Abstract
This study aims to evaluate the effect of septal correction on the blood pressure (BP) of patients with symptomatic nasal septal deviation and to assess whether a positive association exists between deviated nasal septum and hypertension. A prospective observational clinical study was conducted at Kempegowda Institute of Medical Sciences, Bangalore. Hundred adults, aged 18–40 years, with symptomatic nasal septal deviation, newly detected untreated hypertension (mean BP ≥140/90 mmHg), undergoing submucosal resection of the septum and submucosal diathermy of hypertrophied inferior turbinate (when present), were included. Postoperative follow up for ENT examination and BP measurement was done at 1, 6 and 12 months. Seventy five males and 25 females met the inclusion criteria. 48 % were aged 31–35 years (mean = 31.83 ± 5.19 years). 71 % had anterior septal deviation, 13 % posterior deviation and 16 % a combination of both. Preoperatively, mean systolic blood pressure was 141.82 ± 1.70 mmHg and mean diastolic blood pressure was 91.04 ± 1.21 mmHg, which postoperatively decreased by 10–12 mmHg and 4–5 mmHg respectively. 79 % showed a significant (P < 0.001) decrease in BP postoperatively. 13 % showed no change in BP, of which 53.8 % had posterior deviation, demonstrating a significant association (P < 0.001) between type of deviation and response to surgery. In 8 %, a rise in BP over the follow up period was seen; of these, 62.5 % were aged 36–40 years, indicating a significant association (P < 0.001) between age and BP. Surgical correction of septal deviation is thus effective in controlling the BP of patients with anterior deviation, aged <35 years.
Keywords: Nasal septum, Nasal obstruction, Deviation, Hypertension, Blood pressure
Introduction
The nasal septum is the bone and cartilage of the nose that separates the nasal cavity into two passages [1]. Aside from being a key support mechanism of the nose and a major determinant of its shape, the space between the septum and the lateral walls of the nasal cavity regulates nasal airflow and respiration [2].
The nose normally accounts for approximately half of the respiratory resistance to airflow and the nasal valve is responsible for at least half of the nasal resistance to airflow [1]. Nasal septum deviation is one of the most frequent reasons for nasal obstruction presented with a reduction in nasal airflow and chronic mucosal irritation [3]. This condition increases upper airway resistance and has been shown to decrease oxygen saturation and increase the arterial carbon dioxide content. The response to hypoxia and hypercarbia is vasoconstriction induced arterial resistance [1]. Thus abnormal upper airway resistance can play a role in the development of hypertension [4].
Hypertension is a major contributing factor to the current epidemic of cardiovascular disease in India [5]. The current definition and classification of hypertension, based on the Seventh report of the Joint National Committee on Prevention, detection, evaluation and treatment of high blood pressure (JNC 7), specifies the threshold for defining high blood pressure (BP) as ≥140/90 mmHg [6]. A high and increasing prevalence of hypertension in both rural and urban areas of India has been reported in recent studies. Detection and effective management of hypertension decreases the risk of stroke, myocardial infarction, chronic kidney disease and heart failure [5].
In literature, the effect of chronic upper respiratory obstruction such as hypertrophied tonsils, adenoid vegetation and nasal polyposis on cardiopulmonary system has been studied, but the effect of pure nasal deviation on cardiac system has not been precisely investigated [1].
This study was therefore undertaken with the aims of evaluating the effect of submucosal resection (SMR) of the nasal septum on the BP of patients with nasal septal deviation, and to assess whether a positive association exists between deviated nasal septum and hypertension.
Materials and Methods
A prospective observational clinical study was conducted from October 2012 to May 2014 at the Department of ENT, Kempegowda Institute of Medical Sciences, Bangalore with the approval of the Institute ethics committee and in accordance with ethical standards.
Hundred consenting adults of both sexes aged 18–40 years, suffering from symptomatic nasal septal deviation and newly detected hypertension (mean BP ≥140/90 mm Hg), undergoing SMR of the deviated septum, were included in the study from October 2012 to May 2013.
Those who suffered either preoperatively or during the postoperative follow up period, from other nasal conditions (allergic rhinitis, acute or chronic infection of the nose or paranasal sinuses, polypi, middle turbinate hypertrophy, choncha bullosa, septal perforation, septal haematoma, synechiae, granulomatous disease, sinonasal malignancies, nasopharyngeal mass), had undergone previous nasal or septal surgery, received head and neck radiotherapy, had craniofacial syndrome, other systemic conditions such as endocrine disorders (hypothyroidism, acromegaly), uncontrolled asthma, other lung pathology, pregnancy, obstructive sleep apnoea or it’s risk factors such as adenoid hypertrophy or enlarged tonsils, were known hypertensives or on any antihypertensive medication, had other risk factors for hypertension such as smoking, chewing tobacco, consumption of alcohol, Body mass index ≥25, central obesity i.e. waist circumference greater than 90 cm in men and 80 cm in women, high dietary salt intake, low fruit and vegetable intake, sedentary lifestyle, family history of hypertension or cardiovascular disease, or attrition to follow up or death from a cause not related to the study parameters in the observation period, were excluded from the study.
After a detailed history was taken, preoperative evaluation was done by clinical examination and nasal endoscopy. Nasal septal deformities were classified according to the Dreher scale (0 = none i.e. no deviation, 1 = mild deviation i.e. deviation less than half of the total distance to the lateral wall, 2 = moderate deviation i.e. deviation greater than half of the total distance to the lateral wall but not touching it, 3 = severe deviation i.e. deviation touching the lateral wall). Compensatory inferior turbinate hypertrophy, when present, was noted.
BP was measured in a well rested patient, in supine position, in the right upper limb, using a standard mercury sphygmomanometer, on three separate occasions, with a minimum of 10 min between recordings. The average of these three readings was then tabulated. “Hypertension” was defined as average systolic blood pressure (SBP) ≥140 mm Hg and diastolic blood pressure (DBP) ≥90 mm Hg.
Routine preoperative work up was carried out. All patients were given Amlodipine 5 mg orally on the night before the surgery and morning of the surgery in order to lower the BP and thereby minimise intraoperative bleeding.
SMR of the deviated nasal septum was performed in all cases. In patients who had compensatory inferior turbinate hypertrophy, submucosal diathermy of the hypertrophied turbinate was also done.
Post operative care included oral antibiotic and analgesic for 1 week and antihistamine for 10 days. Following nasal pack removal, saline nasal douching was advised for 2 weeks.
Postoperatively, patients were followed up after 1 month, 6 months and at the end of 1 year. On each of these visits, general and ENT examination were carried out and BP was recorded (average of three readings on each visit, as was done preoperatively).
Postoperatively, hypertension was considered “controlled” in patients who had a mean SBP <140 mm Hg and mean DBP <90 mm Hg on follow up, therefore requiring no further intervention. Patients in whom SBP was ≥140 mm Hg and/or DBP ≥90 mm Hg, were considered as “uncontrolled” hypertensives and thus initiated on medical treatment for hypertension.
Results
The mean age of the study patients (75 males and 25 females) was 31.83 ± 5.19 years, with a range of 20–39 years. Age distribution of the study patients was as follows: 48 % were aged between 31 to 35 years, 27 % were aged 26–30 years, 14 % were aged 20–25 years and 11 % were 36–40 years of age.
Subjects suffered from symptoms of nasal septal deviation for a duration ranging from 1 to 9 years, with a mean of 3.9 ± 1.74 years. 64 % were symptomatic for 3–5 years, 22 % for 1–2 years and 14 % for 6–10 years.
71 % of patients had anterior deviation of septal cartilage, 13 % had posterior deviation and 16 % had a combination of both anterior and posterior deviation of the nasal septum.
Mild septal deviation was seen in 22 % of patients, moderate deviation in 63 % and severe deviation in 15 %. 24 % of patients had compensatory hypertrophy of the inferior turbinate (8 % on the right and 16 % on the left side).
Preoperatively, mean SBP was 141.82 ± 1.70 mm Hg and mean DBP was 91.04 ± 1.21 mm Hg. Post submucous resection of septum, hypertension was “controlled” in 79 % of patients who showed a strongly significant (P < 0.001) decrease in BP i.e. a 10–12 mm Hg decrease in SBP and 4–5 mm Hg decrease in DBP. (Table 1, Table 2).
Table 1.
Changes in systolic blood pressure
| Systolic blood pressure (mm Hg) | Min–max | Mean ± SD | Comparison with pre submucosal resection of septum | |||
|---|---|---|---|---|---|---|
| Difference | t value | P value | ||||
| Pre submucosal resection of septum | 140.00–146.00 | 141.82 ± 1.70 | – | – | – | |
| Post submucosal resection of septum | ||||||
| 1 month | 123.00–145.00 | 130.90 ± 6.31 | 10.920 | 18.040 | <0.001* | |
| 6 months | 121.00–148.00 | 129.13 ± 7.75 | 12.690 | 16.799 | <0.001* | |
| 12 months | 120.00–152.00 | 128.93 ± 8.60 | 12.890 | 15.336 | <0.001* | |
* Strongly significant
Table 2.
Changes in diastolic blood pressure
| Diastolic blood pressure (mm Hg) | Min–max | Mean ± SD | Comparison with pre submucosal resection of septum | |||
|---|---|---|---|---|---|---|
| Difference | t value | P value | ||||
| Pre Submucosal Resection of septum | 90.00–94.00 | 91.04 ± 1.21 | – | – | – | |
| Post Submucosal Resection of septum | ||||||
| 1 month | 82.00–95.00 | 86.05 ± 3.25 | 4.990 | 17.654 | <0.001* | |
| 6 months | 78.00–97.00 | 85.09 ± 4.16 | 5.950 | 15.662 | <0.001* | |
| 12 months | 78.00–99.00 | 85.05 ± 4.85 | 5.990 | 13.330 | <0.001* | |
* Strongly significant
In 21 % of the study participants, hypertension remained “uncontrolled” following surgical correction of nasal obstruction. On further evaluation of these patients, it was observed that 13 % showed no change in BP post operatively and 8 % of patients showed an increase in BP over the 1 year follow up period.
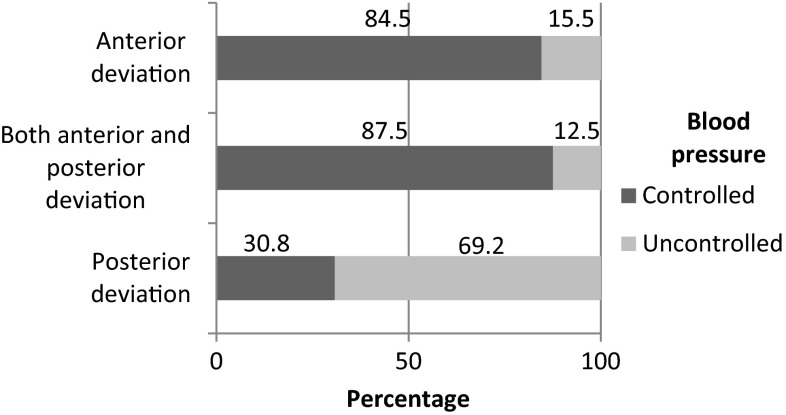
A statistically significant association (P < 0.001) was seen between type of nasal septal deviation and response of BP to septal correction, with anterior septal deviation showing the maximum response. Of the 13 % of patients who showed no difference between pre and postoperative BP values, 53.8 % had posterior deviation (Fig 1).
Fig. 1.
Type of septal deviation and response of blood pressure to septal correction
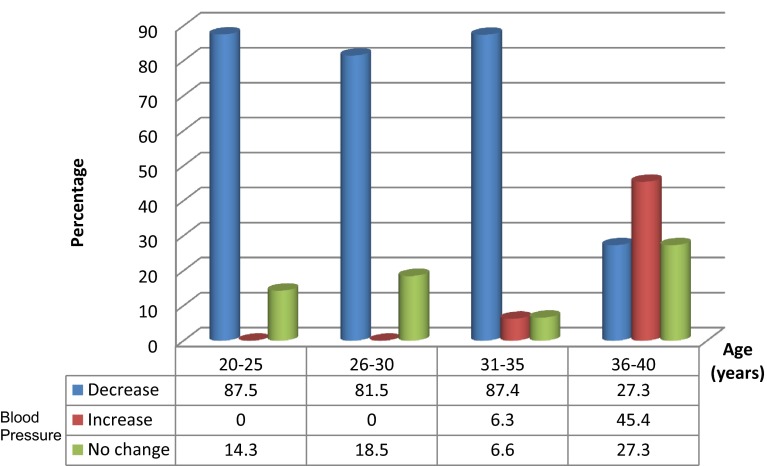
Similarly, a strongly significant association was found between BP and age (P < 0.001) as 62.5 % of the patients showing a rise in BP over the postoperative follow up period were aged 36–40 years (Fig 2).
Fig. 2.
Age distribution of patients studied according to changes in blood pressure
No statistically significant association (P > 0.10) was seen between the duration of symptoms of septal deviation and BP (P = 0.204), and similarly between gender and BP (P = 0.688).
No intraoperative or immediate or delayed postoperative complications such as septal haematoma, septal perforation, synechiae, deformity, etc. were seen in any of the study subjects over the follow up period.
Discussion
The nasal septum is a midline support structure of the nasal cavity. Deviation of the nasal septum is a common structural cause of nasal obstruction [2] and one of the most common causes of upper respiratory tract obstruction. Deviated nasal septum with nasal obstruction has profound effects on the body as a whole [7]. Nasal obstruction disrupts the physiological ventilation of the lung by obstructing airflow [1]. This reduces oxygenation in the lungs, and causes an increased respiratory and heart rate. Moreover, an increased respiratory rate does not allow sufficient gas exchange in patients with deviated nasal septum. Mechanical upper airway obstruction with nasal septal deviation can lead to hypoxia, hypercapnia, and significant changes in intrathoracic pressure. All these factors may affect sympathetic, parasympathethic activation and may also affect cardiac autonomic responses [7]. Sympathetic stimulation increases heart rate. The autonomic nervous system control areas of breathing and heart are located in the brainstem anatomically close to each other and there is a continuous interaction between these areas [8]. As a result, deviated nasal septum patients can be predisposed to several pulmonary and cardiovascular disorders [7].
Changes in blood carbon dioxide are supposed to affect vessels both directly and by way of the vasomotor centres. Actions are thought to be opposite in direction, central effect being the stronger, i.e. a high carbon dioxide level causes an overall vasoconstriction because of its effect on the vasomotor centres, even though the direct action is to dilate vessels. Thus breathing carbon dioxide increases arterial BP [9].
Patients with severe septal deviation have chronic mucosal contact and mucosal irritation occurs by stimulation of afferent neurons of trigeminal nerve which induces a complex physiological response consisting of apnoea, bradycardia, vasoconstriction, and inhibition of respiratory drive, which involves the integration of afferent impulses, carried on fibers innervating somatic receptors, chemoreceptors, and baroreceptors [3].
Hypertension is a progressive cardiovascular syndrome arising from complex and interrelated etiologies. Hypertension is diagnosed when an individual crosses an established BP threshold. Throughout most of the world today, “high BP” is defined as elevation in BP ≥140/90 mm Hg [6], which was the value used in our study to define hypertension. Recent studies among Indians have shown a high prevalence of hypertension. Over one-fifth of Indian adults have hypertension. Detection and effective management of hypertension decreases the risk of stroke, myocardial infarction, chronic kidney disease and heart failure [5].
Adults aged below 40 years were included in our study, as literature revealed that the risk of essential hypertension increases beyond this age [6]. Only patients with symptomatic nasal obstruction were included in our study, as studies have shown that anterior and posterior anatomic characteristics were associated with the subjective severity of nasal obstruction [10]. Studies have revealed that physical examination from nasal endoscopy or anterior rhinoscopy is an accurate method of diagnosing patients with nasal septal deviation requiring septal surgery [2]. It has also been found that ipsilateral rhinoscopic grading and resistance values were directly related and application of Ohm’s law for parallel resistors to rhinoscopic grading also showed a direct relationship with measured total nasal resistance [11]. Thus participants in our study were examined and the septal deviation evaluated and graded clinically. Rhinomanometry has been shown to be of limited diagnostic value in the clinical setting due to its ability to only diagnose major septal deviations in the anterior region [2] and was thus not performed in our study.
Septal correction with reduction of hypertrophic nasal turbinates is considered standard treatment [12]. SMR has been shown to be effective in reducing nasal resistance in patients with uncomplicated deviated nasal septum [13]. Submucosal diathermy is shown to be a safe, effective procedure for improving nasal breathing in patients with chronic obstructive inferior turbinates, both on a short term and long term basis [14]. Thus our study followed surgical correction of nasal septum by SMR, along with submucosal diathermy of the hypertrophied inferior turbinate when present. Lack of a control group is because there is no effective alternate treatment for deviated nasal septum, and ethically a placebo treatment could not be carried out due to accepted treatment standards for septal deviation.
A study by Nakata S. et al. demonstrated a significant decrease in nasal resistance and a significant increase in lowest SpO2 following SMR of deviated nasal septum [15]. Autonomic dysfunction that occured due to nasal septal deviation was found to decrease after surgical correction of the deviated septum in a study conducted by Yuritas et al. [7]. Comparable results were noted in our study, as a significant number of patients (79 %) benefitted from SMR, bringing their mean BP to normal values postoperatively.
The nasal valve is responsible for at least half of nasal resistance to airflow [1]. Anterior part of the nose is thus most susceptible and differences of one millimetre in lumen can be critical [16]. A study by Garcia et al. concluded that the posterior nasal cavity can accommodate significant septal deviations without a substantial increase in airway resistance. In contrast, a deviation in the nasal valve region more than doubled nasal resistance. These findings are in agreement with rhinomanometry literature and with the observation that patients with anterior septal deviations benefit the most from septal correction [17]. These findings concurred with the results of our study as over 80 % of our patients with pure anterior deviation and combined type of deviation showed control of BP following surgical correction nasal septum, whereas only 30.8 % of those with pure posterior deviation had their BP controlled postoperatively.
Stamler et al. demonstrated a positive relationship between age and systolic pressure in their study, as a more rapid increase in BP was seen in older subjects [18]. Similarly, in our study, of the 8 % of individuals who showed a gradual rise in BP in the postoperative follow up period, 62.5 % were aged between 36 to 40 years, indicating a significant association between higher age and hypertension not amenable to surgical intervention.
Conclusion
Surgical correction of the deviated nasal septum is safe and effective in controlling the BP of patients with anterior septal deviation, aged less than 35 years. Patients should therefore be encouraged to undergo septal correction for the prevention of cardio-pulmonary complications secondary to hypertension.
Compliance with Ethical Standards
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments and comparable ethical standards.
Conflict of interest
All authors declare that they have no conflict of interest.
References
- 1.Hassanpour SE, Moosavizadeh SM, Araghi MF, Eshraghi B. Pulmonary artery pressure in patients with markedly deviated septum candidate for septorhinoplasty. World J Plast Surg. 2014;3(2):119–121. [PMC free article] [PubMed] [Google Scholar]
- 2.Aziz T, Biron VL, Ansari K, Mir CF. Measurement tools for the diagnosis of nasal septal deviation: a systematic review. J otolaryngol Head Neck Surg. 2014;43(1):11. doi: 10.1186/1916-0216-43-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Acar B, Yavuz B, Karabulut H, Gunbey E, Babademez MA, Yalcin AA, et al. Sympathetic overactivity in patients with nasal septum deformities. Eur Arch Otorhinolaryngol. 2010;267:73–76. doi: 10.1007/s00405-009-1055-z. [DOI] [PubMed] [Google Scholar]
- 4.Guilleminault C, Stoohs R, Shiomi T, Kushida C, Schnittger I. Upper airway resistance syndrome, nocturnal blood pressure monitoring, and borderline hypertension. Chest. 1995;109(4):901–908. doi: 10.1378/chest.109.4.901. [DOI] [PubMed] [Google Scholar]
- 5.Moser KA, Agarwal S, Smith GD, Ebrahim S. Socio-demographic inequalities in the prevalence, diagnosis and management of hypertension in India: analysis of nationally representative survey data. PLoS ONE. 2014;9(1):e86043. doi: 10.1371/journal.pone.0086043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giles TD, Berk BC, Black HR, Cohn JN, Kostis JB, et al. Expanding the definition and classification of hypertension. J Clin Hypertens. 2005;7(9):505–512. doi: 10.1111/j.1524-6175.2005.04769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuritas V, Ozturk S, Apuhan T, Demirhan A, Tekelioglu UY, Akkaya A, et al. Pre and postoperative evaluation of cardiac autonomic function in patients with nasal septum deviation. Acta Medica. 2014;30:149. [Google Scholar]
- 8.Poyhonen M, Syvaoja S, Hartikainen J, et al. The effect of carbon dioxide, respiratory rate and tidal volume on human heart rate variability. Acta Anaesthesiol Scand. 2004;48:93–101. doi: 10.1111/j.1399-6576.2004.00272.x. [DOI] [PubMed] [Google Scholar]
- 9.Burnum JF, Hickam JB, McIntosh HD. The effect of hypocapnia on arterial blood pressure. Circulation. 1995;9(1):89–95. doi: 10.1161/01.CIR.9.1.89. [DOI] [PubMed] [Google Scholar]
- 10.Cho GS, Kim JH, Jang YJ. Correlation of nasal obstruction with nasal cross-sectional area measured by computed tomography in patients with nasal septal deviation. Ann Otol Rhinol Laryngol. 2012;121(4):239–245. doi: 10.1177/000348941212100409. [DOI] [PubMed] [Google Scholar]
- 11.Kensei N, Philip C, Roman C, et al. Nasal resistance, sensation of obstruction and rhinoscopic findings compared. Am J Rhinology. 1988;2(2):65–69. doi: 10.2500/105065888781693177. [DOI] [Google Scholar]
- 12.Enache A, Lieder A, Issing W. Nasal septoplasty with submucosal diathermy to inferior turbinate improves symptoms at 3 months postoperatively in a study of one hundred and one patients. Clin Otolaryngol. 2014;39(1):57–63. doi: 10.1111/coa.12219. [DOI] [PubMed] [Google Scholar]
- 13.Nofal F, Thomas M. Rhinomanometry evaluation of the effects of pre and postoperative SMR on exercise. J Laryngol Otol. 1990;104(2):126–128. doi: 10.1017/S0022215100112034. [DOI] [PubMed] [Google Scholar]
- 14.Irfan M, Jihan W. Submucosal diathermy for inferior turbinates hypertrophy—how long does it sustain? Int J Otorhinolaryngol. 2009;10(1):911–915. [Google Scholar]
- 15.Nakata S, Noda A, Yagi H, Yanagi E, Mimura T, Okada T, et al. Nasal resistance for determinant factor of nasal surgery in CPAP failure patients with obstructive sleep apnoea syndrome. Rhinology. 2005;44:296–299. [PubMed] [Google Scholar]
- 16.Cole P, Chaban R, Naito K, Oprysk D. The Obstructive nasal septum: effect of simulated deviations on nasal airflow resistance. Arch Otolaryngol Head Neck Surg. 1988;114(4):410–412. doi: 10.1001/archotol.1988.01860160054020. [DOI] [PubMed] [Google Scholar]
- 17.Garcia GJM, Rhee JS, Senior BA, Kimbell JS, et al. Septal deviation and nasal resistance:an investigation using virtual surgery and computational fluid dynamics. Am J Rhinol Allergy. 2010;24(1):e46–e53. doi: 10.2500/ajra.2010.24.3428. [DOI] [PubMed] [Google Scholar]
- 18.Stamler J, Berkson DM, Dyer A, Lepper MH, Lindberg HA, Paul O et al (1975) Relationship of multiple variables to blood pressure-findings from four Chicago epidemiologic studies. In: Epidemiology and control of hypertension, Miami, Symposia Specialists 307–356