Abstract
Identifying risk factors for future change in sleep duration can clarify whether, and if so how, sleep and morbidity are bi-directionally related. To date, only limited longitudinal evidence exists characterizing changes to sleep duration among older adults. We aimed to identify factors associated with change in sleep duration in a large sample of older adults (≥60 years) residing in Singapore (n=10335). These adults were monitored as part of the Singapore Chinese Health Study, which collected information regarding daily sleep duration at baseline (assessed in 1993-1998) and at a follow-up wave conducted over a mean of 12.7 years later (assessed in 2006-2010). Among adults sleeping 6-8 hours at baseline (n=8265), most participants (55.6%) remained 6-8 hour sleepers at follow-up, while 8.4% became short (<6 hour) and 36.0% became long (>8 hours) sleepers. A history of stroke, diabetes, cancer, hip fracture, and greater age all independently increased the odds of having long sleep duration at follow-up, while greater educational attainment and weekly physical activity were both associated with reduced the odds becoming a long sleeper. Other than greater baseline age, the only factor related to higher odds of becoming a short sleeper was concurrent stomach/duodenal ulcer at follow-up. Long sleep duration among older adults may therefore reflect longstanding disease processes, whereas the etiology of short sleep may predominately involve factors other than those examined. Future research is needed to distinguish if/when long sleep duration serves the disease recovery process and when long sleep duration complicates disease and requires sleep medicine interventions.
Keywords: epidemiology, Singapore Chinese Health Study, aging, sleep, longitudinal
The role of reverse causality in the relationship between sleep duration and risk of developing serious chronic diseases remains the subject of lively debate (Holliday et al., 2013, Kurina et al., 2013, Grandner and Drummond, 2007). The relationship between sleep duration and future disease risk may be confounded by temporally antecedent effects of disease on sleep. In other words, sleep duration may be both a cause and consequence of ongoing disease process, rather than sleep duration necessarily conferring disease risk unidirectionally. Although systematic evidence already exists regarding the relationship between sleep and mortality (Cappuccio et al., 2010), relatively few prior studies have examined the determinants of changes to sleep in aging (Smagula et al., 2015).
Given that the global population of older adults is rapidly expanding (Cauley, 2013), longitudinal studies are needed to understand how commonly, and why, sleep duration changes in late-life. Identifying risk factors for the development of short or long sleep duration can help inform future interventions, potentially to curtail a viscous cycle wherein feedback between disease processes and sleep duration impact each other and health overall. Most existing longitudinal research examining changes to sleep in aging has focused on predictors of incident sleep complaints, rather changes to sleep duration (Smagula et al., 2015). One study that was not able to control for baseline sleep duration found that inflammatory marker levels predicted future long sleep duration (Dowd et al., 2011). Another study found chronic medical conditions predicted incident hypersomnia complaints (Roberts et al., 1999).
These prior findings are consistent with the notion that long sleep duration is a marker of pre-existing disease. However, no prior population-based, prospective study has directly tested whether chronic disease predicts future changes in self-reported sleep duration among older adults. If short or long sleep duration is marker of pre-existing disease, then longitudinal research should find increased risk for changes to sleep duration among individuals with disease. To test this hypothesis, we examined associations between demographic, lifestyle, and chronic disease histories with change in sleep duration within a large, population-based cohort of older adults living in Singapore.
Methods
Participants
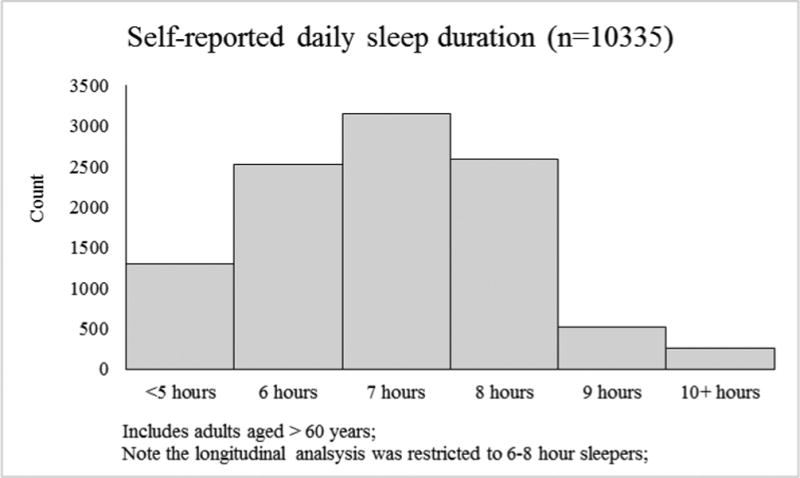
The baseline interview during the recruitment of participants for the Singapore Chinese Health Study (SCHS) was conducted from 1993-1998. The Singapore Chinese Health Study was designed to assess associations between diet and cancer risk and details of recruitment have been described previously (Hankin et al., 2001). The current report is a secondary data analysis. Two follow-up interviews were conducted between 1999 and 2004, and between 2006 and 2010, respectively. At the baseline and second follow-up interviews, self-reported daily sleep duration was assessed. The current report includes only older adults (≥60 years of age at baseline) that provided information regarding self-reported sleep duration at both baseline and the second follow-up interviews (n=10,335) and had normative (6-8 hour) baseline daily sleep duration (n=8265). We defined normative sleep duration as 6-8 hours based on the older adult sample's distribution (see Figure 1) and published recommendations for older adults (Hirshkowitz et al., 2015). All participants provided informed consent and the study was approved by the institutional review boards of the National University of Singapore.
Figure 1. Self-reported daily sleep duration at baseline among older adults in the Singapore Chinese Health Study.
Measures
Sleep duration
A single question administered at baseline and the second follow-up interviews, respectively, was used to assess self-reported daily sleep duration and its change. Participants were asked: “On the average, during the last year, how many hours in a day did you sleep (including naps)?” Response options were: “5 hours or less,” “6 hours,” “7 hours,” “8 hours,” “9 hours,” or “10 hours or more.” Change in sleep was categorized as: incident short sleep duration (defined as sleep duration of <6 hours at the second follow-up), incident long sleep duration (defined as having >8 hours at the second follow-up) and stable sleep duration (maintaining 6 to 8 hours of sleep).
Predictors of change in sleep duration
We examined all available health status and lifestyle factors that, based on clinical reasoning and prior research (see introduction), might predict changes to sleep duration. These included self-reported: age, gender, birth place, educational attainment, marital status, body mass index, cigarette smoking, weekly alcohol consumption, and physical activity. These factors were categorized as in Table 1 or otherwise expressed continuously. Self-reported medical diagnoses of the following chronic diseases/conditions were obtained at baseline and both follow-up visits: stomach/duodenal ulcer, high blood pressure, heart attack/angina, stroke, and diabetes; history of these diseases was examined at three-level variable indicating the disease/condition was: never indicated as present, prevalent at baseline, or newly reported at either follow-up interview. Arthritis was assessed only at the first and second follow-up interview, and was examined as either never indicated, present at follow-up one, or newly present at follow-up two. Ascertainment of incident cancer cases among cohort participants was via record linkage with the databases of the nationwide Singapore Cancer Registry (2002). Cancer status was defined as absent, prevalent at baseline, or incident cancer that was diagnosed after the date of baseline interview. Hip fractures were ascertained via linkage with the nationwide hospital discharge summary database (Dai et al., 2014), and were defined as never present, prevalent at baseline, or incident between baseline and follow-up two.
Table 1. Distributions of lifestyle and demographic characteristics among older adults who completed follow-up interviews (n=8265), The Singapore Chinese Health Study 1993-2010.
| Characteristics | ||
|---|---|---|
| Category | Mean (SD) or Percent (N) | |
| Age | 64.59 (3.69) | |
| Gender female | 58.95 (4872) | |
| Birth place | ||
| Singapore | 64.77 (5353) | |
| Malaysia | 12.93 (1069) | |
| China, Hong Kong, Macau, Taiwan | 20.90 (1727) | |
| Other parts of the world | 1.4 (116) | |
| Educational attainment | ||
| None | 39.87 (3295) | |
| Primary school | 44.49 (3677) | |
| Secondary school | 13.16 (1088) | |
| Junior college | 1.81 (150) | |
| University/technical school | 0.67 (55) | |
| Marital Status | ||
| Married | 76.45 (6319) | |
| Separated or divorced | 1.58 (131) | |
| Widowed | 19.42 (1605) | |
| Never married | 2.54 (210) | |
| Body mass index, mean (SD) | 23.13 (3.22) | |
| Cigarette smoking | ||
| Never | 68.68 (5676) | |
| Former | 14.79 (1222) | |
| Current | 16.54 (1367) | |
| Alcohol consumption (drinks per week) | 0.60 (2.91) | |
| Moderate physical activity (per week) | ||
| <30 minutes | 67.51 (5580) | |
| 0.5-3 hours | 18.20 (1504) | |
| 4+ hours | 14.29 (1181) |
Statistical Analysis
For descriptive purposes, the prevalence of baseline sleep duration is presented from the entire sample (not restricted to 6-8 hour sleepers) of SCHS participants aged >60. All predictor variables were examined in separate multinominal logistic regression models, and the outcomes of developing short sleep duration and long sleep duration at the follow-up were both compared with the “stable sleep duration” reference group. Crude models were adjusted for age and gender only, and crude associations that achieved p<0.15 were selected into a maximum model. Backwards elimination was applied to select only predictors retaining p<0.15 in the maximum model. In this final model, we defined the statistical significance of predictors as p<0.05. Sensitivity analyses were conducted adjusting for baseline sleep duration (results were not altered and are therefore not reported).
Results
The median daily sleep duration at baseline among all older adult SCHS participants was 7 hours (6-8 hour interquartile range). Most participants (n=8265/10335, 79%) reported 6-8 hours of daily sleep (Figure 1). Demographic, lifestyle, and chronic disease characteristics of these “normative,” 6-8 hour sleepers are shown for descriptive purposes (Tables 1 and 2).
Table 2. The prevalence of chronic disease history among participants who completed two follow-up interviews (n=8265), The Singapore Chinese Health Study 1993-2010.
| Percent (N) | ||
|---|---|---|
|
|
||
| Stomach/duodenal Ulcer | ||
| Absent | 89.62 (7407) | |
| Baseline | 4.46 (369) | |
| New report at FUP 1/2 | 5.92 (489) | |
| High blood pressure | ||
| Absent | 33.60 (2777) | |
| Baseline | 27.71 (2290) | |
| New report at FUP1/2 | 38.69 (3198) | |
| Heart attack/angina | ||
| Absent | 85.92 (7101) | |
| Baseline | 4.97 (411) | |
| New report at FUP 1/2 | 9.11 (753) | |
| Stroke | ||
| Absent | 92.27 (7626) | |
| Baseline | 1.26 (104) | |
| New report at FUP 1/2 | 6.47 (535) | |
| Diabetes | ||
| Absent | 75.56 (6245) | |
| Baseline | 9.46 (782) | |
| New report at FUP 1/2 | 14.98 (1238) | |
| Arthritis* | ||
| Absent | 75.91 (6230) | |
| Prevalent at FUP 1 | 13.37 (1097) | |
| New report at FUP2 | 10.72 (880) | |
| Cancer | ||
| Absent | 89.62 (7407) | |
| Prevalent | 3.10 (256) | |
| Incident | 7.28 (602) | |
| Hip fracture | ||
| Absent | 96.86 (8014) | |
| Baseline | 0.19 (16) | |
| Incident | 2.84 (235) |
FUP, follow-up wave;
numbers do not sum to total due to missing <1% of the data;
At follow-up, most of these individuals remained in the 6-8 hour daily sleep duration range (n=4593/8265, 55.57%). However, a large portion developed long (> 8 hour) sleep duration (n=2979, 36.04%), and a smaller but substantial group became short (<6 hour) sleepers over time (n=693, 8.38%).
The final multivariable model (Table 3) yielded adjusted odds ratios for becoming short and long sleepers (relative to remaining a stable “normative” sleeper). Each standard deviation higher baseline age was associated with 26% greater odds of becoming a long sleeper, and 11% higher odds of becoming a short sleeper. Educational attainment was inversely related to odds of becoming a long sleeper; ORs (95% CIs) of becoming a long sleeper for primary school, secondary school, junior college, and university/technical school were 0.81 (0.72-0.90), 0.75 (0.64-0.88), 0.54 (0.36-0.80), and 0.50 (0.26-0.96), respectively, compared with no formal schooling (P for trend=0.0003) after adjustment for age, physical activity, and history of chronic diseases.. Having any level of weekly moderate physical activity greater than 30 minutes per week was protective against becoming a long sleeper.
Table 3.
Adjusted odds ratios (95% confidence interval) of becoming shorter or longer sleep according to different levels of selected characteristics among participants who completed two follow-up interviews (n=8265), The Singapore Chinese Health Study 1993-2010
| Characteristic and levels | Incident Short (<6 hours) | Incident Long (>8 hours) | |
|---|---|---|---|
|
|
|||
|
|
|||
| Age, per SD (3.7 years) | 1.11 (1.02-1.20) | 1.26 (1.21-1.32) | |
| Gender female (vs. male) | 1.07 (0.89-1.29) | 0.94 (0.84-1.05) | |
| Educational Attainment | |||
|
|
|||
| No education | 1.00 | 1.00 | |
| Primary school | 0.86 (0.71-1.04) | 0.81 (0.72-0.90) | |
| Secondary school | 0.77 (0.58-1.01) | 0.75 (0.64-0.88) | |
| Junior college | 1.03 (0.59-1.79) | 0.54 (0.36-0.80) | |
| University/technical school | 0.48 (0.15-1.58) | 0.50 (0.26-0.96) | |
| Duration of moderate-level activity per week | |||
|
|
|||
| None | 1.00 | 1.00 | |
| 0.5-3 hours | 0.85 (0.68-1.06) | 0.74 (0.65-0.84) | |
| 4+ hours | 1.14 (0.91-1.43) | 0.83 (0.72-0.95) | |
| Chronic Disease | |||
|
|
|||
| Stomach/duodenal ulcer baseline (vs. none) | 1.03 (0.70-1.51) | 0.88 (0.70-1.11) | |
| Stomach/duodenal ulcer FUP (vs. none) | 1.42 (1.05-1.93) | 0.91 (0.74-1.11) | |
| Stroke baseline (vs. none) | 1.48 (0.74-2.95) | 1.63 (1.08-2.47) | |
| Stroke FUP (vs. none) | 1.09 (0.77-1.55) | 1.68 (1.39-2.02) | |
| Diabetes baseline (vs. none) | 0.96 (0.72-1.28) | 1.33 (1.13-1.56) | |
| Diabetes FUP (vs. none) | 0.98 (0.78-1.23) | 1.19 (1.04-1.36) | |
| Baseline cancer (vs. none) | 1.19 (0.75-1.86) | 1.29 (0.99-1.69) | |
| Incident cancer (vs. none) | 0.88 (0.63-1.23) | 1.24 (1.04-1.48) | |
| Baseline hip fracture (vs. none) | 0.79 (0.10-6.32) | 1.29 (0.47-3.58) | |
| Incident hip fracture (vs. none) | 0.89 (0.51-1.54) | 1.52 (1.16-2.00) | |
FUP, reported at follow-up interview; Analytic sample restricted to normative (6-8 hour) sleepers at study baseline, therefore the adjusted odds ratio estimates represent the odds of changing from normative (6-8 hour sleep) at baseline to either short and long sleep duration at FUP, compared with the referent group who remained 6-8 hour sleepers at FUP;
The history of stroke, whether occurred remotely or recently prior to the second follow-up interview when the sleep duration was reassessed, was associated with a statistically significant approximately 65% higher odds of becoming a long sleeper. Prevalent diabetes and new reports of diabetes were associated with statistically significant 33% and 19%, respectively, higher odds of becoming a long sleeper. Recent occurrence of cancer or hip fracture were also associated with statistically significantly increased odds of becoming a long sleeper. Besides age, the only factor examined that was significantly associated with odds ratio of becoming a short sleeper was having a stomach/duodenal ulcer during follow-up.
Discussion
To our knowledge, our study is the first to examine associations between chronic disease and lifestyle factors with longitudinal change in sleep-duration among older adults. In our study, the majority of older adults slept 6-8 hours daily, and most of these participants continued to report a daily sleep duration in this range over twenty years later. Consistent with prior reports linking chronic diseases to future sleep disturbance (Smagula et al., 2015), we found that diseases of aging (including stroke, diabetes, cancer, and hip fracture) may confer risk for long sleep duration. The observed associations persisted after adjusting for baseline sleep hours, implying that these health factors, and not baseline sleep duration, accounted for change in sleep duration over time. Considering that 36% of the study population became long sleepers over 12.7 years of follow-up, aging may be predominately associated with a lengthening of daily sleep duration, potentially in response to ongoing chronic-disease processes increasing homeostatic burden and sleep drive.
The strong associations observed between a history of stroke and future long sleep duration is biologically plausible. Cerebrovascular damage incurred via stroke may directly lead to an increasing homeostatic load/sleep drive and/or damage to the central circadian clock (required to oppose sleep drive and maintain wakefulness). Interestingly, the association of diabetes and future long sleep appeared somewhat more robust when diabetes was present at baseline (vs. new onset during the follow-up period). This difference in strength of association (with long sleep) between prevalent and new cases of diabetes may suggest the relationship between diabetes and changes in sleep depends on the length of illness. Incident cancer may be associated with future long sleep duration as a consequence of increased homeostatic burden caused by either the disease or treatment. Alternatively or in addition, the identified predictors of change in sleep disturbances may act as markers of underlying, unmeasured processes.
Rather than directly causing long sleep duration, low level of education, lack of physical activity, and recent occurrence of hip fracture may be general markers of the poor health determinants of long sleep duration. Interestingly, none of the chronic diseases or lifestyle factors investigated predicted becoming a short sleeper except for individuals with newly diagnosed stomach/duodenal ulcers, which may directly shorten sleep via stomach pain and discomfort causing restlessness. Patients with stomach/duodenal ulcers should be aware that shortened sleep duration may result from their condition, and clinical efforts to prevent sleep curtailment among these patients may be needed to prevent short sleep from further complicating metabolic disease (Holliday et al., 2013).
Several limitations should be noted. The current work can only speculate on the mechanisms through which the above mentioned chronic diseases are linked to changes in sleep. Future work with repeated measures of putative mediators between these diseases and sleep duration is required to further isolate pathways by which sleep patterns change through the biological aging process. Depression may be among the primary determinants of new sleep disturbances among older adults (Smagula et al., 2015), however our study did not include assessments of psychiatric disorders or mood. Our sleep outcome was defined by self-report of total daily sleep duration; lacking objective measures, our study cannot determine if participants slept longer, albeit less efficiently. Estimating total sleep duration over the past year (as attempted with our sleep measure) is likely very challenging among older adults in whom mild cognitive impairment and dementia become prevalent (Kim et al., 2011); it is likely that participants reported their most recent, rather than average yearly sleep duration. Further, our sleep measure included total daily (rather than nightly) sleep duration, and in older adults sleep consolidation may give way to common daytime napping; therefore, it is impossible for our analysis to determine whether the observed changes in sleep-duration represent changes to the duration of nighttime or daytime sleep
Future studies are warranted to examine changes to multiple aspects of sleep (e.g. naps, diurnal rhythmicity, fragmentation, etc.) using objective assessments. In terms of external validity, our findings can likely only be generalized to older Singaporeans who survive into their 80's. Note that while the proportion with formal education appears low, this does not indicate a biased selection process/related generalizability limitations. Schools in Singapore closed during World War II, and it was not until the development of Singapore's national economy that universal education policies came into effect; therefore, the prevalence of educational attainment observed is reasonably generalizable to our target population. Nevertheless, as in all aging research, the sample likely reflects a healthy survivor bias; because participants who died prior to follow-up are more likely to have changed sleep duration, we may have over-estimated the longitudinal stability of sleep duration.
In conclusion, our results provide evidence that self-reported long sleep duration is, at least in part, a marker of longstanding, antecedent disease processes. In a previous analysis of data from the Singapore Chinese Health Study, short and long sleep duration predicted cardiovascular mortality (Shankar et al., 2008); despite adjustments for several health measures, this prior report concluded unmeasured disease processes may have still confounded the association between sleep duration and mortality. The current study provides evidence that, indeed, ongoing disease processes can cause both long sleep duration and future mortality risk. While not addressed by our study, our results also beg the question of whether (and in which cases) long sleep duration serves an adaptive purpose, or whether long sleep duration is an unwanted disease complication that does contribute to worsening pathology. If the latter situation is the case, this vicious cycle of dysregulation of sleep regulation and normal physiology (i.e. in the metabolic and vascular systems) would call for a greater role of sleep medicine in managing chronic diseases in aging.
References
- Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB. Cancer incidence in five continents. Volume VIII: IARC scientific publications; pp. 2002pp. 1–781. [PubMed] [Google Scholar]
- Cappuccio FP, D'elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–92. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauley J. The Demography of Aging. In: A C, NEWMAN J, editors. The Epidemiology of Aging. Vol. 2013. Springer; New York: pp. 3–14. [Google Scholar]
- Dai Z, Wang R, Ang LW, Low YL, Yuan JM, Koh WP. Protective effects of dietary carotenoids on risk of hip fracture in men: the Singapore Chinese Health Study. J Bone Miner Res. 2014;29:408–17. doi: 10.1002/jbmr.2041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowd JB, Goldman N, Weinstein M. Sleep duration, sleep quality, and biomarkers of inflammation in a Taiwanese population. ANN EPIDEMIOL. 2011;21:799–806. doi: 10.1016/j.annepidem.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1:40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- Grandner MA, Drummond SPA. Who Are the Long Sleepers? Towards an Understanding of the Mortality Relationship. SLEEP MED REV. 2007;11:341–60. doi: 10.1016/j.smrv.2007.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin JH, Stram DO, Arakawa K, et al. Singapore Chinese Health Study: development, validation, and calibration of the quantitative food frequency questionnaire. Nutr Cancer. 2001;39:187–95. doi: 10.1207/S15327914nc392_5. [DOI] [PubMed] [Google Scholar]
- Holliday EG, Magee CA, Kritharides L, Banks E, Attia J. Short Sleep Duration Is Associated with Risk of Future Diabetes but Not Cardiovascular Disease: a Prospective Study and Meta-Analysis. PLoS ONE. 2013;8:e82305. doi: 10.1371/journal.pone.0082305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim KW, Park JH, Kim MH, et al. A nationwide survey on the prevalence of dementia and mild cognitive impairment in South Korea. J Alzheimers Dis. 2011;23:281–91. doi: 10.3233/JAD-2010-101221. [DOI] [PubMed] [Google Scholar]
- Kurina LM, Mcclintock MK, Chen JH, Waite LJ, Thisted RA, Lauderdale DS. Sleep duration and all-cause mortality: a critical review of measurement and associations. ANN EPIDEMIOL. 2013;23:361–70. doi: 10.1016/j.annepidem.2013.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts RE, Shema SJ, Kaplan GA. Prospective data on sleep complaints and associated risk factors in an older cohort. Psychosom Med. 1999;61:188–96. doi: 10.1097/00006842-199903000-00011. [DOI] [PubMed] [Google Scholar]
- Shankar A, Koh WP, Yuan JM, Lee HP, Yu MC. Sleep Duration and Coronary Heart Disease Mortality Among Chinese Adults in Singapore: A Population-based Cohort Study. Am J Epidemiol. 2008;168:1367–73. doi: 10.1093/aje/kwn281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smagula SF, Stone KL, Fabio A, Cauley JA. Risk factors for sleep disturbances in older adults: evidence from prospective studies. SLEEP MED REV. 2015 doi: 10.1016/j.smrv.2015.01.003. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]


