Abstract
To compare the results, in terms of graft uptake and hearing improvement, of modified cartilage shield technique of tympanoplasty using either partial thickness tragal cartilage or full thickness tragal cartilage for type I procedures. 35 patients were included in group A where a partial thickness tragal cartilage was used and 27 patients included in group B where a full thickness tragal cartilage was used for modified cartilage shield tympanoplasty. Audiometry done at 4 months after surgery and the results compared. The graft take up rate for both these techniques is excellent. There had been no statistically significant difference in hearing gain between these two groups, except at 4,000 Hz, where hearing gain had been more in group A than group B with P value being 0.027. The modified cartilage shield tympanoplasty is a good technique for closure of tympanic membrane perforations. Hearing gain is very much similar between thin and thick cartilage groups, except at 4,000 Hz.
Keywords: Tympanoplasty, Thickness of cartilage, Modified cartilage shield, Frequency wise hearing gain
Introduction
The cartilage shield tympanoplasty has been advocated by many otologists for repair of tympanic membrane (TM) perforations. There has been concern regarding TM movements after placement of a cartilage piece medial to the ear drum remnant. Aarnisalo et al. [1] have concluded that the placement of cartilage on the medial surface of TM reduces the motion of the TM that apposes the cartilage. These obvious local changes occur even though the cartilage had little effect on the sound-induced motion of the stapes. Milewski [2] and Amedee et al. [3] have shown good graft take up and good hearing results by using cartilage as grafting material for tympanoplasty. Cavaliere et al. [4] have mentioned that tragal cartilage shield tympanoplasty is a reliable technique. The current study aims at comparing results of cartilage shield tympanoplasty (CST) by full thickness or by partial thickness cartilage graft where all ossicles are intact and mobile (type I).
Materials and Methods
A total of 62 patients more than 18 years of age were included in the study with inclusion criteria being a TM perforation, absence of retractions and a dry ear for at least 3 weeks. After thorough clinical examination, pure tone audiometry and microscopic examination, the surgical procedure scheduled. All procedures performed under general anesthesia. Post auricular incision used in all patients. The technique is the same as described by Duckert et al. [5] with the following changes: No notch made in the cartilage and perichondrium preserved on the lateral side of the cartilage. The tensor tympani tendon cut to make space in those cases where the handle was foreshortened or medially displaced. The cartilage piece was kept lateral to the incudo-stapedial (I-S) joint and medial to the handle of malleus. The anterior edge of the cartilage doesnot extend till the anterior annulus but lags about 1 mm behind. Thinning of the cartilage was done with the help of a No 15 knife by cutting the cartilage piece in a saggital plane, so the approximate thickness of the cartilage becomes less than half. Thinning was done in 35 of the cases. Temporalis fascia was kept lateral to the cartilage piece and lateral to the handle of malleus and medial to the annulus as an over—under grafting, as recommended by Kartush et al. [6]. Adequate gelfoam kept in middle ear to prevent medialisation. Anterior tucking of the fascia done in all cases in addition.
The ears were examined under microscope at 3 weeks, then at 6 weeks and then at 3 months post operatively after surgery. Figures 1 and 2 show post operative picture of tympanoplasty at 3 months after surgery, using partial thickness tragal shield and full thickness tragal shield. Pure tone audiometry was done at 4 months post operatively and the results were compared.
Fig. 1.
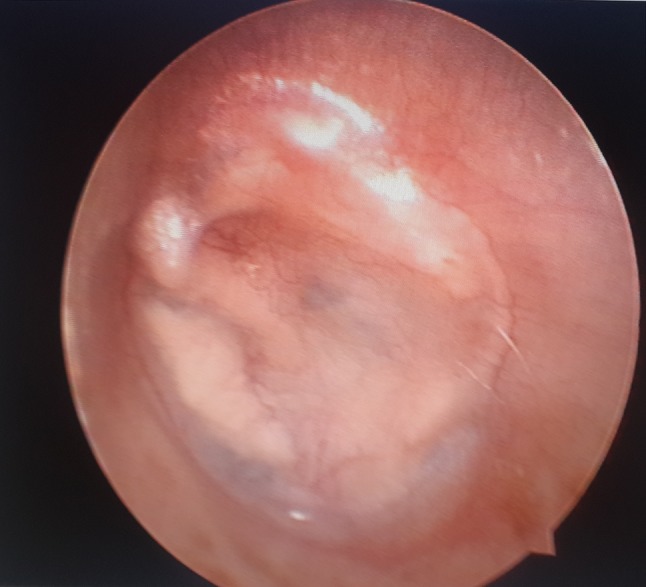
Post operative picture of partial thickness tragal cartilage shield procedure at 3 months
Fig. 2.
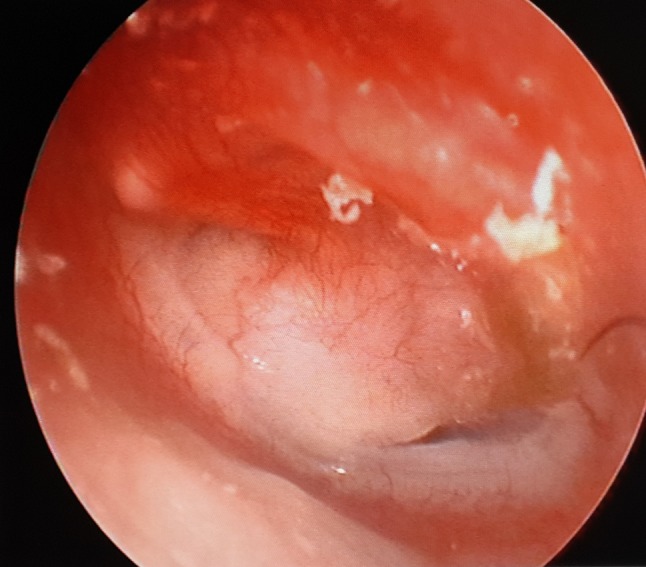
Post operative picture of left ear full thickness tragal cartilage shield procedure at 3 months. The anterior angle maintained well
Results
34 out of 35 patients in group A had successful graft take up. All 27 patients in group B had successful closure of TM defect. So the graft take up rate is 97.14 for group A and 100 % for group B. No lateralisation or medialisation seen in any case.
Table 1 shows frequency wise hearing gain in both the groups. These values represent gain in terms of reduction in air bone gap (ABG). No worsening of bone conduction threshold indicative of sensori—neural loss was seen in any of the cases.
Table 1.
Comparison of hearing gain at various frequencies between group A and B
| Frequency (Hz) | Group A average hearing gain (n = 35) |
Group B average hearing gain (n = 27) |
P value |
|---|---|---|---|
| 250 | 17.57 | 16.67 | 0.444 not significant |
| Mean of 500,1,000,2,000 | 19.05 | 18.98 | 0.238 not significant |
| 4,000 | 15.00 | 12.41 | 0.027 significant |
| 8,000 | 12.00 | 10.36 | 0.355 not significant |
It is apparent that hearing gain is maximum in mid frequencies, i.e. 500, 1,000 and 2,000 Hz in both groups. At 4,000 and 8,000 Hz, hearing gain is less. The difference of hearing gain, between group A and B at mid frequencies, at 8,000 Hz as well as at 250 Hz, is statistically not significant. Only at 4,000 Hz, there is statistically significant difference in hearing gain between group A and group B with group A having more hearing gain. (p = 0.027).
For both group A and B, the hearing gain at mid frequencies is significantly greater than the hearing gain at 4,000 and at 8,000 Hz. There is no statistically significant difference in hearing gain at 250 Hz and at mid frequencies for both groups (Tables 2, 3).
Table 2.
Comparison of hearing gain at different frequencies for group A cases
| Frequency (Hz) | Average pre op/post op | Average hearing gain | Compare with hearing gain at 250 Hz | Compare with hearing gain at 500, 1,000 and 2,000 |
|---|---|---|---|---|
| 250 | 34.14/16.57 | 17.57 | P = 0.112 not significant | |
| 500, 1,000, 2,000 | 36.81/17.76 | 19.05 | ||
| 4,000 | 34.14/19.14 | 15 | P = 0.000068 significant | |
| 8,000 | 34.29/22.29 | 12 | P = 0.0000000049 significant | P < 0.00000001 significant |
Table 3.
Comparison of hearing gain at different frequencies for group B cases
| Frequency (Hz) | Average pre op/post op | Average hearing gain | Compare with hearing gain at 250 Hz | Compare with hearing gain at 500, 1,000 and 2,000 |
|---|---|---|---|---|
| 250 | 32.78/16.11 | 16.67 | P = 0.14 not significant | |
| 500, 1,000, 2,000 | 36.66/18.47 | 18.98 | ||
| 4,000 | 33.70/21.30 | 12.41 | P = 0.000000048 significant | |
| 8,000 | 33.15/22.04 | 11.11 | P = 0.0000173 significant | P < 0.000001 significant |
Discussion
As early as in 1963, the use of cartilage for tympanoplasty has been advised. [7] Many otologists have made many changes with time in the technique of cartilage tympanoplasty. Mürbe et al. [8] have compared different cartilage techniques and stated that from an acoustical point of view, the 0.5-mm cartilage plate seems preferable compared with the palisade technique. Mohamad et al. [9] have concluded that tympanoplasty using cartilage with or without perichondrium has better morphological outcome than tympanoplasty using temporalis fascia. However, there was no statistically significant difference in hearing outcomes between the 2 grafts. Nicholas et al. [10] have stated that the use of cartilage as a graft material in pediatric myringoplasty is a safe and effective technique.
Lee et al. [11] have developed a cartilage plate-TM-coupled model using high-resolution computed tomography and finite element analysis and from their study they concluded that the optimal thickness of a cartilage graft for myringoplasty appears to be 0.1–0.2 mm for medium and large TM perforations. For small perforations, a cartilage of less than 1.0 mm is a good compromise between mechanical stability and low acoustic transfer loss. Yung [12] in 2008 have mentioned from literary review that concerns that the stiffness and mass of cartilage grafts may adversely affect hearing have not been substantiated in clinical reports thus far. Mokbel et al. [13] have used ultrathin cartilage and concluded that the hearing results of 0.2 mm partial thickness cartilage are more or less similar to that of temporalis fascia which is little better.
In our study, we have used thin cartilage in group A where the approximate thickness is 0.45 mm. In group B, thinning was not done and approximate thickness is 0.9 mm. In this study, the cartilage shield technique has been modified as well. Various reference books mention that the distance between the lateral and medial walls of the middle ear is 2 mm at the level of umbo, 4 mm in the attic and 6 mm in the hypotympanum. By cutting the tensor tympani tendon and putting adequate gelfoam in middle ear, this distance can be modified to accommodate even full thickness tragal cartilage without compromising the middle ear space significantly.
Conclusion
The graft take up rates are excellent for both partial and full thickness tragal cartilage material in modified cartilage shield technique of tympanoplasty. Difference in hearing gain is not statistically significant between the two groups, except at 4,000 Hz where hearing gain in partial thickness tragal cartilage recipients (Group A) is more than full thickness tragal cartilage recipients (Group B). For both group A and B, hearing gain is more at 250, 500, 1,000 and 2,000 Hz than at 4,000 and 8,000 Hz frequencies. No other complications seen in any of the cases in any group. This technique is good for closure of TM perforations and it provides good hearing gain by thick or thin cartilage pieces.
Acknowledgments
Authors’ independent work. No grant or funds taken.
Contributor Information
Sohil Vadiya, Email: sohilv81@gmail.com.
Sushen Bhatt, Email: sushenbhatt@hotmail.com.
References
- 1.Aarnisalo AA, Cheng JT, Ravicz ME, Furlong C, Merchant SN, Rosowski JJ. Motion of the tympanic membrane after cartilage tympanoplasty determined by stroboscopic holography. Hear Res. 2010;263(1–2):78–84. doi: 10.1016/j.heares.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Milewski C. Composite graft tympanoplasty in the treatment of ears with advanced middle ear pathology. Laryngoscope. 1993;103:1352–1356. doi: 10.1288/00005537-199312000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Amedee RG, Mann WJ, Rie-cheimann H. Cartilage palisade tympanoplasty. Am J Otol. 1989;10:447–450. doi: 10.1097/00129492-198911000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Cavaliere M, Mottola G, Rondinelli M, Iemma M. Tragal cartilage in tympanoplasty: anatomic and functional results in 306 cases. Acta Otorhinolaryngol Ital. 2009;29(1):27–32. [PMC free article] [PubMed] [Google Scholar]
- 5.Duckert LG, Müller J, Makielski KH, Helms J. Composite autograft “shield” reconstruction of remnant tympanic membranes. Am J Otol. 1995;16(1):21–26. [PubMed] [Google Scholar]
- 6.Kartush JM, Michaelides EM, Becvarovski Z, LaRouere MJ. Over – under tympanoplasty. Laryngoscope. 2002;112(5):802–807. doi: 10.1097/00005537-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Jansen C. Cartilagen—tympanoplasty. Laryngoscope. 1963;73:1288–1302. doi: 10.1288/00005537-196310000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Mürbe D, Zahnert T, Bornitz M, Hüttenbrink K-B. Acoustic properties of different cartilage reconstruction techniques of the tympanic membrane. Laryngoscope. 2002;112:1769–1776. doi: 10.1097/00005537-200210000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Mohamad SH, Khan I, Hussain SS. Is cartilage tympanoplasty more effective than fascia tympanoplasty? A systematic review. Otol Neurotol. 2012;33(5):699–705. doi: 10.1097/MAO.0b013e318254fbc2. [DOI] [PubMed] [Google Scholar]
- 10.Nicholas BD, O’Reilly RC. Is cartilage preferable to fascia myringoplasty in children? Laryngoscope. 2010;120(11):2136–2137. doi: 10.1002/lary.21006. [DOI] [PubMed] [Google Scholar]
- 11.Lee CF, Chen JH, Chou YF, Hsu LP, Chen PR, Liu TC. Optimal graft thickness for different sizes of tympanic membrane perforation in cartilage myringoplasty: a finite element analysis. Laryngoscope. 2007;117(4):725–730. doi: 10.1097/mlg.0b013e318031f0e7. [DOI] [PubMed] [Google Scholar]
- 12.Yung M. Cartilage tympanoplasty: literature review. J Laryngol Otol. 2008;122:663–672. doi: 10.1017/S0022215108001813. [DOI] [PubMed] [Google Scholar]
- 13.Mukbel KM, Thabet ESM. Repair of subtotal tympanic membrane perforation by ultrathin cartilage shield: evaluation of take rate and hearing result. Eur Arch Otorhinolaryngol. 2013;270:33–36. doi: 10.1007/s00405-011-1903-5. [DOI] [PubMed] [Google Scholar]


