Abstract
Background
Transvaginal measurement of cervical length has been advocated as a screening tool to prevent preterm birth, but controversy remains regarding the overall utility of universal screening.
Objective
We aimed to evaluate the acceptability of a universal cervical length screening program. Additionally we evaluated risk factors associated with declining screening and subsequent delivery outcomes of women who accepted or declined screening.
Study Design
This was a retrospective cohort study of transvaginal cervical length screening at a single institution between July 1, 2011 and December 31, 2014. Institutional protocol recommended transvaginal cervical length measurement at the time of anatomic survey between 17 – 23 weeks in all women with singleton, viable pregnancies, without current or planned cerclage, with patients able to opt-out. Patients with cervical length ≤ 20 mm were considered to have clinically significant cervical shortening and were offered treatment. We assessed acceptance rate, risk factors for declining cervical length screening, and the trend of acceptance of cervical length screening over time. We also calculated the prevalence of cervical length ≤ 25, ≤ 20, and ≤ 15 mm, and estimated the association between cervical length screening and spontaneous preterm birth.
Results
Of 12,740 women undergoing anatomic survey during the study period, 10,871 (85.3%, 95% CI 84.7%, 85.9%) underwent cervical length screening. Of those, 215 (2.0%) had a cervical length ≤25 millimeters and 131 (1.2%) had a cervical length ≤20 millimeters. After the first six months of implementation, there was no change in rates of acceptance of cervical length screening over time (p for trend=0.15). Women were more likely to decline cervical length screening if they were African American (aOR 2.17 95% CI 1.93,2.44), obese (aOR 1.18, 95% CI 1.06,1.31), multiparous (aOR 1.45, 95% CI 1.29,1.64), younger than 35 years (aOR 1.24, 95% CI 1.08,1.43), or smoked (aOR 1.42, 95% CI 1.20,1.68). Rates of spontaneous preterm birth before 28 weeks were higher in those who declined cervical length screening (aOR 2.01, 95% CI 1.33, 3.02).
Conclusion
Universal cervical length screening was implemented successfully with 85% of women screened. Overall incidence of short cervix was low and women with significant risk factors for preterm birth were more likely to decline screening. Patients who declined cervical length screening were more likely to be African American, obese, multiparous, younger than age 35, and to smoke. Rates of early, but not late, spontaneous preterm birth were significantly higher among women who did not undergo cervical length screening.
Keywords: Cervical length measurement, cervical length screening, preterm birth prevention, preterm birth, vaginal progesterone
Introduction
The incidence of preterm birth in the United States has remained stable despite efforts aimed at preterm birth reduction.1 Of the nearly 400,000 babies delivered prematurely annually, approximately two-thirds are spontaneous preterm births, with an estimated 15% occurring in women with a history of preterm birth. 2, 3 There remains an urgent need to develop effective strategies for screening and prevention of preterm birth among those with and without a history of preterm birth.
Women who are identified as having a short cervix in the midtrimester are at increased risk of delivering preterm.4 Recent studies have shown vaginal progesterone reduces the incidence of spontaneous preterm birth prior to 34 weeks gestation by approximately 45% in women with a short cervix.5, 6 With potentially effective treatments available, many have advocated for implementation of universal transvaginal cervical length (TVCL) screening to identify women at risk of preterm birth. However, controversy exists over the utility of TVCL screening in low risk patients. Advocates for TVCL screening point to the efficacy of interventions when short cervix is identified, the potential cost-effectiveness of screening, and the limited harm with TVCL screening.7–9 Opponents question the standardization and reproducibility of TVCL measurement, whether screening and intervention will provide meaningful risk reduction and remain cost effective outside of clinical trials, and raise concerns regarding “indication creep,” with increasing interventions in situations where benefit is unproven.10 In spite of this controversy, there has been rapid uptake of TVCL screening programs, with the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal and Fetal Medicine (SMFM) publishing clinical guidelines suggesting, but not mandating, implementation of universal TVCL screening and treatment with either vaginal progesterone or cerclage as indicated if the cervix is short.11, 12 To date, there have been few publications on the implementation of a universal cervical length screening program, uptake among patients, and effectiveness of universal transvaginal cervical length screening.13–16
Our primary aim was to evaluate the acceptability and uptake of a universal transvaginal cervical length screening program. Our secondary aim was to evaluate risk factors associated with declining cervical length measurement. Additionally, we evaluated the likelihood of preterm delivery in women who declined cervical length measurement as compared to women who accepted cervical length measurement.
Materials and Methods
We conducted a retrospective cohort study of all patients undergoing anatomy screening in the midtrimester at a single institution between July 1, 2011 and December 31, 2014. Beginning in July 2011, institutional protocol recommended TVCL measurement in all women with singleton, viable pregnancies, without current or planned cerclage at the time of anatomic survey performed between 17 0/7 weeks and 23 6/7 weeks gestation, with patients able to opt-out if they desired. The study was conducted after approval from the Washington University School of Medicine Human Research Protection Office.
Cervical length measurements are performed by trained ultrasonographers using the standard technique.17, 18 Briefly, after the patients’ bladder has been emptied, the probe is inserted into the anterior fornix of the vagina. A sagittal view of the cervix is obtained with a long axis view of the echogenic endocervical mucosa along the length of the cervical canal. The probe is withdrawn until the image is blurred and then reinserted, avoiding excessive pressure. The image is enlarged to occupy two-thirds of the screen and three measurements are obtained from the internal to external os along the entire endocervical canal, with the shortest, best measurement used.
Patients with cervical length ≤ 20 mm were considered to have clinically significant cervical shortening and offered treatment. Women with cervical length between 21 and 25 mm were considered to have borderline short cervix and returned for repeat cervical length measurements prior to 24 weeks. For the purposes of this study, only the shortest cervical length measured prior to 23 6/7 weeks was used for analysis.
Details regarding maternal and obstetrical history, pregnancy complications, delivery outcomes, and neonatal characteristics for women obtaining ultrasounds at our institution are collected and entered into a prospective computerized database in an ongoing manner. This database was originally created in 1990 and has been validated and maintained since that time by dedicated perinatal research nurses. Maternal demographic and pregnancy information are entered prospectively at the time of ultrasound exam at our institution. Neonatal and pregnancy outcome information are obtained using electronic medical records and telephone contact with the patient or referring provider as needed. Maternal demographics, including age, race/ethnicity, tobacco use, body mass index (BMI), and gestational age at the time of ultrasound were obtained from this database. Race/ethnicity was defined as Caucasian, used as the reference group, African American, Hispanic, or other and was based on self-report. Those who did not report race/ethnicity were noted. Additional information regarding cervical length, pregnancy complications, mode of delivery, and neonatal outcomes was collected from the perinatal database. Trained research staff reviewed charts of patients with cervical length ≤ 20 mm to extract further data on treatments received. Gestational age was determined based on last menstrual period (LMP) if first trimester ultrasound agreed with the estimated date of confinement (EDC) within seven days or second trimester ultrasound agreed with EDC within 14 days. If the due date differed by more than seven days in the first trimester or 14 days in the second trimester, or if the LMP was unknown, the EDC was changed to that calculated from earliest available ultrasound.
We calculated the acceptance rate of cervical length screening overall and for each year since implementation. We also evaluated risk factors for declining cervical length screening by comparing demographic and pregnancy characteristics between women who underwent cervical length screening and those who declined. We also compared rates of spontaneous preterm birth (after 20 weeks but prior to 37, 34, 28, and 24 weeks gestation) between the two groups for those patients with delivery data available. Spontaneous preterm birth included all patients with spontaneous labor or preterm premature rupture of membranes resulting in delivery. The analysis was repeated limited to women without a history of preterm birth. Additionally, the prevalence of short cervix was determined in our population and was defined as a CL ≤ 20 mm, with prevalence ≤ 25 mm and ≤ 15 mm also determined.
Data analysis was performed using descriptive and bivariate statistics. Normality of distribution for continuous variables was tested using histograms and the Kolmogorov-Smirnov test. An unpaired student’s t- test or Wilcoxon rank-sum test was then used as appropriate. Chi-square or Fisher exact tests were used for categorical variables as appropriate. A p-value of <0.05 was considered significant. A multivariable model including age less than 35, gestational age at ultrasound, race/ethnicity, tobacco, obesity, multiparity and history of preterm birth was used to determine risk factors for declining cervical length screening. The chi-square test of trend was used to assess for changes in acceptability of TVCL screening over time. Multivariable logistic regression was used to estimate of the impact of cervical length screening on preterm birth. The final models controlled for African-American race, tobacco use, and a history of previous preterm birth. Goodness-of-fit of the final model was tested using the Hosmer-Lemeshow test.
Results
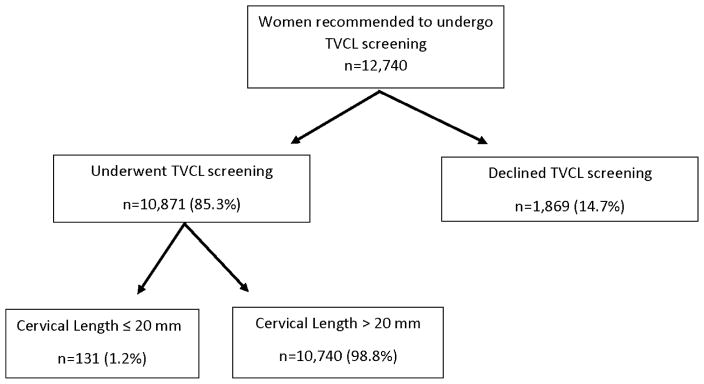
Of 12,740 women undergoing anatomic screening at the midtrimester, 10,871 (85.3%, 95% CI 84.7%, 85.9%) underwent TVCL screening, with 1,869 (14.7%, 95% CI 14.1%, 15.3%) declining cervical screening (Figure 1). Basic characteristics of the cohort are seen in Table 1. Rates of acceptance of cervical length screening increased from 77.4% (95% CI 75.4%, 79.2%) in 2011 when universal TVCL screening was implemented to 86.7% (95% CI 85.5%, 87.8%) in 2012, 85.6% (95% CI 84.4%, 86.7%) in 2013, and 87.8% (95% CI 86.3%, 88.9%) in 2014. There was no statistically significant change in acceptance of cervical length screening from 2012 to 2014 (p for trend=0.149). Women were more likely to decline cervical length screening if they were African American, Hispanic, other race/ethnicity, or if they did not report race/ethnicity when compared to patients of Caucasian race. Women were also more likely to decline cervical length screening if they were obese, multiparous, younger than age 35, or if they smoked (Table 2). Similar risk factors were identified when analysis was limited to only those women without a history of PTB (supplemental table 1).
Figure 1.
Study Participants: Rates of acceptance and short cervix among women in an opt-out universal transvaginal cervical length (TVCL) screening program.
Table 1.
Characteristics of the study cohort
| Characteristic | Rate in Entire Cohort n=12740 | 95% Confidence Interval |
|---|---|---|
| Age (years) (Median, IQR) | 29 (25,33) | |
| Age less than 35 | 10,311 (80.1%) | 80.2%, 81.6% |
| Gestational Age at scan (weeks) (Mean ± SD) | 19.9 ± 1.3 | |
| Caucasian | 6088 (47.1%) | 46.9%, 48.7% |
| African American | 4306 (33.8%) | 33.0%, 34.6% |
| Hispanic | 615 (4.8%) | 4.5%, 5.2% |
| Other Race/Ethnicity | 797 (6.3%) | 5.8%, 6.7% |
| Race/Ethnicity not reported | 1014 (8.0%) | 7.5%, 8.4% |
| Tobacco Use | 951 (7.5%) | 7.0%, 7.9% |
| Maternal Body Mass Index (kg/m2) (Median, IQR) | 24.5 (21.5, 29.6) | |
| Normal Weight | 8990 (70.6%) | 69.8%, 71.4% |
| Obese | 3750 (29.4%) | 28.6%, 30.2% |
| Morbid Obesity | 1578 (12.4%) | 11.8%, 13.0% |
| History of preterm birth | 1209 (9.5%) | 9.0%, 10.0% |
| Multiparity | 8730 (68.5%) | 67.7%, 69.3% |
IQR=Interquartile range
Table 2.
Risk factors for declining cervical length screening
| Risk Factor n= 12740 | Cervical Length Not Screened (n=1869, 14.7%) | Cervical Length Screened (n=10871, 85.3 %) | Adjusted Odds Ratio1 (95% Confidence Interval) |
|---|---|---|---|
| Age (years) (Median, IQR) | 27 (23,32) | 30 (25,33) | p<0.0001 |
| Age less than 35 | 1585 (84.8%) | 8726 (80.3%) | 1.24 (1.08,1.43) |
| Gestational Age at scan (weeks) (Mean ± SD) | 20.1 ± 1.6 | 19.9 ± 1.2 | 1.01 (0.98, 1.06) |
| Caucasian | 574 (30.7%) | 5434 (50.0%) | Reference |
| African American | 861 (46.1%) | 3445 (31.2%) | 2.17 (1.93,2.44) |
| Hispanic | 98 (5.2%) | 517 (4.8%) | 1.56 (1.23,1.98) |
| Other Race/Ethnicity | 151 (8.1%) | 646 (5.9%) | 2.27 (1.86,2.77) |
| Race/Ethnicity not reported | 185 (9.9%) | 829 (7.63%) | 1.76 (1.46,2.12) |
| Tobacco Use | 202 (10.8%) | 749 (6.9%) | 1.42 (1.20,1.68) |
| Maternal Body Mass Index (kg/m2) (Median, IQR) | 25.1 (21.6, 30.7) | 24.4 (21.5,29.3) | p=0.0002 |
| Normal Weight | 1223 (65.4%) | 7767 (71.5%) | Reference |
| Obese | 646 (34.6%) | 3104 (28.6%) | 1.18 (1.06,1.31) |
| Morbid Obesity | 302 (16.2%) | 1276 (11.7%) | 1.36 (1.22,1.52) |
| History of preterm birth | 194 (10.4%) | 1015 (9.3%) | 0.96 (0.81,1.14) |
| Multiparity | 1373 (73.5%) | 7357 (67.7%) | 1.45 (1.29,1.64) |
IQR=Interquartile range
Multivariable model including age less than 35, gestational age at scan, race/ethnicity, tobacco, obesity, history of preterm birth, and multiparity
Delivery data was available for 9,731 (85.4%, 95% CI 84.8%, 86.0%) who underwent TVCL screening and 1,661 (14.6%, 95% CI 13.9%, 15.2%) who declined. Loss to follow-up rates did not differ between the screened and unscreened groups (p=0.39). Women who declined TVCL screening delivered at an earlier mean gestational age than those who underwent screening (Table 3). After adjusting for race/ethnicity, tobacco use, and a history of preterm birth, rates of spontaneous preterm birth before 28 weeks (aOR 2.01, 95% CI 1.33, 3.02) and before 24 weeks (aOR 3.62, 95% CI 2.15, 6.09) were higher in women who declined cervical length screening. Rates of spontaneous preterm birth before 37 weeks and before 34 weeks were not significantly different between the two groups. Similar results were observed when analysis was repeated for only those women without a history of preterm birth (supplemental table 2).
Table 3.
Gestational age at delivery in screened and unscreened women.
| Outcome n=11392 | Cervical Length Not Screened (n=1661, 14.6%) | Cervical Length Screened (n=9731, 85.4%) | aOR1 (95% Confidence Interval) |
|---|---|---|---|
| Mean Gestational Age at Delivery (weeks) (mean ± SD) | 37.4 ± 4.5 | 38.1 ± 2.7 | p<0.0001 |
| Spontaneous preterm birth < 37 weeks1 | 121 (7.3%) | 639 (6.6%) | 1.02 (0.83,1.25) |
| Spontaneous preterm birth < 34 weeks1 | 50 (3.0%) | 207 (2.1%) | 1.23 (0.89,1.69) |
| Spontaneous preterm birth < 28 weeks1 | 34 (2.0%) | 85 (0.9%) | 2.01 (1.33,3.02) |
| Spontaneous preterm birth < 24 weeks1 | 25 (1.6%) | 36 (0.4%) | 3.62 (2.15,6.09) |
Adjusted for race/ethnicity, tobacco use, and history of preterm
Of the 10,871 patients who underwent TVCL screening, 131 (1.2%) had cervical length ≤ 20.0 mm, with 81 (0.8%) ≤ 15 mm. An additional 84 patients had cervical length between 20.0 mm and 25.0 mm, for a total of 215 (2.0%) with cervical length ≤ 25 mm. Of the 131 patients with a cervical length ≤ 20 mm, delivery and treatment information was available for 101. The most common treatment for short cervical length was vaginal progesterone (n=56, 55.4%), given to those with a short cervix and no history of preterm birth. Some patients received cerclage (n=35, 34.7%), typically performed for those with a history of preterm birth and cervical length ≤25 mm or based on physical exam and provider preference. A few women were managed with pessary (n=3, 3.0%) while 7 (6.9%) declined treatment. Of those with cervical length ≤20 mm, 23 patients had a history of preterm birth and 20 of these patients were compliant with 17-hydroxyprogesterone injections. The rate of spontaneous preterm birth prior to 37 weeks was high (49.6%) among all women with short cervix. A similarly high rate of spontaneous preterm birth prior to 37 weeks (47.4%) was noted among women without a history of preterm birth and a short cervix.
Comment
Implementation of an opt-out universal transvaginal cervical length screening program resulted in high rates of screening. Patients who were African American, Hispanic, or other race/ethnicity, obese, multiparous, younger than age 35, and who smoked were more likely to decline cervical length screening. Rates of early, but not late, spontaneous preterm birth were significantly higher among women who did not undergo cervical length screening.
Orzechowski et al described their experience with a TVCL screening program and reported a 72.3–75.0% acceptance rate with 1,569 women screened. 13, 14 The rate of short cervix ≤ 20 mm in their cohort was similar to ours at 1.1%, and there were no differences in spontaneous preterm birth rates ≤ 37, 34, or 32 weeks gestation in women who underwent screening compared to those who did not.14 Women with term birth had a trend toward lower incidence of short cervix.15 Likewise, Miller et. al found a 0.9% rate of cervical length ≤ 25 mm among 18,250 women undergoing TVCL screening.16 The authors suggested that limiting cervical length measurement to those with risk factors for short cervix could improve overall specificity of screening.16 Similarly, Facco et al recommended targeted screening to improve specificity based on a secondary analysis of a multicenter observational trial that found low rates of short cervix among low risk women.19
Although we found high rates of sustained acceptability of TVCL screening over 3 years after implementation of a universal screening program, women with important risk factors for preterm birth, including African American race, other minority race/ethnicity, and tobacco use, were more likely to go unscreened for reasons that are unclear.11 These findings differ from those of Orzechowski et al, who found that women who were multiparous or had a language barrier were more likely to decline screening.13 Although screening was offered to all patients as a routine part of anatomic survey, there may have been other unmeasured factors that account for differences in who accepted screening. This study does not assess whether additional patient, provider, or healthcare system factors may contribute to differences in screening. Regardless of the reasons, our findings highlight the potential challenges and complexities of universal cervical length screening. Future efforts should be aimed at improving the uptake of screening by these patients who have risk factors for preterm birth.
We found higher rates of early spontaneous preterm birth among women who did not undergo TVCL screening. These findings differ from the results of Orzechowski et al, who found no differences in spontaneous preterm birth rates in those screened and those who declined screening.14 The larger sample size in our study may have provided the power to detect this difference. The increased rates of early preterm birth among those unscreened remained even among women without a prior history of preterm birth. While the higher risk of preterm birth among those unscreened may be secondary to unmeasured confounders rather than a true benefit of TVCL screening, it further highlights the observation that risk factors for preterm birth were also associated with declining screening.
The 1.2% incidence of short cervix differs from previous publications and has implications for the overall cost effectiveness of screening. Although the prevalence of short cervix in this cohort is lower than the 1.7–2.3% reported in the original trials of vaginal progesterone and used in initial cost effectiveness analyses, it is more similar to the prevalence found in subsequent studies following implementation of universal TVCL screening.7, 9, 13, 14 In a recent reevaluation of cost effectiveness, screening remained cost effective, but was no longer cost saving when the prevalence of cervical length ≤ 20 mm was ≤0.83%.20 The rate of preterm birth before 34 weeks among those screened with a short cervix in the updated cost effectiveness model was 25.8%.20 While the incidence of short cervix in our cohort was higher than that used in the updated cost effectiveness model, the rate of preterm birth before 34 weeks among those with a short cervix in our cohort was higher at 36.5%. This incidence may be higher than reported in some previous studies as it includes those with a short cervix who declined treatment. The increased rates of preterm birth among those screened in our cohort could decrease the overall cost effectiveness of screening.
This large study illustrates the successful institutional implementation of universal transvaginal cervical length screening. There are also limitations that should be considered. The retrospective study design limits the ability to determine the reasons patients declined screening and makes it vulnerable to errors in data collection. However, the database used has been well validated in several previous studies with errors in the database found to be rare.21–26 Additionally, race/ethnicity was self-reported and not reported for 8% of patients which may limit conclusions that can be drawn. Further, the lack of delivery data for 10.6% of patients, which includes 16 of the 131 patients with short cervix limits the interpretation of the delivery data. If the patients without delivery data indeed delivered preterm, the relative benefit of screening might be overestimated by this analysis. We did not adjust for multiple comparisons, raising the possibility that some significant differences could have occurred by chance. While we adjusted for confounders using logistic regression there is the possibility of residual confounding by unmeasured factors.
In conclusion, we found that universal TVCL screening was implemented successfully for the majority of patients, but women at risk for preterm birth were less likely to be screened. These findings are important considerations in the continuing debate about universal TVCL screening.
Supplementary Material
Acknowledgments
Dr. Temming is supported by a NIH T32 training grant (5T32HD055172-07). This publication was also made possible by Grant Number UL1 TR000448 from the NIH National Center for Advancing Translational Sciences (NCATS), components of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
Footnotes
The authors report no conflict of interest.
Will be presented as oral presentation #15 at the 36th annual meeting of the Society for Maternal and Fetal Medicine, Atlanta, GA, February 1st–6th, 2016.
Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCATS or NIH.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hamilton BEPD, Martin JA, Osterman MMHS, Curtain SMA. Births: Preliminary Data for 2014. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2015;64:1–19. [PubMed] [Google Scholar]
- 2.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. The Lancet. 371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parry S, Simhan H, Elovitz M, Iams J. Universal maternal cervical length screening during the second trimester: Pros and cons of a strategy to identify women at risk of spontaneous preterm delivery. American journal of obstetrics and gynecology. 2012;207:101–06. doi: 10.1016/j.ajog.2012.04.021. [DOI] [PubMed] [Google Scholar]
- 4.Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network The New England journal of medicine. 1996;334:567–72. doi: 10.1056/NEJM199602293340904. [DOI] [PubMed] [Google Scholar]
- 5.Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH. Progesterone and the risk of preterm birth among women with a short cervix. The New England journal of medicine. 2007;357:462–9. doi: 10.1056/NEJMoa067815. [DOI] [PubMed] [Google Scholar]
- 6.Hassan SS, Romero R, Vidyadhari D, et al. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound in obstetrics & gynecology: the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2011;38:18–31. doi: 10.1002/uog.9017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cahill AG, Odibo AO, Caughey AB, et al. Universal cervical length screening and treatment with vaginal progesterone to prevent preterm birth: a decision and economic analysis. American journal of obstetrics and gynecology. 2010;202:548 e1–8. doi: 10.1016/j.ajog.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berghella V. Universal cervical length screening for prediction and prevention of preterm birth. Obstetrical & gynecological survey. 2012;67:653–8. doi: 10.1097/OGX.0b013e318270d5b2. [DOI] [PubMed] [Google Scholar]
- 9.Werner EF, Han CS, Pettker CM, et al. Universal cervical-length screening to prevent preterm birth: a cost-effectiveness analysis. Ultrasound in obstetrics & gynecology: the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2011;38:32–7. doi: 10.1002/uog.8911. [DOI] [PubMed] [Google Scholar]
- 10.Parry S, Elovitz MA. Pros and cons of maternal cervical length screening to identify women at risk of spontaneous preterm delivery. Clinical obstetrics and gynecology. 2014;57:537–46. doi: 10.1097/GRF.0000000000000051. [DOI] [PubMed] [Google Scholar]
- 11.Committee on Practice Bulletins-Obstetrics TACoO, Gynecologists. Practice bulletin no 130: prediction and prevention of preterm birth. Obstetrics and gynecology. 2012;120:964–73. doi: 10.1097/AOG.0b013e3182723b1b. [DOI] [PubMed] [Google Scholar]
- 12.Society for Maternal Fetal Medicine Publications C. ACOG Committee Opinion number 419 October 2008 (replaces no. 291, November 2003) Use of progesterone to reduce preterm birth. Obstetrics and gynecology. 2008;112:963–5. doi: 10.1097/AOG.0b013e31818b1ff6. [DOI] [PubMed] [Google Scholar]
- 13.Orzechowski KM, Nicholas SS, Baxter JK, Weiner S, Berghella V. Implementation of a universal cervical length screening program for the prevention of preterm birth. American journal of perinatology. 2014;31:1057–62. doi: 10.1055/s-0034-1371710. [DOI] [PubMed] [Google Scholar]
- 14.Orzechowski KM, Boelig RC, Baxter JK, Berghella V. A universal transvaginal cervical length screening program for preterm birth prevention. Obstetrics and gynecology. 2014;124:520–5. doi: 10.1097/AOG.0000000000000428. [DOI] [PubMed] [Google Scholar]
- 15.Orzechowski KM, Boelig R, Nicholas SS, Baxter J, Berghella V. Is universal cervical length screening indicated in women with prior term birth? American journal of obstetrics and gynecology. 2015;212:234 e1–5. doi: 10.1016/j.ajog.2014.08.029. [DOI] [PubMed] [Google Scholar]
- 16.Miller ES, Tita AT, Grobman WA. Second-Trimester Cervical Length Screening Among Asymptomatic Women. Obstetrics and gynecology. 2015;126:61–66. doi: 10.1097/AOG.0000000000000864. [DOI] [PubMed] [Google Scholar]
- 17.Owen J, Iams JD. What we have learned about cervical ultrasound. Seminars in perinatology. 2003;27:194–203. doi: 10.1016/s0146-0005(03)00021-1. [DOI] [PubMed] [Google Scholar]
- 18.Berghella V, Baxter JK, Hendrix NW. Cervical assessment by ultrasound for preventing preterm delivery. The Cochrane database of systematic reviews. 2013;1:CD007235. doi: 10.1002/14651858.CD007235.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Facco FL, Simhan HN. Short ultrasonographic cervical length in women with 1 low-risk obstetric history. Obstetrics and gynecology. 2013;122:858–62. doi: 10.1097/AOG.0b013e3182a2dccd. [DOI] [PubMed] [Google Scholar]
- 20.Werner EF, Hamel MS, Orzechowski K, Berghella V, Thung SF. Cost-effectiveness of transvaginal ultrasound cervical length screening in singletons without a prior preterm birth: an update. American journal of obstetrics and gynecology. 2015 doi: 10.1016/j.ajog.2015.06.020. [DOI] [PubMed] [Google Scholar]
- 21.Tuuli MG, Rampersad R, Stamilio D, Macones G, Odibo AO. Perinatal outcomes in women with preeclampsia and superimposed preeclampsia: do they differ? American journal of obstetrics and gynecology. 2011;204:508 e1–7. doi: 10.1016/j.ajog.2011.01.065. [DOI] [PubMed] [Google Scholar]
- 22.Tuuli MG, Dicke JM, Stamilio DM, et al. Prevalence and likelihood ratios for aneuploidy in fetuses diagnosed prenatally with isolated congenital cardiac defects. American journal of obstetrics and gynecology. 2009;201:390 e1–5. doi: 10.1016/j.ajog.2009.06.035. [DOI] [PubMed] [Google Scholar]
- 23.Stout MJ, Odibo AO, Graseck AS, Macones GA, Crane JP, Cahill AG. Leiomyomas at routine second-trimester ultrasound examination and adverse obstetric outcomes. Obstetrics and gynecology. 2010;116:1056–63. doi: 10.1097/AOG.0b013e3181f7496d. [DOI] [PubMed] [Google Scholar]
- 24.Odibo AO, Singla A, Gray DL, Dicke JM, Oberle B, Crane J. Is chorionic villus sampling associated with hypertensive disorders of pregnancy? Prenatal diagnosis. 2010;30:9–13. doi: 10.1002/pd.2410. [DOI] [PubMed] [Google Scholar]
- 25.Carbone JF, Tuuli MG, Dicke JM, Macones GA, Odibo AO. Revisiting the risk for aneuploidy in fetuses with isolated pyelectasis. Prenatal diagnosis. 2011;31:566–70. doi: 10.1002/pd.2749. [DOI] [PubMed] [Google Scholar]
- 26.Cahill AG, Macones GA, Stamilio DM, Dicke JM, Crane JP, Odibo AO. Pregnancy loss rate after mid-trimester amniocentesis in twin pregnancies. American journal of obstetrics and gynecology. 2009;200:257 e1–6. doi: 10.1016/j.ajog.2008.09.872. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.