Abstract
We investigated the association between breastfeeding and cognitive development in infants during their first 3 years. The present study was a part of the Mothers’ and Children’s Environmental Health (MOCEH) study, which was a multi-center birth cohort project in Korea that began in 2006. A total of 697 infants were tested at age 12, 24, and 36 months using the Korean version of the Bayley Scales of Infant Development II (K-BSID-II). The use and duration of breastfeeding and formula feeding were measured. The relationship between breastfeeding and the mental development index (MDI) score was analyzed by multiple linear regression analysis. The results indicated a positive correlation between breastfeeding duration and MDI score. After adjusting for covariates, infants who were breastfed for ≥ 9 months had significantly better cognitive development than those who had not been breastfed. These results suggest that the longer duration of breastfeeding improves cognitive development in infants.
Keywords: Breastfeeding, Korean Bayley Scales of Infant Development II (K-BSID-II), Mental Development Index
Graphical Abstract
INTRODUCTION
Cognitive development of infants is determined by heredity (1), psychosocial factors, and their interactions (2). There is increasing focus on the effects of parenting and emotional interactions between the mother and child on cognitive development in infants (3,4,5).
Breastfeeding provides nutritional and immunological benefits to infants and also prevents infections (6,7,8). Breastfeeding improves cognitive development and emotional interactions between the mother and infant (9). A previous meta-analysis of 20 studies that compared breastfeeding with formula-feeding reported that breastfeeding is associated with significantly improved cognitive development from infancy to adolescence (10). Bartels et al. (9) found that breastfeeding is strongly correlated with cognitive development, even after controlling for the mother’s IQ and education level. In addition, the Promotion of Breastfeeding Intervention Trial reported that breastfed infants have higher IQs (11,12). However, other studies have shown contrasting results. For example, a meta-analysis by Der et al. (13) showed that improved cognitive development associated with breastfeeding disappears or declines significantly after controlling for other related variables. These studies may have had discrepant results because they adjusted for different covariates, had limitations in research design, or methodological problems (14). Other studies have reported that the relationship between cognitive development and breastfeeding is weak or nonexistent after controlling for confounding variables (15,16).
The present study aimed to clarify the relationship between breastfeeding and cognitive development in a Korean birth cohort using data from the Mothers and Children’s Environmental Health (MOCEH) study. We addressed two specific questions: Is breastfeeding positively correlated with cognitive development in early childhood after adjusting for covariates? What is the optimal breastfeeding duration for improving cognitive development?
MATERIALS AND METHODS
Participants and methods
The present investigation is a component of the MOCEH study, a multi-center prospective birth cohort study (17). Infants were followed-up 12, 24, and 36 months after recruitment. The 36-month follow-up was completed in December 2010. Prior to enrolment, all study participants (mothers) provided written informed consent.
Each mother was asked at the 6- and 12-month follow-ups whether she was breastfeeding her infant, breastfeeding duration, and whether formula was being used. Then, each woman was placed into one of six categories: 1) formula feeding only, 2) breastfeeding for < 3 months, 3) breastfeeding for 3–5 months, 4) breastfeeding for 6–8 months, 5) breastfeeding for 9–11 months, and 6) breastfeeding for ≥ 12 months.
All infants completed K-BSID-II at the 12-, 24-, and 36-month follow-ups to derive a mental development index (MDI) score and a psychomotor development index (PDI) score. A total of 697 infants were followed up at 12 months, 551 infants at 24 months, and 433 infants at 36 months.
The parents of each infant were interviewed by trained personnel using a detailed questionnaire to obtain the mothers’ age, educational level (lower than high school, high school diploma, college degree, university degree, and higher than a university degree), family income, job status (employed/unemployed), sex of infant, gestational age, and infant birth weight.
Statistical analyses
The distributions of the mother’s and children’s variables were described according to the type and duration of feeding. The chi-square test was used to compare categorical variables and one-way analysis of variance was used to compare continuous variables of the different subgroups. If a difference was significant in this analysis, then Dunnett’s test was used for the post-hoc comparison. The relationship between breastfeeding duration and child cognitive development was evaluated using multivariate linear regression after controlling for possible confounding factors. Missing data were deleted case-wise. SPSS (22.0) software (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses, and a P value < 0.05 was considered significant.
Ethics statement
This study protocol was approved by the institutional review boards of Ewha Womans University (Seoul) (IRB No. 12-07B-15), Dankook University Hospital (Cheonan) (IRB No. 2011-09-0340), and Ulsan University Hospital (Ulsan) (IRB No. 06-29), all of which are in the Republic of Korea. All of the study participants provided their informed consent prior to the enrollment.
RESULTS
Characteristics of the participants
Table 1 shows the sociodemographic characteristics of the study subjects who used formula only (n = 125) and of those who breastfed with or without formula (n = 572). The number of mothers who breastfed for durations < 3, 3–5, 6–8, 9–11, and ≥ 12 months were 108 (15.5%), 70 (10.0%), 57 (8.2%), 276 (39.6%), and 61 (8.8%), respectively. Mean maternal age at birth was 30.0 years in the formula-only group and 30.1 years in the breastfeeding group (P = 0.766). Use of breastfeeding was significantly greater in women who had more education (P = 0.001) and in those with higher family incomes (P = 0.041) than in those included in the other groups. Maternal job status, sex of the infant, gestational age, and infant birth weight did not affect type of feeding.
Table 1. Sociodemographic characteristics of the subjects who used formula only and those who breastfed with or without formula.
| Variables | Formula only n = 125 |
Breastfeeding n = 572 |
Total n = 697 |
P value* |
|---|---|---|---|---|
| Maternal age at birth, yr mean ± SD | 30.0 ± 3.5 | 30.1 ± 3.5 | 30.1 ± 3.5 | 0.766 |
| Maternal education, No. (%) | ||||
| High school or lower | 54 (43.2) | 144 (25.2) | 198 | 0.001 |
| College degree | 15 (12.0) | 87 (15.2) | 102 | |
| University or higher | 54 (43.2) | 332 (58.0) | 386 | |
| Unknown | 2 (1.6) | 9 (1.6) | 11 | |
| Family income, No. (%) | ||||
| < 2,000 USD | 37 (29.6) | 148 (25.9) | 185 | 0.041 |
| 2,000-3,999 USD | 75 (60.0) | 301 (52.6) | 376 | |
| ≥ 4,000 USD | 10 (8.0) | 103 (18.0) | 113 | |
| Unknown | 3 (2.4) | 20 (3.5) | 23 | |
| Maternal employment status, No. (%) | ||||
| Unemployed | 83 (66.4) | 348 (60.8) | 431 | 0.485 |
| Employed | 33 (26.4) | 181 (31.7) | 214 | |
| Unknown | 9 (7.2) | 43 (7.5) | 52 | |
| Sex of infant, No. (%) | ||||
| Boy | 73 (58.4) | 295 (51.6) | 368 | 0.166 |
| Girl | 52 (41.6) | 277 (48.4) | 329 | |
| Gestational age | (n = 122) | (n = 558) | (n = 680) | 0.098 |
| Mean weeks ± SD | 38.6 ± 1.49 | 38.9 ± 1.50 | 38.8 ± 1.50 | |
| Birth weight (g) | (n = 118) | (n = 497) | (n = 615) | 0.871 |
| Mean ± SD | 3426 ± 243 | 3422 ± 278 | 3422 ± 272 | |
| MDI scores (Mean ± SD) | ||||
| 12 mon of age | 97.8 ± 16.66 | 101.8 ± 15.23 | 101.1 ± 15.56 | 0.009 |
| 24 mon of age | 93.1 ± 14.49 | 97.5 ± 14.53 | 96.7 ± 14.61 | 0.005 |
| 36 mon of age | 87.5 ± 13.44 | 93.2 ± 14.35 | 92.1 ± 14.34 | 0.001 |
| PDI scores (Mean ± SD) | ||||
| 12 mon of age | 91.5 ± 16.68 | 94.4 ± 15.74 | 93.9 ± 15.94 | 0.062 |
| 24 mon of age | 97.2 ± 12.98 | 95.9 ± 14.01 | 96.1 ± 13.82 | 0.385 |
| 36 mon of age | 88.8 ± 12.80 | 90.9 ± 13.34 | 90.5 ± 13.25 | 0.198 |
*P value estimated by chi-square or t-test. MDI, mental development index; PDI, psychomotor development index.
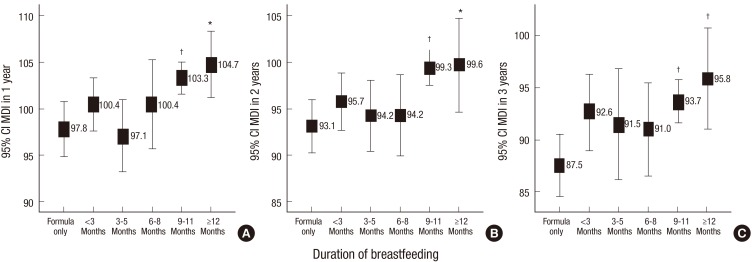
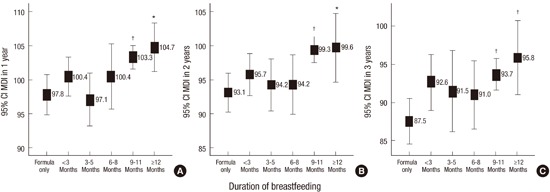
Fig. 1 shows the relationships between breastfeeding duration and infant MDI score at the 1-, 2-, and 3-year follow-ups. The results of Dunnett’s post-hoc test at each follow-up time showed that infants who were breastfed for 9–11 months or ≥ 12 months had higher MDI scores than those who received formula only. In particular, infants at the 1-year follow-up who were breastfed for 9–11 months had a mean MDI score of 103.3, those breastfed for ≥ 12 months had a mean score of 104.7, and those who received formula exclusively had a mean score of 97.8. Infants at the 2-year follow-up who were breastfed for 9–11 months had a mean MDI score of 99.3, those breastfed for ≥ 12 months had a mean score of 99.6, and those who received formula exclusively had a mean score of 93.1. Infants at the 3-year follow-up who were breastfed for 9–11 months had a mean MDI score of 93.7, those breastfed ≥ 12 months had a mean score of 95.8, and those who received formula exclusively had a mean score of 87.5. No significant differences in the PDI scores were observed although the scores showed an increasing trend at the 1- and 3-year follow-up periods for those breastfed (data not shown).
Fig. 1.
Mental development index (MDI) scores of infants who were breastfed for different durations at 1 (A), 2 (B), and 3 years (C). *,†Significant difference from formula only. Dunnett’s post-hoc test (P < 0.05, P < 0.01, respectively). MDI indicates mental development index in Korean Bayley Scales of Infant Development II (K-BSID-II).
Table 2 shows the results of multivariate analysis for the effect of breastfeeding duration on MDI score. This analysis was adjusted for maternal education level, maternal age, family income, sex of infant, gestational age, and infant birth weight. The results show that more prolonged breastfeeding was associated with a significantly higher MDI score at 1 year (β = 0.39; 95% confidence interval [CI], 0.13–0.64), 2 years (β = 0.40; 95% CI, 0.14–0.66), and 3 years (β = 0.37; 95% CI, 0.08–0.66). Moreover, a comparison of male and female infants showed that females had significantly higher MDI scores at 1 year (β = 4.89; 95% CI, 2.43–7.34), 2 years (β = 7.68; 95% CI, 5.15–10.21), and 3 years (β = 7.19; 95% CI, 4.38–10.00) than those of males. The estimated beta coefficient for MDI scores predicting the duration of breastfeeding was significant over the entire follow-up period. However, we did not find any difference in cognitive development according to maternal educational level itself after adjusting other confounding factors.
Table 2. Multiple linear regression analysis for the infant mental development index score and covariates according to breastfeeding duration after adjustment*.
| Cognitive development | Independent variable | β | 95% CI | P | R2 (P) |
|---|---|---|---|---|---|
| 12 mon of age | Duration of breastfeeding | 0.39 | 0.13-0.64 | 0.003 | 0.066 (< 0.001) |
| Sex (female vs. male) |
4.89 | 2.43-7.34 | < 0.001 | ||
| 24 mon of age | Duration of breastfeeding | 0.40 | 0.14-0.66 | 0.003 | 0.105 (< 0.001) |
| Sex (female vs. male) |
7.68 | 5.15-10.21 | < 0.001 | ||
| 36 mon of age | Duration of breastfeeding | 0.37 | 0.08-0.66 | 0.013 | 0.101 (< 0.001) |
| Sex (female vs. male) |
7.19 | 4.38-10.00 | < 0.001 |
*Covariates included maternal age, educational level of mother, family income, gestational age and birth weight. CI, confidence interval.
DISCUSSION
The present longitudinal study examined the effect of breastfeeding duration on infant cognitive development. Our initial analysis of sociodemographic factors indicated that mothers who were more educated were more likely to breastfeed than use formula. This result agrees with findings of earlier studies (18,19).
Our analysis indicated that infants had better cognitive development (MDI score) when they were breastfed ≥ 9 months from years 1–3 after birth. Moreover, comparisons of infants who were breastfed ≥ 12 months with those who were not breastfed indicated a 6.9 difference in MDI score when the infants were 1-year old, a difference of 6.5 when the infants were 2-year old, and a difference of 8.3 when the infants were 3-year old. The beneficial effect of breastfeeding on MDI score was also detected after adjusting for maternal education, maternal age, family income, sex of infant, gestational age, and infant birth weight. A recent cohort study of 1,312 infants indicated that continuing breastfeeding until month 12 positively influences cognitive development of infants from 3 to 7 years of age (20). That study indicated that as the breastfeeding period increased, the Peabody Picture Vocabulary Test score increased in 3-year old infants, and that the cognitive development score on the Kaufman Brief Intelligence Test increased at age 7. Guxens et al. (21) investigated the relationship between cognitive development and breastfeeding until 14 months after birth. They found that breastfeeding duration had a stronger influence on cognitive development than other factors, such as the mother’s educational background and social status. A longitudinal study of 468 Polish infants on the effect of breastfeeding on cognitive development indicated that infants breastfed > 3 months had IQs that were 2.1 points higher, infants breastfed 4–6 months scored 2.6 points higher, and infants breastfed > 6 months scored 3.8 points higher (14). Other studies have indicated that the risks of respiratory disorders, otitis media, diarrheal diseases, and pneumonia also decrease significantly as breastfeeding duration increases (22,23).
The positive correlation between breastfeeding and cognitive development may be because breast milk provides the nutrients required for development of the immature brain. In particular, human breast milk may support development of the newborn brain because it has long-chain polyunsaturated fatty acids (LCPUFAs), such as docosahexaenoic acid (DHA) and arachidonic acid (AA). Extensive studies on experimental animals, primates, and humans support this interpretation (24,25,26). Bjerve et al. (27) reported that serum DHA concentration is positively correlated with Bayley Mental and Psychomotor Development Scale results. Furthermore, several studies have reported that serum and erythrocyte DHA concentrations are lower in formula-fed than those in breast-fed infants (28,29,30). Early studies in primates and human infants showed that breast-fed infants score higher on visual acuity tests than that of formula-fed infants, and that this performance is correlated with DHA erythrocyte concentration (31,32).
Furthermore, the intimate relationship and physical contact between the mother and infant during breastfeeding can indirectly influence cognitive development of the infant. For example, Stack and Muir reported that increased physical contact between the mother and infant, increase visual attention of the infant. More physical contact occurs when the mother breastfeeds, but not necessarily during formula feeding (33). Furthermore, the infant experiences more cognitive assimilation and control during breastfeeding than during bottle-feeding (34). In particular, the infant matches their lip shape to the mother’s nipple and must repeatedly alternate breathing and sucking. Breastfeeding may also improve attachment between the mother and infant, which can improve the infant’s social and cognitive abilities (35). Intimate physical contact during breastfeeding may also promote a more positive and secure attachment between the mother and infant, which, in turn, increases the infant’s cognitive ability. Future studies are needed to investigate this relationship.
The advantages associated with a 6.5- to 8.3-point higher cognitive function score are significant. For example, an IQ increase of 6.5 points (44% of the SD) from 93.1 to 99.6 would elevate an individual from the 39th to the 59th percentile of the population. This increase would potentially be associated with higher educational achievement, occupational achievement, and social adjustment.
In the present study, female infants consistently had higher MDI scores after adjusting for covariates. Previous studies have also reported sex differences in cognitive development among young children, and girls tend to exceed boys, particularly in verbal skills and cognitive development (36,37).
The findings of our study have important public health implications. First, they point to the positive influence of breastfeeding on cognitive development during early childhood. Thus, breastfeeding may protect against cognitive impairment in children of vulnerable social groups or with biological impairment. Therefore, public health programs that promote increased breastfeeding duration may provide long-term benefits for children. The present findings support the recommendations of the World Health Organization and the American Academy of Pediatrics, which recommend exclusive breastfeeding for about 6 months, followed by continued breastfeeding as complementary foods are introduced, and continuing breastfeeding for ≥ 1 year (38,39).
The present study had several important strengths. First, this was a longitudinal study that used birth cohort data. Our follow-up of a large-scale sample for 3 years after birth is an additional strength. Second, this study focused on the breastfeeding duration rather than whether breastfeeding was performed or not. Finally, the present study examined Korean mothers. This is somewhat unique because most other breastfeeding studies examined Western societies, and few studies have examined Asian cultures (40).
A limitation of this study is that the cognitive development score was measured using a single test (K-BSID-II) 36 months after birth. The MOCEH study used additional tests, such as the Korean version of the Wechsler Preschool and Primary Scale of Intelligence scale, but that study is ongoing. Future studies will report these results.
In conclusion, our results indicate that breastfeeding for longer than 9 months improved cognitive development of Korean infants. The positive effect of breastfeeding persisted until infants were 3 years old after adjusting for covariates.
Footnotes
Funding: This study was supported by the MOCEH (Mothers and Children’s Environmental Health) project and was funded by the National Institute of Environmental Research, Republic of Korea.
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Design and concept of the study: Kim Y, Park H, Ha E, Hong YC, Ha M, Park H, Kim BN, Jeong KS. Acquisition of data: Park H, Lee B, Lee SJ, Lee KY, Kim JH, Ha E, Ha M, Park H. Drafting manuscript of the study: Lee H. Revising manuscript: Kim Y, Park H. Manuscript approval: all authors.
References
- 1.Bouchard TJ, Jr, McGue M. Genetic and environmental influences on human psychological differences. J Neurobiol. 2003;54:4–45. doi: 10.1002/neu.10160. [DOI] [PubMed] [Google Scholar]
- 2.Berk LE. Child Development. 8th ed. Boston, MA: Allyn & Bacon/Pearson Education; 2009. Cognitive development: Piagetian, core knowledge, and Vygotskian perspectives; pp. 258–266. [Google Scholar]
- 3.Englund MM, Luckner AE, Whaley GJ, Egeland B. Children’s achievement in early elementary school: longitudinal effects of parental involvement, expectations, and quality of assistance. J Educ Psychol. 2004;96:723–730. [Google Scholar]
- 4.Landry SH, Smith KE, Swank PR. Responsive parenting: establishing early foundations for social, communication, and independent problem-solving skills. Dev Psychol. 2006;42:627–642. doi: 10.1037/0012-1649.42.4.627. [DOI] [PubMed] [Google Scholar]
- 5.Mills-Koonce WR, Willoughby MT, Zvara B, Barnett M, Gustafsson H, Cox MJ, Family Life Project Key Investigators Mothers’ and fathers’ sensitivity and children’s cognitive development in low-income, rural families. J Appl Dev Psychol. 2015;38:1–10. doi: 10.1016/j.appdev.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bachrach VR, Schwarz E, Bachrach LR. Breastfeeding and the risk of hospitalization for respiratory disease in infancy: a meta-analysis. Arch Pediatr Adolesc Med. 2003;157:237–243. doi: 10.1001/archpedi.157.3.237. [DOI] [PubMed] [Google Scholar]
- 7.Bhandari N, Bahl R, Mazumdar S, Martines J, Black RE, Bhan MK, Infant Feeding Study Group Effect of community-based promotion of exclusive breastfeeding on diarrhoeal illness and growth: a cluster randomised controlled trial. Lancet. 2003;361:1418–1423. doi: 10.1016/S0140-6736(03)13134-0. [DOI] [PubMed] [Google Scholar]
- 8.Howie PW, Forsyth JS, Ogston SA, Clark A, Florey CD. Protective effect of breast feeding against infection. BMJ. 1990;300:11–16. doi: 10.1136/bmj.300.6716.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bartels M, van Beijsterveldt CE, Boomsma DI. Breastfeeding, maternal education and cognitive function: a prospective study in twins. Behav Genet. 2009;39:616–622. doi: 10.1007/s10519-009-9293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anderson JW, Johnstone BM, Remley DT. Breast-feeding and cognitive development: a meta-analysis. Am J Clin Nutr. 1999;70:525–535. doi: 10.1093/ajcn/70.4.525. [DOI] [PubMed] [Google Scholar]
- 11.Kramer MS, Aboud F, Mironova E, Vanilovich I, Platt RW, Matush L, Igumnov S, Fombonne E, Bogdanovich N, Ducruet T, et al. Breastfeeding and child cognitive development: new evidence from a large randomized trial. Arch Gen Psychiatry. 2008;65:578–584. doi: 10.1001/archpsyc.65.5.578. [DOI] [PubMed] [Google Scholar]
- 12.Kramer MS, Chalmers B, Hodnett ED, Sevkovskaya Z, Dzikovich I, Shapiro S, Collet JP, Vanilovich I, Mezen I, Ducruet T, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA. 2001;285:413–420. doi: 10.1001/jama.285.4.413. [DOI] [PubMed] [Google Scholar]
- 13.Der G, Batty GD, Deary IJ. Effect of breast feeding on intelligence in children: prospective study, sibling pairs analysis, and meta-analysis. BMJ. 2006;333:945. doi: 10.1136/bmj.38978.699583.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jedrychowski W, Perera F, Jankowski J, Butscher M, Mroz E, Flak E, Kaim I, Lisowska-Miszczyk I, Skarupa A, Sowa A. Effect of exclusive breastfeeding on the development of children’s cognitive function in the Krakow prospective birth cohort study. Eur J Pediatr. 2012;171:151–158. doi: 10.1007/s00431-011-1507-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wigg NR, Tong S, McMichael AJ, Baghurst PA, Vimpani G, Roberts R. Does breastfeeding at six months predict cognitive development? Aust N Z J Public Health. 1998;22:232–236. doi: 10.1111/j.1467-842x.1998.tb01179.x. [DOI] [PubMed] [Google Scholar]
- 16.Jacobson SW, Chiodo LM, Jacobson JL. Breastfeeding effects on intelligence quotient in 4- and 11-year-old children. Pediatrics. 1999;103:e71. doi: 10.1542/peds.103.5.e71. [DOI] [PubMed] [Google Scholar]
- 17.Kim BM, Ha M, Park HS, Lee BE, Kim YJ, Hong YC, Kim Y, Chang N, Roh YM, Kim BN, et al. The mothers and children’s environmental health (MOCEH) study. Eur J Epidemiol. 2009;24:573–583. doi: 10.1007/s10654-009-9370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harwood L, Fergusson D. Breastfeeding and later cognitive and academic outcome. Pediatrics. 1998;101:1–7. doi: 10.1542/peds.101.1.e9. [DOI] [PubMed] [Google Scholar]
- 19.Celi AC, Rich-Edwards JW, Richardson MK, Kleinman KP, Gillman MW. Immigration, race/ethnicity, and social and economic factors as predictors of breastfeeding initiation. Arch Pediatr Adolesc Med. 2005;159:255–260. doi: 10.1001/archpedi.159.3.255. [DOI] [PubMed] [Google Scholar]
- 20.Belfort MB, Rifas-Shiman SL, Kleinman KP, Guthrie LB, Bellinger DC, Taveras EM, Gillman MW, Oken E. Infant feeding and childhood cognition at ages 3 and 7 years: effects of breastfeeding duration and exclusivity. JAMA Pediatr. 2013;167:836–844. doi: 10.1001/jamapediatrics.2013.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guxens M, Mendez MA, Moltó-Puigmartí C, Julvez J, García-Esteban R, Forns J, Ferrer M, Vrijheid M, López-Sabater MC, Sunyer J. Breastfeeding, long-chain polyunsaturated fatty acids in colostrum, and infant mental development. Pediatrics. 2011;128:e880–9. doi: 10.1542/peds.2010-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quigley MA, Kelly YJ, Sacker A. Breastfeeding and hospitalization for diarrheal and respiratory infection in the United Kingdom Millennium Cohort Study. Pediatrics. 2007;119:e837–42. doi: 10.1542/peds.2006-2256. [DOI] [PubMed] [Google Scholar]
- 23.Chantry CJ, Howard CR, Auinger P. Full breastfeeding duration and associated decrease in respiratory tract infection in US children. Pediatrics. 2006;117:425–432. doi: 10.1542/peds.2004-2283. [DOI] [PubMed] [Google Scholar]
- 24.Makrides M, Neumann MA, Gibson RA. Effect of maternal docosahexaenoic acid (DHA) supplementation on breast milk composition. Eur J Clin Nutr. 1996;50:352–357. [PubMed] [Google Scholar]
- 25.Janssen CI, Zerbi V, Mutsaers MP, de Jong BS, Wiesmann M, Arnoldussen IA, Geenen B, Heerschap A, Muskiet FA, Jouni ZE, et al. Impact of dietary n-3 polyunsaturated fatty acids on cognition, motor skills and hippocampal neurogenesis in developing C57BL/6J mice. J Nutr Biochem. 2015;26:24–35. doi: 10.1016/j.jnutbio.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 26.Janssen CI, Kiliaan AJ. Long-chain polyunsaturated fatty acids (LCPUFA) from genesis to senescence: the influence of LCPUFA on neural development, aging, and neurodegeneration. Prog Lipid Res. 2014;53:1–17. doi: 10.1016/j.plipres.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Bjerve KS, Brubakk AM, Fougner KJ, Johnsen H, Midthjell K, Vik T. Omega-3 fatty acids: essential fatty acids with important biological effects, and serum phospholipid fatty acids as markers of dietary omega 3-fatty acid intake. Am J Clin Nutr. 1993;57:801S–5S. doi: 10.1093/ajcn/57.5.801S. [DOI] [PubMed] [Google Scholar]
- 28.Carlson SE, Werkman SH, Rhodes PG, Tolley EA. Visual-acuity development in healthy preterm infants: effect of marine-oil supplementation. Am J Clin Nutr. 1993;58:35–42. doi: 10.1093/ajcn/58.1.35. [DOI] [PubMed] [Google Scholar]
- 29.Clandinin MT, Jumpsen J, Suh M. Relationship between fatty acid accretion, membrane composition, and biologic functions. J Pediatr. 1994;125:S25–32. doi: 10.1016/s0022-3476(06)80733-x. [DOI] [PubMed] [Google Scholar]
- 30.Uauy RD, Birch DG, Birch EE, Tyson JE, Hoffman DR. Effect of dietary omega-3 fatty acids on retinal function of very-low-birth-weight neonates. Pediatr Res. 1990;28:485–492. doi: 10.1203/00006450-199011000-00014. [DOI] [PubMed] [Google Scholar]
- 31.Birch EE, Birch DG, Hoffman DR, Uauy R. Dietary essential fatty acid supply and visual acuity development. Invest Ophthalmol Vis Sci. 1992;33:3242–3253. [PubMed] [Google Scholar]
- 32.Makrides M, Simmer K, Goggin M, Gibson RA. Erythrocyte docosahexaenoic acid correlates with the visual response of healthy, term infants. Pediatr Res. 1993;33:425–427. doi: 10.1203/00006450-199304000-00021. [DOI] [PubMed] [Google Scholar]
- 33.Stack DM, Muir DW. Adult tactile stimulation during face-to-face interactions modulates five-month-olds’ affect and attention. Child Dev. 1992;63:1509–1525. [PubMed] [Google Scholar]
- 34.Wambach K, Riordan J. Breastfeeding and human lactation. 5th ed. Burlington, MA: Jones & Bartlett Learning; 2014. Chapter 17. Child health: theories of development; p. 679. [Google Scholar]
- 35.Schaffer HR. The early experience assumption: past, present, and future. Int J Behav Dev. 2000;24:5–14. [Google Scholar]
- 36.Bornstein MH, Hahn CS, Haynes OM. Specific and general language performance across early childhood: stability and gender considerations. First Lang. 2004;24:267–304. [Google Scholar]
- 37.Cho B, Park H. The standardization study (1) of Korean Bayley Scales of Infant Development (K-BSID-II): analyses of Korean infants’ performance of K-BSID-II in terms of demographical variables. Korean J Dev Psychol. 2004;17:191–206. [Google Scholar]
- 38.World Health Organization. The optimal duration of exclusive breastfeeding: report of an expert consultation. Geneva, Switzerland 28-30 March 2001 [Internet] Geneva: World Health Organization; 2002. [accessed on 25 May 2015]. Available at http://apps.who.int/iris/bitstream/10665/67219/1/WHO_NHD_01.09.pdf?ua=1&ua=1. [Google Scholar]
- 39.Johnston M, Landers S, Noble L, Szucs K, Viehmann L. Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827–41. doi: 10.1542/peds.2011-3552. [DOI] [PubMed] [Google Scholar]
- 40.Cai S, Pang WW, Low YL, Sim LW, Sam SC, Bruntraeger MB, Wong EQ, Fok D, Broekman BF, Singh L, et al. Infant feeding effects on early neurocognitive development in Asian children. Am J Clin Nutr. 2015;101:326–336. doi: 10.3945/ajcn.114.095414. [DOI] [PubMed] [Google Scholar]