ABSTRACT
To improve our understanding of the similarities and differences between neutralizing antibodies elicited by simian-human immunodeficiency virus (SHIV)-infected rhesus macaques and human immunodeficiency virus type 1 (HIV-1)-infected humans, we examined the plasma of 13 viremic macaques infected with SHIVSF162P3N and 85 HIV-1-infected humans with known times of infection. We identified 5 macaques (38%) from 1 to 2 years postinfection (p.i.) with broadly neutralizing antibodies (bnAbs) against tier 2 HIV-1. In comparison, only 2 out of 42 (5%) human plasma samples collected in a similar time frame of 1 to 3 years p.i. exhibited comparable neutralizing breadths and potencies, with the number increasing to 7 out of 21 (30%) after 3 years p.i. Plasma mapping with monomeric gp120 identified only 2 out of 9 humans and 2 out of 4 macaques that contained gp120-reactive neutralizing antibodies, indicating distinct specificities in these plasma samples, with most of them recognizing the envelope trimer (including gp41) rather than the gp120 monomer. Indeed, a total of 20 gp120-directed monoclonal antibodies (MAbs) isolated from a human subject (AD358) and a Chinese rhesus macaque (GB40) displayed no or limited neutralizing activity against tier 2 strains. These isolated MAbs, mapped to the CD4-binding site, the V3 loop, the inner domain, and the C5 region of gp120, revealed genetic similarity between the human and macaque immunoglobulin genes used to encode some V3-directed MAbs. These results also support the use of envelope trimer probes for efficient isolation of HIV-1 bnAbs.
IMPORTANCE HIV-1 vaccine research can benefit from understanding the development of broadly neutralizing antibodies (bnAbs) in rhesus macaques, commonly used to assess vaccine immunogenicity and efficacy. Here, we examined 85 HIV-1-infected humans and 13 SHIVSF162P3N-infected macaques for bnAbs and found that, similar to HIV-1-infected humans, bnAbs in SHIV-infected macaques are also rare, but their development might have been faster in some of the studied macaques. Plasma mapping with monomeric gp120 indicated that most bnAbs bind to the envelope trimer rather than the gp120 monomer. In support of this, none of the isolated gp120-reactive monoclonal antibodies (MAbs) displayed the neutralization breadth observed in the corresponding plasma. However, the MAb sequences revealed similarity between human and macaque genes used to encode some V3-directed MAbs. Our study sheds light on the timing and development of bnAbs in SHIV-infected macaques in comparison to HIV-1-infected humans and highlights the use of envelope trimer probes for efficient recovery of bnAbs.
INTRODUCTION
The isolation and characterization of human broadly neutralizing antibodies (bnAbs) against human immunodeficiency virus type 1 (HIV-1) (1, 2) have demonstrated the ability of the human immune system to mount effective antibody responses against the virus. Following this line of investigation, a large analysis of 205 chronically infected sera found that half of the tested sera were capable of neutralizing half of the 219 viral strains tested (3). These results indicate that neutralizing antibodies with 50% breadth are common in chronically infected individuals and support the current goal of inducing a similar spectrum of antibody responses with vaccines. However, current HIV-1 vaccines cannot induce such antibody responses. As HIV-1 vaccine candidates rely on nonhuman primates (NHP) for preclinical tests (4), it is also important to characterize NHP antibody responses to the HIV-1 envelope (Env) in simian-human immunodeficiency virus (SHIV)-infected rhesus macaques and to compare them to the responses in HIV-1-infected humans.
To date, bnAbs against HIV-1 tier 2 isolates have rarely been detected in SHIV-infected macaques (5–9). A previous screening of 40 macaques infected with uncloned SHIVAD8 or a molecular clone of SHIVAD8-CK15 identified a single animal, CE8J, that developed potent bnAbs directed to the N332 glycosylation site (5). In an additional study of 19 macaques infected with uncloned SHIVAD8 or a molecular clone of SHIVAD8-EO, CE8J-like bnAb response was not detected (6). Instead, 7 macaques in the latter study exhibited cross-reactive antibodies with limited potency, and one animal, CL5E, displayed impressive neutralization breadth and potency (6). Here, we screened 13 viremic macaques infected with the clade B R5 uncloned SHIVSF162P3N (10–13) or its derivative molecular clones (14) for neutralizing activity against HIV-1. Compared with the commonly used SHIVSF162P3, the lineage-related late isolate SHIVSF162P3N is more macaque adapted and more pathogenic (10), and macaques infected with the virus are more likely to demonstrate a sustained viral load (13). Since high levels of plasma viral load have been associated with bnAb development in HIV-1-infected individuals (15), these viremic SHIVSF162P3N-infected animals are of interest to screen for possible bnAbs against HIV-1.
As most experimental SHIV infections are terminated at 2 years p.i., parallel analysis of antibody responses during the first 2 years of infection in HIV-1-infected humans is warranted. Although early studies of human samples have initially focused on time points relatively late during infection (i.e., >3 years p.i.) (16–18), more recent research has shifted to analyzing longitudinal samples from individuals newly infected with HIV-1 (19–22). These studies documented that autologous antibody responses develop early, within 1 year p.i. (19, 22), but that bnAbs take 1 to 3 years of infection to become detectable (21). While still a work in progress, research has also attempted to track bnAb maturation pathways (23, 24) and to identify sequential Env variants that can be attributed to bnAb development (25). Here, we analyzed the plasma of 85 HIV-1-infected individuals who are part of the Aaron Diamond AIDS Research Center (ADARC) Acute and Early HIV-1 Infection Cohort (26–28) and identified those with neutralization breadth.
To further characterize the human and macaque broadly neutralizing plasma samples, and in particular their antibody epitope specificities, we generated gp120-based probes for plasma-mapping analysis. The RSC3 probe (29), derived from the HXB2 gp120 core and designed to expose the CD4-binding site (CD4bs) of gp120, has been successfully used to isolate the monoclonal antibody (MAb) VRC01 (29) and other bnAbs targeting the CD4bs (23, 30–32). Because RSC3 does not bind to CD4 and thus does not interfere with the CD4 cellular receptor, it has also been used directly in the TZM-bl-based neutralization assay for plasma mapping (23, 29, 30, 32). However, since certain bnAb epitopes at the CD4bs are altered in RSC3, we generated additional gp120 probes with point mutations to minimize CD4 interference for direct plasma-mapping analysis and isolation of MAbs from a subset of study samples.
MATERIALS AND METHODS
Human specimens.
The plasma and peripheral blood mononuclear cell (PBMC) samples analyzed in this study were collected from 85 participants in the ADARC Acute and Early HIV-1 Infection Cohort (26–28), in which newly infected individuals were recruited and followed longitudinally, with Institutional Review Board (IRB)-approved protocols at the Rockefeller University. All the individuals were infected with clade B HIV-1 (26, 27). At the time of sampling, these subjects had been infected for 3 to 85 months and had not initiated antiretroviral therapy.
Rhesus specimens.
The rhesus plasma and PBMC samples analyzed in this study were from macaques described in previous studies that had been inoculated with the pathogenic clade B R5 SHIVSF162P3N (10–14) as an uncloned viral swarm or with its derivative molecular clones. All of the rhesus specimens were collected at the Tulane National Primate Research Center in compliance with its Guide for Care and Use of Laboratory Animals and under protocols approved by the Institutional Animal Care and Use Committee (IACUC).
Antibodies, CD4-Ig, cells, plasmids, and viruses.
The anti-gp120 MAbs VRC01 (CD4bs), 17b (coreceptor binding site [CoRbs]), and A32 (inner domain) were obtained from the NIH AIDS Reagent Program and were contributed by John Mascola (VRC01) and James Robinson (17b and A32). The anti-V3-loop MAb 447-52D was provided by Susan Zolla-Pazner. The anti-V3-stem MAb PGT128 (33) was produced by gene synthesis and cloning (34). The sheep anti-gp120 C5 polyclonal antibody D7324 was purchased from Aalto Bio Reagents (Dublin, Ireland). CD4-Ig was produced by gene synthesis and cloning into pcDNA3.1 (Invitrogen, Thermo Fisher Scientific, Waltham, MA). The TZM-bl cells and the HIV-1 SG3Δenv backbone (35, 36) were obtained from the NIH AIDS Reagent Program and were contributed by John Kappes and Xiaoyun Wu. The HIV-1 clade A, B, and C reference rev-env expression plasmids (37–40) were obtained from the NIH AIDS Reagent Program and were contributed by Julie Overbaugh, Beatrice Hahn, Cynthia Derdeyn, Lynn Morris, and Carolyn Williamson. The HIV-1 Env pseudoviruses were prepared by cotransfecting 293T clone 17 (ATCC, Manassas, VA) with the rev-env plasmids and the SG3Δenv backbone.
HIV-1 env SGA and sequence analysis.
The AD358 autologous env gene was amplified from a plasma sample collected at 2 months p.i. using a single-genome amplification (SGA) method described previously (41–43). Briefly, 140 μl plasma was used to extract viral RNA using the QIAamp viral RNA minikit (Qiagen, Valencia, CA). Reverse transcription (RT) was carried out at 50°C for 60 min, followed by 55°C for an additional 60 min, in a total volume of 100 μl, including 50 μl viral RNA, 20 μl 5× first-strand buffer, 5 μl deoxynucleoside triphosphates (dNTPs) (each at 10 mM), 1.25 μl antisense primer envB3out (43) at 20 μM, 5 μl dithiothreitol (DTT) at 100 mM, 5 μl RNaseOut (Invitrogen), and 5 μl SuperScript III (Invitrogen). Synthesized cDNA was titrated to single copy, where PCR-positive wells constitute about 30% of the reactions. Nested PCRs were carried out in a volume of 20 μl consisting of 2 μl 10× buffer, 0.8 μl MgSO4, 0.4 μl dNTP (each at 10 mM), 0.2 μl of each primer at 20 μM, 0.1 μl Platinum Taq High Fidelity DNA polymerase (Invitrogen), and 1 μl template DNA. The primers were envB5out and envB3out for 1st-round PCR and envB5in and envB3in for the 2nd round (43). The cycler parameters were 94°C for 2 min and 35 cycles (45 cycles for the 2nd round) of 94°C for 15 s, 55°C for 30 s, and 68°C for 4 min, followed by 68°C for 10 min. The PCR amplicons were subjected to direct Sanger sequencing, and all sequencing chromatograms were inspected in Sequencher 5.3 (Gene Codes, Ann Arbor, MI) for mixed bases (double peaks), which were evidence of priming from more than one template or of PCR errors. Any sequence with double peaks was excluded. A total of 38 env SGA sequences were obtained from the AD358 2-month-p.i. plasma sample and codon aligned using ClustalW built in BioEdit (http://www.mbio.ncsu.edu/bioedit/bioedit.html). The aligned nucleotide sequences were submitted to DNADist built in BioEdit for calculation of the pairwise distance. With one exception, 37 out of the 38 env sequences were homogeneous, with 20 being identical and the rest varying by 0.19% at maximum. The one variant (AD358_m2_37) differs by 3.16 to 3.33% from the 37 homogeneous sequences. A representative of the 37 env sequences, AD358_m2, was reamplified from the 1st-round PCR mixture containing full-length rev-env and cloned into pcDNA3.1 Directional TOPO (Invitrogen).
HIV-1 gp120 expression and purification.
Codon-optimized genes encoding the CD5 leader and the JR-FL and AC10.29 gp120s (amino acids 32 to 507, according to the HXB2 codon position) with C-terminal Avi and 6×His tags were synthesized and cloned into pcDNA3.1 (Invitrogen) at ImmuneTech (New York, NY). The Yu2 gp120 expression plasmid was obtained from Joseph Sodroski. Point mutations D368R (44) and W479A (45) were generated by site-directed mutagenesis (GB Biosciences, Gaithersburg, MD). Soluble gp120s were expressed by transfecting 293F cells (Invitrogen); after 6 days, the culture supernatants were harvested and filtered through 0.45-μm filters, and the buffer was changed to PBS using Pierce Slide-A-Lyzer flasks (Thermo Fisher Scientific). The gp120 proteins were purified via 6×His using HisTalon gravity columns (Clontech, Mountain View, CA), and then the buffer was changed to PBS and concentrated to 1 mg/ml with Amicon 30K filter units (Millipore, Billerica, MA). The purified gp120s were examined on SDS-PAGE (Invitrogen) and stored in aliquots at −80°C.
Single-B-cell sorting by fluorescence-activated cell sorter (FACS).
Avi-tagged gp120 proteins were biotinylated using the biotin ligase Bir A (Avidity, Denver, CO), followed by streptavidin-mediated conjugation of allophycocyanin (APC) or phycoerythrin (PE) (Invitrogen). PBMCs were stained with a cocktail of antibodies to CD3-PE-CF594 (BD Biosciences, San Jose, CA), CD19-PE-Cy7 (BioLegend, San Diego, CA), CD20-APC-Cy7 (BioLegend), IgG-fluorescein isothiocyanate (FITC) (BD Biosciences), and IgM-V450 (BD Biosciences). In addition, LIVE/DEAD yellow stain (Invitrogen) was used to exclude dead cells. After washing, the cells were sorted using a multilaser MoFlo sorter (Beckman Coulter, Jersey City, NJ) contained with biosafety level 3 standards. Fluorescence compensation was performed with anti-mouse IgG(κ) beads (BD Biosciences) stained with each antibody in a separate tube. Individual B cells were sorted into 96-well PCR plates containing 20 μl lysis buffer per well. The lysis buffer contained 0.5 μl RNaseOut (Invitrogen), 5 μl 5× first-strand buffer, 1.25 μl 0.1 M DTT, and 0.0625 μl IGEPAL (Sigma, St. Louis, MO). The PCR plates with sorted cells were frozen on dry ice and then stored at −80°C. The total content of PBMCs passing through the sorter was analyzed with FlowJo (TreeStar, Cupertino, CA).
Single-B-cell RT-PCR, sequencing, and cloning.
From each sorted cell, the variable regions of IgG heavy and light chains were amplified by RT-PCR and cloned into expression vectors as previously described (34). Briefly, frozen plates with single B-cell RNAs were thawed at room temperature, and RT was carried out by adding to each well 3 μl random hexamers at 150 ng/μl (Gene Link, Hawthorne, NY), 2 μl dNTPs (each at 10 mM), and 1 μl SuperScript II (Invitrogen), followed by incubation at 42°C for 2 h. We note that these RT parameters may be suboptimal compared to those described previously (29, 34). After RT, 25 μl water was added to each well to dilute the cDNA, and the cDNA plates were stored at −20°C. The IgG heavy and light chain variable regions were amplified independently by nested PCR in 50 μl volumes, using 5 μl cDNA as the template, with HotStarTaq Plus DNA polymerase (Qiagen) and primer mixtures described previously (34, 46). The cycler parameters were 94°C for 5 min, 50 cycles of 94°C for 30 s, 52 to 55°C for 30 s, and 72°C for 1 min, followed by 72°C for 10 min. The PCR amplicons were subjected to direct Sanger sequencing. Human antibody sequences were analyzed using IMGT/V-QUEST (http://www.imgt.org/). Rhesus antibody sequences were analyzed using IgBLAST (47) to align them against a collection of rhesus germ line V genes (48, 49) and to calculate hypermutation frequencies. The rhesus germ line V gene that gave the lowest hypermutation frequency for each query sequence was assigned and reported. Selected PCR sequences that gave productive heavy or light chain rearrangements were reamplified with custom primers containing unique restriction digest sites and cloned into the corresponding human IgG1 heavy and light chain expression vectors as described previously (34). Full IgG1 was expressed by cotransfecting 293F cells (Invitrogen) with equal amounts of paired heavy and light chain plasmids and purified using Pierce recombinant protein A agarose (Thermo Fisher Scientific).
ELISA, endo H treatment, and MAb competition analyses.
HIV-1 gp120 or gp120-derived proteins (e.g., RSC3 and ΔRSC3, obtained from the NIH AIDS Reagent Program and contributed by Zhi-Yong Yang, Peter Kwong, and Gary Nabel) were used to coat enzyme-linked immunosorbent assay (ELISA) plates at 2 μg/ml in phosphate-buffered saline (PBS) overnight at 4°C. For endo-β-N-acetylglucosaminidase H (endo H) treatment, the amount of undiluted gp120 required to coat the plates was first calculated and mixed with 1 μl endo H (New England BioLabs, Ipswich, MA) and 10× buffer for 1 h at 37°C; an equal amount of gp120 (untreated) was processed under identical conditions without endo H. Both treated and untreated gp120s were diluted in PBS to 2 μg/ml to coat the plates. The coated plates were blocked with 1% bovine serum albumin (BSA) in PBS for 1 h at 37°C, followed by incubation with serially diluted MAbs for 1 h at 37°C. Horseradish peroxidase (HRP)-conjugated goat anti-human IgG Fc (Jackson ImmunoResearch, West Grove, PA) was added at 1:10,000 for 1 h at 37°C. All ELISA incubation volumes were 100 μl/well, except that 200 μl/well was used for blocking. The plates were washed between steps with 0.1% Tween 20 in PBS and developed with 3,3′,5,5′-tetramethylbenzidine (TMB) (Novex, Life Technologies) for 5 min with 1 M H2SO4 as the terminator and read at 450 nm. For competition ELISA, MAbs with known epitopes, such as CD4-Ig for CD4bs, 447-52D for V3 loop, PGT128 for V3 stem, 17b for CoRbs, and A32 for the inner domain, were biotinylated using EZ-Link NHS-Biotin (Thermo Fisher Scientific). The MAbs isolated in this study, such as GB40_b11 and GB40_b13, were also biotinylated and tested against competing antibodies with known epitopes. Serially diluted competing antibodies were first added at 50 μl to gp120-coated plates for 15 min at room temperature; another 50 μl of biotin-labeled MAbs was then added at a fixed final concentration as follows: to JR-FL and AC10.29 gp120s, 100 ng/ml CD4-Ig–biotin and 5 ng/ml 447-52D–biotin; to JR-FL gp120, 1 μg/ml PGT128-biotin; and to AC10.29 gp120, 2 μg/ml 17b-biotin, 150 ng/ml A32-biotin, 400 ng/ml GB40_b11-biotin, and 100 ng/ml GB40_b13-biotin. The plates were incubated at 37°C for 1 h, followed by incubation with 250 ng/ml streptavidin-HRP (Sigma) at room temperature for 30 min, and finally developed with TMB as described above.
HIV-1 neutralization assay and gp120 competition.
HIV-1 neutralization was measured using single-round infection of TZM-bl cells with Env pseudoviruses as described previously (37, 50). Neutralization curves were fitted by 5-parameter nonlinear regression (50) built in Prism 6.0 (GraphPad Software, La Jolla, CA). The 50% inhibitory titers were reported as the plasma reciprocal dilutions (50% inhibitory plasma dilutions [ID50s]) or antibody concentrations (50% inhibitory concentrations [IC50s]) required to inhibit infection by 50%. Neutralization competition was assessed by adding a fixed amount (25 μg/ml) of gp120 proteins to serially diluted plasma samples or antibodies for 15 min at 37°C prior to addition of virus. The resulting neutralization curves were compared to control curves with mock PBS added.
Statistical analysis.
The numbers of human and macaque broadly neutralizing plasma samples identified within 1 to 3 years p.i. were compared using Fisher's exact test and the chi-square analysis built into Prism 6.0 (GraphPad Software).
Nucleotide sequence accession numbers.
The nucleotide sequence of AD358_m2 env is available in GenBank under accession number KT808396. The nucleotide sequences of the heavy and light chain variable regions of 17 AD358 MAbs (7 unique clones) are available in GenBank under accession numbers KT799877 to KT799909. The nucleotide sequences of the heavy and light chain variable regions of 26 Chinese rhesus macaque GB40 MAbs (13 unique clones) are available in GenBank under accession numbers KT778824 to KT778875.
RESULTS
Plasma screening from HIV-1-infected humans.
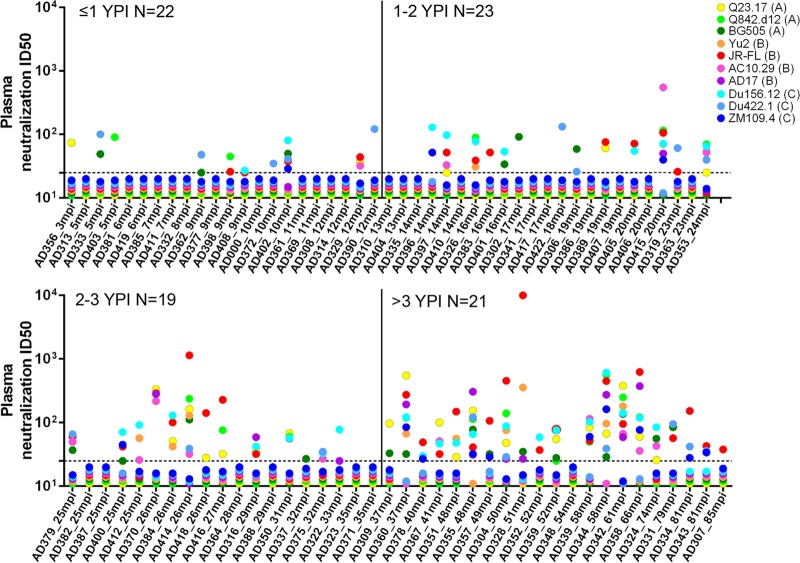
Using the TZM-bl-based neutralization assay, we screened plasma samples collected from 3 to 85 months p.i. for neutralizing activity against 10 HIV-1 Env pseudoviruses (Fig. 1). These Env isolates were selected from clades A, B, and C, and the majority of them represent tier 2 neutralization susceptibilities of HIV-1 primary isolates (50). Plasma samples that neutralized 5 or more out of the 10 tested HIV-1 strains with at least one ID50 value of >100 reciprocal dilutions were considered broadly neutralizing. Of 22 plasma samples collected within 1 year p.i., only sporadic and weak neutralizing activity (ID50 < 100) was detected; among those showing activity, individual plasma samples often neutralized only one or two strains. A single broadly reactive plasma of this group, AD402_10mpi, showed weak ID50s against 5 tested strains. In 23 plasma samples collected between 1 and 2 years p.i., neutralizing activity, although still weak, was more frequently detected; among those showing activity, two plasma samples, AD415_20mpi and AD353_24mpi, neutralized at least 5 strains, with AD415_20mpi meeting our definition of broad neutralization. In 19 plasma samples from 2 to 3 years p.i., neutralizing activity was comparable to the activity of those from 1 to 2 years p.i. but became slightly more potent, with ID50s often >100. Two plasma samples of this group, AD379_25mpi and AD414_26mpi, neutralized at least 5 tested strains, with AD414_26mpi defined as broadly neutralizing. Because the neutralization profiles of the 1- to 2-year-p.i. and 2- to 3-year-p.i. groups are comparable, we combined the two into a single 1- to 3-year-p.i. group comprising a total of 42 plasma samples. Based on our criteria, 2 of the 42 plasma samples (5%) from 1 to 3 years p.i. were broadly neutralizing. Consistent with the observation that neutralization breadth is often developed after 3 years p.i. (21), in 21 plasma samples collected after 3 years p.i., neutralizing activity was much more commonly detected—every tested plasma except one (AD348_54mpi) showed some activity. Similar to a larger study (3) that found relatively common broadly neutralizing activity in chronic sera, we also identified in the 3-year-p.i. group 7 plasma samples that were broadly neutralizing. Taken together, of 85 plasma samples tested, we identified 9 (11%) showing neutralization breadth, namely, AD415_20mpi, AD414_26mpi, AD360_37mpi, AD355_48mpi, AD304_50mpi, AD339_58mpi, AD344_58mpi, AD342_61mpi, and AD358_66mpi (Fig. 1).
FIG 1.
Neutralization ID50 titers of plasma (reciprocal dilutions) from 85 HIV-1-infected human subjects from the ADARC cohort against 10 HIV-1 Env pseudoviruses as indicated, with clades in parentheses. The dashed horizontal lines indicate the tested limit of 1:25 dilution; resistant values (<25) are plotted between 11 and 20. The study subjects are grouped based on the estimated lengths of their infection times. mpi, months postinfection; YPI, year(s) postinfection.
Screening plasma from SHIV-infected macaques.
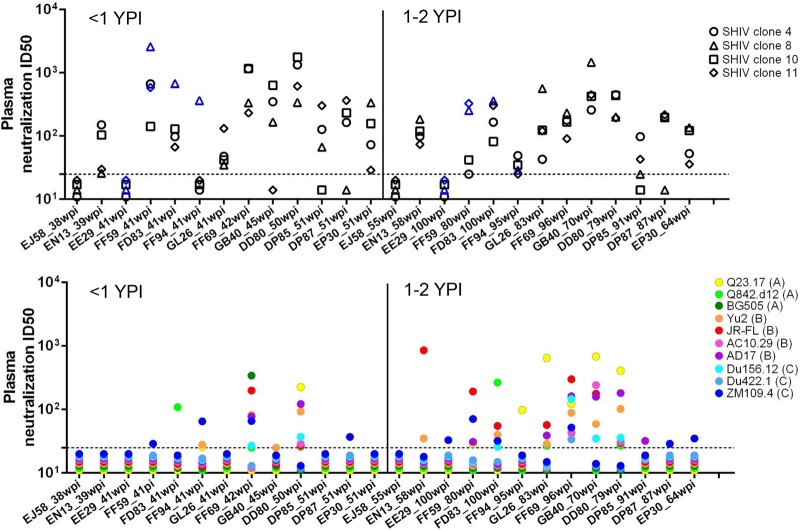
Previously, we infected Indian and Chinese rhesus macaques with a single-dose intrarectal challenge of pathogenic uncloned SHIVSF162P3N (10–13) or its derivative molecular clones (14). We identified 13 animals with sustained viral loads for at least a year, including two Chinese rhesus macaques, GL26 and GB40 (12). Using banked plasma samples, we tested two time points for each animal, one at less than 1 year p.i. and another at 1 to 2 years p.i. (Fig. 2). In addition to the same 10 HIV-1 Env pseudoviruses used for human plasma screening, we also tested 4 homologous molecular clones, 4, 8, 10, and 11, derived from the SHIVSF162P3N inoculum (14). Because animals EE29 and FF59 were infected with clones 8 and 11 (C. Cheng-Mayer, personal communication) and animals FD83 and FF94 were infected with clone 8 (14), their antibody responses to these clones are considered autologous. Consistent with the finding that autologous and homologous neutralizing antibody responses are common and arise relatively early in viremic animals (6–8), 11 of the 13 viremic macaques developed autologous or homologous neutralizing antibodies within 1 year p.i., with ID50s reaching or exceeding 1:1,000 dilution. In contrast, cross-reactivity to HIV-1 in these animals was weak and sporadic within 1 year p.i. Only two plasma samples, FF69_42wpi and DD80_50wpi, cross-neutralized 7 HIV-1 strains tested. Over time, from 1 to 2 years p.i., the autologous and homologous responses were largely maintained in these animals and did not appear to increase further. On the other hand, their HIV-1 cross-reactivity was clearly broadened. FF69_96wpi plasma neutralized all 10 tested HIV-1 Env pseudoviruses, indicating further broadening of neutralization from its 42-week-p.i. plasma. Interestingly, FF69 neutralized the HIV-1 strain BG505 most potently at 42 weeks p.i., and this activity dropped by 10-fold at 96 weeks p.i., indicating the dynamics of antibodies in the animal. DD80_79wpi plasma remained similar to that from 50 weeks p.i. Notably, GB40_70wpi neutralized 6 HIV-1 strains, and GL26_83wpi and FD83_100wpi each neutralized 5 HIV-1 strains, demonstrating progressive breadth development in these animals. Taken together, we identified 5 macaque plasma samples (38%) that were broadly neutralizing, namely, FF69_96wpi, DD80_79wpi, GB40_70wpi, GL26_83wpi, and FD83_100wpi. These numbers (5 out of 13), if treated as independent observations, are significantly higher than the 2 out of 42 (5%) seen in similarly studied human plasma samples from 1 to 3 years p.i., as determined by Fisher's exact test or a chi-square test ( Table 1). Even if we relax the criteria to include 2 additional human plasma samples (AD353_24mpi and AD379_25mpi) that neutralized 5 strains but with ID50s of <100, the numbers (4 out of 42 [10%] human samples from 1 to 3 years p.i.) are still significantly lower than those for the macaques (Table 1) (Fisher's exact test or chi-square test). However, given the fact that the macaques were infected with the same SHIV isolate or its derivative molecular clones, they cannot be treated as independent observations. Therefore, the difference observed here cannot be generalized to other SHIV-infected macaques. With this limitation in mind, the tested SHIVSF163P3N-infected macaques did not appear to lag behind the general population of HIV-1-infected humans in mounting bnAb responses.
FIG 2.
Neutralization ID50 titers of plasma (reciprocal dilutions) from 13 viremic SHIVSF162P3N-infected rhesus macaques against 4 homologous SHIV Env pseudoviruses (top) and 10 HIV-1 Env pseudoviruses (bottom), as indicated. The dashed horizontal lines indicate the tested limit of 1:25 dilution; resistant values (<25) are plotted between 11 and 20. The blue symbols in the top diagram indicate autologous responses, as animals EE29 and FF59 were infected with the SHIVSF162P3N inoculum-derived molecular clones 8 and 11 and animals FD83 and FF94 were infected with clone 8. Each animal was tested at two time points. wpi, weeks postinfection.
TABLE 1.
Statistical comparison of numbers of broadly neutralizing plasma samples (based on the indicated criteria) between HIV-1-infected humans and SHIVSF162P3N-infected macaques
| Criterion | Neutralization | No. of plasma samples |
||
|---|---|---|---|---|
| Humans 1–3 yr p.i. | Macaques 1–2 yr p.i. | Total no. | ||
| Neutralizing ≥5 out of 10 tested HIV-1 strains with an ID50 of >100a | Broad | 2 | 5 | 7 |
| Not broad | 40 | 8 | 48 | |
| Total no. | 42 | 13 | 55 | |
| Neutralizing ≥5 out of 10 tested HIV-1 strainsb | Broad | 4 | 5 | 9 |
| Not broad | 38 | 8 | 46 | |
| Total no. | 42 | 13 | 55 | |
Fisher's exact test, P = 0.006; chi-square test, P = 0.001.
Fisher's exact test, P = 0.026; chi-square test, P = 0.014.
Development of full-length gp120 probes.
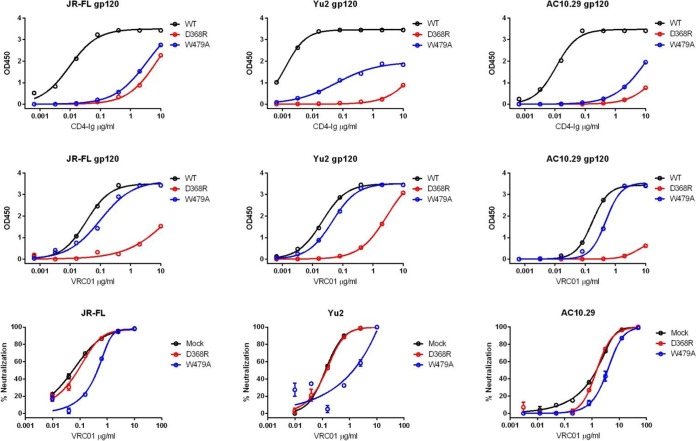
As an initial attempt to map the antibody specificities in broadly neutralizing plasma samples, we generated recombinant soluble gp120 probes based on the sequences of JR-FL, Yu2, and AC10.29. Because soluble wild-type (WT) gp120s bind effectively to the CD4 receptor and block baseline infection, they cannot be used directly in the neutralization assay to interrogate antibody specificities. We therefore introduced the D368R (44) mutation, which greatly reduces CD4 binding to minimize the soluble-gp120 interference with CD4. As the D368R mutation also reduces gp120 binding by most CD4bs-directed bnAbs, including VRC01 and its class (29), we generated another mutant, W479A, to complement D368R for plasma mapping and MAb isolation. The W479A mutation reduces gp120-CD4 interaction by keeping gp120 in an unliganded conformation (45) but largely retains binding by most CD4bs MAbs. We expressed and purified these soluble gp120 WT and mutant proteins and examined their binding to CD4-Ig (Fig. 3, top) and VRC01 (Fig. 3, middle). CD4-Ig and VRC01 bound well to all three WT gp120s. Compared with its binding to WT gp120s, CD4-Ig showed substantially reduced binding to both D368R and W479A mutants, as expected. In contrast, VRC01 showed substantially reduced binding only to D368R gp120s but largely retained its binding to W479A gp120s compared to the WT. The D368R and W479A gp120s were then tested at 25 μg/ml to adsorb VRC01-mediated neutralizing activity against each gp120 sequence-matched strain (Fig. 3, bottom). Because D368R gp120s lacked tight binding to VRC01, they were unable to adsorb VRC01-mediated neutralizing activity. In contrast, W479A gp120s retained binding affinity to VRC01 close to that of the WT, and thus, they were effective at adsorbing VRC01. These results supported the use of soluble D368R and W479A mutant gp120s to map neutralizing specificities in complex plasma.
FIG 3.
Characterization of recombinant gp120s for ELISA binding with CD4-Ig (top) and VRC01 (middle) and for neutralization competition with VRC01 (bottom). The gp120 sequences were based on JR-FL, Yu2, and AC10.29, as indicated. Each strain was tested as the WT or with a point mutation (D368R or W479A). (Bottom) For neutralization competition assays, the D368R and W479A gp120 mutants were tested at 25 μg/ml to adsorb VRC01 neutralizing activity against the indicated gp120-matched strains.
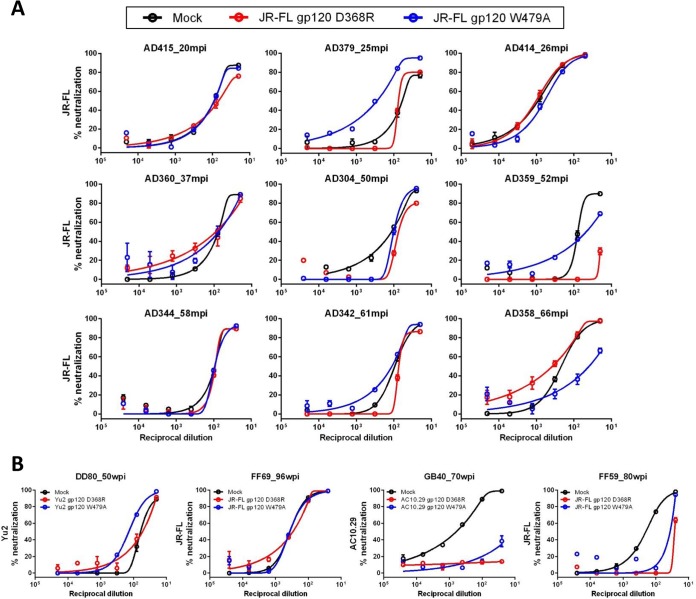
Plasma mapping using gp120 mutants.
We applied JR-FL D368R and W479A gp120s to interrogate neutralizing activities (Fig. 4A) from 7 human broadly neutralizing plasma samples that neutralized JR-FL with ID50s of >100, along with 2 additional plasma samples (AD379_25mpi and AD359_52mpi) that also neutralized JR-FL. With the exceptions of AD359_52mpi and AD358_66mpi, the plasma neutralization curves against JR-FL were mostly unchanged after adding either D368R or W479A gp120 compared to a mock control, indicating that these gp120s were ineffective at adsorbing JR-FL neutralizing activities from the tested plasma samples. From AD358 and AD359 plasma samples, D368R and W479A gp120s distinctively adsorbed neutralizing activities. Specifically, W479A gp120, but not D368R, partially adsorbed neutralizing activity from AD358_66mpi, while the opposite was observed for AD359_52mpi—D368R gp120 was more effective than W479A. Because the D368R mutation is specific for CD4bs and W479A is not, these results suggest that AD358 contains neutralizing antibodies directed to the CD4bs and AD359 contains neutralizing antibodies directed to gp120 but not to the CD4bs.
FIG 4.
Plasma-mapping analysis using recombinant gp120 proteins. Broadly neutralizing plasma samples from 9 HIV-1-infected humans (A) and 4 SHIVSF162P3N-infected macaques (B) were tested for antibody neutralization against HIV-1 strain JR-FL, Yu2, or AC10.29, as indicated, in the presence of strain-matched gp120 recombinant proteins with a D368R or W479A mutation. The gp120s were tested at 25 μg/ml to adsorb plasma neutralizing activity. Compared with mock controls, reduced or ablated activities indicate the presence of neutralizing antibodies directed to the corresponding gp120s.
Similarly, we applied the D368R and W479A gp120s (Fig. 4B) to analyze 3 macaque broadly neutralizing plasma samples that neutralized JR-FL, Yu2, or AC10.29 with an ID50 of >100, along with FF59_80wpi, which also neutralized JR-FL. Compared to mock controls, addition of either D368R or W479A gp120 did not change the neutralization curves of DD80_50wpi and FF69_96wpi, suggesting that neutralizing antibodies in these animals are not directed to these gp120s. Both D368R and W479A gp120s were effective at adsorbing neutralizing activities from GB40_70wpi and FF59_80wpi, indicating neutralizing specificities directed to these gp120s. To our knowledge, this is the first plasma-mapping analysis of SHIV-infected macaques using gp120-based proteins, although BG505 gp120 D368R has been used to map the postimmune plasma samples of macaques immunized with a BG505-based gp140 immunogen (51). Importantly, two of the best neutralizing plasma samples identified in this study, FF69_96wpi and GB40_70wpi, displayed distinct neutralizing antibody specificities.
AD358 MAbs isolated by gp120 probes.
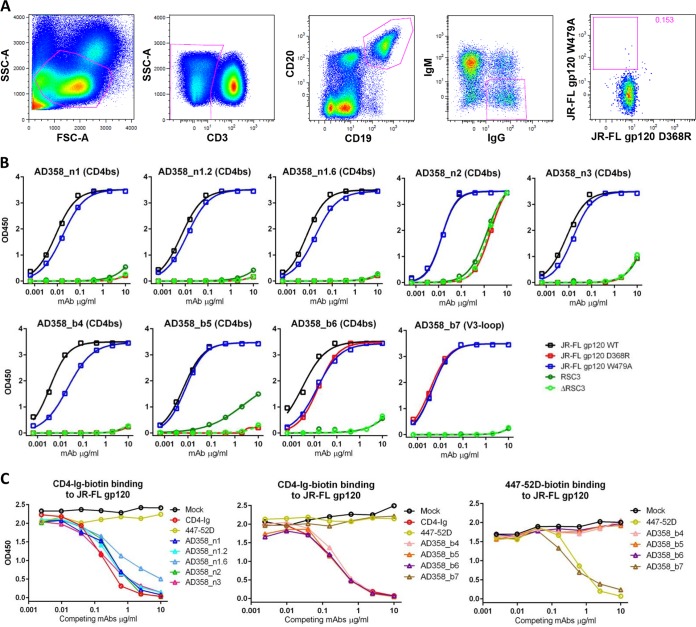
The effectiveness of gp120 adsorption suggested that the gp120 probes could be applied to AD358 and AD359 samples for MAb isolation. Since the AD358_66mpi plasma displayed a broader and more potent neutralization profile than AD359_52mpi, we proceeded with AD358_66mpi PBMCs for MAb isolation. From 7 million PBMCs, we sorted 34 B cells that stained positive for JR-FL gp120 W479A-PE and negative for JR-FL gp120 D368R-APC (Fig. 5A). We recovered 7 unique gp120-reactive MAb clones, including a major clone, AD358_n1, with 10 clonal variants. The immunoglobulin gene usage, somatic hypermutations, and CDR3 lengths of these isolated MAbs are summarized in Table 2. We cloned and expressed three variants, AD358_n1, AD358_n1.2, and AD358_n1.6, for neutralization and binding tests. The AD358_n1 MAbs neutralized JR-FL, Yu2, REJO.67, and the subject's early autologous Env clone AD358_m2 (Table 3). Two additional AD358 MAb clones, AD358_n2 and AD358_n3, also neutralized the autologous AD358_m2, JR-FL, and REJO.67 (Table 3). When tested by ELISA, these MAbs bound well to JR-FL gp120 WT and W479A, but not to D368R (Fig. 5B), consistent with the CD4bs specificity; this specificity was further supported by their effective competitions with biotin-labeled CD4-Ig (Fig. 5C). These CD4bs MAbs did not bind to RSC3, with the exception of moderate binding to RSC3 and ΔRSC3 by AD358_n2 (Fig. 5B). The other 4 AD358 MAbs comprised three (AD358_b4 to AD358_b6) to the CD4bs and one (AD358_b7) to the V3 loop (Table 2 and Fig. 5B); these specificities were supported by their effective competitions with biotin-labeled CD4-Ig or 447-52D, known to target V3 (Fig. 5C). Unlike the “conventional” CD4bs-directed MAbs, the MAb AD358_b6 largely retained its binding to gp120 D368R (Fig. 5B), indicative of an epitope not centered at the key CD4 contact residue, Asp368. Two previously known human CD4bs bnAbs, HJ16 and 179NC75, also bind to some gp120s with D368R (32, 52, 53). The MAbs AD358_b4 to AD358_b7 neutralized only tier 1 strains and did not neutralize the tier 2 strains tested (Table 3). Thus, while MAbs with the CD4bs specificity can be isolated from AD358 using gp120 probes, they are not broadly neutralizing.
FIG 5.
Isolation and characterization of AD358 MAbs. (A) B-cell staining and sorting from the PBMCs of AD358_66mpi by FACS. SSC, side scatter; FSC, forward scatter. (B) ELISA binding curves of AD358 MAbs to gp120 and RSC3 proteins, as indicated. (C) Competition ELISA analysis of AD358 MAbs.
TABLE 3.
Neutralization IC50 titers of isolated human and macaque gp120-specific MAbs
| MAb ID | Epitope | Neutralization IC50 (μg/ml)a |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tier 1 |
Tier 2 |
||||||||||
| HXB2 | SF162 | BaL.01 | JR-FL | Yu2 | AC10.29 | REJO.67 | AD358_m2 | SHIVSF162P3Nclone 8 | SHIVSF162P3Nclone 10 | ||
| AD358_n1 | CD4bs | 0.22 | 0.10 | 50 | 0.19 | 5.3 | >50 | 9.1 | 3.7 | ||
| AD358_n1.2 | CD4bs | 0.05 | 0.16 | 0.26 | 0.34 | 8.6 | >50 | 1.5 | 3.0 | ||
| AD358_n1.6 | CD4bs | 15.0 | >50 | >50 | 2.4 | >50 | >50 | 1.8 | 0.91 | ||
| AD358_n2 | CD4bs | 0.28 | 0.06 | 0.05 | 0.17 | >50 | >50 | 31.0 | 6.3 | ||
| AD358_n3 | CD4bs | >50 | 2.7 | >50 | 50.0 | >50 | >50 | 0.69 | 4.7 | ||
| AD358_b4 | CD4bs | 0.41 | 1.4 | >50 | >50 | >50 | >50 | >50 | >50 | ||
| AD358_b5 | CD4bs | 0.05 | 0.21 | 7.0 | >50 | ND | ND | ND | >50 | ||
| AD358_b6 | CD4bs | 0.06 | 0.38 | >50 | >50 | ND | ND | ND | >50 | ||
| AD358_b7 | V3 loop | >50 | 0.002 | 0.11 | >50 | ND | ND | ND | >50 | ||
| GB40_b1 | V3 loop | >50 | 0.03 | 0.72 | 50.0 | >50 | >50 | >50 | >50 | ||
| GB40_b2 | V3 loop | 0.72 | 0.01 | 0.85 | 50.0 | >50 | >50 | >50 | >50 | ||
| GB40_b3 | V3 loop | >50 | 16.4 | 15.5 | >50 | >50 | >50 | >50 | >50 | ||
| GB40_b4 | V3 loop | >50 | 0.02 | 0.34 | 45.0 | >50 | >50 | >50 | >50 | ||
| GB40_b5 | V3 loop | 0.03 | 0.08 | 2.4 | >50 | >50 | >50 | >50 | >50 | ||
| GB40_b6 | V3 loop | 11.5 | 0.23 | 2.6 | 50.0 | >50 | >50 | >50 | >50 | ||
| GB40_b7 | V3 loop | 1.9 | 0.05 | 7.9 | >50 | >50 | >50 | >50 | >50 | ||
| GB40_b8 | V3 loop | >50 | 0.09 | 1.7 | >50 | >50 | >50 | >50 | >50 | ||
| GB40_b9 | V3 stem | >50 | 0.04 | 1.1 | 45.0 | >50 | >50 | >50 | >50 | ||
| GB40_b10 | Inner domain | >50 | >50 | >50 | >50 | >50 | >50 | >50 | >50 | ||
| GB40_b11 | C5 | >50 | >50 | >50 | 45.0 | >50 | >50 | >50 | >50 | ||
| GB40_b12 | C5 | >50 | >50 | >50 | >50 | >50 | >50 | >50 | >50 | ||
| GB40_b13 | C5 | >50 | >50 | >50 | >50 | >50 | >50 | >50 | >50 | ||
ND, not done.
TABLE 2.
Genetic compositions and epitopes of isolated human and macaque gp120-specific MAbs
| MAb identifier (ID) | Origin | Host | Time p.i. | Isotype | V genea (% hypermutation) | CDR3 lengthb (aa) | Epitope on gp120 |
|---|---|---|---|---|---|---|---|
| AD358_n1 | Human | AD358 | 66 mo | IgG1 | HV3-11 (19) | H3, 13; L3, 10 | CD4bs |
| LV2-14 (13) | |||||||
| AD358_n1.2 | Human | AD358 | 66 mo | IgG1 | HV3-11 (19) | H3, 13; L3, 10 | CD4bs |
| LV2-14 (11) | |||||||
| AD358_n1.6 | Human | AD358 | 66 mo | IgG1 | HV3-11 (19) | H3, 13; L3, 10 | CD4bs |
| LV2-14 (9) | |||||||
| AD358_n2 | Human | AD358 | 66 mo | IgG1 | HV3-11 (22) | H3, 13; L3, 10 | CD4bs |
| LV2-14 (12) | |||||||
| AD358_n3 | Human | AD358 | 66 mo | IgG1 | HV3-11 (19) | H3, 13; L3, 10 | CD4bs |
| LV2-11 (9) | |||||||
| AD358_b4 | Human | AD358 | 66 mo | IgG1 | HV1-18 (10) | H3, 16; L3, 9 | CD4bs |
| KV3-11 (5) | |||||||
| AD358_b5 | Human | AD358 | 66 mo | IgG1 | HV1-18 (14) | H3, 17; L3, 10 | CD4bs |
| KV3-11 (6) | |||||||
| AD358_b6 | Human | AD358 | 66 mo | IgG1 | HV3-11 (13) | H3, 14; L3, 8 | CD4bs |
| KV3-15 (5) | |||||||
| AD358_b7 | Human | AD358 | 66 mo | IgG1 | HV5-51 (15) | H3, 8; L3, 9 | V3 loop |
| LV6-57 (9) | |||||||
| GB40_b1 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV5.46 (13) | H3, 14; L3, 11 | V3 loop |
| LV1.22 (7) | |||||||
| GB40_b2 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV3.63 (8) | H3, 17; L3, 10 | V3 loop |
| LV2A (7) | |||||||
| GB40_b3 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV3.24 (10) | H3, 6; L3, 11 | V3 loop |
| LV1.22 (5) | |||||||
| GB40_b4 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV3.44 (12) | H3, 7; L3, 8 | V3 loop |
| KV2E (9) | |||||||
| GB40_b5 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV3.44 (13) | H3, 21; L3, 9 | V3 loop |
| KV2E (5) | |||||||
| GB40_b6 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV3.44 (10) | H3, 20; L3, 9 | V3 loop |
| KV2E (6) | |||||||
| GB40_b7 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV3.44 (7) | H3, 21; L3, 9 | V3 loop |
| KV2E (4) | |||||||
| GB40_b8 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV1.53 (13) | H3, 14; L3, 11 | V3 loop |
| LV1A (9) | |||||||
| GB40_b9 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV4-F (7) | H3, 7; L3, 9 | V3 stem |
| KV2E (7) | |||||||
| GB40_b10 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV4.11 (12) | H3, 13; L3, 11 | Inner domain |
| LV1D (3) | |||||||
| GB40_b11 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV3.58 (12) | H3, 18; L3, 9 | C5 |
| KV2.44 (11) | |||||||
| GB40_b12 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV3.24 (13) | H3, 10; L3, 8 | C5 |
| KV2.46 (4) | |||||||
| GB40_b13 | Chinese rhesus macaque | GB40 | 75 wk | IgG1 | HV3.17 (10) | H3 11; L3 8 | C5 |
| KV3K (6) |
The MAb sequences were assigned to the closest known human or macaque germ line V genes, as appropriate.
The MAb CDR3 lengths were determined according to the Kabat definition (67).
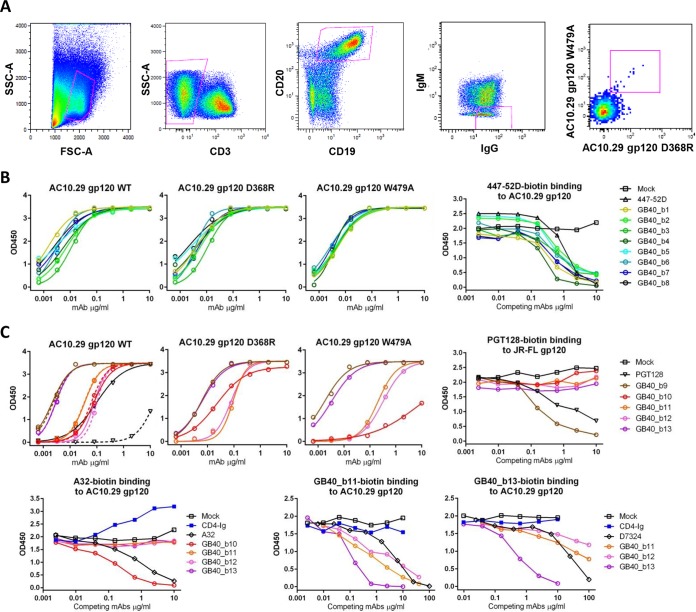
GB40 MAbs isolated by gp120 probes.
We next processed PBMCs from the Chinese rhesus macaque GB40 for MAb isolation because of its better neutralization profile over FF59. From 7.5 million GB40_75wpi PBMCs, we sorted 160 B cells that were dual positive for AC10.29 gp120 D368R and W479A (Fig. 6A). We recovered 13 unique gp120-reactive MAbs, and their immunoglobulin gene usage, somatic hypermutations, and CDR3 lengths are listed in Table 2. When tested by ELISA, the GB40 MAbs GB40_b1 to GB40_b8 bound tightly to AC10.29 WT, D368R, and W479A gp120s (Fig. 6B); this binding profile is consistent with the gp120 probes used for the B-cell sort (Fig. 6A). Competition ELISA against 447-52D–biotin indicated that MAbs GB40_b1 to GB40_b8 are directed to V3 (Fig. 6B, right). The other 5 non-V3 GB40 MAbs showed varying binding affinities to AC10.29 WT, D368R, and W479A gp120s, with two (GB40_b9 and GB40_b13) bound tightly, two (GB40_b11 and GB40_b12) moderately, and one (GB40_b10) poorly to gp120 W479A (Fig. 6C, top). We tested these MAbs in competition ELISA against CD4-Ig–biotin and 17b-biotin and confirmed that they are not directed to CD4bs or CoRbs. We determined that GB40_b9 is directed to the V3 stem, as it effectively competed with PGT128-biotin (Fig. 6C, top right). As PGT128 binds to glycans N301/N332 at the V3 base (54), we deglycosylated AC10.29 WT gp120 with endo H and tested it for MAb binding (Fig. 6C, top left). All 5 GB40 non-V3 MAbs bound the endo H-treated (dashed lines) and untreated (solid lines) gp120s equally well. As a control, the glycan-dependent PGT128 lost most of its binding to the endo H-treated gp120. These results indicate that the tested GB40 MAbs do not rely on gp120 glycans for binding. We also determined that GB40_b10 is directed to the inner domain of gp120, as suggested by its effective competition with biotin-labeled A32 (55, 56) (Fig. 6C, bottom left). Based on similar binding curves of GB40_b11 and GB40_b12 to AC10.29 WT, D368R, and W479A gp120s (Fig. 6C, top), we biotin labeled only GB40_b11 and GB40_b13 and examined GB40_b11 to GB40_b13 for cross-reactivity, as well as against the sheep polyclonal antibody D7324, known to target a conserved peptide in the C5 region of gp120 (Fig. 6C, bottom right). All three GB40 MAbs cross-competed, with GB40_b13 being most effective, as it has the best binding affinity to AC10.29 gp120. D7324, as a polyclonal antibody, was tested at a higher concentration (100 μg/ml) and was effective at competing against GB40_b11-biotin and GB40_b13-biotin. These results suggest that the epitopes of GB40_b11 to GB40_b13 overlap D7324 and involve gp120 C5. The V3 loop- and V3 stem-directed GB40 MAbs GB40_b1 to GB40_b9 neutralized tier 1 but generally not tier 2 strains (Table 3), including the homologous SHIVSF162P3N clones 8 and 10, which are most sensitive to GB40 plasma neutralization (Fig. 2, top). The non-V3-directed GB40 MAbs GB40_b10 to GB40_b13 lacked neutralizing activity against even tier 1 strains (Table 3). Therefore, the isolated gp120-reactive MAbs from GB40 are mainly V3 directed, with minimal cross-neutralizing activity.
FIG 6.
Isolation and characterization of GB40 MAbs. (A) B-cell staining and sorting from the PBMCs of GB40_75wpi by FACS. (B) ELISA and competition ELISA analyses of 8 GB40 MAbs directed to the V3 loop of gp120. (C) ELISA and competition ELISA analyses of 5 non-V3-loop-directed GB40 MAbs; the dashed lines in the top left graph show MAb binding curves to endo H-treated gp120.
Human anti-V3 MAbs have been associated with preferred use of the IGHV5-51 gene (57), which is also used by the only anti-V3 MAb isolated from AD358 (GB40_b7 [Table 2]). In this regard, the isolated macaque anti-V3 MAb GB40_b1, with three clonal variants, uses the rhesus VH5.46 gene (Table 2), which resembles the human IGVH5-51 gene, suggesting similarity between the human and macaque immunoglobulin genes used to encode some V3-directed MAbs.
DISCUSSION
Compared to chronically or long-term HIV-1-infected individuals, the development of bnAbs against tier 2 HIV-1 has rarely been detected in SHIV-infected macaques; this was also the case for the SHIVSF162P3N-infected rhesus macaques in this study. Several factors of current SHIV models may have contributed to this poor bnAb response in macaques. First, the number and genetic diversity of the available SHIV strains are limited compared to those of circulating HIV-1 strains. Consequently, the types of antibody responses induced by these limited SHIVs may be constrained as opposed to those induced by HIV-1 infections. Second, the duration of infection has been shorter for macaques. As the infected macaques have been typically followed for up to 2 years p.i., it is difficult to compare antibody responses in these animals with those in long-term-infected humans with a different course of infection, often lasting for more than 10 years. Third, viral loads are highly variable in macaques, with most animals failing to sustain viremia (58–60). Of 13 viremic macaques infected with SHIVSF162P3N, 11 (85%) were identified with homologous neutralizing titers and 5 (38%) with breadth, according to our definition for the tested HIV-1 strains. Since the macaque plasma samples were collected at 1 to 2 years p.i., we compared their neutralization profiles to those of the infected human plasma samples collected at 1 to 3 years p.i. Unlike plasma samples from chronic infection, the development of bnAbs in infected humans is also uncommon in the early course of infection. Among the plasma samples from 85 individuals who have been followed during the acute and early course of infection, we identified a total of 9 subjects (11%) with neutralization breadth and potency, but only 2 of them were from 1 to 3 years p.i. These numbers suggest that with specific SHIV strains, such as SHIVSF162P3N, studied here, and SHIVAD8, identified previously (5, 6), some infected macaques can sustain viremia and mount effective and timely bnAb responses against tier 2 HIV-1 strains. These results support the feasibility of developing SHIV models that consistently produce bnAbs. For this purpose, it would be of interest to track the bnAb maturation process in selected macaques, such as the animals FF69 and GB40 in this study and CE8J and CL5E from previous SHIVAD8 studies (5, 6), and to determine if inoculations with SHIVs expressing sequential Env clones from these animals reproduce similar bnAb responses.
Based on our prior success in mapping neutralizing antibody specificities and in isolating VRC01 and other CD4bs MAbs using a gp120 core-based probe, monomeric gp120s with either D368R or W479A mutations were generated to further characterize plasma samples with neutralization breadth. We recognize that while these probes were designed to bind and adsorb most gp120-directed antibodies, including those directed to CD4bs, removing one specificity in a competition assay may not be sufficient to cause decrease of the overall neutralizing activity of plasma that is likely to contain complex antibodies with diverse epitopes. With this caveat, only 2 of 9 human plasma samples, AD358 and AD359, and 2 of 4 macaque plasma samples, GB40 and FF59, were found to contain neutralizing antibodies directed to monomeric gp120, suggesting that the bulk of human and macaque bnAbs bind to the Env trimer (including gp41) rather than to the gp120 monomer. Characterization of the isolated gp120-reactive MAbs showed that 6 of 7 MAbs recovered from AD358 were directed to CD4bs, with 3 CD4bs-directed MAbs (AD358_n1 to AD358_n3) exhibiting neutralizing activity against JR-FL and the autologous Env strain AD358_m2. These CD4bs MAbs with limited cross-reactivity are clearly different from the VRC01 class or other CD4bs-directed bnAbs. Nevertheless, the “narrow” CD4bs-directed MAbs with autologous neutralizing activity may be important in shaping env evolution in vivo, as implied in a study (25) showing cooperation of two autologous neutralizing MAb lineages in driving env evolution and guiding the maturation of bnAbs. Moreover, their presence suggests that the levels of steric hindrance posed by the Env trimer to shield CD4bs vary among HIV-1 strains and/or between early and late Env variants within an infected individual. As these MAbs do not bind to RSC3 or cannot be distinguished by RSC3/ΔRSC3 binding, the D368R and W479A gp120 probes described here will be useful in identifying them.
The GB40 MAbs recovered from dual staining of gp120 W479A+ D368R+ B cells showed only tier 1 (GB40_b1 to GB40_b9) or no (GB40_b10 to GB40_b13) neutralizing activity, indicating that this dual staining with gp120s was not specific enough to select bnAbs from this macaque. Nonetheless, these rhesus gp120-reactive MAbs provided insights into the similarity in antibody responses between HIV-1 and SHIV infections. For example, 8 out of the 13 isolated GB40 MAbs are directed to the V3 loop. This is similar to the V3 immunodominance observed in HIV-1 infection (61, 62). Moreover, the macaque anti-V3 clone GB40_b1 uses the rhesus VH5.46 gene (Table 2), which resembles the human IGVH5-51 gene used preferentially to encode human anti-V3 MAbs (57). The MAb GB40_b10 cross-competed with the human MAb A32. Since A32 has been shown to mediate antibody-dependent cellular cytotoxicity (ADCC) (63), it would be of interest to determine whether GB40_b10 also mediates similar ADCC activity. Other GB40 MAbs (GB40_b11 to GB40_b13) mapped to the C5 region of gp120 may also be useful to replace D7324 to capture gp120 or gp140 for ELISA or Env immunogen purifications (51, 64–66), in particular GB40_b13, which has the highest binding affinity to gp120.
In summary, we have focused on identifying broadly neutralizing plasma samples from individuals with acute and early HIV-1 infection and from SHIVSF162P3N-infected rhesus macaques. We were able to identify broadly neutralizing human and rhesus plasma samples with specificities directed to monomeric gp120, but they are infrequent, and the B-cell staining with gp120 probes was not specific enough to isolate the corresponding bnAbs. Nonetheless, characterization and sequencing of the rhesus gp120-reactive MAbs provided insights into the similarity to their human counterparts. A better understanding of bnAb development as a function of time in SHIV-infected rhesus macaques and identification of sequential Env clones that are more efficient in driving bnAb responses should improve the use of this model for HIV-1 vaccine discovery. As neutralizing activity in most broadly neutralizing plasma samples does not appear to be directed to monomeric gp120, it remains to be determined if Env trimer probes would be more successful in isolating bnAbs from these human and rhesus subjects.
ACKNOWLEDGMENTS
We thank the participants in the ADARC Acute and Early Infection Program. We thank Andres Finzi for discussion of the gp120 W479A mutation. We thank Eric Waltari for assistance with the macaque antibody sequence analysis and for proofreading of the manuscript. We thank Vincent Sahi for assistance with B-cell sorting and Leslie St. Bernard for technical support.
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
REFERENCES
- 1.Burton DR, Mascola JR. 2015. Antibody responses to envelope glycoproteins in HIV-1 infection. Nat Immunol 16:571–576. doi: 10.1038/ni.3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwong PD, Mascola JR. 2012. Human antibodies that neutralize HIV-1: identification, structures, and B cell ontogenies. Immunity 37:412–425. doi: 10.1016/j.immuni.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hraber P, Seaman MS, Bailer RT, Mascola JR, Montefiori DC, Korber BT. 2014. Prevalence of broadly neutralizing antibody responses during chronic HIV-1 infection. AIDS 28:163–169. doi: 10.1097/QAD.0000000000000106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lifson JD, Haigwood NL. 2012. Lessons in nonhuman primate models for AIDS vaccine research: from minefields to milestones. Cold Spring Harb Perspect Med 2:a007310. doi: 10.1101/cshperspect.a007310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walker LM, Sok D, Nishimura Y, Donau O, Sadjadpour R, Gautam R, Shingai M, Pejchal R, Ramos A, Simek MD, Geng Y, Wilson IA, Poignard P, Martin MA, Burton DR. 2011. Rapid development of glycan-specific, broad, and potent anti-HIV-1 gp120 neutralizing antibodies in an R5 SIV/HIV chimeric virus infected macaque. Proc Natl Acad Sci U S A 108:20125–20129. doi: 10.1073/pnas.1117531108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shingai M, Donau OK, Schmidt SD, Gautam R, Plishka RJ, Buckler-White A, Sadjadpour R, Lee WR, LaBranche CC, Montefiori DC, Mascola JR, Nishimura Y, Martin MA. 2012. Most rhesus macaques infected with the CCR5-tropic SHIV(AD8) generate cross-reactive antibodies that neutralize multiple HIV-1 strains. Proc Natl Acad Sci U S A 109:19769–19774. doi: 10.1073/pnas.1217443109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Montefiori DC, Reimann KA, Wyand MS, Manson K, Lewis MG, Collman RG, Sodroski JG, Bolognesi DP, Letvin NL. 1998. Neutralizing antibodies in sera from macaques infected with chimeric simian-human immunodeficiency virus containing the envelope glycoproteins of either a laboratory-adapted variant or a primary isolate of human immunodeficiency virus type 1. J Virol 72:3427–3431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kraft Z, Derby NR, McCaffrey RA, Niec R, Blay WM, Haigwood NL, Moysi E, Saunders CJ, Wrin T, Petropoulos CJ, McElrath MJ, Stamatatos L. 2007. Macaques infected with a CCR5-tropic simian/human immunodeficiency virus (SHIV) develop broadly reactive anti-HIV neutralizing antibodies. J Virol 81:6402–6411. doi: 10.1128/JVI.00424-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamamoto T, Lynch RM, Gautam R, Matus-Nicodemos R, Schmidt SD, Boswell KL, Darko S, Wong P, Sheng Z, Petrovas C, McDermott AB, Seder RA, Keele BF, Shapiro L, Douek DC, Nishimura Y, Mascola JR, Martin MA, Koup RA. 2015. Quality and quantity of TFH cells are critical for broad antibody development in SHIVAD8 infection. Sci Transl Med 7:298ra120. doi: 10.1126/scitranslmed.aab3964. [DOI] [PubMed] [Google Scholar]
- 10.Ho SH, Tasca S, Shek L, Li A, Gettie A, Blanchard J, Boden D, Cheng-Mayer C. 2007. Coreceptor switch in R5-tropic simian/human immunodeficiency virus-infected macaques. J Virol 81:8621–8633. doi: 10.1128/JVI.00759-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ren W, Tasca S, Zhuang K, Gettie A, Blanchard J, Cheng-Mayer C. 2010. Different tempo and anatomic location of dual-tropic and X4 virus emergence in a model of R5 simian-human immunodeficiency virus infection. J Virol 84:340–351. doi: 10.1128/JVI.01865-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mumbauer A, Gettie A, Blanchard J, Cheng-Mayer C. 2013. Efficient mucosal transmissibility but limited pathogenicity of R5 SHIV SF162P3N in Chinese-origin rhesus macaques. J Acquir Immune Defic Syndr 62:496–504. doi: 10.1097/QAI.0b013e31827f1c11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shakirzyanova M, Tsai L, Ren W, Gettie A, Blanchard J, Cheng-Mayer C. 2012. Pathogenic consequences of vaginal infection with CCR5-tropic simian-human immunodeficiency virus SHIVSF162P3N. J Virol 86:9432–9442. doi: 10.1128/JVI.00852-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ren W, Mumbauer A, Zhuang K, Harbison C, Knight H, Westmoreland S, Gettie A, Blanchard J, Cheng-Mayer C. 2013. Mucosal transmissibility, disease induction and coreceptor switching of R5 SHIVSF162P3N molecular clones in rhesus macaques. Retrovirology 10:9. doi: 10.1186/1742-4690-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gray ES, Madiga MC, Hermanus T, Moore PL, Wibmer CK, Tumba NL, Werner L, Mlisana K, Sibeko S, Williamson C, Abdool Karim SS, Morris L, CAPRISA002 Study Team . 2011. The neutralization breadth of HIV-1 develops incrementally over four years and is associated with CD4+ T cell decline and high viral load during acute infection. J Virol 85:4828–4840. doi: 10.1128/JVI.00198-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Simek MD, Rida W, Priddy FH, Pung P, Carrow E, Laufer DS, Lehrman JK, Boaz M, Tarragona-Fiol T, Miiro G, Birungi J, Pozniak A, McPhee DA, Manigart O, Karita E, Inwoley A, Jaoko W, Dehovitz J, Bekker LG, Pitisuttithum P, Paris R, Walker LM, Poignard P, Wrin T, Fast PE, Burton DR, Koff WC. 2009. Human immunodeficiency virus type 1 elite neutralizers: individuals with broad and potent neutralizing activity identified by using a high-throughput neutralization assay together with an analytical selection algorithm. J Virol 83:7337–7348. doi: 10.1128/JVI.00110-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doria-Rose NA, Klein RM, Daniels MG, O'Dell S, Nason M, Lapedes A, Bhattacharya T, Migueles SA, Wyatt RT, Korber BT, Mascola JR, Connors M. 2010. Breadth of human immunodeficiency virus-specific neutralizing activity in sera: clustering analysis and association with clinical variables. J Virol 84:1631–1636. doi: 10.1128/JVI.01482-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doria-Rose NA, Klein RM, Manion MM, O'Dell S, Phogat A, Chakrabarti B, Hallahan CW, Migueles SA, Wrammert J, Ahmed R, Nason M, Wyatt RT, Mascola JR, Connors M. 2009. Frequency and phenotype of human immunodeficiency virus envelope-specific B cells from patients with broadly cross-neutralizing antibodies. J Virol 83:188–199. doi: 10.1128/JVI.01583-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lynch RM, Rong R, Boliar S, Sethi A, Li B, Mulenga J, Allen S, Robinson JE, Gnanakaran S, Derdeyn CA. 2011. The B cell response is redundant and highly focused on V1V2 during early subtype C infection in a Zambian seroconverter. J Virol 85:905–915. doi: 10.1128/JVI.02006-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lynch RM, Tran L, Louder MK, Schmidt SD, Cohen M, Dersimonian R, Euler Z, Gray ES, Abdool Karim S, Kirchherr J, Montefiori DC, Sibeko S, Soderberg K, Tomaras G, Yang ZY, Nabel GJ, Schuitemaker H, Morris L, Haynes BF, Mascola JR. 2012. The development of CD4 binding site antibodies during HIV-1 infection. J Virol 86:7588–7595. doi: 10.1128/JVI.00734-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mikell I, Sather DN, Kalams SA, Altfeld M, Alter G, Stamatatos L. 2011. Characteristics of the earliest cross-neutralizing antibody response to HIV-1. PLoS Pathog 7:e1001251. doi: 10.1371/journal.ppat.1001251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gray ES, Moody MA, Wibmer CK, Chen X, Marshall D, Amos J, Moore PL, Foulger A, Yu JS, Lambson B, Abdool Karim S, Whitesides J, Tomaras GD, Haynes BF, Morris L, Liao HX. 2011. Isolation of a monoclonal antibody that targets the alpha-2 helix of gp120 and represents the initial autologous neutralizing-antibody response in an HIV-1 subtype C-infected individual. J Virol 85:7719–7729. doi: 10.1128/JVI.00563-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liao HX, Lynch R, Zhou T, Gao F, Alam SM, Boyd SD, Fire AZ, Roskin KM, Schramm CA, Zhang Z, Zhu J, Shapiro L, NISC Comparative Sequencing Program, Mullikin JC, Gnanakaran S, Hraber P, Wiehe K, Kelsoe G, Yang G, Xia SM, Montefiori DC, Parks R, Lloyd KE, Scearce RM, Soderberg KA, Cohen M, Kamanga G, Louder MK, Tran LM, Chen Y, Cai F, Chen S, Moquin S, Du X, Joyce MG, Srivatsan S, Zhang B, Zheng A, Shaw GM, Hahn BH, Kepler TB, Korber BT, Kwong PD, Mascola JR, Haynes BF. 2013. Co-evolution of a broadly neutralizing HIV-1 antibody and founder virus. Nature 496:469–476. doi: 10.1038/nature12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doria-Rose NA, Schramm CA, Gorman J, Moore PL, Bhiman JN, DeKosky BJ, Ernandes MJ, Georgiev IS, Kim HJ, Pancera M, Staupe RP, Altae-Tran HR, Bailer RT, Crooks ET, Cupo A, Druz A, Garrett NJ, Hoi KH, Kong R, Louder MK, Longo NS, McKee K, Nonyane M, O'Dell S, Roark RS, Rudicell RS, Schmidt SD, Sheward DJ, Soto C, Wibmer CK, Yang Y, Zhang Z, NISC Comparative Sequencing Program, Mullikin JC, Binley JM, Sanders RW, Wilson IA, Moore JP, Ward AB, Georgiou G, Williamson C, Abdool Karim SS, Morris L, Kwong PD, Shapiro L, Mascola JR, Becker J, Benjamin B, Blakesley R, Bouffard G, Brooks S, Coleman H, Dekhtyar M, Gregory M, Guan X, Gupta J, Han J, Hargrove A, Ho SL, Johnson T, Legaspi R, Lovett S, Maduro Q, Masiello C, Maskeri B, McDowell J, Montemayor C, Mullikin J, Park M, Riebow N, Schandler K, Schmidt B, Sison C, Stantripop M, Thomas J, Thomas P, Vemulapalli M, Young A. 2014. Developmental pathway for potent V1V2-directed HIV-neutralizing antibodies. Nature 509:55–62. doi: 10.1038/nature13036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gao F, Bonsignori M, Liao HX, Kumar A, Xia SM, Lu X, Cai F, Huang KK, Song H, Zhou T, Lynch R, Alam SM, Moody MA, Ferrari G, Berrong M, Kelsoe G, Shaw GM, Hahn BH, Montefiori DC, Kamanga G, Cohen MS, Hraber P, Kwong PD, Korber BT, Mascola JR, Kepler TB, Haynes BF. 2014. Cooperation of B-cell lineages in induction of HIV-1 broadly neutralizing antibodies. Cell 158:481–491. doi: 10.1016/j.cell.2014.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salazar-Gonzalez JF, Salazar MG, Keele BF, Learn GH, Giorgi EE, Li H, Decker JM, Wang S, Baalwa J, Kraus MH, Parrish NF, Shaw KS, Guffey MB, Bar KJ, Davis KL, Ochsenbauer-Jambor C, Kappes JC, Saag MS, Cohen MS, Mulenga J, Derdeyn CA, Allen S, Hunter E, Markowitz M, Hraber P, Perelson AS, Bhattacharya T, Haynes BF, Korber BT, Hahn BH, Shaw GM. 2009. Genetic identity, biological phenotype, and evolutionary pathways of transmitted/founder viruses in acute and early HIV-1 infection. J Exp Med 206:1273–1289. doi: 10.1084/jem.20090378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li H, Bar KJ, Wang S, Decker JM, Chen Y, Sun C, Salazar-Gonzalez JF, Salazar MG, Learn GH, Morgan CJ, Schumacher JE, Hraber P, Giorgi EE, Bhattacharya T, Korber BT, Perelson AS, Eron JJ, Cohen MS, Hicks CB, Haynes BF, Markowitz M, Keele BF, Hahn BH, Shaw GM. 2010. High multiplicity infection by HIV-1 in men who have sex with men. PLoS Pathog 6:e1000890. doi: 10.1371/journal.ppat.1000890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liao HX, Chen X, Munshaw S, Zhang R, Marshall DJ, Vandergrift N, Whitesides JF, Lu X, Yu JS, Hwang KK, Gao F, Markowitz M, Heath SL, Bar KJ, Goepfert PA, Montefiori DC, Shaw GC, Alam SM, Margolis DM, Denny TN, Boyd SD, Marshal E, Egholm M, Simen BB, Hanczaruk B, Fire AZ, Voss G, Kelsoe G, Tomaras GD, Moody MA, Kepler TB, Haynes BF. 2011. Initial antibodies binding to HIV-1 gp41 in acutely infected subjects are polyreactive and highly mutated. J Exp Med 208:2237–2249. doi: 10.1084/jem.20110363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu X, Yang ZY, Li Y, Hogerkorp CM, Schief WR, Seaman MS, Zhou T, Schmidt SD, Wu L, Xu L, Longo NS, McKee K, O'Dell S, Louder MK, Wycuff DL, Feng Y, Nason M, Doria-Rose N, Connors M, Kwong PD, Roederer M, Wyatt RT, Nabel GJ, Mascola JR. 2010. Rational design of envelope identifies broadly neutralizing human monoclonal antibodies to HIV-1. Science 329:856–861. doi: 10.1126/science.1187659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu X, Zhou T, Zhu J, Zhang B, Georgiev I, Wang C, Chen X, Longo NS, Louder M, McKee K, O'Dell S, Perfetto S, Schmidt SD, Shi W, Wu L, Yang Y, Yang ZY, Yang Z, Zhang Z, Bonsignori M, Crump JA, Kapiga SH, Sam NE, Haynes BF, Simek M, Burton DR, Koff WC, Doria-Rose NA, Connors M, NISC Comparative Sequencing Program, Mullikin JC, Nabel GJ, Roederer M, Shapiro L, Kwong PD, Mascola JR. 2011. Focused evolution of HIV-1 neutralizing antibodies revealed by structures and deep sequencing. Science 333:1593–1602. doi: 10.1126/science.1207532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou T, Zhu J, Wu X, Moquin S, Zhang B, Acharya P, Georgiev IS, Altae-Tran HR, Chuang GY, Joyce MG, Do Kwon Y, Longo NS, Louder MK, Luongo T, McKee K, Schramm CA, Skinner J, Yang Y, Yang Z, Zhang Z, Zheng A, Bonsignori M, Haynes BF, Scheid JF, Nussenzweig MC, Simek M, Burton DR, Koff WC, Mullikin JC, Connors M, Shapiro L, Nabel GJ, Mascola JR, Kwong PD. 2013. Multidonor analysis reveals structural elements, genetic determinants, and maturation pathway for HIV-1 neutralization by VRC01-class antibodies. Immunity 39:245–258. doi: 10.1016/j.immuni.2013.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou T, Lynch RM, Chen L, Acharya P, Wu X, Doria-Rose NA, Joyce MG, Lingwood D, Soto C, Bailer RT, Ernandes MJ, Kong R, Longo NS, Louder MK, McKee K, O'Dell S, Schmidt SD, Tran L, Yang Z, Druz A, Luongo TS, Moquin S, Srivatsan S, Yang Y, Zhang B, Zheng A, Pancera M, Kirys T, Georgiev IS, Gindin T, Peng HP, Yang AS, Mullikin JC, Gray MD, Stamatatos L, Burton DR, Koff WC, Cohen MS, Haynes BF, Casazza JP, Connors M, Corti D, Lanzavecchia A, Sattentau QJ, Weiss RA, West AP Jr, Bjorkman PJ, Scheid JF, Nussenzweig MC, Shapiro L, Mascola JR, Kwong PD. 2015. Structural repertoire of HIV-1-neutralizing antibodies targeting the CD4 supersite in 14 donors. Cell 161:1280–1292. doi: 10.1016/j.cell.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Walker LM, Huber M, Doores KJ, Falkowska E, Pejchal R, Julien JP, Wang SK, Ramos A, Chan-Hui PY, Moyle M, Mitcham JL, Hammond PW, Olsen OA, Phung P, Fling S, Wong CH, Phogat S, Wrin T, Simek MD, Protocol G Principal Investigators, Koff WC, Wilson IA, Burton DR, Poignard P. 2011. Broad neutralization coverage of HIV by multiple highly potent antibodies. Nature 477:466–470. doi: 10.1038/nature10373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tiller T, Meffre E, Yurasov S, Tsuiji M, Nussenzweig MC, Wardemann H. 2008. Efficient generation of monoclonal antibodies from single human B cells by single cell RT-PCR and expression vector cloning. J Immunol Methods 329:112–124. doi: 10.1016/j.jim.2007.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wei X, Decker JM, Liu H, Zhang Z, Arani RB, Kilby JM, Saag MS, Wu X, Shaw GM, Kappes JC. 2002. Emergence of resistant human immunodeficiency virus type 1 in patients receiving fusion inhibitor (T-20) monotherapy. Antimicrob Agents Chemother 46:1896–1905. doi: 10.1128/AAC.46.6.1896-1905.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wei X, Decker JM, Wang S, Hui H, Kappes JC, Wu X, Salazar-Gonzalez JF, Salazar MG, Kilby JM, Saag MS, Komarova NL, Nowak MA, Hahn BH, Kwong PD, Shaw GM. 2003. Antibody neutralization and escape by HIV-1. Nature 422:307–312. doi: 10.1038/nature01470. [DOI] [PubMed] [Google Scholar]
- 37.Li M, Gao F, Mascola JR, Stamatatos L, Polonis VR, Koutsoukos M, Voss G, Goepfert P, Gilbert P, Greene KM, Bilska M, Kothe DL, Salazar-Gonzalez JF, Wei X, Decker JM, Hahn BH, Montefiori DC. 2005. Human immunodeficiency virus type 1 env clones from acute and early subtype B infections for standardized assessments of vaccine-elicited neutralizing antibodies. J Virol 79:10108–10125. doi: 10.1128/JVI.79.16.10108-10125.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li M, Salazar-Gonzalez JF, Derdeyn CA, Morris L, Williamson C, Robinson JE, Decker JM, Li Y, Salazar MG, Polonis VR, Mlisana K, Karim SA, Hong K, Greene KM, Bilska M, Zhou J, Allen S, Chomba E, Mulenga J, Vwalika C, Gao F, Zhang M, Korber BT, Hunter E, Hahn BH, Montefiori DC. 2006. Genetic and neutralization properties of subtype C human immunodeficiency virus type 1 molecular env clones from acute and early heterosexually acquired infections in Southern Africa. J Virol 80:11776–11790. doi: 10.1128/JVI.01730-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Long EM, Rainwater SM, Lavreys L, Mandaliya K, Overbaugh J. 2002. HIV type 1 variants transmitted to women in Kenya require the CCR5 coreceptor for entry, regardless of the genetic complexity of the infecting virus. AIDS Res Hum Retroviruses 18:567–576. doi: 10.1089/088922202753747914. [DOI] [PubMed] [Google Scholar]
- 40.Blish CA, Jalalian-Lechak Z, Rainwater S, Nguyen MA, Dogan OC, Overbaugh J. 2009. Cross-subtype neutralization sensitivity despite monoclonal antibody resistance among early subtype A, C, and D envelope variants of human immunodeficiency virus type 1. J Virol 83:7783–7788. doi: 10.1128/JVI.00673-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Keele BF, Giorgi EE, Salazar-Gonzalez JF, Decker JM, Pham KT, Salazar MG, Sun C, Grayson T, Wang S, Li H, Wei X, Jiang C, Kirchherr JL, Gao F, Anderson JA, Ping LH, Swanstrom R, Tomaras GD, Blattner WA, Goepfert PA, Kilby JM, Saag MS, Delwart EL, Busch MP, Cohen MS, Montefiori DC, Haynes BF, Gaschen B, Athreya GS, Lee HY, Wood N, Seoighe C, Perelson AS, Bhattacharya T, Korber BT, Hahn BH, Shaw GM. 2008. Identification and characterization of transmitted and early founder virus envelopes in primary HIV-1 infection. Proc Natl Acad Sci U S A 105:7552–7557. doi: 10.1073/pnas.0802203105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Salazar-Gonzalez JF, Bailes E, Pham KT, Salazar MG, Guffey MB, Keele BF, Derdeyn CA, Farmer P, Hunter E, Allen S, Manigart O, Mulenga J, Anderson JA, Swanstrom R, Haynes BF, Athreya GS, Korber BT, Sharp PM, Shaw GM, Hahn BH. 2008. Deciphering human immunodeficiency virus type 1 transmission and early envelope diversification by single-genome amplification and sequencing. J Virol 82:3952–3970. doi: 10.1128/JVI.02660-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu X, Wang C, O'Dell S, Li Y, Keele BF, Yang Z, Imamichi H, Doria-Rose N, Hoxie JA, Connors M, Shaw GM, Wyatt RT, Mascola JR. 2012. Selection pressure on HIV-1 envelope by broadly neutralizing antibodies to the conserved CD4-binding site. J Virol 86:5844–5856. doi: 10.1128/JVI.07139-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li Y, Migueles SA, Welcher B, Svehla K, Phogat A, Louder MK, Wu X, Shaw GM, Connors M, Wyatt RT, Mascola JR. 2007. Broad HIV-1 neutralization mediated by CD4-binding site antibodies. Nat Med 13:1032–1034. doi: 10.1038/nm1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Desormeaux A, Coutu M, Medjahed H, Pacheco B, Herschhorn A, Gu C, Xiang SH, Mao Y, Sodroski J, Finzi A. 2013. The highly conserved layer-3 component of the HIV-1 gp120 inner domain is critical for CD4-required conformational transitions. J Virol 87:2549–2562. doi: 10.1128/JVI.03104-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Scheid JF, Mouquet H, Ueberheide B, Diskin R, Klein F, Oliveira TY, Pietzsch J, Fenyo D, Abadir A, Velinzon K, Hurley A, Myung S, Boulad F, Poignard P, Burton DR, Pereyra F, Ho DD, Walker BD, Seaman MS, Bjorkman PJ, Chait BT, Nussenzweig MC. 2011. Sequence and structural convergence of broad and potent HIV antibodies that mimic CD4 binding. Science 333:1633–1637. doi: 10.1126/science.1207227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ye J, Ma N, Madden TL, Ostell JM. 2013. IgBLAST: an immunoglobulin variable domain sequence analysis tool. Nucleic Acids Res 41:W34–W40. doi: 10.1093/nar/gkt382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sundling C, Li Y, Huynh N, Poulsen C, Wilson R, O'Dell S, Feng Y, Mascola JR, Wyatt RT, Karlsson Hedestam GB. 2012. High-resolution definition of vaccine-elicited B cell responses against the HIV primary receptor binding site. Sci Transl Med 4:142ra96. doi: 10.1126/scitranslmed.3003752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Francica JR, Sheng Z, Zhang Z, Nishimura Y, Shingai M, Ramesh A, Keele BF, Schmidt SD, Flynn BJ, Darko S, Lynch RM, Yamamoto T, Matus-Nicodemos R, Wolinsky D, Nason M, Valiante NM, Malyala P, De Gregorio E, Barnett SW, Singh M, O'Hagan DT, Koup RA, Mascola JR, Martin MA, Kepler TB, Douek DC, Shapiro L, Seder RA. 2015. Analysis of immunoglobulin transcripts and hypermutation following SHIV(AD8) infection and protein-plus-adjuvant immunization. Nat Commun 6:6565. doi: 10.1038/ncomms7565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Seaman MS, Janes H, Hawkins N, Grandpre LE, Devoy C, Giri A, Coffey RT, Harris L, Wood B, Daniels MG, Bhattacharya T, Lapedes A, Polonis VR, McCutchan FE, Gilbert PB, Self SG, Korber BT, Montefiori DC, Mascola JR. 2010. Tiered categorization of a diverse panel of HIV-1 Env pseudoviruses for assessment of neutralizing antibodies. J Virol 84:1439–1452. doi: 10.1128/JVI.02108-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sanders RW, van Gils MJ, Derking R, Sok D, Ketas TJ, Burger JA, Ozorowski G, Cupo A, Simonich C, Goo L, Arendt H, Kim HJ, Lee JH, Pugach P, Williams M, Debnath G, Moldt B, van Breemen MJ, Isik G, Medina-Ramirez M, Back JW, Koff WC, Julien JP, Rakasz EG, Seaman MS, Guttman M, Lee KK, Klasse PJ, LaBranche C, Schief WR, Wilson IA, Overbaugh J, Burton DR, Ward AB, Montefiori DC, Dean H, Moore JP. 2015. HIV-1 neutralizing antibodies induced by native-like envelope trimers. Science 349:aac4223. doi: 10.1126/science.aac4223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Corti D, Langedijk JP, Hinz A, Seaman MS, Vanzetta F, Fernandez-Rodriguez BM, Silacci C, Pinna D, Jarrossay D, Balla-Jhagjhoorsingh S, Willems B, Zekveld MJ, Dreja H, O'Sullivan E, Pade C, Orkin C, Jeffs SA, Montefiori DC, Davis D, Weissenhorn W, McKnight A, Heeney JL, Sallusto F, Sattentau QJ, Weiss RA, Lanzavecchia A. 2010. Analysis of memory B cell responses and isolation of novel monoclonal antibodies with neutralizing breadth from HIV-1-infected individuals. PLoS One 5:e8805. doi: 10.1371/journal.pone.0008805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Freund NT, Horwitz JA, Nogueira L, Sievers SA, Scharf L, Scheid JF, Gazumyan A, Liu C, Velinzon K, Goldenthal A, Sanders RW, Moore JP, Bjorkman PJ, Seaman MS, Walker BD, Klein F, Nussenzweig MC. 2015. A New glycan-dependent CD4-binding site neutralizing antibody exerts pressure on HIV-1 in vivo. PLoS Pathog 11:e1005238. doi: 10.1371/journal.ppat.1005238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pejchal R, Doores KJ, Walker LM, Khayat R, Huang PS, Wang SK, Stanfield RL, Julien JP, Ramos A, Crispin M, Depetris R, Katpally U, Marozsan A, Cupo A, Maloveste S, Liu Y, McBride R, Ito Y, Sanders RW, Ogohara C, Paulson JC, Feizi T, Scanlan CN, Wong CH, Moore JP, Olson WC, Ward AB, Poignard P, Schief WR, Burton DR, Wilson IA. 2011. A potent and broad neutralizing antibody recognizes and penetrates the HIV glycan shield. Science 334:1097–1103. doi: 10.1126/science.1213256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moore JP, McCutchan FE, Poon SW, Mascola J, Liu J, Cao Y, Ho DD. 1994. Exploration of antigenic variation in gp120 from clades A through F of human immunodeficiency virus type 1 by using monoclonal antibodies. J Virol 68:8350–8364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pancera M, Majeed S, Ban YE, Chen L, Huang CC, Kong L, Kwon YD, Stuckey J, Zhou T, Robinson JE, Schief WR, Sodroski J, Wyatt R, Kwong PD. 2010. Structure of HIV-1 gp120 with gp41-interactive region reveals layered envelope architecture and basis of conformational mobility. Proc Natl Acad Sci U S A 107:1166–1171. doi: 10.1073/pnas.0911004107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gorny MK, Wang XH, Williams C, Volsky B, Revesz K, Witover B, Burda S, Urbanski M, Nyambi P, Krachmarov C, Pinter A, Zolla-Pazner S, Nadas A. 2009. Preferential use of the VH5-51 gene segment by the human immune response to code for antibodies against the V3 domain of HIV-1. Mol Immunol 46:917–926. doi: 10.1016/j.molimm.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Harouse JM, Gettie A, Eshetu T, Tan RC, Bohm R, Blanchard J, Baskin G, Cheng-Mayer C. 2001. Mucosal transmission and induction of simian AIDS by CCR5-specific simian/human immunodeficiency virus SHIV(SF162P3). J Virol 75:1990–1995. doi: 10.1128/JVI.75.4.1990-1995.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pahar B, Wang X, Dufour J, Lackner AA, Veazey RS. 2007. Virus-specific T cell responses in macaques acutely infected with SHIV(sf162p3). Virology 363:36–47. doi: 10.1016/j.virol.2007.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chenine AL, Siddappa NB, Kramer VG, Sciaranghella G, Rasmussen RA, Lee SJ, Santosuosso M, Poznansky MC, Velu V, Amara RR, Souder C, Anderson DC, Villinger F, Else JG, Novembre FJ, Strobert E, O'Neil SP, Secor WE, Ruprecht RM. 2010. Relative transmissibility of an R5 clade C simian-human immunodeficiency virus across different mucosae in macaques parallels the relative risks of sexual HIV-1 transmission in humans via different routes. J Infect Dis 201:1155–1163. doi: 10.1086/651274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Javaherian K, Langlois AJ, McDanal C, Ross KL, Eckler LI, Jellis CL, Profy AT, Rusche JR, Bolognesi DP, Putney SD. 1989. Principal neutralizing domain of the human immunodeficiency virus type 1 envelope protein. Proc Natl Acad Sci U S A 86:6768–6772. doi: 10.1073/pnas.86.17.6768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Spear GT, Takefman DM, Sharpe S, Ghassemi M, Zolla-Pazner S. 1994. Antibodies to the HIV-1 V3 loop in serum from infected persons contribute a major proportion of immune effector functions including complement activation, antibody binding, and neutralization. Virology 204:609–615. doi: 10.1006/viro.1994.1575. [DOI] [PubMed] [Google Scholar]
- 63.Ferrari G, Pollara J, Kozink D, Harms T, Drinker M, Freel S, Moody MA, Alam SM, Tomaras GD, Ochsenbauer C, Kappes JC, Shaw GM, Hoxie JA, Robinson JE, Haynes BF. 2011. An HIV-1 gp120 envelope human monoclonal antibody that recognizes a C1 conformational epitope mediates potent antibody-dependent cellular cytotoxicity (ADCC) activity and defines a common ADCC epitope in human HIV-1 serum. J Virol 85:7029–7036. doi: 10.1128/JVI.00171-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Moore JP, Cao Y, Ho DD, Koup RA. 1994. Development of the anti-gp120 antibody response during seroconversion to human immunodeficiency virus type 1. J Virol 68:5142–5155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wu X, Zhou T, O'Dell S, Wyatt RT, Kwong PD, Mascola JR. 2009. Mechanism of human immunodeficiency virus type 1 resistance to monoclonal antibody B12 that effectively targets the site of CD4 attachment. J Virol 83:10892–10907. doi: 10.1128/JVI.01142-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sanders RW, Derking R, Cupo A, Julien JP, Yasmeen A, de Val N, Kim HJ, Blattner C, de la Pena AT, Korzun J, Golabek M, de Los Reyes K, Ketas TJ, van Gils MJ, King CR, Wilson IA, Ward AB, Klasse PJ, Moore JP. 2013. A next-generation cleaved, soluble HIV-1 Env Trimer, BG505 SOSIP.664 gp140, expresses multiple epitopes for broadly neutralizing but not non-neutralizing antibodies. PLoS Pathog 9:e1003618. doi: 10.1371/journal.ppat.1003618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kabat EA, Wu TT, Perry HM, Gottesman KS, Foeller C. 1991. Sequences of proteins of immunological interest, 5th ed. NIH publication no. 91-3242. National Institutes of Health, U.S. Department of Health and Human Services, Bethesda, MD. [Google Scholar]