Abstract
Infection is a potentially serious complication of epidural analgesia and with an increase in its use in wards there is a necessity to demonstrate its safety. We aimed to compare the incidence of colonization of epidural catheters retained for short duration (for 48 h) postoperative analgesia in postanesthesia care unit and wards. It was a prospective observational study done in a tertiary care teaching public hospital over a period of 2 years and included 400 patients with 200 each belonged to two groups PACU and ward. We also studied epidural tip culture pattern, skin swab culture at the entry point of the catheter, their relation to each other and whether colonization is equivalent to infection. Data were analyzed using statistical software GraphPad. Overall positive tip culture was 6% (24), of them 7% (14) were from PACU and 5% (10) were from ward (P = 0.5285). Positive skin swab culture was 38% (150), of them 20% (80) were from PACU and 18% (70) were from ward (P = 0.3526). The relation between positive tip culture and positive skin swab culture in same patients is extremely significant showing a strong linear relationship (95% confidence interval = 0.1053–0.2289). The most common microorganism isolated was Staphylococcus epidermidis. No patient had signs of local or epidural infection. There is no difference in the incidence of epidural catheter tip culture and skin swab culture of patients from the general ward and PACU. Epidural analgesia can be administered safely for 48 h in general wards without added risk of infection. The presence of positive tip culture is not a predictor of epidural space infection, and colonization is not equivalent to infection; hence, routine culture is not needed. Bacterial migration from the skin along the epidural track is the most common mode of bacterial colonization; hence, strict asepsis is necessary.
Keywords: Epidural catheter infection, epidural catheterization, epidural colonization
Introduction
Postoperative epidural analgesia is one of the best pain relief modality with many advantages, but there is a potential for development of epidural infection.[1,2,3,4] Literature has mentioned the safety of epidural analgesia considering infectious complications time and again; nevertheless, some studies have reported severe complications such as meningitis and epidural abscess.[1,2,3,4,5,6]
In our institute, patients are observed in postanesthesia care unit (PACU/ICU) for postoperative epidural analgesia but due to limited beds in PACU some patients are sent to surgical wards. Stabille et al. proved that use of postoperative epidural analgesia in surgical ward patients has a low risk of infection.[2]
As there is a substantial increase in the use of epidural analgesia in wards, it is essential to demonstrate its safety and improve the quality of postoperative pain management in wards in a public hospital setup. Hence, we resolute to compare the incidence of colonization of epidural catheters retained for short duration (48 h) postoperative analgesia in PACU and wards. We also studied epidural tip culture pattern, skin swab culture at the entry point of the catheter, their relation with each other, and whether colonization is equivalent to infection.
Methodology
It was a prospective observational study conducted after approval from institutional ethics committee and valid, written, informed consent from patients. The study was carried out in the PACU and general wards of a tertiary care teaching public hospital over a period of 2 years and included 400 patients.
All consecutive adult patients (18–90 years) undergoing surgery requiring epidural anesthesia/analgesia were included in the study. These patients underwent abdominal, urological, orthopedic, and gynecological procedures (elective and emergency). We excluded patients who refused consent, epidural catheter malposition, malfunction or accidental removal of catheter. Anesthesia for the surgical procedures was according to the surgical requirement and attending anesthesiologist discretion which included epidural alone or combined with spinal or general anesthesia. Perioperative antibiotics were administered to all patients according to the surgical discretion.
Epidural catheter insertion was done in the operation theater by trained anesthesiologist at the lumbar or thoracic site. Standard aseptic protocol (wearing mask, sterile gown, gloves, and complete scrubbing) was followed. The parts were prepared with 10% povidone-iodine solution and rectified spirit twice and then covered with sterile drapes. The sterile disposable epidural catheter set 16/18 G with filter (Portex, Smiths Medical ASD, Inc., USA) was used. Dressing was done with transparent adhesive sterile drape (Primewear Hygiene Products Ltd., India)
Postoperatively, patients were attended thrice a day by pain control team in PACU and in wards. Complete aseptic precautions were followed during the administration of drugs for postoperative analgesia which was according to attending anesthesiologist decision and patients' need. Features suggestive of epidural space infection such as fever, pain in the back, tenderness, root pain, sensory or motor deficit, and laboratory parameters of infection were checked and epidural site was inspected for any tenderness, redness, or discharge. Routine dressing change was not done unless needed.
After 48 h, first the skin swab around the catheter was taken for culture then epidural catheter was removed after antiseptic skin preparation to avoid contamination by skin flora during withdrawal. The distal 2 cm catheter tip was aseptically cut with sterile scissors and sent to microbiology. In laboratory, samples were rolled in specific agar, incubated and observed for colonization, and recognized and reported by standard methods and criteria.[1,3]
We also noted age, sex, American Society of Anesthesiology (ASA) status, site of surgery, elective or emergency, number of attempts, temperature, and blood counts. The patients were followed up for symptoms and signs of epidural space infection daily till discharge from the hospital and they were asked to report if any of the above symptoms occurs.
Statistical analysis
Quantitative data expressed as a mean ± standard deviation or number of patients and percentage as appropriate. Qualitative data represented in the form of frequency and percentage. Sample size calculated considering the study by Srivastava et al. with 80% power of study and 95% confidence interval (CI).[1] The sample size was found to be 384 which were rounded to 400. Association between qualitative variables was assessed by Fisher's exact test for all 2 × 2 tables. P value was taken as significant when <0.05 and 95% CI of that fraction. Data were analyzed using statistical software (GraphPad Software Inc., California USA).
Results
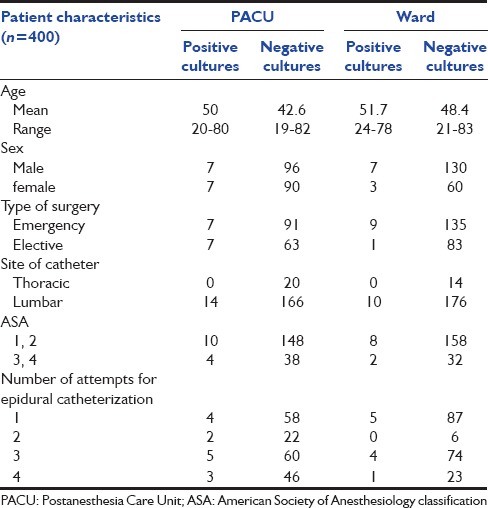
Of the 400 epidural catheter tips studied, 200 each belonged to two groups PACU and ward. Both the groups were comparable with respect to demographic parameters, site and type (elective or emergency) of surgical procedure, ASA status, number of attempts, etc., No statistically significant difference (P > 0.05) in the frequency of the catheter colonization was found in both the groups with respect to above factors. Of 400 tips sent for culture, 6% (24) showed positive culture, of them 14 (7%) were from PACU and 10 (5%) were from wards. On comparing catheter tip cultures of PACU and ward using Fisher's exact test the two-sided P value is 0.5285 (not significant).
Out of 400 skin swab culture, 38% (150) showed positive culture, of them 80 (20%) were from PACU and 70 (18%) were from wards. On comparing skin swab cultures of PACU and ward using Fisher's exact test, two-sided P value is 0.3526 (not significant). All 24 patients with positive tip culture had positive skin swab culture of the same microorganisms which is extremely significant with two-sided P < 0.0001. These variables show a strong linear relationship with 95% CI of that fraction: 0.1053–0.2289. Other characteristics studied among study groups are described in Table 1, and none of them had a significant association [Table 1].
Table 1.
Patient characteristics of postanesthesia care unit and ward
The most common microorganism identified was Staphylococcus epidermidis which represented 75% (18) of positive culture tips. Details of organisms isolated in PACU and ward are depicted in Figures 1 and 2.
Figure 1.
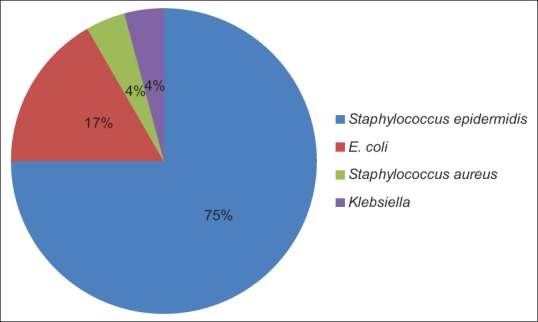
Organisms isolated in epidural tip culture
Figure 2.
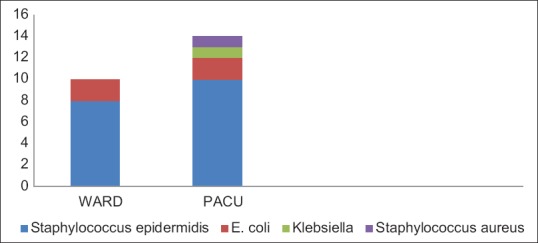
Comparison of organisms isolated from postanesthesia care unit and ward
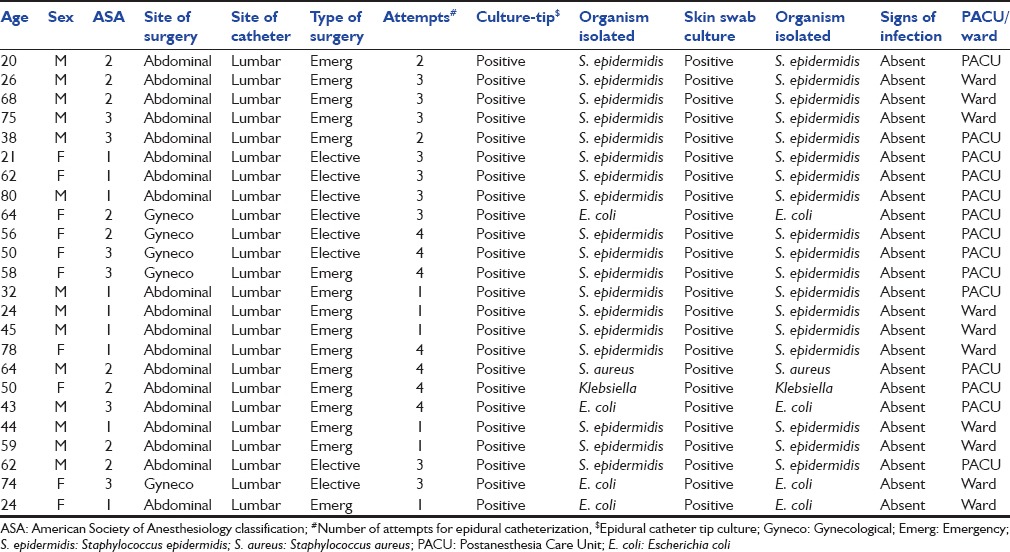
No patient including those with positive cultures had signs of local or epidural space infection. The clinical and bacteriological data of the patients with positive epidural catheter tip culture are detailed in Table 2.
Table 2.
Clinical and bacteriological data of patients with positive epidural tip culture
Discussion
The incidence of catheter tip colonization in this study was 6%. The reported incidence in the literature varies from 0% to 55%.[1,2,3,4,5,6,7,8,9,10] This broad variation could be due to the duration of catheter, use of perioperative antibiotics, different methodologies, and patient subsets.[7,8,9,10]
The rate of positive epidural catheter tip culture (5%) and skin swab culture of ward patients are comparable to PACU (7%) patients. Hence, if standard asepsis is maintained then there is no increased risk of epidural catheter infection in ward as compared to PACU. Stabille et al. also proved that use of postoperative epidural analgesia in surgical ward patients, under strict aseptic care, has low risk of bacterial colonization.[2]
We studied skin swab culture at the entry point of catheter was also studied along with epidural catheter tip. All 24 patients with positive tip culture had positive skin swab culture of the same microorganisms showing a strong linear relationship proving a significant correlation between bacterial colonization of the skin around the epidural catheter insertion site and the tip of the epidural catheter. This proves that bacteria migrate along epidural catheter track from the surrounding skin leading to colonization of epidural catheter tip; moreover, same microorganisms were isolated in these sites. Hence, meticulous disinfection of the skin during catheter insertion, sterile dressing and keeping the area dry and sterile during postoperative use are important points to reduce the incidence of catheter colonization. Yuan et al. suggested a common route for catheter colonization is via migration of bacteria along the catheter and advised a strict asepsis.[3] Few studies mention that alcoholic chlorhexidine for cutaneous antisepsis before epidural catheter insertion, subcutaneous tunneling of epidural catheter, using prophylactic antibiotics reduces the risk of catheter colonization.[10,11,12,13]
The most common microorganism identified in this study was S. epidermidis which represented 75% of positive culture tips. It is main human skin commensal of little clinical significance. Other studies also have shown it to be the most common pathogen of epidural catheter tip culture.[1,2,3,4,5,6,7,8,9,10,11,12] Other organisms identified were Escherichia coli 17% (4), Staphylococcus aureus, 4% (1) and Klebsiella 4% (1) of positive culture tips. Among E. coli positive epidural tip patients, 2 were from PACU and 2 from ward and all of them had undergone contaminated lower abdominal surgery. One patient each of SA and Klebsiella positive epidural tip was from PACU and had a respiratory infection of the same organism. The possibility of virulent microorganism colonizing epidural catheter is mentioned.[1,2,3,4,5,6,7,12]
Although there were positive catheter tips, there were no clinical findings of epidural space infection. Thus, despite colonization of the epidural catheter tip, infection of epidural space is not common, and the presence of positive tip culture is not a reliable predictor of epidural space infection demonstrating that routine culture of catheters may not be indicated. Many other studies have proved that colonization is not equivalent to infection, and routine culture of catheter tips is unnecessary.[1,2,3,4,5,6,7,10,11,12,13,14,15]
We also studied few risk factors supposed to be predictive of colonization [Table 1]. Although the colonization rate was higher in emergency and lower abdominal and gynecological surgeries than elective and lower limb and thoracic surgeries but the association is not significant. Similarly, even though all the positive catheter tips were from the lumbar site and none from the thoracic site; association could not be proved because of a lesser number of thoracic catheters.
Literature had mentioned many risk factors for developing epidural catheter infection; however, except few none had proved association. Longer durations of catheters are associated with higher incidence of infection.[2,9,15] However, in the current study, we analyzed catheters kept only for postoperative analgesia (48 h). The requirement of intense analgesia reduces after 48 h postoperatively and can be substituted with other modes of analgesia. Catheter localization in the groin, removal of the dressing, and omission of postoperative antibiotics as mentioned by Morin may be associated with but were not causal for bacterial colonization.[9] In this study, short duration use of catheter and perioperative antibiotics might have contributed to the low incidence of catheter colonization although not proven again stressing the point that short duration (48 h) postoperative epidural analgesia in wards can be safely continued.
Limitation of the study was that all the potential risk factors for epidural catheter infection could not be studied. To reduce epidural catheter colonization by skin flora due to migration through epidural track warrants further studies.
This study concludes that there is no difference in the rates of epidural catheter tip culture and skin swab culture of patients from the general ward and PACU/ICU. The presence of positive tip culture is not a predictor of epidural space infection, and colonization is not equivalent to infection. The most common organism in catheter tip culture and skin swab culture is S. epidermidis which is normal skin flora proving bacterial migration along the epidural track as the most common mode of bacterial colonization. Skin asepsis and maintaining sterility are critical to reduce colonization rate. Hence, we recommend that routine culture of epidural catheter is not advisable even in patients going to general wards and the quality postoperative analgesia using an epidural catheter with aseptic precautions can be continued in general wards without additional risk of infection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like acknowledge support from Dr. Anjali Swami Associate Professor Department of Microbiology TNMC and BYL Nair Ch. Hospital.
References
- 1.Srivastava U, Chandra P, Saxena S, Kumar A, Kannaujia A, Singh Rana SP, et al. Bacterial colonization and infection of epidural catheters: A prospective study of incidence and risk factors in surgical patients. Indian J Anaesth. 2007;51:496–500. [Google Scholar]
- 2.Stabille DM, Filho AD, Mandim BL, Araújo LB, Mesquita PM, Jorge MT. Frequency of colonization and isolated bacteria from the tip of the epidural catheter implanted for postoperative analgesia. Rev Bras Anestesiol. 2015;65:200–6. doi: 10.1016/j.bjan.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 3.Yuan HB, Zuo Z, Yu KW, Lin WM, Lee HC, Chan KH. Bacterial colonization of epidural catheters used for short-term postoperative analgesia: Microbiological examination and risk factor analysis. Anesthesiology. 2008;108:130–7. doi: 10.1097/01.anes.0000296066.79547.f3. [DOI] [PubMed] [Google Scholar]
- 4.Steffen P, Seeling W, Essig A, Stiepan E, Rockemann MG. Bacterial contamination of epidural catheters: Microbiological examination of 502 epidural catheters used for postoperative analgesia. J Clin Anesth. 2004;16:92–7. doi: 10.1016/j.jclinane.2003.05.007. [DOI] [PubMed] [Google Scholar]
- 5.Li J, Halaszynski TM. Regional anesthesia for acute pain management in elderly patients. World J Anesthesiol. 2014;3:82–95. [Google Scholar]
- 6.Trojanowski A, Janicki P. Bacterial contamination of epidural catheters used for perioperative analgesia. Internet J Anesthesiol. 2008;20:2. [Google Scholar]
- 7.Kostopanagiotou G, Kyroudi S, Panidis D, Relia P, Danalatos A, Smyrniotis V, et al. Epidural catheter colonization is not associated with infection. Surg Infect (Larchmt) 2002;3:359–65. doi: 10.1089/109629602762539571. [DOI] [PubMed] [Google Scholar]
- 8.Mishra S, Bhatnagar S, Srikanti M, Gupta D. Clinical implication of routine bacterial culture from epidural catheter tips in postoperative cancer patients: A prospective study. Anaesthesia. 2006;61:878–82. doi: 10.1111/j.1365-2044.2006.04753.x. [DOI] [PubMed] [Google Scholar]
- 9.Morin AM, Kerwat KM, Klotz M, Niestolik R, Ruf VE, Wulf H, et al. Risk factors for bacterial catheter colonization in regional anaesthesia. BMC Anesthesiol. 2005;5:1. doi: 10.1186/1471-2253-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sethna NF, Clendenin D, Athiraman U, Solodiuk J, Rodriguez DP, Zurakowski D. Incidence of epidural catheter-associated infections after continuous epidural analgesia in children. Anesthesiology. 2010;113:224–32. doi: 10.1097/ALN.0b013e3181de6cc5. [DOI] [PubMed] [Google Scholar]
- 11.Kinirons B, Mimoz O, Lafendi L, Naas T, Meunier J, Nordmann P. Chlorhexidine versus povidone iodine in preventing colonization of continuous epidural catheters in children: A randomized, controlled trial. Anesthesiology. 2001;94:239–44. doi: 10.1097/00000542-200102000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Yentur EA, Luleci N, Topcu I, Degerli K, Surucuoglu S. Is skin disinfection with 10% povidone iodine sufficient to prevent epidural needle and catheter contamination? Reg Anesth Pain Med. 2003;28:389–93. doi: 10.1016/j.rapm.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Min BM, Kim JH. Epidural catheterization with a subcutaneous injection port for the long-term administration of opioids and local anesthetics to treat zoster-associated pain – A report of two cases. Korean J Anesthesiol. 2013;65:462–7. doi: 10.4097/kjae.2013.65.5.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seth N, Macqueen S, Howard RF. Clinical signs of infection during continuous postoperative epidural analgesia in children: The value of catheter tip culture. Paediatr Anaesth. 2004;14:996–1000. doi: 10.1111/j.1460-9592.2004.01553.x. [DOI] [PubMed] [Google Scholar]
- 15.Ruppen W, Derry S, McQuay HJ, Moore RA. Infection rates associated with epidural indwelling catheters for seven days or longer: Systematic review and meta-analysis. BMC Palliat Care. 2007;6:3. doi: 10.1186/1472-684X-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


