Abstract
Background:
The purpose of this study was to evaluate the influence of three different luting protocols on shear bond strength of computer aided design/computer aided manufacturing (CAD/CAM) resin nanoceramic (RNC) material to dentin.
Materials and Methods:
In this in vitro study, 30 disks were milled from RNC blocks (Lava Ultimate/3M ESPE) with CAD/CAM technology. The disks were subsequently cemented to the exposed dentin of 30 recently extracted bovine permanent mandibular incisors. The specimens were randomly assigned into 3 groups of 10 teeth each. In Group 1, disks were cemented using a total-etch protocol (Scotchbond™ Universal Etchant phosphoric acid + Scotchbond Universal Adhesive + RelyX™ Ultimate conventional resin cement); in Group 2, disks were cemented using a self-etch protocol (Scotchbond Universal Adhesive + RelyX™ Ultimate conventional resin cement); in Group 3, disks were cemented using a self-adhesive protocol (RelyX™ Unicem 2 Automix self-adhesive resin cement). All cemented specimens were placed in a universal testing machine (Instron Universal Testing Machine 3343) and submitted to a shear bond strength test to check the strength of adhesion between the two substrates, dentin, and RNC disks. Specimens were stressed at a crosshead speed of 1 mm/min. Data were analyzed with analysis of variance and post-hoc Tukey's test at a level of significance of 0.05.
Results:
Post-hoc Tukey testing showed that the highest shear strength values (P < 0.001) were reported in Group 2. The lowest data (P < 0.001) were recorded in Group 3.
Conclusion:
Within the limitations of this in vitro study, conventional resin cements (coupled with etch and rinse or self-etch adhesives) showed better shear strength values compared to self-adhesive resin cements. Furthermore, conventional resin cements used together with a self-etch adhesive reported the highest values of adhesion.
Keywords: Adhesive cements, computer aided design/computer aided manufacturing ceramic, shear bond strength
INTRODUCTION
To reproduce highly esthetic tooth-colored fixed dental prostheses, computer aided design/computer aided manufacturing (CAD/CAM) techniques are becoming frequently used. Since the commercial introduction of polymeric blanks into the dental market, CAD/CAM manufacturing of temporaries has become increasingly important.[1] Lava Ultimate resin nanoceramic (RNC) blocks (3M ESPE, St. Paul, MN, USA) are innovative new CAD/CAM materials that make it possible to achieve superior esthetic results in easy steps. The blocks are made of nanoceramic particles embedded in a highly cured resin matrix. The milled RNC restorations can be individualized intra- or extra-orally, either before or after insertion.[2]
In recent years, researchers have tried to achieve a more effective and longer-lasting adhesion between restorative materials and the dental substrate. The adhesive techniques are based on research on the hybrid layer and on chemical and mechanical adhesion. Some researchers have attempted to shorten the application time and reduce the number of steps,[3] creating new generations of materials and improving their quality. Increasing demand for esthetic restorations has led to greater use of all ceramic materials because of their improved biocompatibility and optical properties, compared with metal-ceramic restorations.[4] Advances in CAD and CAM systems are providing new options for dentistry, creating an alternative to the conventional impression and casting technique for producing dental restorations.[5] A requirement for the successful function of a CAD/CAM restoration is adequate adhesion between ceramic and tooth substance;[6] however, the literature is unclear on which cement, ceramic, conditioning treatment, and dentine bonding agent produce the highest bond strength. Resin composite cements are used to lute conventional metal crowns, fixed partial dentures, ceramic crowns, and veneers and to repair fractured metal ceramic restorations.[7] Resin cements have been selected for their advantageous mechanical and adhesive properties compared with conventional luting agents.[8] They have shown good marginal integrity and low microleakage.[9] The use of resin luting agents also appears to be essential in determining an effective stress distribution, which will prevent crack initiation.[10] Bond strength to ceramic material is influenced by the composition of the ceramic substrate as well as by mechanical and chemical interaction between substrate and bonding agent.[11]
The aim of this study was to evaluate the influence of three different luting protocols (total-etch, self-etch, and self-adhesive) on shear bond strength of CAD/CAM RNC material, based on CAD/CAM technology, to dentin.
MATERIALS AND METHODS
Specimens preparation
In the present in vitro study, 30 disks (5 mm in diameter, 3 mm thick) were designed with CEREC software 4.2 platform (Sirona Dental GmbH, Salzburg, Austria) and obtained by milling from RNC blocks for CAD/CAM (Lava™ Ultimate Restorative, 3M ESPE, St. Paul, MN, USA) with CEREC MC XL (Sirona Dental Gmbh, Salzburg, Austria) [Figure 1]. The specifications of materials tested are listed in Table 1.
Figure 1.
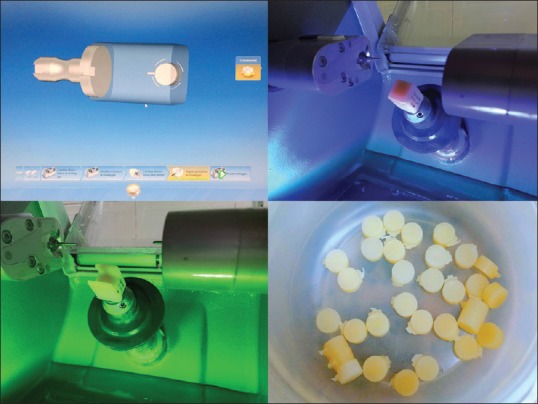
Computer aided design/computer aided manufacturing of Lava™ Ultimate Restorative disks. The disks were obtained by milling from resin nano ceramic blocks for computer aided design/computer aided manufacturing with CEREC MC XL.
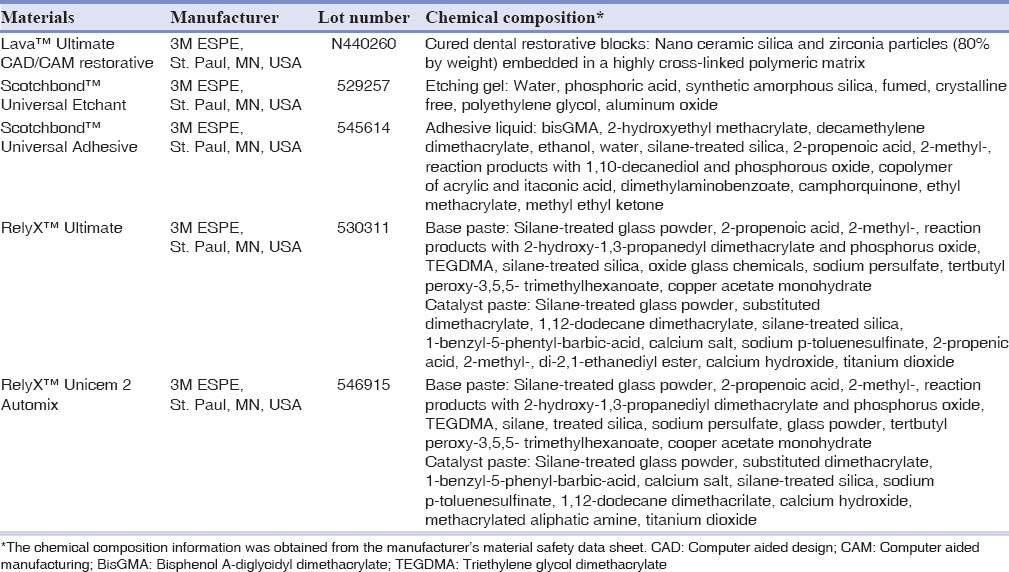
Table 1.
Characteristics of materials tested
The disks were subsequently cemented to the exposed dentin of 30 bovine permanent mandibular incisors freshly extracted and stored in a 0.1% (wt/vol) thymol solution, which were used as a substitute for human teeth.[12,13] The criteria for tooth selection included intact buccal enamel with no cracks caused by extraction, the absence of caries, and adequate dimension of the crown. The teeth were cleansed of soft tissue remnants and debris with periodontal curettes, stored in the thymol solution for 1 week, and later in saline solution at room temperature until testing. Then the roots of the teeth were embedded in self-curing, fast-setting acrylic resin (Rapid Repair, Degu Dent GmbH, Hanau, Germany). Specially fabricated cylindrical Teflon mold with an internal diameter of 14 mm were filled with the acrylic resin and allowed to cure, thus encasing each specimen while allowing the buccal surface of dentin to be exposed. Each tooth was oriented so that its labial surface was parallel to the shearing force. The buccal enamel was removed using a high-speed carbide rotary instrument (No. H21 L.314.014; Komet, Lemgo, Germany) under copious water irrigation, to expose midcoronal dentin. The exposed dentin surfaces were finished off with an automated polishing machine (APL-4; Arotec S.A. Ind Com, Cotia, SP, Brazil) with a 600-grit silicon carbide abrasive paper disks for 5 s, to obtain a flat and uniform dentin surface and reduce any micromechanical interlocking that could affect the real bonding influence of the tested adhesive cements. Before cementation, to remove the smear layer and to treat the dental surface with cleaning solution, the dentin surface was rinsed for 1 min with a cotton pellet impregnated with Tubulicid Blue (Dental Therapeutics AB, Saltsjö-Boo, Sweden) without fluorine. The surface was then rinsed and dried before cementation; the labial surface of each incisor was cleaned for 10 s with a mixture of water and fluoride-free pumice and rubber polishing cup in a low-speed handpiece. The dentinal surface was rinsed with water to remove pumice or debris and then dried with an oil-free air stream. The bonding surface of each disk was cleaned with alcohol and rinsed with water to remove oil debris contained in the milling liquid.
Cementation procedures
The specimens were randomly assigned to 3 groups of 10 teeth each [Figure 1] according to different luting procedures (total-etch, self-etch, and self-adhesive). One operator carried out all procedures to maximize standardization.
Group 1: ULT-TE: Disks were cemented on the dentin surface, which had been acid-etched with Scotchbond™ Universal Etchant phosphoric acid (3M ESPE, St. Paul, MN, USA) for 15 s, the etched substrates were rinsed with water for 15 s, and gently air dried for 15 s to remove excess water and treated with Scotchbond Universal Adhesive (3M ESPE, St. Paul, MN, USA) with adhesive resin cement (RelyX™ Ultimate/3M ESPE, St. Paul, MN, USA)
Group 2: ULT-SE: Disks were cemented on the dentin surface, which had been treated with Scotchbond Universal Adhesive, with the adhesive resin cement (RelyX™ Ultimate)
Group 3: U2-SA: Disks were cemented on the dentin surface with the dual polymerization resin luting agent RelyX™ Unicem 2 Automix.
A vinyl ring with an internal diameter of 4.5 mm was applied under the dentin surface to standardize the adhesion area. For all groups, no further procedures were applied in order to avoid bias and confounding factors.
During cementation, a thin layer of cement was applied and distributed to the bonding surface of the cylinders by means of a Heidemann spatula. On each specimen, five surfaces were identified: Mesial, lingual, distal, buccal, and occlusal. As suggested by the manufacturer, every surface was light-polymerized for 20 s at a light intensity of 1000 mW/cm2 using a light-emitting diode (LED) curing light in soft start-polymerization mode (Celalux 2 High-power LED curing light, Voco GmbH, Cuxhaven, Germany). The power output (light intensity) of the LED was measured with a Cure Rite radiometer (Caulk-Dentsply mod. 644726, Konstanz, Germany).
All samples were stored in distilled water at room temperature for 24 h.
Shear bond strength test
After storing, the specimens were all submitted to a shear bond strength test to check the strength of adhesion between the two substrates, dentin, and RNC. This test is defined as a test in which two materials are connected by an adhesive agent and loaded in shear until separation occurs.[14] Specimens were placed in a universal testing machine (Model 3343, Instron Corporation, Norwood, MA, USA). Teeth were secured in the lower jaw of the machine so that the bonded cylinder base was parallel to the shear force direction. Specimens were stressed in an occlusogingival direction at a crosshead speed of 1 mm/min [Figure 2].[15] The maximum load necessary to debond was recorded in Newton (N) and calculated in MPa as a ratio of Newton to the surface area of the cylinder (the calculated shear bond strength was determined by dividing the strength at which bond failure occurred by the bonding area).[14]
Figure 2.
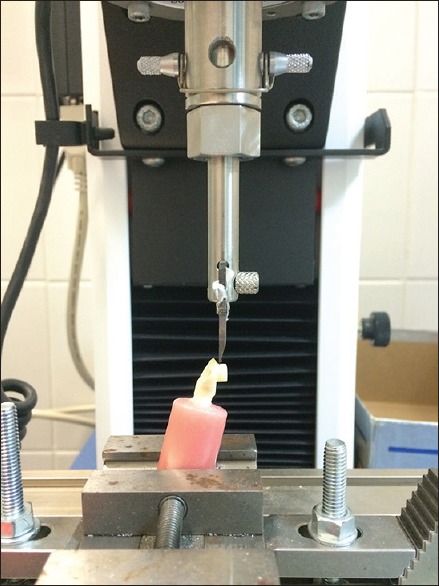
Shear bond strength testing. Specimens were placed in a universal testing machine, secured in the lower jaw of the machine so that the bonded cylinder base was parallel to the shear force direction.
After the testing procedure, the fractured surfaces were examined with an optical microscope (Stereomicroscope SR, Zeiss, Oberkochen, Germany).
Statistical analysis
Statistical analysis was performed with Stata 12.0 software (Stata, College Station, Texas, USA). Descriptive statistics, including the mean, standard deviation, median, and minimum and maximum values were calculated for all groups.
The normality of the data was calculated using the Shapiro-Wilk test. Analysis of variance (ANOVA) was applied to determine whether significant differences in debond strength values existed among the groups. Tukey's test was used post-hoc. Significance for all statistical tests was predetermined at P < 0.05.
RESULTS
Descriptive statistics are presented in Table 2. ANOVA showed the presence of significant differences among the various groups (P < 0.0001). As showed in Figure 3, post-hoc Tukey testing showed that the highest shear strength values (P < 0.001) were reported in Group 2 (ULT-SE). Significant differences were found among the three groups (P > 0.05). The lowest data (P < 0.001) were recorded in Group 3 (U2-SA).
Table 2.
Descriptive statistics (MPa) of the different groups
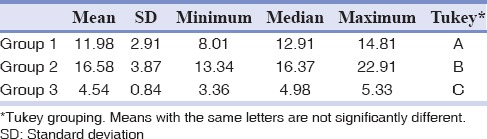
Figure 3.
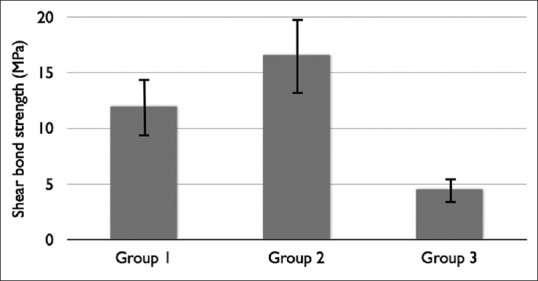
Shear bond strength values (MPa) obtained in the three groups.
DISCUSSION
Patients’ needs and desires and developments in adhesive dentistry have made the use of all-ceramic restorations increasingly frequent, particularly silica-based ones such as crowns, inlay-onlays, and laminate veneers.[16] In order to improve the impression and casting procedure steps and to produce indirect restorations faster and easier, without the need for provisional restorations and dental laboratories, CAD/CAM systems are commonly used.[17] Lava Ultimate RNC (3M ESPE, St. Paul, MN, USA) is a new composite/nanoceramic material for CAD/CAM manufacturing. This material allows the possibility to use composite materials to characterize and adjust the restoration after milling. Unlike conventional ceramic restorations, customization and glaze firing is neither necessary nor possible with RNC restorations. This opens up the opportunity for intraoral individualization and adaptation of the restorations.[2]
Industrially, prefabricated CAD/CAM restorations are polymerized by standardized methods and improving material properties, in particular, predictability and consistency. Comparing these machinable prostheses to laboratory-handmade restorations, it has been advocated that, due to a highly homogeneous quality crystalline content, the bond strength to hard tooth tissues and the clinical longevity of these CAD/CAM restorations have been increased. In contrast, conventional manual polymerization and processing is greatly influenced by the operator and can cause a high level of variations.[18]
However, to achieve a long duration of restoration and, therefore, its long-term success, durable bond strength between the tooth and the restorative material is fundamental.[1] To date, no study has evaluated the shear bond strength between the new nanoceramic Lava Ultimate material and tooth structures. The aim of this study was to investigate the influence of different luting protocols (total-etch, self-etch, and self-adhesive) on the shear bond strength values between dentin and this innovative RNC material, based on CAD/CAM technology.
Although it is preferable to use extracted human teeth for bonding research,[19] it has become increasingly difficult to obtain such samples for laboratory studies in Italy. To compare data from the current study with that reported in previous bovine enamel bond strength tests, bovine teeth were used as a substitute for human teeth in the current study. Bovine teeth have some advantages, as they are easy to obtain in large quantities, are in good condition and have less composition variables than human enamel.[20] Bovine teeth also have large, flat surfaces and are unlikely to have undergone prior caries challenges that could affect the test result. The mineral distribution within the carious lesions in bovine teeth is reportedly similar to that found in human teeth, and the structural changes that occur in human and bovine teeth are also similar.[21]
For the cementation procedure, three different luting protocols have been evaluated in this study: Total etch/etch and rinse protocol (Group 1 - ULT-TE: Sco35% phosphoric acid + Scotchbond Universal Adhesive + RelyX™ Ultimate conventional resin cement); self-etch protocol (Group 2 - ULT-SE: Scotchbond Universal Adhesive + RelyX™ Ultimate conventional resin cement), and self-adhesive protocol (Group 3 - U2-SA: RelyX™ Unicem 2 Automix self-adhesive resin cement). These three different cementation techniques have been selected according to contemporary adhesive systems classification into etch-and-rinse and self-etch adhesives.[22] While the etch-and-rinse approach requires a separate acid-etch step to promote dentin and enamel demineralization before monomer infiltration, demineralization and infiltration occur simultaneously in the self-etch approach, although with no perfect synchronism.[23] In addition, the separate etch-and-rinse step completely removes the smear layer, while the combined etch and bonding step in self-etch adhesive systems only partially dissolve the smear layer. Complete removal of the smear layer may allow for more intimate contact of the hydrophilic primer and hydrophobic bonding agent to the tooth. This allows the characteristic microretentive resin tags and a hybrid layer to be formed.[24]
Many articles related to adhesive procedures used for the cementation of ceramic to tooth structure have shown that the presence of a hybrid layer between adhesive resin and dentin seems to adequately seal the dentinal tubules and allows a cellular reorganization of the pulpal tissues.[25,26] In the present study, all the tested cements are based on adhesive procedures, which determine the formation of the hybrid layer and lead to the creation of a stronger link between dental structure and composite cement.
In general two different types of resin composite cements exist: The conventional and the self-adhesive resin composite cements. These two different types of cements have been both evaluated in our study. To bond CAD/CAM restoration to dentin, RelyX™ Ultimate conventional resin cement was used together with a etch and rinse adhesive or with a self-etch adhesive; while RelyX™ Unicem 2 Automix self-adhesive resin cement was used alone.
A pretreatment of tooth abutment is necessary in case of use of conventional resin composite cements. Obviously the required pretreatment is both technique-sensitive and time-consuming. For this reason, since they do not necessitate any pretreatment of tooth substrate, self-adhesive resin composite cements have been developed.[27] Self-adhesive resin composite cements contain acid monomers, resulting in an initial lower pH value for the infiltration into the demineralized collagen network,[28] In our study significant differences were found between conventional and self-adhesive resin cements. The lowest shear bond strength values were recorded in Group 3; i.e., Lava Ultimate RNC disks bonded to dentin with self-adhesive cements. This is in accordance with a study by Stawarczyk et al., which reported lower tensile bond strength with self-adhesive resin composite cements to polymeric crowns, compared to the bonding with conventional resin cements.[29] However, the bond strength of these resin composite cements is highly variable. While some products have equal bond strength of self-adhesive resin cement to dentin, other products show an inferior bond to enamel.[30] The success of the restoration depends not only on the bond between tooth and resin cement but also on the bond between restoration and resin composite cement. According to some authors to achieve a resistant bond, further conditioning of the restoration material is needed.[31]
When comparing the shear bond strength values of conventional resin cements used together with an etch and rinse adhesive or with a self-etch adhesive, significantly higher bond strength values were recorded in Group 2 (self-etch protocol). Our results are in accordance with a study by Flury et al.[32] However, recent reviews in literature showed conflicting results.[11] Accurate and meticulous procedures during the cementation phase may play an essential clinical role in achieving a valuable connection between the dentin and the ceramic restoration. Retention form of the preparation, marginal integrity, and clinical micro-leakage are the key parameters used to judge the effectiveness of a resin composite cement system. Further studies should be conducted to test the correlation of bond strength for both tested materials to 48 h, 1 week, 1 month, and 1 year to evaluate the time factor related to the effective quality of bonding between ceramic material and dentin. Additional research should also be conducted to test the correlation between porosity, poor wetting, high viscosity, and failures.[1]
CONCLUSION
Within the limitations of this in vitro study, conventional resin cements (coupled with etch and rinse or self-etch adhesives) showed better shear strength values compared to self-adhesive resin cements. Then, for the tested polymeric CAD/CAM materials, the use of additional adhesives for conditioning is necessary. Furthermore, conventional resin cements used together with a self-etch adhesive reported the highest values of adhesion. However, future researches are needed to evaluate the bond strength to new ceramic/polymer prosthetic materials.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or non-financial in this article
REFERENCES
- 1.Bähr N, Keul C, Edelhoff D, Eichberger M, Roos M, Gernet W, et al. Effect of different adhesives combined with two resin composite cements on shear bond strength to polymeric CAD/CAM materials. Dent Mater J. 2013;32:492–501. doi: 10.4012/dmj.2012-329. [DOI] [PubMed] [Google Scholar]
- 2.Koller M, Arnetzl GV, Holly L, Arnetzl G. Lava ultimate resin nano ceramic for CAD/CAM: Customization case study. Int J Comput Dent. 2012;15:159–64. [PubMed] [Google Scholar]
- 3.Cura C, Saraçoglu A, Cötert HS. Effect of different bonding agents on shear bond strengths of composite-bonded porcelain to enamel. J Prosthet Dent. 2003;89:394–9. doi: 10.1067/mpr.2003.58. [DOI] [PubMed] [Google Scholar]
- 4.Saygili G, Sahmali S. Effect of ceramic surface treatment on the shear bond strengths of two resin luting agents to all-ceramic materials. J Oral Rehabil. 2003;30:758–64. doi: 10.1046/j.1365-2842.2003.01027.x. [DOI] [PubMed] [Google Scholar]
- 5.Kamada K, Yoshida K, Atsuta M. Effect of ceramic surface treatments on the bond of four resin luting agents to a ceramic material. J Prosthet Dent. 1998;79:508–13. doi: 10.1016/s0022-3913(98)70170-2. [DOI] [PubMed] [Google Scholar]
- 6.Ozcan M, Vallittu PK. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent Mater. 2003;19:725–31. doi: 10.1016/s0109-5641(03)00019-8. [DOI] [PubMed] [Google Scholar]
- 7.Kamada K, Yoshida K, Atsuta M. Early bond strength and durability of bond between a ceramic material and chemically-cured or dual-cured resin luting agent. Am J Dent. 2001;14:85–8. [PubMed] [Google Scholar]
- 8.Attar N, Tam LE, McComb D. Mechanical and physical properties of contemporary dental luting agents. J Prosthet Dent. 2003;89:127–34. doi: 10.1067/mpr.2003.20. [DOI] [PubMed] [Google Scholar]
- 9.Rosentritt M, Behr M, Lang R, Handel G. Influence of cement type on the marginal adaptation of all-ceramic MOD inlays. Dent Mater. 2004;20:463–9. doi: 10.1016/j.dental.2003.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Bindl A, Lüthy H, Mörmann WH. Strength and fracture pattern of monolithic CAD/CAM-generated posterior crowns. Dent Mater. 2006;22:29–36. doi: 10.1016/j.dental.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Spitznagel FA, Horvath SD, Guess PC, Blatz MB. Resin bond to indirect composite and new ceramic/polymer materials: A review of the literature. J Esthet Restor Dent. 2014;26:382–93. doi: 10.1111/jerd.12100. [DOI] [PubMed] [Google Scholar]
- 12.Montes MA, de Goes MF, Sinhoreti MA. The in vitro morphological effects of some current pre-treatments on dentin surface: A SEM evaluation. Oper Dent. 2005;30:201–12. [PubMed] [Google Scholar]
- 13.Nikaido T, Takano Y, Sasafuchi Y, Burrow MF, Tagami J. Bond strengths to endodontically-treated teeth. Am J Dent. 1999;12:177–80. [PubMed] [Google Scholar]
- 14.Al-Dohan HM, Yaman P, Dennison JB, Razzoog ME, Lang BR. Shear strength of core-veneer interface in bi-layered ceramics. J Prosthet Dent. 2004;91:349–55. doi: 10.1016/j.prosdent.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 15.Cacciafesta V, Sfondrini MF, De Angelis M, Scribante A, Klersy C. Effect of water and saliva contamination on shear bond strength of brackets bonded with conventional, hydrophilic, and self-etching primers. Am J Orthod Dentofacial Orthop. 2003;123:633–40. doi: 10.1016/s0889-5406(03)00198-7. [DOI] [PubMed] [Google Scholar]
- 16.Erdemir U, Sancakli HS, Sancakli E, Eren MM, Ozel S, Yucel T, et al. Shear bond strength of a new self-adhering flowable composite resin for lithium disilicate-reinforced CAD/CAM ceramic material. J Adv Prosthodont. 2014;6:434–43. doi: 10.4047/jap.2014.6.6.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peumans M, Hikita K, De Munck J, Van Landuyt K, Poitevin A, Lambrechts P, et al. Effects of ceramic surface treatments on the bond strength of an adhesive luting agent to CAD-CAM ceramic. J Dent. 2007;35:282–8. doi: 10.1016/j.jdent.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Kara HB, Dilber E, Koc O, Ozturk AN, Bulbul M. Effect of different surface treatments on roughness of IPS empress 2 ceramic. Lasers Med Sci. 2012;27:267–72. doi: 10.1007/s10103-010-0860-3. [DOI] [PubMed] [Google Scholar]
- 19.Schilke R, Bauss O, Lisson JA, Schuckar M, Geurtsen W. Bovine dentin as a substitute for human dentin in shear bond strength measurements. Am J Dent. 1999;12:92–6. [PubMed] [Google Scholar]
- 20.Edmunds DH, Whittaker DK, Green RM. Suitability of human, bovine, equine, and ovine tooth enamel for studies of artificial bacterial carious lesions. Caries Res. 1988;22:327–36. doi: 10.1159/000261132. [DOI] [PubMed] [Google Scholar]
- 21.Tsuchiya H, Tsubota K, Iwasa M, Ando S, Miyazaki M, Platt JA. Influence of adhesive application time on enamel bond strength of single-step self-etch adhesive systems. Oper Dent. 2010;35:77–83. doi: 10.2341/09-064-L. [DOI] [PubMed] [Google Scholar]
- 22.Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, et al. Buonocore memorial lecture. Adhesion to enamel and dentin: Current status and future challenges. Oper Dent. 2003;28:215–35. [PubMed] [Google Scholar]
- 23.Carvalho RM, Chersoni S, Frankenberger R, Pashley DH, Prati C, Tay FR. A challenge to the conventional wisdom that simultaneous etching and resin infiltration always occurs in self-etch adhesives. Biomaterials. 2005;26:1035–42. doi: 10.1016/j.biomaterials.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 24.Tay FR, King NM, Suh BI, Pashley DH. Effect of delayed activation of light-cured resin composites on bonding of all-in-one adhesives. J Adhes Dent. 2001;3:207–25. [PubMed] [Google Scholar]
- 25.Nakabayashi N, Kojima K, Masuhara E. The promotion of adhesion by the infiltration of monomers into tooth substrates. J Biomed Mater Res. 1982;16:265–73. doi: 10.1002/jbm.820160307. [DOI] [PubMed] [Google Scholar]
- 26.Olmez A, Oztas N, Basak F, Sabuncuoglu B. A histopathologic study of direct pulp-capping with adhesive resins. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:98–103. doi: 10.1016/s1079-2104(98)90157-3. [DOI] [PubMed] [Google Scholar]
- 27.Radovic I, Monticelli F, Goracci C, Vulicevic ZR, Ferrari M. Self-adhesive resin cements: A literature review. J Adhes Dent. 2008;10:251–8. [PubMed] [Google Scholar]
- 28.Behr M, Rosentritt M, Regnet T, Lang R, Handel G. Marginal adaptation in dentin of a self-adhesive universal resin cement compared with well-tried systems. Dent Mater. 2004;20:191–7. doi: 10.1016/s0109-5641(03)00091-5. [DOI] [PubMed] [Google Scholar]
- 29.Stawarczyk B, Basler T, Ender A, Roos M, Ozcan M, Hämmerle C. Effect of surface conditioning with airborne-particle abrasion on the tensile strength of polymeric CAD/CAM crowns luted with self-adhesive and conventional resin cements. J Prosthet Dent. 2012;107:94–101. doi: 10.1016/S0022-3913(12)60031-6. [DOI] [PubMed] [Google Scholar]
- 30.De Munck J, Vargas M, Van Landuyt K, Hikita K, Lambrechts P, Van Meerbeek B. Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater. 2004;20:963–71. doi: 10.1016/j.dental.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 31.Soares CJ, Soares PV, Pereira JC, Fonseca RB. Surface treatment protocols in the cementation process of ceramic and laboratory-processed composite restorations: A literature review. J Esthet Restor Dent. 2005;17:224–35. doi: 10.1111/j.1708-8240.2005.tb00119.x. [DOI] [PubMed] [Google Scholar]
- 32.Flury S, Lussi A, Peutzfeldt A, Zimmerli B. Push-out bond strength of CAD/CAM-ceramic luted to dentin with self-adhesive resin cements. Dent Mater. 2010;26:855–63. doi: 10.1016/j.dental.2010.05.001. [DOI] [PubMed] [Google Scholar]


