Introduction
Papular acantholytic dyskeratosis (PAD) of the genitocrural area is a rarely reported skin disorder in women and even less frequently reported in men. We present a case of PAD localized to the inguinal fold of a 78-year-old man. PAD should be added to the differential diagnosis of intertrigo.
Case report
A 78-year-old man was hospitalized for resection of a craniopharyngioma. His postoperative course was complicated by infections and a 4-month-long hospitalization. The dermatology department was consulted because of a new inguinal rash. The patient noted a 7-day history of a nonpruritic, nontender eruption localized to the right inguinal fold, treated with miconazole powder without improvement. He denied a history of similar eruption in the past. The patient denied family members with skin disease. Physical examination of the right inguinal fold found 15 to 20 pink-white verrucous papules in a linear, nonblaschkoid distribution (Figs 1 and 2). There was no involvement of the left crural fold, genitalia, or other areas of the body. His hands and feet were free of papules, and nail examination was negative for longitudinal erythronychia. A 3-mm punch biopsy was performed to clarify the diagnosis. Histologic examination found suprabasilar acantholysis and dyskeratosis, including the presence of corps ronds and grains, parakeratosis, and hyperkeratosis (Fig 3). There was no evidence of herpetic infection. Given the focal nature of these papules, a diagnosis of papular acantholytic dyskeratosis was made.
Fig 1.

Papular acantholytic dyskeratosis. Red-pink verrucous papules in a linear distribution.
Fig 2.

Papular acantholytic dyskeratosis. White macerated papules in the intertriginous fold.
Fig 3.
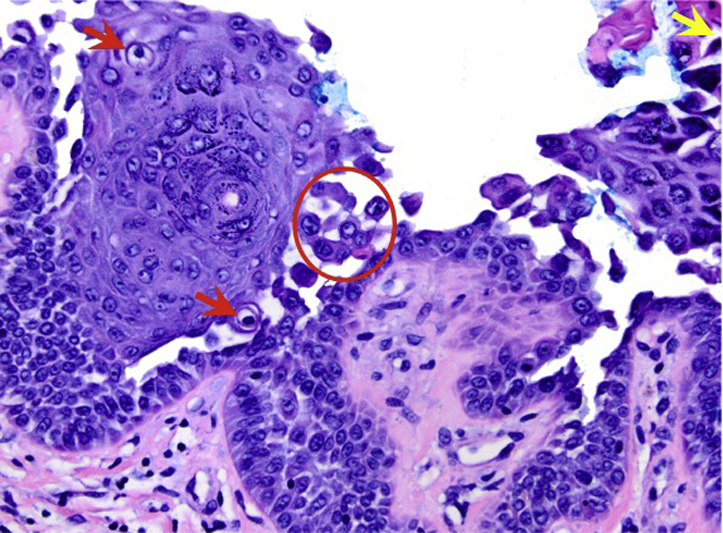
Papular acantholytic dyskeratosis. Hematoxylin-eosin staining at ×40 magnification shows suprabasilar acantholysis (circle) and dyskeratosis with the presence of corps ronds (red arrows) and grains (yellow arrow) are seen.
Discussion
PAD localized to the genitocrural area is a subtype of focal acantholytic dyskeratosis, a concept first coined by Ackerman1 in 1972 to describe a distinctive histologic pattern associated with variable clinical expression. PAD of the genitocrural area is characterized by skin-colored to white papules localized to the vulva, penis, scrotum, perianal area, and inguinal folds. The lesions are pink-red papules but become white with maceration and intertriginous location. Papules may be pruritic or painful, but most often are asymptomatic.2, 3, 4, 5, 6, 7 Histologic findings include acantholysis of the epidermis and dyskeratosis; corps ronds and grains may be seen.1 Parakeratosis and hyperkeratosis are reported in many but not all cases. PAD is rarely reported in women3, 4, 6 and even less frequently in men.2, 5, 8
The differential diagnosis for linear verrucous papules in the crural area includes segmental Darier's disease, Hailey-Hailey disease, inflammatory linear verrucous epidermal nevus, seborrheic keratosis, herpes simplex virus infection, and condyloma acuminata. Given the unique histopathologic features, it is important to distinguish PAD of the genitocrural area from cases of segmental Darier's and Hailey-Hailey disease. The few examples of segmental Darier's and Hailey-Hailey disease reported in the literature describe patients with papules of the intertriginous areas. However, these patients often had a positive family history associated with autosomal dominant mutations, ATP2A2 (ATPase gene associated with Darier's disease) and ATP2C1 (ATPase gene associated with Hailey-Hailey disease), respectively, and had other areas of skin involvement. Additionally, lesions of segmental Darier's and Hailey-Hailey exhibit a blaschkoid distribution, which was not observed in our patient.9 A negative family history and late onset of disease make either diagnosis less likely. However, a form of localized genetic mosaicism of segmental Darier's disease cannot be absolutely excluded.10 It is also important to distinguish PAD from Grover's disease, which shares histopathologic features of acantholysis and dyskeratosis, but the clinical features and the distribution of the lesions, distinguish the two.
We present a unique case of PAD isolated to the inguinal area in a male patient, a unifying diagnosis that reconciles clinical and histologic evidence. Our case highlights the importance of considering PAD in the differential diagnosis for men with genitocrural dermatosis. A review of the English-language literature on the topic found 39 reported cases of isolated genitocrural PAD, with most cases reported in the gynecologic literature (Table I). We highlight 11 cases of male patients, which suggest that the disease may be more common in men than has been previously been described. In asymptomatic patients like our case, lesions may go unobserved outside of the hospital setting, and PAD of the crural area in men may be more prevalent than is suggested by the published literature.
Table I.
Case reports of PAD
| Study | Sex | Age | Family history | Location |
|---|---|---|---|---|
| Hazelrigg and Stoller,11 1977 | F | 29 | N | Vulva (acantholysis) |
| King and Hirose,12 1978 | F | 43 | N | Labia majora (acantholysis) |
| Duray et al,13 1983 | F | 38 | N | Labia majora |
| F | 49 | N | Labia majora | |
| F | 52 | N | Labia majora | |
| Chorzelski et al,7 1984 | F | 23 | - | Labia majora |
| Frances et al,141984 | M | - | - | Genitalia |
| M | - | - | Genitalia | |
| Evron et al,15 1984 | F | 40 | N | Labia majora |
| Coppola et al,16 1986 | F | 44 | N | Labia majora/perineum |
| Van der Putte et al,171986 | M | 34 | - | Penis |
| Warkel et al,181986 | M | 30 | N | Anal canal |
| Cooper,3 1989 | F | 28 | N | Bilateral labium majora |
| F | 37 | N | Right labia majora | |
| F | 47 | N | Left labia majora | |
| F | 83 | N | Left inguinal fold | |
| F | 63 | N | Left inguinal fold | |
| F | 55 | N | Right thigh/inguinal fold | |
| Lee et al,51989 | M | 32 | N | Pubic area |
| Barrett et al,19 1989 | F | 43 | N | Vulva |
| Ridley and Buckley,20 1991 | F | - | - | Vulva |
| Langenberg et al,21 1992 | F | 32 | N | Vulva/inner thighs |
| F | 41 | N | Labia and perineum | |
| M | 27 | N | Perianal/perineal | |
| Salopek et al,22 1993 | F | 5 | N | Vulvar, perivulvar skin |
| Wong et al,81994 | M | 61 | N | Scrotum |
| M | 25 | N | Penis | |
| M | 60 | N | Thigh, sacrum, penis | |
| Pestereli et al,23 2000 | F | 44 | N | Bilateral Labia majora |
| Krishnan et al,4 2001 | F | 27 | N | Vulvocrural area |
| Bell et al,24 2001 | F | 41 | N | Labia majora |
| F | 33 | N | Vulva/inner thighs | |
| Sáenz et al,25 2005 | F | 11 | N | Labia majora |
| Browne et al,26 2007 | F | 24 | N | Genital |
| Roh et al,27 2009 | F | 63 | N | Labia majora |
| Wang et al,28 2009 | F | - | - | Vulva |
| Dittmer et al,6 2010 | F | 45 | N | Vulva/intertriginous area |
| Verma,22013 | M | 26 | N | Perianal/perineal |
| Xiao et al,292013 | M | 48 | N | genital and perianal |
Cases of males with PAD are set in bold.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Ackerman A.B. Focal acantholytic dyskeratosis. Arch Dermatol. 1972;106:702–706. [PubMed] [Google Scholar]
- 2.Verma S.B. Papular acantholytic dyskeratosis localized to the perineal and perianal area in a young male. Indian J Dermatol. 2013;58:393–395. doi: 10.4103/0019-5154.117317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooper P.H. Acantholytic dermatosis localized to the vulvocrural area. J Cutan Pathol. 1989;16:81–84. doi: 10.1111/j.1600-0560.1989.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 4.Krishnan R.S., Ledbetter L.S., Reed J.A., Hsu S. Acantholytic dermatosis of the vulvocrural area. Cutis. 2001;67:217–219. 220. [PubMed] [Google Scholar]
- 5.Lee S.H., Jang J.G. Papular acantholytic dyskeratosis of the genitalia. J Dermatol. 1989;16:312–314. doi: 10.1111/j.1346-8138.1989.tb01270.x. [DOI] [PubMed] [Google Scholar]
- 6.Dittmer C.J., Hornemann A., Rose C., Diedrich K., Thill M. Successful laser therapy of a papular acantholytic dyskeratosis of the vulva: case report and review of literature. Arch Gynecol Obstet. 2010;281:723–725. doi: 10.1007/s00404-009-1313-8. [DOI] [PubMed] [Google Scholar]
- 7.Chorzelski T.P., Kudejko J., Jablonska S. Is papular acantholytic dyskeratosis of the vulva a new entity? Am J Dermatopathol. 1984;6:557–560. doi: 10.1097/00000372-198412000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Wong T.Y., Mihm M.C., Jr. Acantholytic dermatosis localized to genitalia and crural areas of male patients: a report of three cases. J Cutan Pathol. 1994;21:27–32. doi: 10.1111/j.1600-0560.1994.tb00687.x. [DOI] [PubMed] [Google Scholar]
- 9.Bolognia J., Schaffer J.V., Duncan K.O., Ko C.J. Saunders/Elsevier; Oxford: 2014. Dermatology essentials. [Google Scholar]
- 10.Happle R. Mosaicism in human skin. Understanding the patterns and mechanisms. Arch Dermatol. 1993;129(11):1460–1470. [PubMed] [Google Scholar]
- 11.Hazelrigg D.E., Stoller L.J. Isolated familial benign chronic pemphigus. Arch Dermatol. 1977;113(9):1302. [PubMed] [Google Scholar]
- 12.King D.T., Hirose F.M., King L.A. Simultaneous occurrence of familial benign chronic pemphigus (Hailey-Hailey disease) and syringoma on the vulva. Arch Dermatol. 1978;114(5):801. doi: 10.1001/archderm.1978.01640170095037. [DOI] [PubMed] [Google Scholar]
- 13.Duray P.H., Merino M.J., Axiotis C. Warty dyskeratoma of the vulva. Int J Gynecol Pathol. 1983;2(3):286–293. doi: 10.1097/00004347-198303000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Frances C., Boisnic S., Lessana-Leibowitch M., Hewitt J. Male genital dyskeratotic tumor. 2 case reports. Ann Dermatol Venereol. 1984;111(3):233–236. French. [PubMed] [Google Scholar]
- 15.Evron S., Leviatan A., Okon E. Familial benign chronic pemphigus appearing as leukoplakia of the vulva. Int J Dermatol. 1984;23(8):556–557. doi: 10.1111/j.1365-4362.1984.tb04212.x. [DOI] [PubMed] [Google Scholar]
- 16.Coppola G., Muscardin L.M., Piazza P. Papular acantholytic dyskeratosis. Am J Dermatopathol. 1986;8(4):364–365. doi: 10.1097/00000372-198608000-00020. [DOI] [PubMed] [Google Scholar]
- 17.Van der Putte S.C., Oey H.B., Storm I. Papular acantholytic dyskeratosis of the penis. Am J Dermatopathol. 1986;8(4):365–366. doi: 10.1097/00000372-198608000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Warkel R.L., Jager R.M. Focal acantholytic dyskeratosis of the anal canal. Am J Dermatopathol. 1986;8(4):362–363. doi: 10.1097/00000372-198608000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Barrett J.F., Murray L.A., MacDonald H.N. Darier's disease localized to the vulva. Case report. Br J Obstet Gynaecol. 1989;96(8):997–999. doi: 10.1111/j.1471-0528.1989.tb03363.x. [DOI] [PubMed] [Google Scholar]
- 20.Ridley C.M., Buckley C.H. Darier's disease localized to the vulva. Br J Obstet Gynaecol. 1991;98(1):112. doi: 10.1111/j.1471-0528.1991.tb10325.x. [DOI] [PubMed] [Google Scholar]
- 21.Langenberg A., Berger T.G., Cardelli M., Rodman O.G., Estes S., Barron D.R. Genital benign chronic pemphigus (Hailey-Hailey disease) presenting as condylomas. J Am Acad Dermatol. 1992;26(6):951–955. doi: 10.1016/0190-9622(92)70140-b. [DOI] [PubMed] [Google Scholar]
- 22.Salopek T.G., Krol A., Jimbow K. Case report of Darier disease localized to the vulva in a 5-year-old girl. Pediatr Dermatol. 1993;10(2):146–148. doi: 10.1111/j.1525-1470.1993.tb00042.x. [DOI] [PubMed] [Google Scholar]
- 23.Peştereli H.E., Karaveli S., Oztekin S., Zorlu G. Benign persistent papular acantholytic and dyskeratotic eruption of the vulva: a case report. Int J Gynecol Pathol. 2000;19(4):374–376. doi: 10.1097/00004347-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Bell H.K., Farrar C.W., Curley R.K. Papular acantholytic dyskeratosis of the vulva. Clin Exp Dermatol. 2001;26(5):386–388. doi: 10.1046/j.1365-2230.2001.00840.x. [DOI] [PubMed] [Google Scholar]
- 25.Sáenz A.M., Cirocco A., Avendaño M., González F., Sardi J.R. Papular acantholytic dyskeratosis of the vulva. Pediatr Dermatol. 2005;22(3):237–239. doi: 10.1111/j.1525-1470.2005.22312.x. [DOI] [PubMed] [Google Scholar]
- 26.Browne F., Keane H., Walsh M., Maw R. Papular acantholytic dyskeratosis presenting as genital warts. Int J STD AIDS. 2007;18(12):867–868. doi: 10.1258/095646207782716938. [DOI] [PubMed] [Google Scholar]
- 27.Roh M.R., Choi Y.J., Lee K.G. Papular acantholytic dyskeratosis of the vulva. J Dermatol. 2009;36(7):427–429. doi: 10.1111/j.1346-8138.2009.00660.x. [DOI] [PubMed] [Google Scholar]
- 28.Wang L., Yang X.C., Hao F., Mei Y., Ye Q.Y. Papular acantholytic dyskeratosis of the vulva. Eur J Dermatol. 2009;19(4):402–403. doi: 10.1684/ejd.2009.0697. [DOI] [PubMed] [Google Scholar]
- 29.Xiao X.M., Xu H.X., Xu X.L. Papular acantholytic dermatosis of the anogenital areas. Eur J Dermatol. 2013;23(6):886–887. doi: 10.1684/ejd.2013.2174. [DOI] [PubMed] [Google Scholar]


