Introduction
Leishmaniasis is an infectious disease endemic to 88 countries on 5 continents. It is estimated that there are 1 to 1.5 million cases of cutaneous leishmaniasis among local populations, but leishmaniasis also commonly affects travelers to these endemic countries. Leishmaniasis is caused by parasitic protozoa in the genus Leishmania, which are transmitted by phlebotomine sandflies, and is divided into 2 categories: Old World and New World. Old World leishmaniasis is considered mostly benign and self-limited, whereas New World species are able to cause a wide array of clinical manifestations, from benign to life-threatening disease. Through dissemination via blood, lymph, and local extension, New World Leishmania species can cause mucosal and visceral involvement. Although mucosal leishmaniasis was originally attributed exclusively to Leishmania braziliensis, it is now known that Leishmania panamensis, Leishmania guyanensis, and Leishmania peruviana, all of the Viannia subgenuses found in Central and South America, may also cause mucosal involvement.1, 2, 3 Herein, we present an uncommon case of New World leishmaniasis in 2 travelers returning to the United States.
Case report
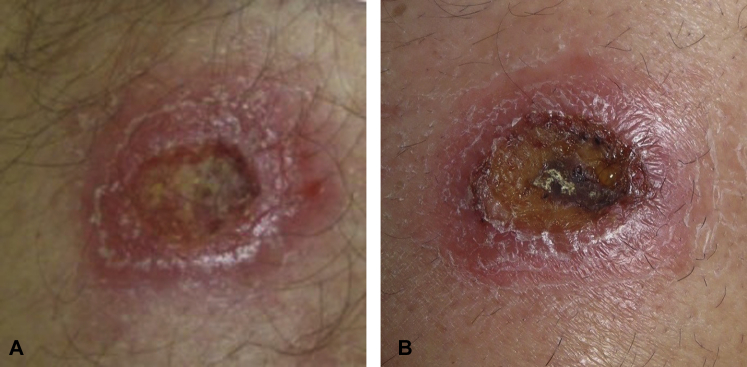
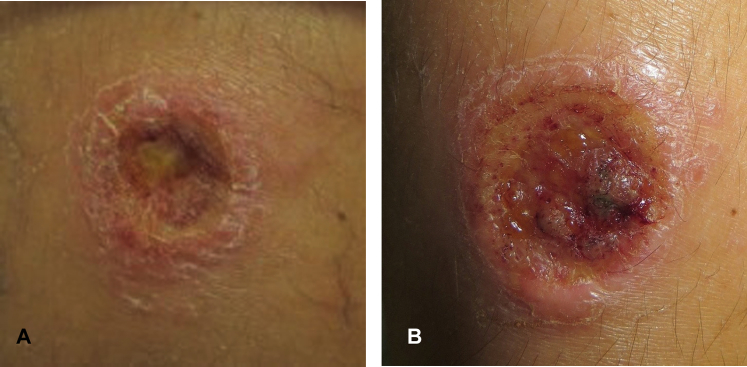
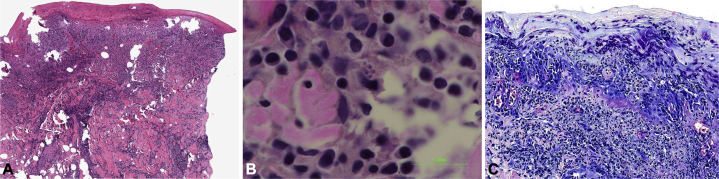
A 49-year-old man and his 17-year-old son presented for evaluation of ulcerative lesions on the left leg (father) and right arm (son). The patients traveled to Costa Rica 3 months prior and noticed multiple bites on the extremities after returning home, all of which resolved except for the lesions as previously noted. These lesions were neither pruritic nor painful, and the patients denied systemic symptoms. Physical examination of the father's left thigh found a 1.5-cm erythematous and indurated nodule with central ulceration (Fig 1, A). There was a similar 1-cm erythematous, ulcerated and heme-crusted nodule on the son's right extensor arm (Fig 2, A). Biopsies of both lesions found a superficial and deep mixed inflammatory infiltrate with overlying ulcerated epidermis. Scattered microorganisms were present, highlighted by Giemsa stain (Fig 3, A-C). Leishmania polymerase chain reaction (PCR) and DNA sequencing, real-time PCR, and microscopy confirmed L panamensis. At 2-week follow-up, the father's lesion had grown in size and developed small satellite nodules (Fig 1, B). The father also had a single enlarged lymph node on the leg near the lesion. The son's lesion had also grown slightly, and he had nontender brachial lymphadenopathy (Fig 2, B). Both patients continued to deny any new symptoms or systemic complaints. Given the risk of mucocutaneous disease, the patients each underwent a 10-day course of intravenous liposomal amphotericin B therapy. After treatment, both patients reported that their lesions had substantially decreased in size. Because L panamensis is a member of the Leishmania Viannia subgenus and confers risk of mucocutaneous disease, oral miltefosine or intravenous pentamidine are other systemic therapies that could be considered as future treatments if necessary.
Fig 1.
A, Ulcer on 49-year-old man on the left, anterior leg at initial presentation. B, The lesion 2 weeks later shows significant enlargement, additional exudate, and increased surrounding induration.
Fig 2.
A, Ulcer on a 17-year-old man on the right, posterior arm at initial presentation. The site was previously biopsied. B, The lesion 2 weeks later shows enlargement and additional exudate.
Fig 3.
A, Superficial and deep dense dermal infiltrate of lymphocytes, plasma cells, histiocytes, and epithelioid cells with overlying epidermis. B, Parasitized macrophages. The Leishmania organisms are round to oval basophilic structures with eccentrically located kinetoplasts. C, Numerous dermal histiocytes containing cytoplasmic Leishmania parasites. (A and B, Hematoxylin-eosin stain; C, Giemsa stain.)
Discussion
Members of the Leishmania (Viannia) subgenus are known to cause destructive lesions of the nasal, oral, and hypopharyngeal mucosa. Mucosal involvement is rare in travelers and has not been well studied.3 L panamensis is less well studied than L braziliensis, but it is thought that mucosal involvement by L panamensis may be less severe. Disease caused by L panamensis tends to be limited to one mucosal surface and less destructive with lower rates of perforation of the nasal septum. The milder clinical manifestation may be caused by the less reactogenic nature of L panamensis, that is, less capability of the organism to induce a destructive immune response.1
Treatment of leishmaniasis in travelers remains controversial. Although evidence exists for treatment in endemic areas, treatment of leishmaniasis in travelers is poorly characterized. Because a species-specific approach may lead to higher cure rates and lower medication side effects, laboratory tests are important in identifying causative species. PCR, as used in this case, offers a highly sensitive means of identification. Presence of Leishmania may also be determined by microscopy of tissue smears or by histopathology of skin biopsy sections. Leishmania may be cultured in specialized media, but the process is difficult and, as demonstrated in this case, may result in a false-negative result. Local treatment with topical applications and intralesional injections may be used in species with little risk of mucosal involvement; however, for species such as L panamensis, which are known to affect the mucosa, systemic therapy is recommended. For treatment of L panamensis, miltefosine, pentamidine, or liposomal amphotericin B, as used in this case, may be used depending on the clinical picture. Pentavalent antimonial agents are effective, but less toxic treatments are preferred.3 We present this case to highlight this uncommon disease in travelers and the importance of early recognition and treatment to avoid mucosal involvement.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Osorio L.E., Castillo C.M., Ochoa M.T. Mucosal leishmaniasis due to Leishmania (Viannia) panamensis in Colombia: clinical characteristics. Am J Trop Med Hyg. 1998;59(1):49–52. doi: 10.4269/ajtmh.1998.59.49. [DOI] [PubMed] [Google Scholar]
- 2.Blum J., Desjeux P., Schwartz E., Beck B., Hatz C. Treatment of cutaneous leishmaniasis among travellers. J Antimicrob Chemother. 2004;53(2):158–166. doi: 10.1093/jac/dkh058. [DOI] [PubMed] [Google Scholar]
- 3.Showler A.J., Boggild A.K. Cutaneous leishmaniasis in travellers: a focus on epidemiology and treatment in 2015. Curr Infect Dis Rep. 2015;17(7):489. doi: 10.1007/s11908-015-0489-2. [DOI] [PubMed] [Google Scholar]