Introduction
The first syphilis epidemic dates back to the 16th century, and was first known as lues venerea, translated literally as venereal pest.1 Schaudinn and Hoffman first described spirochaeta pallida as the etiologic bacterium in 1905. The incidence of the disease declined dramatically with the advent of penicillin and reached an historic low in 2000.2 Since 2001 syphilis rates have increased dramatically, particularly among men who have sex with men (MSM), and among ethnic minorities in urban centers.3 Despite centuries of experience with syphilis, effective early diagnosis and treatment remain difficult, in large part because of the ability of syphilis to mimic other cutaneous eruptions. We present a case of a rare presentation of syphilis, coined rupioid syphilis, because of its likeness to the outer layer of an oyster shell. This case highlights the importance of recalling the diverse presentations of syphilis and its recent nearly epidemic resurgence and public health threat, particularly among MSM.
Case report
A 43-year-old man with no known previous dermatologic history, originally from Guam, presented with pruritic papules and plaques with heaped up mounds of scale of several months' duration involving the dorsal hands and feet, upper extremities, lower extremities, and trunk (Fig 1). All of his nails were noted to be dystrophic with extensive hyperkeratotic, subungual debris. He denied recent sick contacts, sexual activity, or travel outside the United States. He worked as a stocker at a grocery store and noted that exposure to cold temperatures caused worsening of his symptoms. His medical history was remarkable for stage 4 chronic kidney disease and uncontrolled type 2 diabetes mellitus (hemoglobin A1c value, 6.6%). His family history was unremarkable.
Fig 1.
Right forearm with erythematous plaques with heaped up mounds of scale resembling the outer layer of an oyster shell.
Two punch biopsy specimens from the right upper extremity were obtained for histopathologic evaluation (Figs 2 and 3). Laboratory workup included rapid plasma reagin (RPR) and HIV tests. Punch biopsies found marked regular psoriasiform epidermal hyperplasia with parakeratosis and intracorneal neutrophils. There was vascular ectasia with swelling of endothelial cells and a perivascular infiltrate of lymphocytes, numerous plasma cells, and scattered eosinophils. RPR testing returned positive at a titer of 1:4. A positive fluorescent treponemal antibody absorption test result confirmed the diagnosis of late latent syphilis, rupioid type. HIV results were negative.
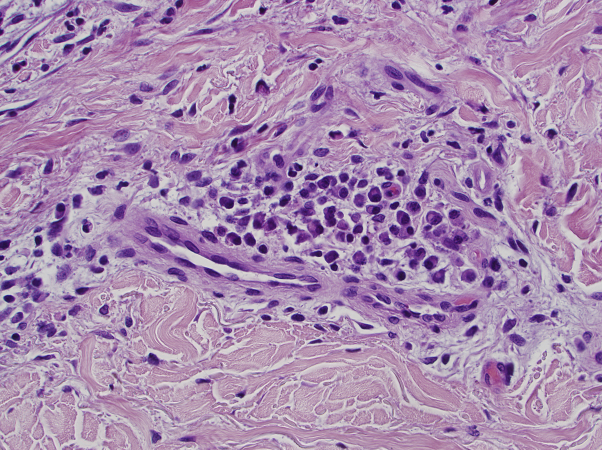
Fig 2.
Biopsy of right forearm shows endothelial swelling with conspicuous perivascular plasma cells. (Original magnification, ×40.)
Fig 3.
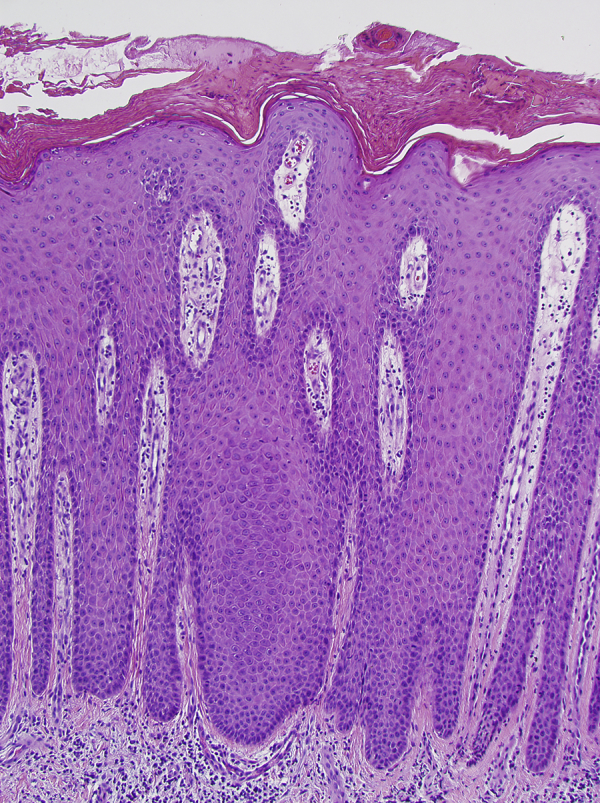
Biopsy of right forearm shows crusted psoriasiform epidermal hyperplasia with a mixed perivascular infiltrate. (Original magnification, ×10.)
Discussion
Syphilis is caused by infection with Treponema pallidum subspecies pallidum, a spirochete bacterium, which solely affects human hosts.4 The most common mode of transmission is through vaginal, anal, or oral sexual contact with an infected partner.5 The number of syphilis infections in the United States has increased steadily from an historic low of 2.1 cases per 100,000 in 2000 to 5.3 cases in 2013.2 A large portion of this increase is owing to an increase in syphilis among men, with a particularly accelerated rate of infection occurring in MSM.2 In 2005, the Centers for Disease Control and Prevention reported that 64% of syphilis cases in 29 states were among MSM.2, 3
T pallidum has a long replication time and is largely reliant on host pathways for survival.4, 5 Transmission of the bacterium occurs via microscopic tears or abrasions in the skin. Primary syphilis first manifests as nonspecific erythema and then evolves into a painless chancre at the site of inoculation 1 to 6 weeks later.4 Subsequent rapid hematogenous dissemination allows for disease at sites distant from the initial site of inoculation, typically 4 to 10 weeks after development of the chancre, giving rise to secondary syphilis.6 It is estimated that less than 40% of patients with syphilis have primary syphilis diagnosed, making familiarity of the diverse manifestations of secondary syphilis of particular importance, as in our case.
Secondary syphilitic lesions last for several weeks before spontaneously resolving. Patients at this stage have early, latent infection.4 When syphilitic lesions recur after 1 year from the initial eruption, or seropositivity is detected more than 1 year after the initial eruption, it is termed late latent syphilis.6 Patients at this stage often represent a diagnostic conundrum, as in our case, because of the protean manifestations of secondary syphilis. For this reason, syphilis has been termed the great imitator. Early secondary lesions have been described as macular, papular, follicular, lichenoid, psoriasiform, or corymbiform.6, 7 Late secondary lesions can be large plaques with a condylomatous, pustular, pigmentary, or, as in this case, a rupioid appearance.6, 7 A rupioid presentation consists of large plaques with darkened, heaped-up mounds of crust and scale resembling the back of an oyster shell. An array of other diseases can present with rupioid skin lesions, including rupioid psoriasis, keratotic scabies, reactive arthritis, and disseminated histoplasmosis. T pallidum does not readily grow in vitro, and attempts to culture the organism to further clarify its unique ability to produce such a diverse array of clinical presentations have been unsuccessful.7
Secondary syphilis also has considerable histopathologic variability; this is thought to be because of the many types of secondary syphilitic lesions and how these lesions evolve over time.8 Typical findings include a lymphocytic, monocytic, and plasmacytic infiltration of the papillary and reticular dermis.4, 9 The epidermis is often involved and shows psoriasiform hyperplasia with superficial neutrophils. There is a lichenoid tissue reaction and numerous plasma cells in approximately one-third of cases.8
All patients with possible syphilis should undergo serologic testing with an RPR. This is a non–treponemal-specific test that detects antibodies to lecithin cholesterol antigen. False-positive results are possible, and confirmatory testing is recommended with a treponemal-specific test, most commonly the fluorescent treponemal antibody absorption test in the United States.6 The latter finding remains positive for life. RPR titers decrease with treatment and should be used to detect treatment response.3, 6
Our patient was referred to both an infectious disease specialist and the Department of Public Health. He received the traditional treatment of 2.4 million units of intramuscular benzathine benzylpenicillin weekly for 3 doses to treat late latent syphilis. He was seen in the clinic 3 months later with complete resolution of cutaneous lesions (Fig 4). Repeat RPR testing failed to show a decline in antibody titer, but given his complete resolution of symptoms he was thought to have an appropriate treatment response. This case shows a rare presentation of an increasingly common disease and the importance of thinking of syphilis in sexually active patients with new skin eruptions.
Fig 4.
Right forearm after treatment with benzathine benzylpenicillin.
Acknowledgments
The authors thank Dr Keliegh Culpepper, MD, Director of Dermatopathology and Clinical Instructor in Dermatology, University of Arizona, Dermpath Diagnostics, Tucson, Arizona. Dr Culpepper provided the histopathologic images and analysis for the case. She did not receive any compensation for her role.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Farhi D., Nicolas D. Origins of syphilis and management in the immunocompetent patient: Facts and controversies. Clin Dermatol. 2010;28:533–538. doi: 10.1016/j.clindermatol.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Primary and secondary syphilis-US, 2005-2013. MMWR Morb Mortal Wkly Rep. 2014;63(18):402–406. [PMC free article] [PubMed] [Google Scholar]
- 3.Daskalakis D. Syphilis: Continuing Public Health and Diagnositic Challenges. Current HIV/AIDS Rep. 2008;5:72–77. doi: 10.1007/s11904-008-0012-6. [DOI] [PubMed] [Google Scholar]
- 4.Goldsmith L.A., Katz S.I., Gilchrest B.A., Paller A.S., Leffell D.J., Wolff K. 8th ed. Vol. 1. McGraw-Hill; New York: 2012. (Fitzpatrick's Dermatology in General Medicine). [Google Scholar]
- 5.Cohen S.E., Klausner J.D., Engelman J., Philip S. Syphilis in the Modern Era An Update for Physicians. Infect Dis Clin N Am. 2013;27:705–722. doi: 10.1016/j.idc.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Lautenschlager S. Cutaneous Manifestations of Syphilis, Recognition and Management. Am J Clin Dermatol. 2006;7(5):291–304. doi: 10.2165/00128071-200607050-00003. [DOI] [PubMed] [Google Scholar]
- 7.Baughn R.E., Musher D.M. Secondary Syphilitic Lesions. Clin Microbiol Rev. 2005;18(1):205–216. doi: 10.1128/CMR.18.1.205-216.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alessi E., Innocenti M. Ragusa G Secondary syphilis. Clinical morphology and histopathology. Am J Dermatopathol. 1983;5(1):11–17. [PubMed] [Google Scholar]
- 9.Peeling R.W., Hook E.W. The Pathogenesis of Syphilis: The Great Mimicker, Revisited. J Pathol. 2006;208:224–232. doi: 10.1002/path.1903. [DOI] [PubMed] [Google Scholar]