Abstract
PURPOSE:
The aim of this study was to report homemade glove port technique for single-incision laparoscopic appendectomy (SILA).
MATERIALS AND METHODS:
Our homemade glove port was composed of a size 6 latex sterile surgical glove, a sterilized plastic bangle, and three pieces of silicon tube (5 cm in length) that were used as the suction tube. Clinical data were retrospectively collected from those patients who underwent SILA at Bucheon St. Mary's Hospital, Bucheon, Gyeonggi-do, South Korea between February 2014 and June 2014, including patient demographics, and operative and postoperative outcomes. To compare the outcomes, a retrospective review was performed for those patients who underwent conventional laparoscopic appendectomy (CLA) between October 2013 and January 2014. Both SILA and CLA were performed by the same surgical team.
RESULTS:
The SILA and CLA groups included 37 and 57 patients, respectively. The mean age, weight, body mass index (BMI), operation time, and pathologic diagnosis of gangrenous appendicitis were not significantly different between the two groups. However, the mean hospital stay in the CLA group was significantly (P = 0.018) longer than that in the SILA group (4.2 days vs 3.5 days). There was no conversion to open surgery in both the groups. Of the cases who underwent SILA, 10 (27.0%) needed insertion of additional port and drain. There was one (3.2%) complication of umbilical surgical site infection.
CONCLUSION:
In this study, SILA, with homemade glove port, was technically feasible and safe at low cost.
Keywords: single-incision laparoscopic appendectomy, glove port
INTRODUCTION
Single-incision laparoscopic surgery (SILS) is increasingly used in various surgical areas due to several advantages including better cosmesis, less incisional pain, and the ability to convert to standard multiport laparoscopic surgery if necessary.[1,2,3,4,5] With the development of laparoscopic instruments, the areas of SILS have expanded. Many surgeons are able to easily begin SILS. These laparoscopic instruments include SILS port (Covidien, Norwalk, CN, USA), Uni-X (Pnavel Systems Inc., Morganville, NJ, USA), X-Cone (KARL STORZ, Tuttlingen, Germany), and specialized customized dissector and graspers.[6] However, using these instruments in SILS might increase health-care costs. To reduce health-care costs, many authors have used their own tools for SILS. In this report, we describe the use of homemade glove port in single-incision laparoscopic appendectomy (SILA).
MATERIALS AND METHODS
A retrospective study was conducted for patients who underwent SILA for acute appendicitis by a surgical team between February 2014 and June 2014. Data pertaining to the patients’ demographics, operative time, length of hospital stay, and perioperative complications (if present) were retrospectively collected. The data collected from these patients were subsequently compared to those who underwent the conventional three-port conventional laparoscopic appendectomy (CLA) from October 2013 to January 2014. This study was approved by the Institutional Review Board of The Catholic University, Bucheon St. Mary's Hospital in Bucheon, Gyeonggi-do, South Korea.
All the patients were diagnosed with appendicitis, based on abdominal computed tomography with contrast enhancement. The patients with complicated appendicitis such as perforated appendicitis, local abscess, or diffuse peritonitis, and those contraindicated for general anesthesia were excluded from the study.
Preparation of Homemade Glove Port
We prepared the homemade glove port with a size 6 latex sterile surgical glove (Ansell, Melaka, Malaysia), one flexible inner ring such as a sterilized plastic bangle (inner diameter = 4.0 cm), and three pieces of the silicon tube (Sejong Medical, Paju, Gyeonggi-do, Korea) (5 cm in length) that was used as the suction tube during the operation (inner diameter = 6 mm, outer diameter = 10 mm, Figures 1a and b). The flexible inner ring was placed within the wrist portion of the glove fold and rolled up to three or four times, and fixed with 2-0 Dermalon (Ethicone, NJ, USA) sutures in three directions. Three silcon tubes of 5 cm length were placed into the third, fourth, and fifth fingers of the glove by 1-0 silk ties (Ethicon, NJ, USA). The thumb of the glove was connected with carbon dioxide gas insufflator by 1-0 silk ties. The index finger was used for specimen removal with LapBag (Sejong Medical, Paju, Gyeonggi-do, Korea) or keeping a specimen when LapBag was not used.
Figure 1.

Homemade port system of SILA. A surgical glove was attached to three pieces of silicon tube (a) silicone tube used as suction tube (b)
Surgical Technique
Standard 5-mm laparoscopic equipment such as 30-degree angle telescope (Stryker, MI, USA) and straight rigid instrument identical to those used in conventional laparoscopy (including Babcock clamp (Covidien, CN, USA), grasper (Covidien, CN, USA), scissors (Covidien, CN, USA), and electrocautery (Covidien, CN, USA)) were used to perform our SILA [Figure 2]. Each patient was placed in the supine position under general anesthesia. Using the open incision method, a vertical incision through the center umbilicus measuring 2-2.5 cm was made. The homemade glove port with three silicon tube channels [Figures 1a and b] was placed into the defect created in the abdominal wall. The inner ring of the glove port was placed deep into the peritoneum. The pneumoperitoneum was established with an intra-abdominal pressure of 12 mmHg. The telescope was introduced through a silicon tube channel that was placed in the fourth glove finger, and the peritoneal cavity was examined. Once the appendix was identified and isolated, the mesoappendix was dissected and cauterized using bipolar diathermy. The diameter of the rigid laparoscopic instruments was smaller than the silicon tube channel's inner diameter. Carbon dioxide gas leaked through the third and fifth finger channels. We solved this by holding silicon tube channels with Kelly clamps (Aesculap, Tuttlingen, Germany) [Figure 3]. The appendiceal base was ligated with one application of Vicryl endo-loop (Sejong Medical, Paju, Gyeonggi-do, Korea). The appendix was retrieved via the umbilical port site with or without LapBag (Sejong Medical, Paju, Gyeonggi-do, Korea) [Figure 4]. The abdominal cavity was washed with saline. If there was any difficulty in some cases, additional port was placed in the right lower quadrant abdomen and then the drain was inserted at the end of SILA. After removing the glove port, the umbilical fascia was closed with 2-0 Vicryl suture (Covidien, CN, USA). The subcutaneous layer was sutured with 4-0 Monocryl suture (Covidien, CN, USA). The umbilical skin was approximated with Steri-Strips (3M, Saint Paul, MN, USA). An umbilical dressing was applied using a piece of gauze packed into the umbilicus covered with an occlusive dressing. CLA was performed using 3-trocar techniques with a 11-mm infraumbilical trocar (Sejong Medical, Paju, Gyeonggi-do, Korea) placed by the Hasson open technique, and two additional 5-mm torcars (Sejong Medical, Paju, Gyeonggi-do, Korea) were placed in the suprapubic area and the right lower quadrant abdomen. The remaining details of the appendectomy procedure were the same as that of SPLA. LapBag (Sejong Medical, Paju, Gyeonggi-do, Korea) was used in all the CLA cases.
Figure 2.
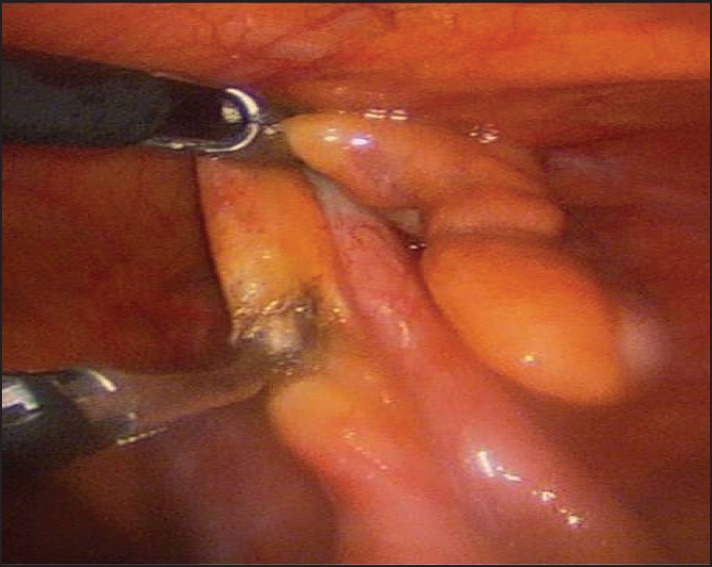
Appendiceal artery was cauterized by dissector
Figure 3.
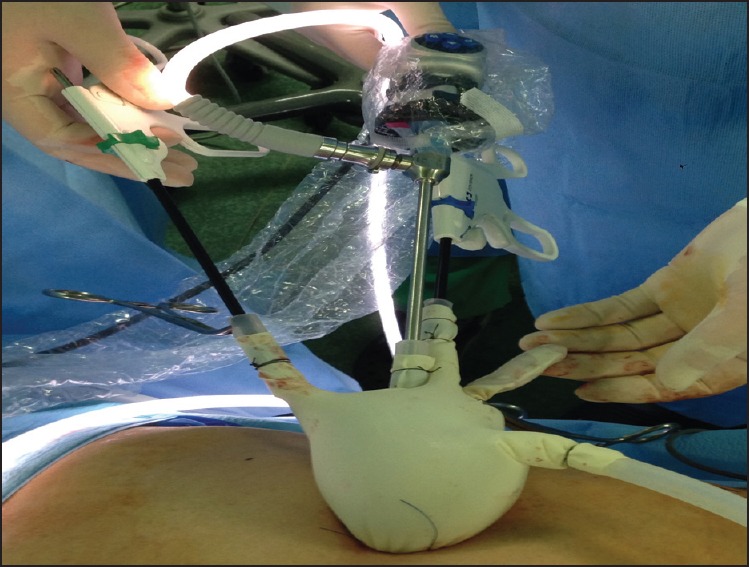
In situ glove port after SILA. An appendix was in the index finger of glove; gas insufflators connected with thumb of glove, and Kelly clamp used to prevent gas leakage
Figure 4.
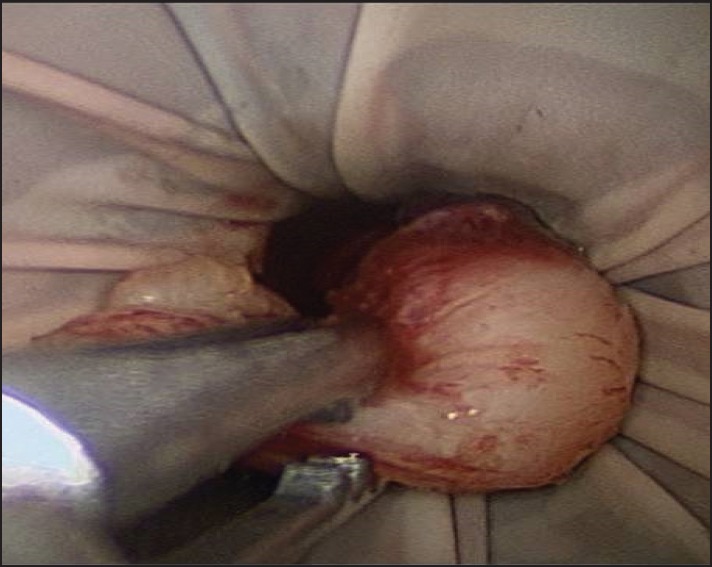
Appendix removed through glove port without LapBag
Statistical analysis
Continuous variables were compared using independent sample and two-tailed Student t test. Discrete variables were analyzed with chi-square test. A P value <0.05 was considered significant.
RESULTS
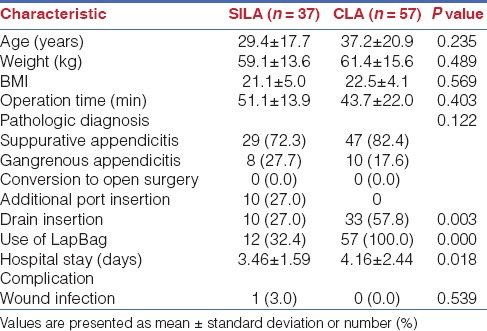
A total of 37 patients underwent SILA from February 2014 to June 2014. By the same surgical team, a total of 57 patients underwent CLA from October 2013 to January 2014. There was no significant difference in the mean age (29.4 years vs 37.2 years, P = 0.235), weight (59.1 kg vs 61.4 kg, P = 0.489), or body mass index (BMI) (21.1 vs 22.5, P = 0.569) between the two groups. In the SILA group, pathologic examinations revealed 29 (72.3%) cases with acute suppurative appendicitis and eight (27.7%) cases with acute gangrenous appendicitis. In the CLA group, 47 (82.4%) patients had acute suppurative appendicitis and 10 (17.6%) patients had acute gangrenous appendicitis (P = 0.122). There was no significant difference in the mean operative time (43.68 min vs 51.08 min, P = 0.403). None of the cases required conversion to open appendectomy. There were 10 (27.0%) cases who needed placement of additional port and drain in the SILA group. Drain was used in 33 (57.8%) cases in the CLA group. LapBag (Sejong Medical, Paju, Gyeonggi-do, Korea) for retrieving the appendix was used in 12 (32.4%) cases in the SILA group and in all (100%) cases in the CLA group (P = 0.000). The mean hospital stay was significantly (P = 0.018) shorter in the SILA group than in the CLA group (3.46 days vs 4.16 days). In both groups, there was no intraoperative complication in the early or late periods. In the SILA group, there was one (3.0%) postoperative complication with umbilical surgical site infection, which was treated at an outpatient setting as a superficial wound infection. The rate of complication was not significantly (P = 0.539) different between the two groups [Table 1].
Table 1.
Clinicopathological characteristics and perioperative outcomes
DISCUSSION
Laparoscopic appendectomy is a widely performed procedure due to its advantages in reducing postsurgical pain and decreasing operative trauma with quicker recovery, shorter hospital stay, and improved cosmesis. Single-incision laparoscopic surgery (SILS) could potentially bring out more advantages of the laparoscopic surgery.[1,2,3,4,5] Usually, many surgeons accepted that SILS would take longer operative time and need specialized, flexible, and curved devices.[6,7] There are several commercially available devices such as SILS port (Covidien, Norwalk, CN, USA), Uni-X (Pnavel Systems Inc., Morganville, NJ, USA), R-port (advanced Surgical Concepts, Wicklow, United Kingdom), and curved or articulating instruments.[6] These instruments have contributed to the expansion of SILS in various surgical areas. However, using them has increased the cost of surgery. To provide the benefits of SILS with low health-care cost, some surgeons have tried SILA using the conventional rigid instruments and noncommercial SILS ports.[8,9] Reflecting this trend, we made our homemade glove port that required a size 6 sterile surgical glove, 2-0 Dermalon (Ethicone, NJ, USA), and three pieces of silicon tube. Our SILA was performed with standard rigid laparoscopic instruments and a 30-degree 5-mm telescope.
In this study, the demographics, operation time, pathologic diagnosis, and complication rate in the two groups were not significantly different. Patients in the SILA group had a significantly shorter (P = 0.018) length of hospital stay than those in the CLA group (3.46 days vs 4.16 days). The length of hospital stay of both the groups is longer than that observed in other countries as the health-care cost for hospitalization is very low in Korea. We used the same postoperative treatments and same policy of discharge for both the groups. Therefore, the difference in the length of hospital stay might be associated with different rates of drain insertion in the SPLA and the CLA groups (27.0% vs 57.8%, P = 0.003). Our policy for drain insertion comprise dirty fluid collection in the abdominopelvic cavity, phlegmonous appendicitis, and any case that is considered delayed bleeding because we used bipolar diathermy for dissection and cauterization instead of energy devices to decrease health-care costs. Those patients with complicated appendicitis were excluded from the study because they needed delicate tissue handling, precise dissection, detailed washing inside the abdominal cavity, and longer operation time. We also excluded such cases in the CLA group for relatively accurate comparisons.
During our SILA, the appendix was retrieved via the umbilical incision site without using LapBag (Sejong Medical, Paju, Gyeonggi-do, Korea). The appendix was placed in the unused glove finger (67.6%). This type of appendix removal was reported by Kang et al.[10] We did not observe any postoperative intra-abdominal complication in the early or late periods (at least 3 months follow-up). If any case in the SILA group or if any part of specimen in the abdominal cavity was likely to be left due to its relatively big size than umbilical incision and friable appendix with severe inflammation, we used LapBag (Sejong Medical, Paju, Gyeonggi-do, Korea) to retrieve the appendix in the SILA group (32.4%). In the CLA group, all the appendices were removed by using LapBag (Sejong Medical, Paju, Gyeonggi-do, Korea).
Performing SILS by these technical modifications is associated with its own set of disadvantages such as leakage of carbon dioxide, sword fighting of instruments, chopstick effect, lack of triangulation, retrieval of specimen, and Swiss cheese hernia.[11] We used Kelly forceps (Aesculap, Tuttlingen, Germany) to occlude a small space between the silicon tube and the laparoscopic instruments to prevent gas leakage. Gas leakage between the telescope and the silicon tube did not occur. However, it made instrument fighting worse. Another big concern was the tearing of the glove port during the procedure. Fortunately, such instances did not occur. Despite these drawbacks, there was a very steep learning curve during the short time to successfully execute the critical steps of SILA. This may be due to the fact that appendectomy itself is not a complex procedure, and that the authors already have a lot of experience in laparoscopic surgery.
The biggest advantage of our homemade glove port and our procedure is that it is extremely cheaper than the other commercial devices. Our homemade port is easy to make and does not affect the patient's health-care cost like the other SILS devices. We also helped decrease the patient's health-care cost by not using LapBag (Sejong Medical, Paju, Gyeonggi-do, Korea) when the appendix was retrieved via the glove port without complications.
There are several limitations of this study. First, this study was retrospective in nature without any complicated cases. We did not analyze the postoperative pain score between SILA and CLA. Postoperative pain is a theoretical benefit of SILS.[5,12,13] However, recently reported meta-analysis[12] revealed similar pain scores between the SILA group and the conventionally treated groups.
CONCLUSION
In conclusion, this study demonstrated that SILA, using homemade glove port, is technically feasible and safe at a low cost. However, we do not want to force the use of our homemade glove port in SILS because commercially available ports for SILS have more advantages and safeties. Our objective is to offer another choice for SILA.
Footnotes
Source of Support: Nil
Conflicts of Interest: No competing financial interests exist.
REFERENCES
- 1.Oltmann SC, Garcia NM, Ventura B, Mitchell I, Fischer AC. Single-incision laparoscopic surgery: Feasibility for pediatric appendectomies. J Pediatr Surg. 2010;45:1208–12. doi: 10.1016/j.jpedsurg.2010.02.088. [DOI] [PubMed] [Google Scholar]
- 2.Lacher M, Muensterer OJ, Yannam GR, Aprahamian CJ, Perger L, Megison M, et al. Feasibility of single-incision pediatric endosurgery for treatment of appendicitis in 415 children. J Laparoendosc Adv Surg Tech A. 2012;22:604–8. doi: 10.1089/lap.2012.0107. [DOI] [PubMed] [Google Scholar]
- 3.Perez EA, Piper H, Burkhalter LS, Fischer AC. Single-incision laparoscopic surgery in children: A randomized control trial of acute appendicitis. Surg Endosc. 2013;27:1367–71. doi: 10.1007/s00464-012-2617-5. [DOI] [PubMed] [Google Scholar]
- 4.St Peter SD, Adibe OO, Juang D, Sharp SW, Garey CL, Laituri CA, et al. Single incision versus standard 3-port laparoscopic appendectomy: A prospective randomized trial. Ann Surg. 2011;254:586–90. doi: 10.1097/SLA.0b013e31823003b5. [DOI] [PubMed] [Google Scholar]
- 5.Kang DB, Lee SH, Lee SY, Oh JT, Park DE, Lee C, et al. Application of single incision laparoscopic surgery for appendectomy in children. J Korean Surg Soc. 2012;82:110–5. doi: 10.4174/jkss.2012.82.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raman JD, Bagrodia A, Cadeddu JA. Single-incision, umbilical laparoscopic versus conventional laparoscopic nephrectomy: A comparison of perioperative outcomes and short-term measures of convalescence. Eur Urol. 2009;55:1198–204. doi: 10.1016/j.eururo.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 7.Hong TH, Kim HL, Lee YS, Kim JJ, Lee KH, You YK, et al. Transumbilical single-port laparoscopic appendectomy (TUSPLA): Scarless intracorporeal appendectomy. J Laparoendosc Adv Surg Tech A. 2009;19:75–8. doi: 10.1089/lap.2008.0338. [DOI] [PubMed] [Google Scholar]
- 8.Bhatia P, Sabharwal V, Kalhan S, John S, Deed JS, Khetan M. Single-incision multi-port laparoscopic appendectomy: How I do it. J Minim Access Surg. 2011;7:28–32. doi: 10.4103/0972-9941.72372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee JA, Sung KY, Lee JH, Lee do S. Laparoscopic appendectomy with a single incision in a single institute. J Korean Soc Coloproctol. 2010;26:260–4. doi: 10.3393/jksc.2010.26.4.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kang KC, Lee SY, Kang DB, Kim SH, Oh JT, Choi DH, et al. Application of single incision laparoscopic surgery for appendectomies in patients with complicated appendicitis. J Korean Soc Coloproctol. 2010;26:388–94. doi: 10.3393/jksc.2010.26.6.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rao PP, Rao PP, Bhagwat S. Single-incision laparoscopic surgery - current status and controversies. J Minim Access Surg. 2011;7:6–16. doi: 10.4103/0972-9941.72360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saldaña LJ, Targarona EM. Single-incision pediatric endosurgery: A systematic review. J Laparoendosc Adv Surg Tech A. 2013;23:467–80. doi: 10.1089/lap.2012.0467. [DOI] [PubMed] [Google Scholar]
- 13.Park JH, Hyun KH, Park CH, Choi SY, Choi WH, Kim DJ, et al. Laparoscopic vs transumbilical single-port laparoscopic appendectomy; results of prospective randomized trial. J Korean Surg Soc. 2010;78:213–8. [Google Scholar]


