Abstract
Cerebral venous thrombosis (CVT) is an uncommon cause of stroke. Paroxysmal nocturnal hemoglobinuria (PNH) is a rare type of hemolytic anemia, frequently associated with thrombophilia. PNH may rarely present with CVT. Approximately, one-third of the patients with CVT develop cerebral hemorrhage. Here, we present a rare combination of CVT presenting with intracerebral hemorrhage in a patient with PNH. High index of suspicion is needed to avoid misdiagnosis. Patient was successfully managed with anticoagulation therapy.
Keywords: Cerebral venous thrombosis, intracerebral hemorrhage, paroxysmal nocturnal hemoglobinuria
Introduction
Cerebral venous thrombosis (CVT) is an uncommon cause of stroke, representing 0.5–1% of all strokes.[1] Paroxysmal nocturnal hemoglobinuria (PNH) is an acquired disorder of hematopoietic stem cells. It is characterized by hemolytic anemia, marrow failure, and thrombophilia. Affected stem cells are deficient in glycosylphosphatidylinositol (GPI)-anchored proteins. Thrombophilia is a major cause of morbidity and mortality in PNH.[2] CVT is reported in 2–8% of patients with PNH.[3]
Approximately, one-third of CVT patients develops intracerebral hemorrhage (ICH). Presentation with cerebral hemorrhage may be challenging and a common pitfall in diagnosing CVT.[4] Identification of these patients is critical given that the pathophysiology underlying hemorrhage in such cases is distinct from other causes of ICH, and this has important treatment implications.[1]
Here, we present a rare case of CVT presenting with ICH in a patient with PNH. Patient was successfully managed with anticoagulation.
Case Report
A 45-year-old female, weighing around 60 kg, presented with severe headache, multiple episodes of vomiting, and confusion for 5 days. It was associated with weakness of right side of the body. On examination, her Glasgow Coma Scale was 14 and motor power was 4/5 in the right upper and lower extremities. Fundoscopy revealed papilledema. There was no history of trauma, and she had no seizure. Computed tomography (CT) scan of the head revealed intracerebral hematoma in the left temporal region with perilesional edema and mass effect [Figure 1]. She was a known case of PNH, diagnosed 5 years back. She had a significant number of CD 55 and CD 59 negative red cells in flow cytometry. She also had an episode of mesenteric vein thrombosis 2 years back, confirmed in CT angiography of the abdomen. Since then she was on life-long anticoagulation with warfarin 4 mg daily. Her blood investigations revealed hemoglobin of 7.2 g/dL and INR of 1.58. Her platelet count was normal. On the background of PNH and subtherapeutic anticoagulation, CVT was suspected. Magnetic resonance venography (MRV) revealed left transverse sinus thrombosis [Figure 2].
Figure 1.
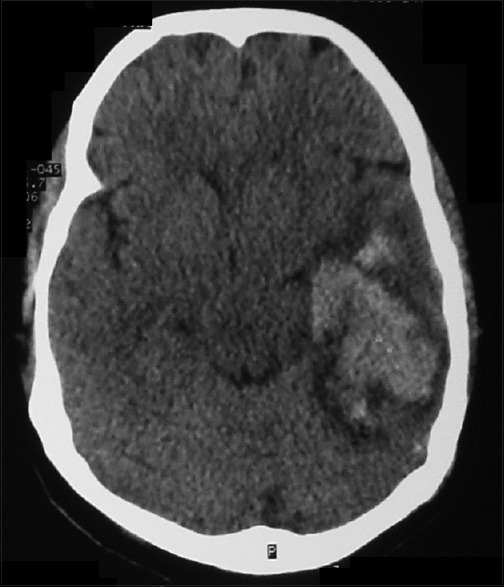
Computed tomography scan of head revealing intracerebral hematoma in left temporal region with perilesional edema and mass effect
Figure 2.
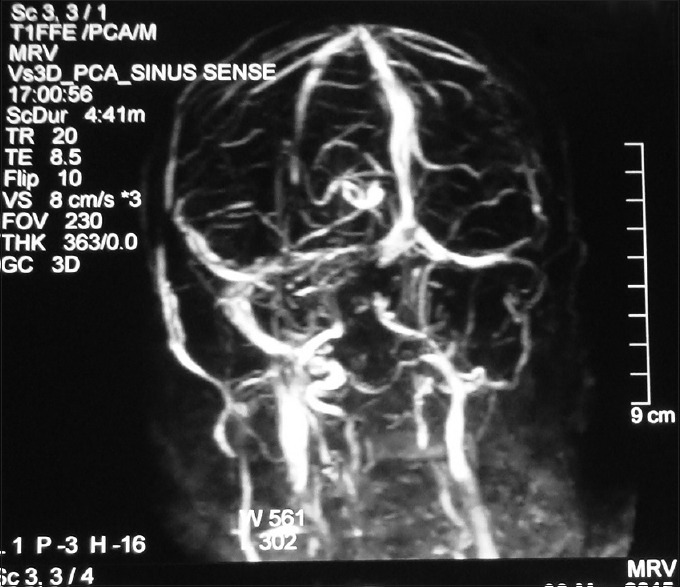
Magnetic resonance venography showing left transverse sinus thrombosis
She was admitted in Intensive Care Unit and started on enoxaparin 60 mg subcutaneous twice daily for 14 days. Warfarin 5 mg daily was overlapped during the last 3 days of therapy with low molecular weight heparin with the target INR of 2.0–3.0. Eculizumab was not started due to nonavailability. Her symptoms progressively improved, and she was discharged home after 15 days of admission.
Discussion
In patients with PNH, deficiency of GPI-anchored complement regulatory proteins CD55 and CD59 accounts for intravascular hemolysis. It is identified in flow cytometry and is diagnostic of PNH.[2] Venous thrombosis occurs in up to 40% of patients with PNH and represents a major cause of death.[3] Involvement of unusual site (hepatic, mesenteric, cerebral, and dermal veins) is characteristic of the thrombophilia of PNH. Indefinite anticoagulation is recommended following a thromboembolic event.[2] Our patient was diagnosed as per the flow cytometric findings. She was on lifetime anticoagulation following mesenteric vein thrombosis.
CVT is uncommon and frequently unrecognized type of stroke. Diagnosis and management can be difficult because of diversity of underlying risk factors, variation in clinical presentation, and absence of uniform treatment approach.[5] It is more commonly seen in young individuals. Prothrombotic conditions are the most widely studied risk factors for CVT.[1] With proper treatment, outcome is often favorable, with mortality between 3% and 8%.[3] Among patients with CVT, incidence of cerebral hemorrhage is 35–39% and is usually associated with poorer outcome.[4]
Headache, generally indicative of an increase in intracranial pressure, is the most common symptom in CVT. Clinical manifestations also depend on the location of thrombosis. Delay in diagnosis is common and around 56% of patients present with subacute (>48 h to 30 days) onset of symptoms.[1] Headache, mental status disorder, confusion, loss of consciousness, aphasia, seizure, and papilledema are commonly found in hemorrhagic CVT, which is consistent with our patient's findings.[4] Recurrent thrombosis is not uncommon in patients with PNH.[6] Subtherapeutic INR in our patient may have predisposed to recurrent thrombosis. Eculizumab, a monoclonal antibody against the complement protein 5, has been shown to dramatically alter the natural course of PNH, also reducing the thrombotic events.[7] It was not administered to our patient because of nonavailability. MRI and MRV are the most recommended imaging modality for the diagnosis of CVT.[1,8]
Anticoagulation therapy in CVT helps to prevent thrombus growth, facilitates recanalization, and prevents deep vein thrombosis or pulmonary embolism. Controversy has ensued as ICH can be present at the time of diagnosis CVT, and it may also complicate treatment.[1] However, anticoagulant treatment has been shown to be safe and associated with potentially important reduction in the risk of death or dependency without promoting ICH.[9] Therefore, patients with CVT without contraindications for anticoagulation should be treated with heparin. Concomitant ICH related to CVT is not a contraindication for heparin therapy.[8] When compared with unfractionated heparin, low molecular weight heparin may be associated with lower hospital mortality in patients with CVT.[10] Hence, enoxaparin was chosen in our patient. Fibrinolytic therapy and thrombectomy were not attempted as the patient gradually improved with anticoagulation.
To conclude, PNH is a rare cause of CVT. High index of suspicion is needed for correct diagnosis of CVT presenting with ICH. Identification of these patients is important due to significant treatment implications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Saposnik G, Barinagarrementeria F, Brown RD, Jr, Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and management of cerebral venous thrombosis: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:1158–92. doi: 10.1161/STR.0b013e31820a8364. [DOI] [PubMed] [Google Scholar]
- 2.Parker C, Omine M, Richards S, Nishimura J, Bessler M, Ware R, et al. Diagnosis and management of paroxysmal nocturnal hemoglobinuria. Blood. 2005;106:3699–709. doi: 10.1182/blood-2005-04-1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meppiel E, Crassard I, Peffault de Latour R, de Guibert S, Terriou L, Chabriat H, et al. Cerebral venous thrombosis in paroxysmal nocturnal hemoglobinuria: A series of 15 cases and review of the literature. Medicine (Baltimore) 2015;94:e362. doi: 10.1097/MD.0000000000000362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pongmoragot J, Saposnik G. Intracerebral hemorrhage from cerebral venous thrombosis. Curr Atheroscler Rep. 2012;14:382–9. doi: 10.1007/s11883-012-0260-1. [DOI] [PubMed] [Google Scholar]
- 5.Sasidharan PK. Cerebral vein thrombosis misdiagnosed and mismanaged. Thrombosis. 2012;2012:210676. doi: 10.1155/2012/210676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferro JM, Canhão P. Cerebral venous sinus thrombosis: Update on diagnosis and management. Curr Cardiol Rep. 2014;16:523. doi: 10.1007/s11886-014-0523-2. [DOI] [PubMed] [Google Scholar]
- 7.Kelly RJ, Hill A, Arnold LM, Brooksbank GL, Richards SJ, Cullen M, et al. Long-term treatment with eculizumab in paroxysmal nocturnal hemoglobinuria: Sustained efficacy and improved survival. Blood. 2011;117:6786–92. doi: 10.1182/blood-2011-02-333997. [DOI] [PubMed] [Google Scholar]
- 8.Einhäupl K, Stam J, Bousser MG, De Bruijn SF, Ferro JM, Martinelli I, et al. EFNS guideline on the treatment of cerebral venous and sinus thrombosis in adult patients. Eur J Neurol. 2010;17:1229–35. doi: 10.1111/j.1468-1331.2010.03011.x. [DOI] [PubMed] [Google Scholar]
- 9.Coutinho J, de Bruijn SF, Deveber G, Stam J. Anticoagulation for cerebral venous sinus thrombosis. Cochrane Database Syst Rev. 2011;8:CD002005. doi: 10.1002/14651858.CD002005.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Misra UK, Kalita J, Chandra S, Kumar B, Bansal V. Low molecular weight heparin versus unfractionated heparin in cerebral venous sinus thrombosis: A randomized controlled trial. Eur J Neurol. 2012;19:1030–6. doi: 10.1111/j.1468-1331.2012.03690.x. [DOI] [PubMed] [Google Scholar]


