Abstract
Background. Hepatitis B virus (HBV) infections are perinatally transmitted from chronically infected mothers. Supplemental antiviral therapy during late pregnancy with lamivudine (LAM), telbivudine (LdT), or tenofovir (TDF) can substantially reduce perinatal HBV transmission compared to postnatal immunoprophylaxis (IP) alone. However, the cost-effectiveness of these measures is not clear.
Aim. This study evaluated the cost-effectiveness from a societal perspective of supplemental antiviral agents for preventing perinatal HBV transmission in mothers with high viral load (>6 log10 copies/mL).
Methods. A systematic review and network meta-analysis were performed for the risk of perinatal HBV transmission with antiviral therapies. A decision analysis was conducted to evaluate the clinical and economic outcomes in China of four competing strategies: postnatal IP alone (strategy IP), or in combination with perinatal LAM (strategy LAM + IP), LdT (strategy LdT + IP), or TDF (strategy TDF + IP). Antiviral treatments were administered from week 28 of gestation to 4 weeks after birth. Outcomes included treatment-related costs, number of infections, and quality-adjusted life years (QALYs). One- and two-way sensitivity analyses were performed to identify influential clinical and cost-related variables. Probabilistic sensitivity analyses were used to estimate the probabilities of being cost-effective for each strategy.
Results. LdT + IP and TDF + IP averted the most infections and HBV-related deaths, and gained the most QALYs. IP and TDF + IP were dominated as they resulted in less or equal QALYs with higher associated costs. LdT + IP had an incremental $2,891 per QALY gained (95% CI [$932–$20,372]) compared to LAM + IP (GDP per capita for China in 2013 was $6,800). One-way sensitivity analyses showed that the cost-effectiveness of LdT + IP was only sensitive to the relative risk of HBV transmission comparing LdT + IP with LAM + IP. Probabilistic sensitivity analyses demonstrated that LdT + IP was cost-effective in most cases across willingness-to-pay range of $6,800 ∼ $20,400 per QALY gained.
Conclusions. For pregnant HBV-infected women with high levels of viremia, supplemental use of LdT during late pregnancy combined with postnatal IP for infants is cost-effective in China.
Keywords: Cost-effective, Pregnancy, Lamivudine, Telbivudine, Tenofovir, Hepatitis b virus, Perinatal transmission
Introduction
Chronic hepatitis B virus (HBV) infection is a serious public health problem in China that affects ∼93 million people (7.18% of the population), representing a quarter of all HBV-infected people worldwide (Liang et al., 2009). HBV-related liver diseases and liver cancer are responsible for up to 300,000 deaths each year (World Health Organization, 2013). The economic burden of HBV infections in China alone is estimated to be in excess of 80 billion US dollars annually (Chinese Center for Disease Control and Prevention, 0000).
The predominant mode of HBV infection involves perinatal transmission from chronically infected mothers to their infants (Gambarin-Gelwan, 2007; Patton & Tran, 2014; Stevens et al., 1975). This can be suppressed by passive immunization with hepatitis B immunoglobulin (HBIG) administered within 12 h of birth and active immunization with a three-dose HBV vaccination series (Lee et al., 2006). The success of these immunoprophylaxis (IP) measures is demonstrated by the low prevalence of hepatitis B surface antigen (HBsAg) in children under five years of age in mainland China and the substantial reduction in HBV infection in Taiwan (Liang et al., 2009; Ni et al., 2007).
Despite these encouraging results, a proportion of infants still test positive for the HBsAg (Lee et al., 2006). The mother’s viral load in serum is an important contributing factor, as infants born from HBeAg (hepatitis B e-antigen) positive mothers with high levels of viremia are at greatest risk for perinatal transmission (Burgis et al., 2014; Burk et al., 1994; Del Canho et al., 1994). HBV replication in pregnant mothers can safely be suppressed with nucleos(t)ide analogues, such as lamivudine (LAM), telbivudine (LdT), and tenofovir(TDF), (Brown et al., 2012; Fontana, 2009; Wang et al., 2013; Yi, Liu & Cai, 2012) which reduce perinatal transmission when administered during the third trimester (Celen et al., 2013; Han et al., 2011; Lu et al., 2014; Pan et al., 2012). Previous studies indicate that supplemental prenatal use of LAM is cost-effective compared with postnatal IP only (Fan et al., 2014; Hung & Chen, 2011; Nayeri et al., 2012; Unal et al., 2011). Although LdT and TDF are more potent, the costs for these treatments are higher. Therefore, the purpose of this study was to examine the cost-effectiveness of these treatments from a societal perspective for prevention of perinatal transmission of HBV in China.
Materials and Methods
Model and strategies
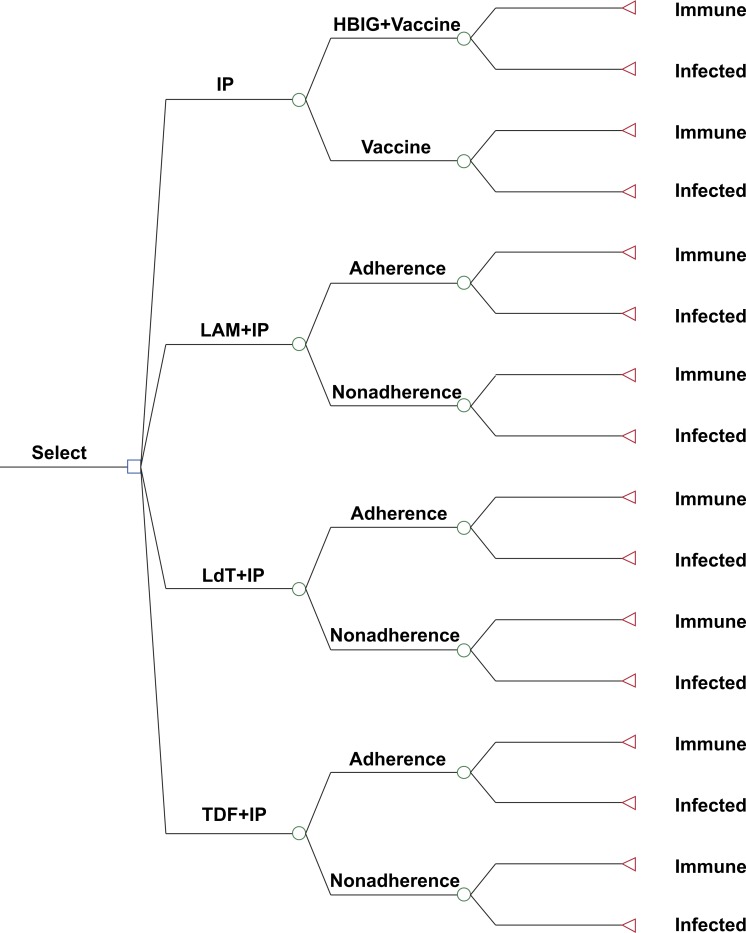
Decision analysis software (TreeAge Pro 2012: TreeAge Software Inc., Williamstown, MA, USA) was used to estimate the clinical and economic outcomes for a hypothetical cohort of 10,000 pregnant Chinese women chronically infected with HBV. All women were considered positive for HBeAg with serum levels of HBV-DNA >6 log10 copies/mL. The following four strategies were compared: (1) postnatal IP for the infants only; (2) perinatal LAM and postnatal IP (LAM + IP); (3) perinatal LdT and postnatal IP (LdT + IP); and (4) perinatal TDF and postnatal IP (TDF + IP) (Fig. 1). Perinatal antiviral treatments were administered to the pregnant women beginning from week 28 of gestation to 4 weeks after birth. Perinatal transmission of HBV was defined as HBsAg positive of infants 6 months after birth.
Figure 1. Decision tree model showing the four strategies for preventing perinatal hepatitis B transmission.
HBIG, hepatitis B immunoglobulin; IP, immunoprophylaxis; LAM, lamivudine; LdT, telbivudine; TDF, tenofovir.
If infants were infected by HBV, their lifetime clinical and economic outcomes were simulated using a Markov model based on a previous study (Hutton, So & Brandeau, 2010) (Fig. S1). This model was composed of the following eight states: normal alanine aminotransferase (ALT), elevated ALT, durable response, compensated cirrhosis, decompensated cirrhosis, hepatocellular carcinoma, liver transplantation, and death. The cycle length was one year and the cycle number was set to 73 corresponding to the life expectancy of Chinese people (National Health and Family Planning Commission of the People’s Republic of China, 2013).
Systematic review and meta-analysis
A systematic review and network meta-analysis were performed to calculate odds ratios (ORs) for perinatal transmission of HBV; see Fig. S2 and Article S1. Briefly, PubMed, Embase, Cochrane Central Register of Controlled Trials, and the Chinese Biomedical Literature Database were searched to identify controlled studies addressing prenatal antiviral therapy. Although a number of studies evaluating LAM + IP or LdT + IP versus IP were identified, very few compared LAM + IP and LdT + IP directly (Fig. S3 and Table S1) (Feng & Zhang, 2007; Guo et al., 2008; Xu et al., 2009; Zhang, 2010; Zhao et al., 2010; Guo & Zhang, 2011; Han et al., 2011; Yao et al., 2011; Zhou et al., 2011; Pan et al., 2012; Peng et al., 2012; Wang, 2012; Wang & Zhao, 2012; Bai, Shang & Li, 2013; Jiang et al., 2013; Sun et al., 2013; Wu et al., 2013; Zeng et al., 2013; Yu et al., 2014; Zhang et al., 2014). As a result, a network meta-analysis was deemed more suitable (Caldwell, Ades & Higgins, 2005). All clinical estimates and their ranges are shown in Table 1.
Table 1. Clinical variables for base-case and sensitivity analysis.
Notes.
- ALT
- alanine aminotransferase
- HBV
- hepatitis B virus
- HCC
- hepatocellular carcinoma
- IP
- immunoprophylaxis
- LAM
- lamivudine
- LdT
- telbivudine
- TDF
- tenofovir
Prevention efficacy of LAM was assumed to not be superior to LdT.
The reported ORs of HBV transmission were 0.21 (95% CI [0.12–0.38]) for LAM + IP versus IP, and 0.55 (95% CI [0.24–1.29]) for LdT + IP versus LAM + IP. The corresponding relative risks (RRs) of HBV transmission were then calculated using the formula: RR = OR∕((1 − P0) + (P0 × OR)), where P0 indicates the incidence of HBV transmission in the IP (for LAM + IP versus IP) or LAM + IP (for LdT + IP versus LAM + IP) groups based on the weighted mean by the study sample size; P0 = 0.117 and 0.027, respectively. Furthermore, the 95% CIs of the ORs were transformed to RR form for sensitivity analyses. An equal risk of HBV transmission was assumed for TDF + IP and LdT + IP in the base-case analyses based on the antiviral potencies of TDF and LdT and two small-sized studies (Celen et al., 2013; Pan et al., 2012; Lai et al., 2007; Marcellin et al., 2008). For sensitivity analyses, it was assumed that the risk for TDF + IP was not likely to be less than half of that for LdT + IP. The range of transmission rates for the IP group reported in each study were recorded and included in sensitivity analyses.
Although IP is the current recommendation in China to interrupt perinatal hepatitis B transmission, (Chinese Society of Hepatology and Chinese Society of Infectious Diseases, 2011; Chinese Society of Gynaecology and Obstetrics, 2013) the compliance rate varies across regions (Cui et al., 2013; Guo et al., 2010; Hu et al., 2012). Using estimates of the proportions of children receiving HBV vaccine plus HBIG in three regions reported by Cui et al. (2013) the overall proportion was calculated by weighting the sample size from each region.
The high reported adherence to antiviral treatment in pregnant mothers (Celen et al., 2013; Feng & Zhang, 2007; Guo et al., 2008; Xu et al., 2009; Zhang, 2010; Zhao et al., 2010; Guo & Zhang, 2011; Han et al., 2011; Yao et al., 2011; Zhou et al., 2011; Pan et al., 2012; Peng et al., 2012; Wang, 2012; Wang & Zhao, 2012; Bai, Shang & Li, 2013; Jiang et al., 2013; Sun et al., 2013; Wu et al., 2013; Zeng et al., 2013; Yu et al., 2014; Zhang et al., 2014) is likely due to a variety of factors, including a strong desire to protect their infants against HBV, the safety of the antiviral agents, short duration of treatment, and low incidence of drug resistance (Brown et al., 2012; Fontana, 2009; Wang et al., 2013; Yi, Liu & Cai, 2012; Ayres et al., 2014; Ho & Tran, 2011). For those who did not fully comply, the risk of HBV transmission was assumed to equal that of IP alone. For mothers who chose antiviral strategies, 100% coverage of IP for their infants was assumed, regardless of their adherence to antiviral treatment.
Under the National Immunization Program, free HBV vaccinations are available to all Chinese infants, covering 97.6% of infants born from HBsAg-positive mothers in 2009 (Cui et al., 2013). Therefore, it was assumed that infants who did not receive HBIG at birth were covered by the HBV vaccination. According to a meta-analysis, the risk of HBV transmission with vaccination only is nearly twice that with vaccination plus HBIG (RR 1.85, 95% CI [1.37–2.44]) (Lee et al., 2006).
We obtained from a published study the natural history estimates of chronic HBV infection and health-state utility weights for calculating quality-adjusted life years (QALYs) (Hutton, So & Brandeau, 2010). An age-specific death rate table was used to estimate the death probabilities for HBV-infected people without complications and uninfected people (National Bureau of Statistics of China, 2013a).
Costs
For cost analyses, the costs of HBV-marker tests (inclusive of HBeAg and HBsAg tests), HBV-DNA quantification, antiviral drugs, vaccination, and HBIG were included. The actual cost of HBV-DNA quantification for one mother who is going to receive antiviral treatment was calculated as n + 1 times the cost of one test, where n indicates the ratio of the proportion of mothers with HBV-DNA < 6 log10 copies/mL to those with HBV-DNA > 6 log10 copies/mL, as previously described (Fung et al., 2011). The cost of only one dose of HBIG was included, as a meta-analysis showed that multiple doses of HBIG are not superior to a single dose of HBIG in preventing perinatal transmission of HBV (Lee et al., 2006).
The costs of vaccination and HBIG were obtained from published studies, (Guo et al., 2012; Shi & Zhang, 2013), LAM and LdT from Price Bureau of Shaanxi Province, (Price Bureau of Shaanxi Province, 0000), and TDF from Kangdele Pharmacy (2014). The costs for HBV-related diseases incorporated direct medical costs and non-medical costs for physician visits, medications, lab tests, and transportation, and indirect costs for work loss, as reported in published studies (Chen, Yao & Chen, 2007; Hu & Chen, 2009).
All cost estimates were converted to US Dollars according to the 2013 conversion rate (1 US Dollar = 6.13 Chinese Yuan) using the medical care component of the Consumer Price Index and discounting costs and QALYs to 2013 amounts at a rate of 3% per year (National Bureau of Statistics of China, 2013b). All cost estimates and their ranges are listed in Table 2.
Table 2. Cost variables for base-case and sensitivity analysis.
| Variable | Base case (USD) | Range (USD) | Ref. |
|---|---|---|---|
| Hepatitis B vaccination, three times | $3.0 | $1.5–6.0 | Shi & Zhang, 2013 |
| Hepatitis B immunoglobulin administration | $40.0 | $20.0–80.0 | Guo et al., 2012; Shi & Zhang, 2013 |
| LAM, dailya | $2.5 | $1.3–5.0 | Price Bureau of Shaanxi Province, 0000 |
| LdT, dailya | $3.6 | $1.8–7.2 | Price Bureau of Shaanxi Province, 0000 |
| TDF, dailya | $8.7 | $4.4–17.4 | Kangdele Pharmacy, 2014 |
| Ratio of proportion of mothers with <6 to>6 log10 copies/mL HBV-DNA | 0.136 | 0.068–0.273 | Fung et al., 2011 |
| HBV-DNA quantification | $16.3 | $8.2–32.6 | Price Bureau of Shaanxi Province, 0000 |
| HBV-marker test | $3.3 | $1.6–6.6 | Price Bureau of Shaanxi Province, 0000 |
| Chronic hepatitis B, annualb | $1,780 | $890–3,560 | Hu & Chen, 2009 |
| Compensated cirrhosis, annual | $2,759 | $1,380–5,518 | Hu & Chen, 2009 |
| Decompensated cirrhosis, annual | $5,130 | $2,565–10,260 | Hu & Chen, 2009 |
| Hepatocellular carcinoma, annual | $7,302 | $3,651–14,604 | Hu & Chen, 2009 |
| Liver transplantation, first year | $37,458 | $18,729–74,916 | Chen, Yao & Chen, 2007 |
| Liver transplantation, second and subsequent years, annual | $3,276 | $1,638–6,552 | Chen, Yao & Chen, 2007 |
| Discount rate, annual | 3% | 0–5% | – |
Notes.
- HBV
- hepatitis B virus
- LAM
- lamivudine
- LdT
- telbivudine
- TDF
- tenofovir
- USD
- US Dollar
Administered from week 28 of gestation to 4 weeks after delivery.
50% of patients with durable response were assumed to continue receiving treatment.
Outcomes
Short-term outcomes evaluated clinical and economic outcomes during the period from the initiation of the strategies to 6 months after birth, including the number of infections, incremental infections averted, prophylaxis costs, incremental costs, and the corresponding incremental cost-effectiveness ratio (ICER). Long-term outcomes evaluated lifetime clinical and economic outcomes under four strategies, including HBV-related death, QALYs, incremental QALYs, lifetime costs, incremental lifetime costs, and the corresponding ICER. The ICER was used to compare alternative strategies after eliminating those that were dominated (more costly and less effective). It was calculated as the incremental cost divided by the incremental health benefit (e.g., infections averted and QALYs gained) for one strategy compared to the next less-costly strategy. The cost-effectiveness analyses were conducted from a societal perspective in accordance with the World Health Organization recommendations, and cost-effectiveness thresholds were based on the gross domestic product (GDP) per capita: highly cost-effective (ICER < GDP per capita); cost-effective (GDP per capita < ICER < 3 × GDP per capita); and not cost-effective (ICER > 3 × GDP per capita) (World Health Organization, 2014). The GDP per capita for China in 2013 was approximately $6,800 (National Bureau of Statistics of China, 2013b).
Sensitivity analyses
One- and two-way sensitivity analyses were performed to identify influential clinical and cost-related variables. In addition, a probabilistic sensitivity analysis was conducted based on a second-order Monte Carlo simulation (Geisler, 2011). All variables from Table 1 that were put into the simulation were assumed to follow a triangle distribution (likeliest, minimum, and maximum values) (Kanwal et al., 2005). A total of 1000 trials were simulated, and cost-effectiveness acceptability curves for competing strategies were constructed.
Results
Base-case analyses
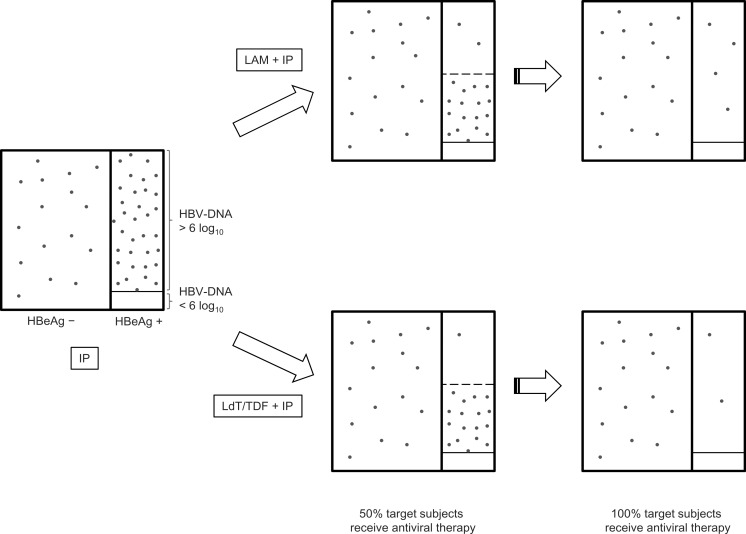
Antiviral strategies prevented more perinatal hepatitis B transmissions than IP alone. The fewest number of infections occurred with LdT + IP and TDF + IP (Fig. 2). Short-term cost was increased with effectiveness, except for TDF + IP, which was equally as effective as LdT + IP, but at more than twice the cost (Table 3).
Figure 2. Effect of antiviral strategies on reducing perinatal hepatitis B transmission.
The area of each rectangle represents the proportion of pregnant women, and the density of dots represents the probability of perinatal transmission of HBV. The unit of HBV-DNA is copies/mL. HBeAg, hepatitis B e antigen; HBV, hepatitis B virus; IP, immunoprophylaxis; LAM, lamivudine; LdT, telbivudine; TDF, tenofovir.
Table 3. Short-term outcomes.
| Strategy | Infections (n) | Incremental infections averted (n) | Cost (USD) | Incremental cost (USD) | ICER |
|---|---|---|---|---|---|
| IP | 1,727 | – | $239,000 | – | – |
| LAM + IP | 284 | 1,443 | $3,078,568 | $2,839,568 | 1,967 |
| LdT + IP | 167 | 117 | $4,147,944 | $1,069,376 | 9,178 |
| TDF + IP | 167 | 0 | $9,105,960 | $4,958,016 | – |
Notes.
- ICER
- incremental cost-effectiveness ratio (US dollars per incremental infection averted)
- IP
- immunoprophylaxis
- LAM
- lamivudine
- LdT
- telbivudine
- TDF
- tenofovir
- USD
- US Dollar
In the long-term, the more effective strategies resulted in fewer instances of hepatocellular carcinoma and HBV-related death, and increased the QALYs (Table 4). IP and TDF + IP were dominated because they resulted in the same or fewer QALYs but at a comparatively higher cost. LdT + IP had an incremental $2,891 per QALY gained (95% CI [−$932 ∼ $20,372]) compared to LAM + IP.
Table 4. Long-term outcomes.
| Strategy | HCC (n) | HBV-related deaths (n) | QALYs | Incremental QALYs | Cost (USD) | Incremental cost (USD) | ICER (95% CI) |
|---|---|---|---|---|---|---|---|
| IP | 385 | 304 | 292,167 | – | $4,897,077 | – | Dominated |
| TDF + IP | 37 | 29 | 295,664 | – | $9,556,428 | – | Dominated |
| LAM + IP | 63 | 50 | 295,403 | – | $3,843,301 | – | – |
| LdT + IP | 37 | 29 | 295,664 | 261 | $4,598,412 | $755,111 | $2,891 (−$932∼$20,372) |
Notes.
- CI
- confidence interval
- HBV
- hepatitis B virus
- HCC
- hepatocellular carcinoma
- ICER
- incremental cost-effectiveness ratio (US Dollar per quality-adjusted life year gained)
- IP
- immunoprophylaxis
- LAM
- lamivudine
- LdT
- telbivudine
- QALY
- quality-adjusted life year
- TDF
- tenofovir
- USD
- US Dollar
Sensitivity analyses
One-way sensitivity analyses were performed across the ranges of all clinical and cost-related variables. The cost-effectiveness of LdT + IP was only sensitive to one of them, the RR of HBV transmission in comparison to LAM + IP. If the RR is above 0.92, LdT + IP would be not cost-effective.
A two-way sensitivity analysis showed that LdT + IP remains cost-effective even when its cost is doubled and that of LAM halved. When TDF + IP protects more infants than LdT + IP and simultaneously the cost of TDF goes down, TDF + IP may become cost-effective (Fig. S4). With lower transmission risk of TDF + IP compared with LdT + IP, TDF + IP may also become cost-effective with changes in additional variables, such as the probabilities of HBV transmission for competing strategies, the discount rate, the cost of LdT, and the utility weight for the state of chronic HBV infection with normal ALT levels.
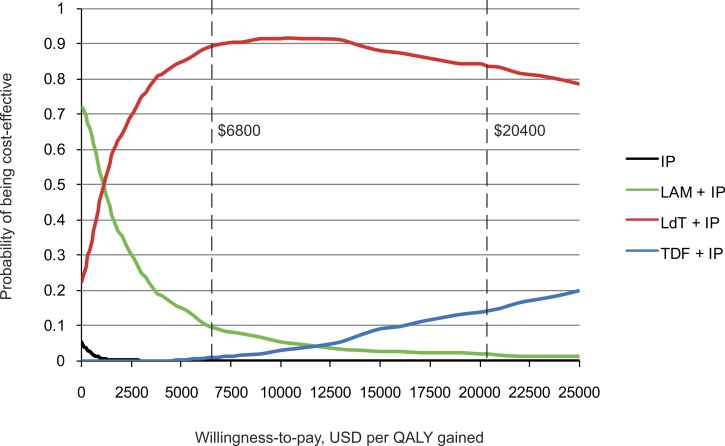
Acceptability curves constructed from probabilistic sensitivity analyses showed that LdT + IP was highly cost-effective in 89.8% of the trials under a willingness-to-pay threshold of $6,800, and cost-effective in 83.7% under a threshold of $20,400 (Fig. 3). As the price of TDF is likely to change in the near future, acceptability curves were simulated for a series of TDF cost from $8 to $3.6 daily. As the cost of TDF decreases, TDF + IP would become the most cost-effective strategy (Fig. S5).
Figure 3. Acceptability curves of the four strategies for preventing perinatal hepatitis B transmission.
Chinese gross domestic product per capita was approximately $6,800 in 2013. IP, immunoprophylaxis; LAM, lamivudine; LdT, telbivudine; TDF, tenofovir; USD, US Dollar; QALY, quality-adjusted life year.
Discussion
Antiviral treatment as prophylaxis for perinatal hepatitis B transmission is recommended in updated guidelines from the European Association for the Study of the Liver, Asian Pacific Association for the Study of the Liver, and the National Institute for Health and Care Excellence (European Association For The Study Of The Liver, 2012; Liaw et al., 2012; Sarri et al., 2013). However, there is no consensus regarding which antiviral agent is most appropriate. Only one agent, LAM, was included in previous cost-effectiveness analyses of high-income areas only (Fan et al., 2014; Hung & Chen, 2011; Nayeri et al., 2012; Unal et al., 2011). The results of the present analyses confirm that conventional IP alone is not cost-effective under any circumstance, and further demonstrate that supplemental use of LdT is highly cost-effective, and preferable over LAM or TDF in China.
Implementation of the National Immunization Program that provides HBV vaccinations to all neonates and extends HBIG administration to those whose mothers are infected with HBV has greatly reduced the prevalence of HBV (Liang et al., 2009; Cui et al., 2013). Thus, antiviral treatment during late pregnancy in women with a high viral load will have a further impact, not only in terms of health benefits but also in terms of economic costs. Supplementation of IP with LdT or LAM will dramatically reduce the overall number of HBV infections, and reduce perinatal transmission by at least half. Thus, one could expect the prevalence of HBV to be <0.5% among those at the highest risk for infection, i.e., children under five years of age. The initial additional cost of antiviral treatment will be outweighed by the reduced economic burden of HBV-related diseases.
From a cost-effectiveness perspective, China will benefit from the use of LAM or LdT antiviral strategies to prevent HBV transmission. Indeed, Chinese hepatologists in tertiary hospitals have been prescribing these agents to pregnant women with chronic HBV infection for several years (Li et al., 2003; Zhang & Wang, 2009). However, pregnant infected women are more likely to visit the obstetrics clinic first, and may not seek consultation from hepatologists. The recent guideline from the Chinese Society of Obstetrics and Gynecology recommends against antiviral treatment as prophylaxis of perinatal transmission of HBV (Chinese Society of Gynaecology and Obstetrics, 2013). A survey of Chinese obstetricians showed that only 11.7% agree with antiviral treatment during pregnancy (Hu et al., 2013). Delayed update of evidence and differences in research interest between obstetricians and hepatologists may contribute to the above knowledge and practices among gynaecology staff. The findings presented in this study highlight the critical need to further summarize the clinical evidence and evaluate the cost-effectiveness of antiviral treatment to prevent perinatal transmission of HBV.
Sensitivity analyses indicate that the tradeoff between the use of LdT and LAM is influenced by the RR of HBV transmission. However, LdT remains more cost-effective than LAM when transmission risk is reduced by >8%. The sensitivity analyses also indicate that more information is needed concerning the efficacy and cost of TDF. It is difficult to determine an added benefit of TDF when studies with large sample sizes show a 100% efficacy with LdT (Han et al., 2011; Yu et al., 2014; Zhang et al., 2014). As a result, the cost of TDF becomes the main variable affecting its cost-effectiveness. TDF is less expensive than LdT in Western countries such as Spain, (Buti et al., 2009), where TDF would be considered more cost-effective assuming an equal efficacy to LdT. On this point, our results are consistent with the recent guidelines of the National Institute for Health and Care Excellence (Sarri et al., 2013). TDF will also become cost-effective in China as its cost decreases.
There are several important strengths of the current study. This study is the first decision analysis that compares all currently available antiviral agents for the prevention of perinatal transmission of HBV. In the model used for the analyses, the only variables that differed among each antiviral strategy were the prevention efficacy and the cost. Consistent with previous studies, (Fan et al., 2014; Hung & Chen, 2011; Nayeri et al., 2012; Unal et al., 2011) LAM was found to be cost-effective compared with the conventional IP, indicating that the findings concerning LdT and TDF are similarly valid and reliable. In addition, a systematic review was performed to summarize the prevention efficacy of each antiviral agent. Included in the current analyses are two newly published high-quality studies with large sample sizes (Yu et al., 2014; Zhang et al., 2014). Finally, a network meta-analysis was used to evaluate the efficacies of each strategy, which combines direct and indirect comparisons and is superior to traditional pairwise analyses when there is an insufficient number of direct comparison studies (Caldwell, Ades & Higgins, 2005).
There are some limitations of this study that should be mentioned. First, the risk of side effects when using antiviral agents during pregnancy was not considered. However, controlled studies demonstrate that LAM, LdT, or TDF do not increase the number of birth defects or complications (Brown et al., 2012; Celen et al., 2013; Feng & Zhang, 2007; Guo et al., 2008; Xu et al., 2009; Zhang, 2010; Zhao et al., 2010; Guo & Zhang, 2011; Han et al., 2011; Yao et al., 2011; Zhou et al., 2011; Pan et al., 2012; Peng et al., 2012; Wang, 2012; Wang & Zhao, 2012; Bai, Shang & Li, 2013; Jiang et al., 2013; Sun et al., 2013; Wu et al., 2013; Zeng et al., 2013; Yu et al., 2014; Zhang et al., 2014). Second, there is no consensus on when antiviral treatment should be withdrawn, though most studies chose four weeks after delivery as the end time. Except for a small fraction of mothers continuing to receive the treatment because of elevated ALT levels, most mothers discontinued the treatment as planned with no associated severe adverse events, though the results for mothers were not included in the current model. Third, there is no consensus on the threshold of HBV-DNA level for initiating antiviral treatment in pregnant women. Like most studies of relevant topic, the analysis used the threshold of 6 log10 copies/mL. Lastly, the analysis focused only on pregnant women positive for HBeAg. Further studies evaluating strategies to prevent perinatal transmission of HBV from HBeAg-negative mothers are needed (Kubo et al., 2014; Pan et al., 2012).
In conclusion, this cost-effectiveness analysis focusing on pregnant women positive for HBeAg with HBV-DNA > 6 log10 copies/mL suggests that supplemental use of LdT during late pregnancy combined with IP for their infants is cost-effective in China.
Supplemental Information
Each infant is immune to or chronically infected with hepatitis B virus (HBV). Infected infants reside in of the following states each year: normal alanine aminotransferase (ALT), elevated ALT, durable response, compensated cirrhosis, decompensated cirrhosis, hepatocellular carcinoma, liver transplantation, or dead (not shown).
The nodes are weighted by sample size and the edges are weighted by the number of studies.
HBV, hepatitis B virus; IP, immunoprophylaxis; LdT, telbivudine; TDF, tenofovir; USD, US Dollar.
TDF cost: $8, $7, $6, $5, $4, and $3.6. Chinese gross domestic product per capita was approximately $6,800 in 2013. IP, immunoprophylaxis; LAM, lamivudine; LdT, telbivudine; TDF, tenofovir; USD, US Dollar; QALY; quality-adjusted life year.
Abbreviations
- ALT
alanine aminotransferase
- CI
confidence interval
- HBeAg
hepatitis B e antigen
- HBIG
hepatitis B immunoglobulin
- HBsAg
hepatitis B surface antigen
- HBV
hepatitis B virus
- ICER
incremental cost-effectiveness ratio
- IP
immunoprophylaxis
- LAM
lamivudine
- LdT
telbivudine
- OR
odds ratio
- QALY
quality-adjusted life year
- RR
relative risk
- TDF
tenofovir
Funding Statement
The authors received no funding for this work.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Wenjun Wang conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Jingjing Wang and Guihua Zhuang performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, reviewed drafts of the paper.
Shuangsuo Dang conceived and designed the experiments, wrote the paper, reviewed drafts of the paper.
Data Availability
The following information was supplied regarding data availability:
The research in this article did not generate any raw data.
References
- Ayres et al. (2014).Ayres A, Yuen L, Jackson KM, Manoharan S, Glass A, Maley M, Yoo W, Hong SP, Kim SO, Luciani F, Bowden DS, Bayliss J, Levy MT, Locarnini SA. Short duration of lamivudine for the prevention of hepatitis B virus transmission in pregnancy: lack of potency and selection of resistance mutations. Journal of Viral Hepatitis. 2014;21:809–817. doi: 10.1111/jvh.12212. [DOI] [PubMed] [Google Scholar]
- Bai, Shang & Li (2013).Bai HL, Shang HL, Li ZL. The clinical study of telbivudine in blocking intrauterine transmission of hepatitis B virus during late pregnancy. Zhong Guo Yi Xue Gong Cheng. 2013;21:53–54. [Google Scholar]
- Brown et al. (2012).Brown RS, Jr, Verna EC, Pereira MR, Tilson HH, Aguilar C, Leu CS, Buti M, Fagan EA. Hepatitis B virus and human immunodeficiency virus drugs in pregnancy: findings from the Antiretroviral Pregnancy Registry. Journal of Hepatology. 2012;57:953–959. doi: 10.1016/j.jhep.2012.06.031. [DOI] [PubMed] [Google Scholar]
- Burgis et al. (2014).Burgis J, Kong D, Salibay C, Zipprich J, Harriman K, So S. Risk factors associated with immunoprophylaxis failure in infants born to mothers with chronic hepatitis b infection in california [Abstract] Gastroenterology. 2014;146:S-762. [Google Scholar]
- Burk et al. (1994).Burk RD, Hwang LY, Ho GY, Shafritz DA, Beasley RP. Outcome of perinatal hepatitis B virus exposure is dependent on maternal virus load. Journal of Infectious Diseases. 1994;170:1418–1423. doi: 10.1093/infdis/170.6.1418. [DOI] [PubMed] [Google Scholar]
- Buti et al. (2009).Buti M, Brosa M, Casado MA, Rueda M, Esteban R. Modeling the cost-effectiveness of different oral antiviral therapies in patients with chronic hepatitis B. Journal of Hepatology. 2009;51:640–646. doi: 10.1016/j.jhep.2009.04.013. [DOI] [PubMed] [Google Scholar]
- Caldwell, Ades & Higgins (2005).Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;331:897–900. doi: 10.1136/bmj.331.7521.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celen et al. (2013).Celen MK, Mert D, Ay M, Dal T, Kaya S, Yildirim N, Gulsun S, Barcin T, Kalkanli S, Dal MS, Ayaz C. Efficacy and safety of tenofovir disoproxil fumarate in pregnancy for the prevention of vertical transmission of HBV infection. World Journal of Gastroenterology. 2013;19:9377–9382. doi: 10.3748/wjg.v19.i48.9377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Yao & Chen (2007).Chen D, Yao GB, Chen W. Economic evaluation of peginterferon afa-2a and lamivudine in the treatment of HBeAg-positive chronic hepatitis B. Chinese Journal of Clinical Infectious Diseases. 2007;25:468–472. [Google Scholar]
- Chinese Center for Disease Control and Prevention (0000).Chinese Center for Disease Control and Prevention Prevention and treatment of viral hepatitis. Available at http://www.chinacdc.cn/rdwd/201107/t20110726_49934.htm (accessed 9 August 2013)
- Chinese Society of Gynaecology and Obstetrics (2013).Chinese Society of Gynaecology and Obstetrics The clinical guideline of prevention for mother-to-child transmission of hepatitis B virus. Zhong Hua Fu Chan Ke Za Zhi. 2013;48:151–154. [Google Scholar]
- Chinese Society of Hepatology and Chinese Society of Infectious Diseases (2011).Chinese Society of Hepatology and Chinese Society of Infectious Diseases The guideline of prevention and treatment for chronic hepatitis B (2010 version) Zhonghua Gan Zang Bing Za Zhi. 2011;19:13–24. doi: 10.3760/cma.j.issn.1007-3418.2011.01.007. [DOI] [PubMed] [Google Scholar]
- Cui et al. (2013).Cui F, Luo H, Wang F, Zheng H, Gong X, Chen Y, Wu Z, Miao N, Kane M, Hennessey K, Hadler SC, Hutin YJ, Liang X, Yang W. Evaluation of policies and practices to prevent mother to child transmission of hepatitis B virus in China: results from China GAVI project final evaluation. Vaccine. 2013;31(Suppl 9):J36–J42. doi: 10.1016/j.vaccine.2012.11.061. [DOI] [PubMed] [Google Scholar]
- Del Canho et al. (1994).Del Canho R, Grosheide PM, Schalm SW, De Vries RR, Heijtink RA. Failure of neonatal hepatitis B vaccination: the role of HBV-DNA levels in hepatitis B carrier mothers and HLA antigens in neonates. Journal of Hepatology. 1994;20:483–486. doi: 10.1016/S0168-8278(05)80494-5. [DOI] [PubMed] [Google Scholar]
- European Association For The Study Of The Liver (2012).European Association For The Study Of The Liver EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. Journal of Hepatology. 2012;57:167–185. doi: 10.1016/j.jhep.2012.02.010. [DOI] [PubMed] [Google Scholar]
- Fan et al. (2014).Fan L, Owusu-Edusei K, Jr, Schillie SF, Murphy TV. Cost-effectiveness of testing hepatitis B-positive pregnant women for hepatitis B e antigen or viral load. Obstetrics and Gynecology. 2014;123:929–937. doi: 10.1097/AOG.0000000000000124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng & Zhang (2007).Feng HF, Zhang SF. Effect on interruption of hepatitis B virus vertical transmission by lamivudine. Shi Yong Er Ke Lin Chuang Za Zhi. 2007;22:1019–1020. [Google Scholar]
- Fontana (2009).Fontana RJ. Side effects of long-term oral antiviral therapy for hepatitis B. Hepatology. 2009;49:S185–S195. doi: 10.1002/hep.22885. [DOI] [PubMed] [Google Scholar]
- Fung et al. (2011).Fung J, Seto WK, Lai CL, Yuen J, Wong DK, Yuen MF. Profiles of HBV DNA in a large population of Chinese patients with chronic hepatitis B: implications for antiviral therapy. Journal of Hepatology. 2011;54:195–200. doi: 10.1016/j.jhep.2010.06.031. [DOI] [PubMed] [Google Scholar]
- Gambarin-Gelwan (2007).Gambarin-Gelwan M. Hepatitis B in pregnancy. Clinics in Liver Disease. 2007;11:945–963. doi: 10.1016/j.cld.2007.08.004. [DOI] [PubMed] [Google Scholar]
- Geisler (2011).Geisler BP. Automating first- and second-order Monte Carlo simulations for Markov models in TreeAge pro. In: Mordechai S, editor. Applications of Monte Carlo method in science and engineering. Shanghai: InTech; 2011. pp. 917–930. [Google Scholar]
- Guo et al. (2008).Guo YZ, Li SX, Ge SL, Wang JH. The clinical application of lamivudine in interdiction of maternal-to-child transmission for HBsAg, HBeAg-positive pregnant women. Lin Chuang He Li Yong Yao. 2008;1:8–9. [Google Scholar]
- Guo et al. (2010).Guo Y, Liu J, Meng L, Meina H, Du Y. Survey of HBsAg-positive pregnant women and their infants regarding measures to prevent maternal-infantile transmission. BMC Infectious Diseases. 2010;10:26. doi: 10.1186/1471-2334-10-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo & Zhang (2011).Guo HJ, Zhang Y. The efficacy of telbivudine in interrupting mother-to-child HBV transmission in pregnant women with high levels of viremia. Chang Zhi Yi Xue Yuan Xue Bao. 2011;25:368–370. [Google Scholar]
- Guo et al. (2012).Guo Y, Zhang W, Zhang Y, Lin X, Zhang B, Chen C, Du Y. Cost-effectiveness analysis of preventing mother-to-child transmission of hepatitis B by injecting hepatitis B immune globulin. European Journal of Gastroenterology & Hepatology. 2012;24:1363–1369. doi: 10.1097/MEG.0b013e32835847c6. [DOI] [PubMed] [Google Scholar]
- Han et al. (2011).Han GR, Cao MK, Zhao W, Jiang HX, Wang CM, Bai SF, Yue X, Wang GJ, Tang X, Fang ZX. A prospective and open-label study for the efficacy and safety of telbivudine in pregnancy for the prevention of perinatal transmission of hepatitis B virus infection. Journal of Hepatology. 2011;55:1215–1221. doi: 10.1016/j.jhep.2011.02.032. [DOI] [PubMed] [Google Scholar]
- Han et al. (2011).Han L, Zhang HW, Xie JX, Zhang Q, Wang HY, Cao GW. A meta-analysis of lamivudine for interruption of mother-to-child transmission of hepatitis B virus. World Journal of Gastroenterology. 2011;17:4321–4333. doi: 10.3748/wjg.v17.i38.4321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho & Tran (2011).Ho A, Tran TT. Pregnant women and their willingness to be treated for hepatitis B during pregnancy [Abstract] Gastroenterology. 2011;140:S930. [Google Scholar]
- Hu & Chen (2009).Hu M, Chen W. Assessment of total economic burden of chronic hepatitis B (CHB)-related diseases in Beijing and Guangzhou, China. Value Health. 2009;12(Suppl 3):S89–S92. doi: 10.1111/j.1524-4733.2009.00636.x. [DOI] [PubMed] [Google Scholar]
- Hu et al. (2013).Hu Y, Dai X, Zhou YH, Yang H. A knowledge survey of obstetrics and gynecology staff on the prevention of mother-to-child transmission of hepatitis B virus. Journal of Infection in Developing Countries. 2013;7:391–397. doi: 10.3855/jidc.2915. [DOI] [PubMed] [Google Scholar]
- Hung & Chen (2011).Hung HF, Chen HH. Cost-effectiveness analysis of prophylactic lamivudine use in preventing vertical transmission of hepatitis B virus infection. PharmacoEconomics. 2011;29:1063–1073. doi: 10.2165/11586470-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Hutton, So & Brandeau (2010).Hutton DW, So SK, Brandeau ML. Cost-effectiveness of nationwide hepatitis B catch-up vaccination among children and adolescents in China. Hepatology. 2010;51:405–414. doi: 10.1002/hep.23310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu et al. (2012).Hu Y, Zhang S, Luo C, Liu Q, Zhou YH. Gaps in the prevention of perinatal transmission of hepatitis B virus between recommendations and routine practices in a highly endemic region: a provincial population-based study in China. BMC Infectious Diseases. 2012;12:221. doi: 10.1186/1471-2334-12-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang et al. (2013).Jiang HN, Fan LY, Li DZ, Wan J, Ye JJ. Clinical trial of telbivudine in the treatment of chronic hepatitis B in patients during the third trimester of pregnancy. Lin Chuang Gan Dan Bing Za Zhi. 2013;29:101–103. [Google Scholar]
- Kangdele Pharmacy (2014).Kangdele Pharmacy 2014. Available at http://www.baiji.com.cn (accessed 16 October 2014)
- Kanwal et al. (2005).Kanwal F, Gralnek IM, Martin P, Dulai GS, Farid M, Spiegel BM. Treatment alternatives for chronic hepatitis B virus infection: a cost-effectiveness analysis. Annals of Internal Medicine. 2005;142:821–831. doi: 10.7326/0003-4819-142-10-200505170-00007. [DOI] [PubMed] [Google Scholar]
- Kubo et al. (2014).Kubo A, Shlager L, Marks AR, Lakritz D, Beaumont C, Gabellini K, Corley DA. Prevention of vertical transmission of hepatitis B: an observational study. Annals of Internal Medicine. 2014;160:828–835. doi: 10.7326/M13-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai et al. (2007).Lai CL, Gane E, Liaw YF, Hsu CW, Thongsawat S, Wang Y, Chen Y, Heathcote EJ, Rasenack J, Bzowej N, Naoumov NV, Di Bisceglie AM, Zeuzem S, Moon YM, Goodman Z, Chao G, Constance BF, Brown NA. Telbivudine versus lamivudine in patients with chronic hepatitis B. New England Journal of Medicine. 2007;357:2576–2588. doi: 10.1056/NEJMoa066422. [DOI] [PubMed] [Google Scholar]
- Lee et al. (2006).Lee C, Gong Y, Brok J, Boxall EH, Gluud C. Hepatitis B immunisation for newborn infants of hepatitis B surface antigen-positive mothers. Cochrane Database of Systematic Reviews. 2006;2006(2) doi: 10.1002/14651858.CD004790.pub2. CD004790. [DOI] [PubMed] [Google Scholar]
- Liang et al. (2009).Liang X, Bi S, Yang W, Wang L, Cui G, Cui F, Zhang Y, Liu J, Gong X, Chen Y, Wang F, Zheng H, Guo J, Jia Z, Ma J, Wang H, Luo H, Li L, Jin S, Hadler SC, Wang Y. Epidemiological serosurvey of hepatitis B in China–declining HBV prevalence due to hepatitis B vaccination. Vaccine. 2009;27:6550–6557. doi: 10.1016/j.vaccine.2009.08.048. [DOI] [PubMed] [Google Scholar]
- Liaw et al. (2012).Liaw YF, Kao JH, Piratvisuth T, Chan HLY, Chien RN, Liu CJ, Gane E, Locarnini S, Lim SG, Han KH, Amarapurkar D, Cooksley G, Jafri W, Mohamed R, Hou JL, Chuang WL, Lesmana LA, Sollano JD, Suh DJ, Omata M. Asian-Pacific consensus statement on the management of chronic hepatitis B: a 2012 update. Hepatology International. 2012;6:531–561. doi: 10.1007/s12072-012-9365-4. [DOI] [PubMed] [Google Scholar]
- Li et al. (2003).Li XM, Yang YB, Hou HY, Shi ZJ, Shen HM, Teng BQ, Li AM, Shi MF, Zou L. Interruption of HBV intrauterine transmission: a clinical study. World Journal of Gastroenterology. 2003;9:1501–1503. doi: 10.3748/wjg.v9.i7.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu et al. (2014).Lu YP, Liang XJ, Xiao XM, Huang SM, Liu ZW, Li J, Hocher B, Chen YP. Telbivudine during the second and third trimester of pregnancy interrupts HBV intrauterine transmission: a systematic review and meta-analysis. Clinical Laboratory. 2014;60:571–586. doi: 10.7754/clin.lab.2013.130408. [DOI] [PubMed] [Google Scholar]
- Marcellin et al. (2008).Marcellin P, Heathcote EJ, Buti M, Gane E, De Man RA, Krastev Z, Germanidis G, Lee SS, Flisiak R, Kaita K, Manns M, Kotzev I, Tchernev K, Buggisch P, Weilert F, Kurdas OO, Shiffman ML, Trinh H, Washington MK, Sorbel J, Anderson J, Snow-Lampart A, Mondou E, Quinn J, Rousseau F. Tenofovir disoproxil fumarate versus adefovir dipivoxil for chronic hepatitis B. New England Journal of Medicine. 2008;359:2442–2455. doi: 10.1056/NEJMoa0802878. [DOI] [PubMed] [Google Scholar]
- National Bureau of Statistics of China (2013a).National Bureau of Statistics of China 2013a. Available at http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm (accessed 9 August 2013)
- National Bureau of Statistics of China (2013b).National Bureau of Statistics of China 2013b. Available at www.stats.gov.cn (accessed 9 August 2013)
- National Health and Family Planning Commission of the People’s Republic of China (2013).National Health and Family Planning Commission of the People’s Republic of China 2013. China Public Health Statistical Yearbook 2011. Available at http://www.moh.gov.cn/zhuzhan/index.shtml (accessed 9 August 2013)
- Nayeri et al. (2012).Nayeri UA, Werner EF, Han CS, Pettker CM, Funai EF, Thung SF. Antenatal lamivudine to reduce perinatal hepatitis B transmission: a cost-effectiveness analysis. American Journal of Obstetrics and Gynecology. 2012;207(3):231. doi: 10.1016/j.ajog.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Ni et al. (2007).Ni YH, Huang LM, Chang MH, Yen CJ, Lu CY, You SL, Kao JH, Lin YC, Chen HL, Hsu HY, Chen DS. Two decades of universal hepatitis B vaccination in taiwan: impact and implication for future strategies. Gastroenterology. 2007;132:1287–1293. doi: 10.1053/j.gastro.2007.02.055. [DOI] [PubMed] [Google Scholar]
- Pan et al. (2012).Pan CQ, Duan ZP, Bhamidimarri KR, Zou HB, Liang XF, Li J, Tong MJ. An algorithm for risk assessment and intervention of mother to child transmission of hepatitis B virus. Clinical Gastroenterology and Hepatology. 2012;10:452–459. doi: 10.1016/j.cgh.2011.10.041. [DOI] [PubMed] [Google Scholar]
- Pan et al. (2012).Pan CQ, Han GR, Jiang HX, Zhao W, Cao MK, Wang CM, Yue X, Wang GJ. Telbivudine prevents vertical transmission from HBeAg-positive women with chronic hepatitis B. Clinical Gastroenterology and Hepatology. 2012;10:520–526. doi: 10.1016/j.cgh.2012.01.019. [DOI] [PubMed] [Google Scholar]
- Pan et al. (2012).Pan CQ, Mi LJ, Bunchorntavakul C, Karsdon J, Huang WM, Singhvi G, Ghany MG, Reddy KR. Tenofovir disoproxil fumarate for prevention of vertical transmission of hepatitis B virus infection by highly viremic pregnant women: a case series. Digestive Diseases and Sciences. 2012;57:2423–2429. doi: 10.1007/s10620-012-2187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton & Tran (2014).Patton H, Tran TT. Management of hepatitis B during pregnancy. Nature Reviews Gastroenterology & Hepatology. 2014;11:402–409. doi: 10.1038/nrgastro.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng et al. (2012).Peng BA, Zhao Y, Yang XF, Liao MF, Xu LH, Yu YH. The efficacy and safety of telbivudine in blocking mother-to-child transmission of hepatitis B virus. Zhong Guo Yao Xue Za Zhi. 2012;47:855–857. [Google Scholar]
- Price Bureau of Shaanxi Province (0000).Price Bureau of Shaanxi Province Available at www.sx111.com (accessed 9 August 2013)
- Sarri et al. (2013).Sarri G, Westby M, Bermingham S, Hill-Cawthorne G, Thomas H. Diagnosis and management of chronic hepatitis B in children, young people, and adults: summary of NICE guidance. BMJ. 2013;346:f3893. doi: 10.1136/bmj.f3893. [DOI] [PubMed] [Google Scholar]
- Shi & Zhang (2013).Shi G, Zhang SX. Decision tree and cost-benefit analysis on strategies related to preventing maternal-infantile transmission of hepatitis B virus infection. Zhonghua Liu Xing Bing Xue Za Zhi. 2013;34:273–278. [PubMed] [Google Scholar]
- Stevens et al. (1975).Stevens CE, Beasley RP, Tsui J, Lee WC. Vertical transmission of hepatitis B antigen in Taiwan. New England Journal of Medicine. 1975;292:771–774. doi: 10.1056/NEJM197504102921503. [DOI] [PubMed] [Google Scholar]
- Sun et al. (2013).Sun WH, Chu LL, Liu WL, Hao AH, Ma L, Wan Q, Ren R, Xin YN. Efficacy and safety of telbivudine in preventing mother-to-infant transmission of HBV in pregnant women in high HBV DNA load. Lin Chuang Gan Dan Bing Za Zhi. 2013;29:596–599. [Google Scholar]
- Unal et al. (2011).Unal ER, Lazenby GB, Lintzenich AE, Simpson KN, Newman R, Goetzl L. Cost-effectiveness of maternal treatment to prevent perinatal hepatitis B virus transmission. Obstetrics and Gynecology. 2011;118:655–662. doi: 10.1097/AOG.0b013e31822ad2c2. [DOI] [PubMed] [Google Scholar]
- Wang (2012).Wang EJ. Comparision of effecacy and safety between lamivudine and telbivudine in blocking vertical transmission of hepatitis B virus in late stage pregnancy. Quan Ke Yi Shi Za Zhi. 2012;15:3628–3630. [Google Scholar]
- Wang et al. (2013).Wang L, Kourtis AP, Ellington S, Legardy-Williams J, Bulterys M. Safety of tenofovir during pregnancy for the mother and fetus: a systematic review. Clinical Infectious Diseases. 2013;57:1773–1781. doi: 10.1093/cid/cit601. [DOI] [PubMed] [Google Scholar]
- Wang & Zhao (2012).Wang WP, Zhao J. The study of efficacy and side effects of telbivudine for treatment of patients with chronic hepatitis B in pregnant women. Xian Dai Fu Chan Ke Jin Zhan. 2012;21:697–699. [Google Scholar]
- World Health Organization (2013).World Health Organization Disease and injury country estimates, 2004-2008. 2013. Available at http://www.who.int/healthinfo/global_burden_disease/estimates_country_2004_2008/en (accessed 9 August 2013)
- World Health Organization (2014).World Health Organization Cost effectiveness and strategic planning (WHO-CHOICE) 2014. Available at http://www.who.int/choice/costs/en/ (accessed 16 October 2014)
- Wu et al. (2013).Wu QX, Deng GH, Li JN, Li L, Sun XW, Pan MM, Huang HF, He DM, Yan ZH, Xu C, Li MS, Tang W, Liu MD, Wang YM. Effects of telbivudine on transmission of HBsAg and HBeAg throught placenta in HBV infected pregnant women in second or third trimester. Di San Jun Yi Da Xue Xue Bao. 2013;35:665–668. [Google Scholar]
- Xu et al. (2009).Xu WM, Cui YT, Wang L, Yang H, Liang ZQ, Li XM, Zhang SL, Qiao FY, Campbell F, Chang CN, Gardner S, Atkins M. Lamivudine in late pregnancy to prevent perinatal transmission of hepatitis B virus infection: a multicentre, randomized, double-blind, placebo-controlled study. Journal of Viral Hepatitis. 2009;16:94–103. doi: 10.1111/j.1365-2893.2008.01056.x. [DOI] [PubMed] [Google Scholar]
- Yao et al. (2011).Yao ZC, Chen MC, Liao WY, Zhang YP, Wu Y, Li LY, Feng J, Lin MS, Chen CA, Zheng DG, Zhuang JQ. The efficacy and safety of telbivudine in blocking intrauterine hepatitis B viral transmission. Shi Yong Gan Zang Bing Za Zhi. 2011;14:259–261. [Google Scholar]
- Yi, Liu & Cai (2012).Yi W, Liu M, Cai HD. Safety of lamivudine treatment for chronic hepatitis B in early pregnancy. World Journal of Gastroenterology. 2012;18:6645–6650. doi: 10.3748/wjg.v18.i45.6645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu et al. (2014).Yu MM, Jiang Q, Ji Y, Wu KH, Ju LL, Tang X, Yang YF. Comparison of telbivudine versus lamivudine in interrupting perinatal transmission of hepatitis B virus. Journal of Clinical Virology. 2014;61:55–60. doi: 10.1016/j.jcv.2014.06.005. [DOI] [PubMed] [Google Scholar]
- Zeng et al. (2013).Zeng YM, Chen R, Lou GQ, Shi JP. Study of the strategy about cessation of lamivudine used in HBV intrauterine infection. Yi Xue Yan Jiu Za Zhi. 2013;42:87–90. [Google Scholar]
- Zhang (2010).Zhang YF. The effect of lamivudine on interruption of mother-to-child transmission in 50 pregnant women with chronic HBV infection. Shi Yong Fu Chan Ke Za Zhi. 2010;26:367–368. [Google Scholar]
- Zhang et al. (2014).Zhang H, Pan CQ, Pang Q, Tian R, Yan M, Liu X. Telbivudine or lamivudine use in late pregnancy safely reduces perinatal transmission of hepatitis B virus in real-life practice. Hepatology. 2014;60:468–475. doi: 10.1002/hep.27034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang & Wang (2009).Zhang LJ, Wang L. Blocking intrauterine infection by telbivudine in pregnant chronic hepatitis B patients. Zhonghua Gan Zang Bing Za Zhi. 2009;17:561–563. [PubMed] [Google Scholar]
- Zhao et al. (2010).Zhao BD, Liao XQ, Peng GJ, Liu J, Lin CH. The efficacy of telbivudine combined with HBV vaccine and HBIG in interrupting mother-to-child transmission of HBV in 60 cases. Zhong Guo Xian Dai Yao Wu Ying Yong. 2010;4:37–38. [Google Scholar]
- Zhou et al. (2011).Zhou YJ, Zheng JL, Pan HJ, Jiang S. Efficacy and safety of telbivudine in pregnant chronic hepatitis B patients. Zhong Hua Gan Zang Bing Za Zhi. 2011;19:861–862. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Each infant is immune to or chronically infected with hepatitis B virus (HBV). Infected infants reside in of the following states each year: normal alanine aminotransferase (ALT), elevated ALT, durable response, compensated cirrhosis, decompensated cirrhosis, hepatocellular carcinoma, liver transplantation, or dead (not shown).
The nodes are weighted by sample size and the edges are weighted by the number of studies.
HBV, hepatitis B virus; IP, immunoprophylaxis; LdT, telbivudine; TDF, tenofovir; USD, US Dollar.
TDF cost: $8, $7, $6, $5, $4, and $3.6. Chinese gross domestic product per capita was approximately $6,800 in 2013. IP, immunoprophylaxis; LAM, lamivudine; LdT, telbivudine; TDF, tenofovir; USD, US Dollar; QALY; quality-adjusted life year.
Data Availability Statement
The following information was supplied regarding data availability:
The research in this article did not generate any raw data.