning, quality of life, and well-being, but our results illustrate one of the challenges of using and interpreting patient-reported outcome measures in diverse populations.
The findings from our study demonstrate that ethnicity cannot be considered a unidimensional concept. The effects of ethnicity may be outweighed by the effects of sociodemographic factors or culturally-based interpretations31. Factors such as depression may be construed as external to ethnicity, but disparities in prevalence may amplify ethnic differences. Each of these factors suggests a different solution to better measurement of patient-reported outcomes. To address sociodemographic issues, ensuring that patient-reported measures are constructed at appropriate levels of literacy and health literacy is critical. To address depression, culturally appropriate and effective methods of identification and treatment of depression need to be developed and implemented. And, to address cultural differences, patient-reported outcomes measures need to be tested not only for accurate translations, but also for cultural equivalence of concepts and response options. Culturally appropriate and equivalent measurements will be needed to conduct meaningful analyses of the extent and source of apparent disparities.
Future research on measurement of patient-reported outcomes should place examination and achievement of cultural and linguistic equivalence at high priority. Both in the US and internationally, many patient-reported outcomes have been developed with the input or collaboration of patients, but many legacy measures have not. Even measures that have included patient collaborators most often include patients who are well-educated and speak the majority language. While such collaboration ensures that the patient’s voice is included, it does not ensure that the measures are appropriate for patients with low literacy, non-majority language, low education, or who are otherwise socially, demographically, or economically vulnerable.
Significance and Innovation.
Significant decrements in patient-reported RA outcomes of function, pain, and fatigue were found for Hispanic women with limited English-language proficiency compared to English-proficient patients regardless of ethnicity. In contrast, there were no substantive differences between outcomes of English-proficient white and English-proficient Hispanic women.
Sociodemographic characteristics accounted for a substantial portion of the differences in outcomes between English- and Spanish-speaking participants.
Depression was significantly higher among the Spanish-speaking Hispanic women and was strongly associated with each outcome, but did not explain the difference in outcomes between the two Hispanic groups. Even after controlling for depression and sociodemographic factors, language remained a significant predictor of outcomes.
Disparities in patient-reported outcomes may be driven less by ethnicity than by sociodemographic or psychological factors, or by measurement instruments that are not culturally appropriate and equivalent.
Acknowledgements
This research was supported by NIH/NIAMS grant P60 AR053308 and by the Rosalind Russell Medical Research Center for Arthritis.
References
- 1.Schmajuk G, Schneeweiss S, Katz J, Weinblatt M, Setoguchi S, Avorn J, Levin R, Solomon D. Treatment of older adult patients diagnosed with rheumatoid arthritis: improved but not optimal. Arthritis Rheum. 2007;57:928–934. doi: 10.1002/art.22890. [DOI] [PubMed] [Google Scholar]
- 2.Jacobi C, Mol G, Boshuizen H. Impact of socioeconomic status on the course of rheumatoid arthritis and on related use of health care services. Arthritis Rheum. 2003;49:567–573. doi: 10.1002/art.11200. [DOI] [PubMed] [Google Scholar]
- 3.Hernández-Garcia C, Vargas E, Abásolo L, Lajas C, Bellajdell B, Morado I, Macarrón P, Pato E, Fernández-Gutiérrez B, Bañares A, Jover J. Lag time between onset of symptoms and access to rheumatology care and DMARD therapy in a cohort of patients with rheumatoid arthritis. J Rheumatol. 2000;27:2323–2328. [PubMed] [Google Scholar]
- 4.Sokka T, Kautiainen H, Pincus T, Toloza S, da Rocha Castelar Pinheiro G, Lazovskis J, Hetland M, Peets T, Immonen K, Maillefert J, Drosos A, Alten R, Pohl C, Rojkovich B, Bresnihan B, Minnock P, Cazzato M, Bombardieri S, Rexhepi S, Rexhepi M, Andersone D, Stropuviene S, Huisman M, Sierakowski S, Karateev D, Skakic V, Naranjo A, Baecklund E, Henrohn D, Gogus F, Badsha H, Mofti A, Taylor P, McClinton C, Yazici Y. Disparities in rheumatoid arthritis disease activity according to gross domestic product in 25 countries in the QUEST-RA database. Ann Rheum Dis. 2009;68:1666–1672. doi: 10.1136/ard.2009.109983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bruce B, Fries J, Murtagh K. Health status disparities in ethnic minority patients with rheumatoid arthritis: a cross-sectional study. J Rheumatol. 2007;34:1475–1479. [PubMed] [Google Scholar]
- 6.Suarez-Almazor M, Berrios-Rivera J, Cox V, Janssen N, Marcus D, Sessoms S. Initiation of disease-modifying antirheumatic drug therapy in minority and disadvantaged patients with rheumatoid arthritis. J Rheumatol. 2007;34:2400–2407. [PubMed] [Google Scholar]
- 7.Margaretten M, Barton J, Julian L, Katz P, Trupin L, Tonner C, Graf J, Imboden J, Yelin E. Socioeconomic determinants of disability and depression in patients with rheumatoid arthritis. Arthritis Care & Research. 2011;63(2):240–246. doi: 10.1002/acr.20345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barton J, Trupin LD, Gansky S, Tonner C, Margaretten M, Chernitskiy V, Graf J, Imboden J, Yelin E. Racial and ethnic disparities in disease activity and function among persons with rheumatoid arthritis from university-affiliated clinics. Arthritis Care Res. 2011;63:1238–1249. doi: 10.1002/acr.20525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hirsh J, Boyle D, Collier D, Oxenfeld A, Nash A, Quinzanos I, Caplan L. Limited health literacy is a common finding in a public hospital's rheumatology clinic and is predictive of disease severity. J Clin Rheumatol. 2011;17:236–241. doi: 10.1097/RHU.0b013e318226a01f. [DOI] [PubMed] [Google Scholar]
- 10.Caplan L, Wolfe F, Michaud K, Quinzanos I, Hirsh J. Strong association of health literacy with functional status among rheumatoid arthritis patients: a cross-sectional study. Arthritis Care Res. 2014;66:508–514. doi: 10.1002/acr.22165. [DOI] [PubMed] [Google Scholar]
- 11.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan G, Bindman A. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 12.Lopez-Quintero C, Berry E, Neumark Y. Limited English proficiency is a barrier to receipt of advice about physical activity and diet among Hispanics with chronic diseases in the United States. J Am Diet Assoc. 2009;109:1769–1774. doi: 10.1016/j.jada.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Wisnivesky J, Kattan M, Evans D, Leventhal H, Musumeci-Szabó T, McGinn T, Halm E. Assessing the relationship between language proficiency and asthma morbidity among inner-city asthmatics. Med Care. 2009;47:243–249. doi: 10.1097/MLR.0b013e3181847606. [DOI] [PubMed] [Google Scholar]
- 14.Molina E, Haas R, Del Rincon I, Battafarano D, Restrepo J, Escalante A. Does the "Hispanic paradox" occur in rheumatoid arthritis? Survival data from a multiethnic cohort. Arthritis Care Res. 2014;66:972–979. doi: 10.1002/acr.22254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bzostek S, Goldman N, Pebley A. Why do Hispanics in the USA report poor health? Soc Sci Med. 2007;65:990–1003. doi: 10.1016/j.socscimed.2007.04.028. [DOI] [PubMed] [Google Scholar]
- 16.Liang J, Quinones A, Bennett J, Ye W, Xu X, Shaw B, Ofstedal M. Evolving self-rated health in middle and old age: how does it differ across black, Hispanic, and white Americans? J Aging Health. 2010;22:3–26. doi: 10.1177/0898264309348877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brewer J, Miyasato G, Gates M, Curto, Hall S, McKinlay J. Contributors to self-reported health in a racially and ethnically diverse population: focus on Hispanics. Ann Epidemiol. 2013;23:19–24. doi: 10.1016/j.annepidem.2012.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenberg J, Spruill T, Shan Y, Reed G, Kremer J, Potter J, Yazici Y, Ogedegbe G, Harrold L. Racial and ethnic disparities in disease activity in patients with rheumatoid arthritis. Amer J Med. 2013;126:1089–1098. doi: 10.1016/j.amjmed.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katz P, Radvanski D, Allen D, Buyske S, Schiff S, Nadkarni A, Rosenblatt L, Maclean R, Hassett A. Development and validation of a short form of the Valued Life Activities Disability Questionnaire for rheumatoid arthritis. Arthritis Care & Research. 2011;63:1664–1671. doi: 10.1002/acr.20617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fries J, Spitz P, Kraines R, Holman H. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980;23:137–145. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- 21.Chew L, Bradley K, Boyko E. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–594. [PubMed] [Google Scholar]
- 22.Kroenke K, Spitzer R, Williams J. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Karpouzas G, Dolatabadi S, Moran R, Li N, Nicassio P, Weisman M. Correlates and predictors of depression in vulnerable US Hispanics with rheumatoid arthritis. Arthritis Care Res. 2012;64:1274–1281. doi: 10.1002/acr.21689. [DOI] [PubMed] [Google Scholar]
- 24.Withers M, Moran R, Nicassio P, Weisman M, Karpouzas G. Perspectives of vulnerable US Hispanics with rheumatoid arthritis on depression: awareness, barriers to disclosure and treatment options. Arthritis Care Res. doi: 10.1002/acr.22462. [DOI] [PubMed] [Google Scholar]
- 25.Health, United States, 2013. Tables 124 and 125. Hyattsville, MD: 2014. National Center for Health statistics. [PubMed] [Google Scholar]
- 26.Cordingley L, Prajapati R, Plant D, Maskell D, Morgan C, Ali F, Morgan A, Wilson A, JD I, The Biologics in Rheumatoid Arthritis Genetics and Genomics Study Syndicate (BRAGGS) Barton A. Impact of psychological factors on subjective disease activity assessments in patients with severe rheumatoid arthritis. Arthritis Care Res. 2014;66:861–868. doi: 10.1002/acr.22249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rahim-Williams B, Riley J, Herrera D, Hastie B, Fillingim R. Ethnic identify predicts experiental pain perception in African Americans and Hispanics. Pain. 2007;129:177–208. doi: 10.1016/j.pain.2006.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rahim-Williams B, Riley J, Williams A, Fillingim R. A quantative review of ethnic group differences in experimental pain response: Do biology, psychology, and culture matter? Pain Medicine. 2012;13:522–540. doi: 10.1111/j.1526-4637.2012.01336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sudano J, Perzynski A, Love T, Lewis S, Murray P, Huber G, Ruo B, Baker D. Measuring disparities: Bias in the Short Form-36v2 among Spanish-speaking medical patients. Medical Care. 2011;49:480–488. doi: 10.1097/MLR.0b013e31820fb944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stewart S, Napoles-Springer A. Advancing health disparities research: can we afford to ignore measurement issues? Med Care. 2003;41:1207–1220. doi: 10.1097/01.MLR.0000093420.27745.48. [DOI] [PubMed] [Google Scholar]
- 31.O'Neill J, Rader T, Guillemin F, Boonen A, Christensen R, Lyddiatt A, Pardo J, Welch V, Singh J, Tugwell P. Including health equity considerations in development of instruments for rheumatology research: an introduction to a novel OMERACT pardigm. J Rheumatol. 2014;41:150–152. doi: 10.3899/jrheum.130812. [DOI] [PubMed] [Google Scholar]