Abstract
Introduction
Rapid developments in technology have encouraged the use of smartphones in health promotion research and practice. Although many applications (apps) relating to physical activity are available from major smartphone platforms, relatively few have been tested in research studies to determine their effectiveness in promoting health.
Methods
In this article, we summarize data on use of smartphone apps for promoting physical activity based upon bibliographic searches with relevant search terms in PubMed and CINAHL.
Results
After screening the abstracts or full texts of articles, 15 eligible studies of the acceptability or efficacy of smartphone apps for increasing physical activity were identified. Of the 15 included studies, 6 were qualitative research studies, 8 were randomized control trials, and one was a nonrandomized study with a pre-post design. The results indicate that smartphone apps can be efficacious in promoting physical activity although the magnitude of the intervention effect is modest. Participants of various ages and genders respond favorably to apps that automatically track physical activity (e.g., steps taken), track progress toward physical activity goals, and are user-friendly and flexible enough for use with several types of physical activity.
Discussion
Future studies should utilize randomized controlled trial research designs, larger sample sizes, and longer study periods to establish the physical activity measurement and intervention capabilities of smartphones. There is a need for culturally appropriate, tailored health messages to increase knowledge and awareness of health behaviors such as physical activity.
Keywords: Smartphone Applications, Health Promotion, Exercise, Obesity, Physical Activity, Randomized Controlled Trials
Introduction
Sedentary behavior and physical activity are important public health issues [1,2]. Approximately one-third of adults in the U.S. are physically inactive [1]. The increasing prevalence of obesity in the U.S. and many other countries and the independent association of obesity with several forms of cancer, cardiovascular disease, diabetes and other forms of chronic illness have prompted interest in identifying efficacious ways to promote physical activity and reduce obesity [2]. Among cancer survivors and persons living with other chronic illnesses, maintaining a healthy body weight reduces the risk of disease recurrence or progression [3]. There has been increasing interest in using cell phone text messaging and smartphone apps to promote physical activity. Smartphone apps provide a useful and generally low-cost way to disseminate information about lifestyle modification (e.g., physical activity and proper diet) to the general populations and to at-risk populations, including cancer survivors and people who are overweight or obese.
Mobile phones are a part of modern life. By the end of 2011, there were an estimated 6 billion mobile subscriptions, accounting for about 87% of the world’s population [4]. Rapid technological advances have led to the emergence of smartphones that combine the voice and text messaging functions of cell phones with powerful computing technology that can support third-party applications, Internet access, and wireless connectivity with other devices [4]. About 85% of adults in the U.S., including most African Americans and Hispanics, own a cell phone, and 53% own a smartphone [5]. All major smartphone platforms provide third-party developers with application programming interfaces that can be used to build special-purpose applications, referred to as native applications [4]. By April 2012, there were an estimated 13,600 consumer health apps for iPhones.
Apps relating to physical activity are available from major smartphone platforms (e.g., iPhone, Android, Nokia, and BlackBerry). Common techniques include providing instruction on how to perform exercises, modeling how to perform exercises, providing feedback on performance, goal-setting, self-monitoring, and planning social support and change in physical activity [6–8]. However, relatively few have been tested in order to determine their efficacy in promoting health. In addition, few of these apps are based on theories of health behavior change, most do not include evidence-based features such as reinforcement, and evidence-based recommendations for physical activity are rarely considered [6, 9].
In this article, we review published studies on the acceptability and efficacy of smartphone apps designed to promote physical activity or to lose weight. Of particular interest were randomized control trials of the efficacy of smartphone apps in increasing physical activity. We also examined the results of qualitative studies.
Materials and Methods
This review is based upon bibliographic searches in PubMed and CINAHL with relevant search terms. Articles published in English through August 2015 were identified using the following MeSH search terms and Boolean algebra commands: (smartphones) and ((physical activity) or (weight loss) or (weight gain) or (body weight) or (exercise weight) or (weight management)). The searches were not limited to words appearing in the title of an article. Studies that focused on patients with chronic diseases other than obesity, e.g., chronic obstructive pulmonary disease, myocardial infarction, or diabetes mellitus, were excluded. Information obtained from bibliographic searchrs (title and topic of article, information in abstract, geographic locality of a study, and key words) was used to determine whether to retain each article identified in this way. In addition, we identified reviews included in Cochrane reviews (http://community.cochrane.org/cochrane-reviews) and published review articles and reviewed their references [8,10]. A total of 510 articles were identified in the PubMed bibliographic search; 71 articles were identified in the CINAHL bibliographic search (Figure 1). After screening the abstracts or full texts of these articles, 15 eligible studies of the acceptability or efficacy of smartphone apps for increasing physical activity were identified.
Figure 1.
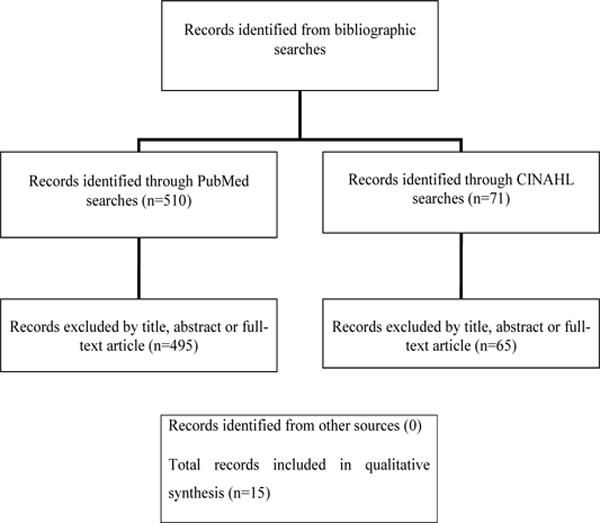
Summary of search and exclusion process: (smartphones) and ((physical activity) or (weight loss) or (weight gain) or (body weight) or (exercise weight) or (weight management).
Of the 15 included studies, 6 were qualitative research studies, 8 were randomized control trials, and one was a nonrandomized study with a pre-post design. Information was obtained from each published article about characteristics of the study population, outcomes of interest, and findings including effect measures. Information was also obtained about the operating system, platform, device, manufacturer, and app version.
The present review extends the work of earlier authors by including studies published in the last few years and by summarizing the results of both qualitative studies and randomized controlled trials [8, 10].
Results
Published studies included qualitative research studies (e.g., focus groups) and quantitative studies (e.g., randomized control trials) of the effectiveness of smartphone apps to increase physical activity (Table 1).
Table 1.
Qualitative Studies and Randomized Controlled Trials of Smartphone Applications for Promoting Physical Activity.
| Study | Sample | Design | Results | Limitations |
|---|---|---|---|---|
| Casey et al. [11] | 12 participants (mean age 42 yrs, 75% female) in 3 primary care centers in Ireland | Semi-structured interviews | Four themes emerged from the analysis: transforming relationships with exercise, persuasive technology tools, usability, and the cascade effect. The app appeared to facilitate a sequential and synergistic process of positive change, which occurred in the relationship between the participants and their exercise behavior. | Non-randomized design, small sample size |
| Rabin and Bock et al. [1] | 15 sedentary adults in Rhode Island | Formative study | The users have preferences with regard to physical activity app features related to physical activity, including provision of automatic tracking of physical activity (e.g., steps taken and calories burned), tracking of progress toward physical activity goals, and integrating a music feature. Participants also preferred that apps be flexible enough to be used with several types of physical activity and have user-friendly interfaces. | Non-randomized design, small sample size |
| Middelweerd et al. [7] | 30 Dutch students aged 18–25 yrs | Focus groups | Participants most often used social networking apps (e.g., Facebook or Twitter), communication apps (e.g., WhatsApp), and content apps (e.g., news reports or weather forecasts). They preferred a simple and structured layout and a companion website for detailed information about their accomplishments and progress. They preferred apps that coached and motivated them and provided tailored feedback toward personally set goals. | Non-randomized design |
| Vandelanotte et al. [12] | 30 middle-aged men in Queensland, Australia | Focus groups | The men supported the use of the Internet to improve and self-monitor physical activity and dietary behaviors provided the interventions were quick and easy to use. Participants preferred smartphones over regular mobile phones. | Non-randomized design |
| Morrison et al. [13] | 13 adults (6 male, 7 female, median age 27 yrs) in Southampton, United Kingdom | Telephone interviews. The participants had an Android smartphone | Access to the app was associated with an increase in participants’ awareness of their physical activity goals (P=0.03). Participants used the POWeR website for similar amounts of time during the weeks when POWeR Tracker was (mean 29 minutes, SD 31 minutes) and was not available (mean 27 minutes, SD 33 minutes). | Non-randomized design, small sample size |
| Kirwan et al. [14] | 12 Australian adults (90% white, 10% Asian), of whom 6 were women (mean female, 49% African-American) in Baltimore, MD who used an iPhone or Android smartphone | Qualitative and quantitative study with premodification testing to identify usability intensive counseling intervention, 2) intensive counseling plus smartphone intervention, 3) a less intensive counseling plus smartphone intervention, and 4) smartphone intervention only. The outcome measures included weight, body mass index (BMI), waist circumference, and self-reported physical activity and dietary intake | Four usability themes emerged from the data related to design, feedback, navigation, and terminology. Design improvements to the app resulted in a reduction in the problems experienced and a monitoring smartphone group tended to lose more weight than other groups (5.4 kg and 3.3 kg, respectively). Of those who completed the 6-month follow-up, 64% of participants in the intensive counseling plus self-monitoring smartphone group and 40% in the less intensive counseling plus self-monitoring smartphone group achieved greater than or equal to 5% decrease in their body weight. In contrast, only 25% in the counseling only group and 20% in the self-monitoring smartphone only group achieved at least a 5% weight loss. Females were more likely to lose weight compared to males (P = 0.005). | Non-randomized design, small sample size |
| Carter et al. [18] | 128 overweight volunteers (77% female, 91% white, mean age 42 yrs) in Leeds, United Kingdom | 6-month randomized controlled trial (pilot study) comparing smartphone app, website intervention, and paper diaries. The outcome measures were change in weight, body mass index, and body fat. The smartphone app uses an Android system. | Mean weight change at 6 months was −4.6 kg (95% CI −6.2 to −3.0) in the smartphone app group, −2.9 kg (95% CI −4.7 to −1.1) in the diary group, and −1.3 kg (95% CI −2.7 to 0.1) in the website group. Change in BMI at 6 months was −1.6 kg/m2 (95% CI −2.2 to −1.1) in the smartphone group, −1.0 kg/m2 (95% CI −1.6 to −0.4) in the diary group, and −0.5 kg/m2 (95% CI −0.9 to 0.0) in the website group. Change in body fat was −1.3% (95% CI −1.7 to −0.8) in the smartphone group, −0.9% (95% CI −1.5 to −0.4) in the diary group, and −0.5% (95% CI −0.9 to 0.0) in the website group [18]. | |
| Duncan et al. [19] | 301 adult men in Queensland, Australia ages 35 to 54 yrs | 9-month randomized trial comparing mobile phone-based intervention to print-based intervention. The outcome measures were total minutes of physical activity and total sessions of physical activity | Participants reported an increased number of minutes and sessions of physical activity at 3 months (exp(β)=1.45, 95% CI 1.09–1.95; exp(β)=1.61, 95% CI 1.17–2.22) and 9 months (exp(β)=1.55, 95% CI 1.14–2.10; exp(β)=1.51, 95% CI 1.15–2.00). The participants in the IT-based arm were less likely to report that 30 minutes of physical activity per day improves health (exp(β)=0.48, 95% CI 0.26–0.90) and more likely to report that vigorous intensity physical activity 3 times per week is essential (exp(β)=1.70, 95% CI 1.02–2.82). | |
| Turner-McGrievay and Tate [20] | 96 overweight adults (75% women, 20% African American, ages 25 to 45 yrs) in Raleigh-Durham, NC | Randomized trial comparing a combination of podcasting, mobile support communication, and mobile diet monitoring. The outcome measures included number of days each participant monitored their weight and weight loss. The participants had an Internet-capable mobile devices: iPhone, iPod Touch, BlackBerry, or an Android-based phone. | Adjusting for randomized group and demographics, users of the physical activity app self-monitored exercise more frequently over the 6-month study (2.6±0.5 days/week) and reported greater intentional physical activity (196.4±45.9 kcal/day) than non-app users (1.2±0.5 days/week physical activity self-monitoring, p<0.01; 100.9±45.1 kcal/day intentional physical activity, p=0.02). At 6 months, users of the physical activity app also had a lower BMI (31.5±0.5 kg/m2) than non-users (32.5±0.5 kg/m2; p=0.02). | |
| Martin et al. [22] | 40 adults in Baton Rouge, LA (25 < BMI < 35 kg/m2, 82.5% female, mean age 44.4 yrs) | 12-week randomized controlled trial comparing smartphone app to health education control group. The outcome measure was weight loss 18 | Weight loss was significantly larger (P < 0.001) in the smartphone app group | Small sample size |
Qualitative Research Studies
Casey et al. [11] conducted a qualitative evaluation of patients’ experiences in using a smartphone app to increase physical activity, embedded within the SMART MOVE trial. The researchers taped and transcribed semi-structured interviews with 12 participants. Four themes emerged from the analysis: transforming relationships with exercise, persuasive technology tools, usability, and the cascade effect. The app appeared to facilitate a sequential and synergistic process of positive change, which occurred in the relationship between the participants and their exercise behavior. Challenges noted included increased battery consumption and adjusting to carrying the smartphone on their person. There was also evidence of a cascade effect involving the families and communities of participants.
To develop a smartphone physical activity app that is empirically and theoretically-based and incorporates user preferences, Rabin and Bock [1] conducted a formative study. They recruited 15 sedentary adults to test three currently available physical activity smartphone apps and provide qualitative and quantitative feedback. They found that users have preferences with regard to physical activity app features related to physical activity, including provision of automatic tracking of physical activity (e.g., steps taken and calories burned), tracking of progress toward physical activity goals, and integrating a music feature. Participants also preferred that apps be flexible enough to be used with several types of physical activity and have well-documented features and user-friendly interfaces such as a one-click main page.
Middelweerd et al. [7] conducted a qualitative study to explore Dutch students’ preferences regarding a physical activity app for smartphones. Thirty Dutch students aged 18–25 years used a physical activity app for three weeks and then attended one of 5 focus group discussions. The participants were primarily female (67%). A discussion guide covered seven main topics, including general app usage, usage and appreciation of the physical activity app, appreciation of and preferences for its features, and the sharing of physical activity accomplishments through social media. The discussions were audio- and video-recorded, transcribed, and evaluated by content analysis. Several themes emerged: app usage, technical aspects, physical activity assessment, coaching aspects, and sharing through social media. Participants most often used social networking apps (e.g., Facebook or Twitter), communication apps (e.g., WhatsApp), and content apps (e.g., news reports or weather forecasts). They preferred a simple and structured layout without unnecessary features. Ideally, the app should enable users to tailor it to their personal preferences by including the capacity to hide features. Participants preferred a companion website for detailed information about their accomplishments and progress, and they liked tracking their workout using GPS. They preferred physical activity apps that coached and motivated them and provided tailored feedback toward personally set goals. They favored apps that enabled competition with friends by ranking or earning rewards, but only if the reward system was transparent. They were not willing to share their regular physical activity accomplishments through social media unless they were exceptionally positive [7].
Vandelanotte et al. [12] conducted a qualitative study to examine the opinions and perceptions of middle-aged men in Australia regarding the use of Internet- and mobile phone-delivered interventions to improve physical activity and nutrition. The researchers conducted 6 focus groups (n = 30). The analyses identified 6 themes: (a) Internet experience, (b) website characteristics, (c) Web 2.0 applications, (d) website features, (e) self-monitoring, and (f) mobile phones as delivery methods. The men supported the use of the Internet to improve and self-monitor physical activity and dietary behaviors on the condition that the website-delivered interventions were quick and easy to use. Commitment levels to engage in online tasks were low. Participants also indicated that they were reluctant to use normal mobile phones to change health behaviors; smartphones were more acceptable.
Morrison et al. [13] used a mixed-methods design to examine individual variation in the impact of a weight management app (POWeR Tracker) on self-reported goal engagement (ie, motivation, self-efficacy, awareness, effort, achievement) when provided alongside a Web-based weight management intervention (POWeR), and participant usage and views of the weight management app. Thirteen adults were provided access to POWeR and were monitored over a 4-week period. Access to POWeR Tracker was provided in 2 alternate weeks. Participants’ self-reported goal engagement was recorded daily. Usage of POWeR and POWeR Tracker was automatically recorded for each participant. Telephone interviews were conducted and analyzed using thematic analysis to explore participants’ experiences using POWeR and POWeR Tracker. Access to POWeR Tracker was associated with an increase in participants’ awareness of their eating (P=0.04) and physical activity goals (P=0.03). The level of increase varied between individual participants. Participants used the POWeR website for similar amounts of time during the weeks when POWeR Tracker was (mean 29 minutes, SD 31 minutes) and was not available (mean 27 minutes, SD 33 minutes). The qualitative data indicated that nearly all participants agreed that it was more convenient to access information on-the-go via their mobile phones than with a computer [13].
Kirwan et al. [14] conducted a formative study of an iPhone app involving 12 Australian adults aged 18 years or older, of whom 8 were women. Data were collected using a usability questionnaire and semi-structured interviews. Four usability themes emerged from the data related to app design, feedback, navigation, and terminology. Design improvements to the app resulted in a reduction in the problems experienced and a decrease in the time take to complete tasks.
Randomized Controlled Trials
Although there have been studies of short message service (SMS) text message-based interventions and smartphone apps used as adjuncts to other treatments, few randomized controlled trials have been conducted of stand-alone smartphone apps for weight loss that focus primarily on self-monitoring of physical activity. In a randomized trial involving 40 participants (20 per group), Gasser et al. [15] compared the efficacy of a smart phone app to a Web-based application for tracking physical activity and diet. Over the 4 weeks of the trial, the smartphone group had a more regular usage pattern than the Web-based group. No significant differences in physical activity goals or nutrition goals were observed across groups [15]. In the SMART MOVE trial, Glynn et al. [16] evaluated the efficacy of a smartphone app to increase physical activity in an 8-week, open-label, randomized controlled trial in 3 primary care practices in rural Ireland. Android smartphone users >16 years of age were recruited. The participants were provided with similar physical activity goals and information on the benefits of exercise. The intervention group was provided with a smartphone app and detailed instructions on how to use it to achieve these goals. The primary outcome was change in physical activity, as measured by a daily step count between baseline and follow-up. Of 139 patients referred by their primary care provider or self-referred, 90 (65%) were randomized to the trial. Of these, 78 provided baseline data and 77 provided outcome data. After adjustment, there was evidence of a significant treatment effect (P = 0.009); the difference in mean improvement in daily step count from week 1 to week 8 inclusive was 1029 (95% confidence interval [CI] 214 to 1843) steps per day, indicating an intervention effect.
To evaluate the feasibility, acceptability, and efficacy of a behavioral intervention delivered by smartphone technology, Allen et al. [17] randomized 68 obese adults (average age 45 years; 78% female’ 49% African American) to receive one of four interventions for six months: 1) intensive counseling intervention, 2) intensive counseling plus smartphone intervention, 3) a less intensive counseling plus smartphone intervention, and 4) smartphone intervention only. The outcome measures of weight, body mass index (BMI), waist circumference, and self-reported physical activity and dietary intake were assessed at baseline [17]. Participants in the intensive counseling plus self-monitoring smartphone group and less intensive counseling plus self-monitoring smartphone group tended to lose more weight than other groups (5.4 kg and 3.3 kg, respectively).
Carter et al. [18] conducted a 6-month pilot study to examine the acceptability and feasibility of a self-monitoring weight management intervention delivered via a smartphone app, compared to a website and a paper diary. Overweight volunteers (n=128) were randomized to receive a weight management intervention delivered by smartphone app, website, or paper diary. The smartphone app (My Meal Mate), developed using an evidence-based behavioral approach, incorporated goal setting, self-monitoring of diet and activity, and feedback via weekly text messages. The website group used a commercially available slimming website from a company called Weight Loss Resources, who also provided the paper diaries. The comparison groups received a similar self-monitoring intervention as the smartphone app, but by different modes of delivery. Participants were recruited from large local employers by email, intranet, newsletters, and posters. The intervention and comparison groups were self-directed, with no ongoing human input from the research team. At baseline enrollment and at brief follow-up sessions at 6 weeks and 6 months, face-to-face interactions were used to take anthropometric measures and administer questionnaires. At 6-months, the retention rates during the trial were 40/43 (93%) in the smartphone group, 19/42 (55%) in the website group, and 20/43 (53%) in the diary group. Adherence was higher in the smartphone group with a mean of 92 days (SD 67) of dietary recording compared with 35 days (SD 44) in the website group and 29 days (SD 39) in the diary group (P<0.001). Self-monitoring declined over time in all groups. In an intention-to-treat analysis, mean weight change at 6 months was −4.6 kg (95% CI −6.2 to −3.0) in the smartphone app group, −2.9 kg (95% CI −4.7 to −1.1) in the diary group, and −1.3 kg (95% CI −2.7 to 0.1) in the website group. Change in BMI at 6 months was −1.6 kg/m2 (95% CI −2.2 to −1.1) in the smartphone group, −1.0 kg/m2 (95% CI −1.6 to −0.4) in the diary group, and −0.5 kg/m2 (95% CI −0.9 to 0.0) in the website group. Change in body fat was −1.3% (95% CI −1.7 to −0.8) in the smartphone group, −0.9% (95% CI −1.5 to −0.4) in the diary group, and −0.5% (95% CI −0.9 to 0.0) in the website group [18].
To promote physical activity and healthy eating in middle-aged men, Duncan et al. [19] conducted a randomized trial (the ManUP study) to examine the efficacy of a 9-month web- and mobile phone-based intervention compared to a print-based intervention. The participants, who were recruited offline (e.g., newspaper ads), were randomized into either an information technology (IT)-based or print-based intervention arm on a 2:1 basis in favor of the fully automated IT-based arm. The participants were adult males aged 35–54 years living in cities in Queensland, Australia, who could access the Internet, owned a mobile phone, and were able to increase their activity level. The intervention, ManUp, was based on social cognitive and self-regulation theories and designed to target males. Educational materials were provided, and self-monitoring of physical activity and nutrition behaviors was promoted. The intervention content was the same in both intervention arms, but the delivery mode differed. The participants’ physical activity, dietary behaviors, and health literacy were measured by online surveys at baseline, 3 months, and 9 months. A total of 301 participants completed baseline assessments, 205 in the IT-based arm and 96 in the print-based arm; 124 participants completed all 3 assessments. There were no significant between-group differences in physical activity and dietary behaviors (P≥0.05). Participants reported an increased number of minutes and sessions of physical activity at 3 months (exp(β)=1.45, 95% CI 1.09–1.95; exp(β)=1.61, 95% CI 1.17–2.22) and 9 months (exp(β)=1.55, 95% CI 1.14–2.10; exp(β)=1.51, 95% CI 1.15–2.00). Overall dietary behaviors improved at 3 months (exp(β)=1.07, 95% CI 1.03–1.11) and 9 months (exp(β)=1.10, 95% CI 1.05–1.13). The proportion of participants in both groups eating high-fiber bread and low-fat milk increased at 3 months (exp(β)=2.25, 95% CI 1.29–3.92; exp(β)=1.65, 95% CI 1.07–2.55). The participants in the IT-based arm were less likely to report that 30 minutes of physical activity per day improves health (exp(β)=0.48, 95% CI 0.26–0.90) and more likely to report that vigorous intensity physical activity 3 times per week is essential (exp(β)=1.70, 95% CI 1.02–2.82). The researchers concluded that the ManUp intervention was effective in improving physical activity and dietary behaviors with no significant differences between IT- and print-based delivery modes [19].
With the Mobile Pounds Off Digitally (Mobile POD) randomized weight-loss intervention. Turner-McGrievy and Tate [20] examined whether a combination of podcasting, mobile support communication, and mobile diet monitoring can assist adults in losing weight. In this 6-month, minimal contact intervention, overweight adults (n=96) were recruited through television advertisements and email list serves and randomly assigned to Podcast-only or Podcast+Mobile groups. Both groups received 2 podcasts per week for 3 months and 2 minipodcasts per week for months 3–6. In addition to the podcasts, the Podcast+Mobile group was also instructed to use a diet and physical activity monitoring app on their mobile device and to interact with study counselors and other participants on Twitter. At 6 months, weight loss did not differ between the two groups at 6 months: mean −2.7% (SD 5.6%) Podcast+Mobile, n = 47; mean −2.7% (SD 5.1%) Podcast, n = 49; P = 0.98. Podcast+Mobile participants were 3.5 times more likely than the Podcast group to use an app to monitor diet (P = 0.01), whereas most Podcast participants reported using the Web (14/41, 34%) or paper (12/41, 29%). The number of Podcast participants reporting downloading over the 6-month period was significantly moderately correlated with weight loss in both the Podcast+Mobile (r = −0.46, P = 0.001) and the Podcast (r = −0.53, P < 0.001) groups. More Podcast participants relied on friends (11/40, 28% vs 4/40, 10%; P = 0.045) whereas Podcast+Mobile participants relied on online sources (10/40, 25% vs 0/40; P = 0.001).
Turner-McGrievey et al. [21] conducted a post hoc analysis of data from the Mobile POD trial to assess the relationship between diet (mobile app, website, or paper journal) and physical activity (mobile app vs no mobile app) self-monitoring and dietary and physical activity behaviors. The participants in both randomized groups were collapsed and categorized by their chosen self-monitoring method for diet and physical activity. All participants received a behavioral weight loss intervention delivered via podcast and were encouraged to self-monitor dietary intake and physical activity. Adjusting for randomized group and demographics, users of the physical activity app self-monitored exercise more frequently over the 6-month study (2.6±0.5 days/week) and reported greater intentional physical activity (196.4±45.9 kcal/day) than non-app users (1.2±0.5 days/week physical activity self-monitoring, p<0.01; 100.9±45.1 kcal/day intentional physical activity, p=0.02). At 6 months, users of the physical activity app also had a lower BMI (31.5±0.5 kg/m2) than non-users (32.5±0.5 kg/m2; p=0.02). Frequency of self-monitoring did not differ by diet self-monitoring method (p=0.63); however, at 6 months, app users consumed less energy (1437±188 kcal/day) than paper journal users (2049±175 kcal/day; p=0.01).
Martin et al. [22] enrolled 40 obese adults in a 12-week randomized controlled trial comparing smartphone app to health education control group. The outcome measure was weight loss. Weight loss was significantly larger (P < 0.001) in the smartphone app group.
Non-randomized study results have also been reported. Fukuoka et al. [23] assessed the efficacy of a pedometer and app-based diary intervention on sedentary lifestyle using a pre-post design. Forty-two women were enrolled in the study. At baseline, the participants received educational information about the benefits of physical activity and entered daily step counts and physical activity frequency, intensity, and duration into an app diary. There was a 20% increase in steps was observed over the course of the two week intervention [23].
Discussion
The results of this review indicate that smartphone apps can be efficacious in promoting physical activity although the number of randomized controlled trials of the efficacy of smartphone apps in increasing physical activity is still modest. In addition, the magnitude of the intervention effect (e.g., increase in steps taken or decrease in BMI) is modest. Qualitative results show that participants of various ages and gender respond favorably to physical activity apps that automatically track physical activity (e.g., steps taken), track progress toward physical activity goals, and are user-friendly and flexible enough to be used with several types of activity [1,7,11]. Participants prefer apps that coach and motivate them and provide tailored feedback toward personally set goals. Smartphone apps are preferred over use of a computer.
The current review of the published literature on physical activity apps differs from the review by Bort-Roig et al. [8] which was based upon studies published through September 2013. Whereas Borg-Roig et al. included apps for elderly patients in special care, cardiac rehabilitation patients, type 2 diabetes, and psychological rehabilitation patients, we excluded studies of the use of apps for chronic illnesses other than obesity. The focus of our review is on smartphone apps potentially useful for health education in the general population rather than mHealth interventions for patients who are post-myocardial infarction, etc. The current review also differs substantially from systematic reviews of physical activity apps identified through online stores that sell apps [4,25, 26]. Middelweerd et al. [25] identified apps for promoting physical activity by searching the iTunes and Google Play stores. The search terms used were based on Boolean logic and included AND combinations for physical activity, healthy lifestyle, exercise, fitness, coach, assistant, motivation, and support. The authors downloaded, reviewed, and rated 64 apps based on the taxonomy of behavior change techniques used in the interventions. Means and ranges were calculated for the number of observed behavior change techniques. On average, the apps included 5 behavior change techniques (range 2–8). Techniques such as self-monitoring, providing feedback on performance, and goal-setting were used frequently, whereas techniques such as motivational interviewing, stress management, relapse prevention, and use of role models were not. No differences were found in the number of behavior change techniques between free and paid apps, or between the app stores [25].
Bender et al. [4] examined the purpose and content of cancer-related smartphone apps available for use by the general public and the evidence for their utility and effectiveness. They systematically reviewed the official stores for the four major smartphone platforms (iPhone, Android, Nokia, and BlackBerry). Apps were included in their review if they were focused on cancer and were available for public use. Many of the apps promoted a charitable organization or supported fundraising efforts. The authors noted several concerns including the lack of evidence of app effectiveness or description of the procedures or data sources (e.g., evidence, theory) and discrepancies between information generated on smartphone apps and evidence-based guidelines.
With respect to limitations of the current review, there was only one reviewer and no rating scale was used to evaluate the quality of published studies. In addition, some published studies may have been overlooked if they were not included in PubMed or CINAHL. To address this issue, the references of previously published reviews were also reviewed.
Future studies should utilize randomized controlled trial research designs, larger sample sizes, and longer study periods to explore the physical activity measurement and intervention capabilities of smartphones [6, 26,27]. There is a need for culturally appropriate, tailored health messages to increase knowledge and awareness of health behaviors such as physical activity. Health promotion messages that are culturally tailored for a group address the unique needs of individuals, increase their motivation, tend to be perceived as more personally relevant, and lead to a greater likelihood of behavior change.
Acknowledgments
Funding Source
This work is funded by the National Cancer Institute (R01CA166785).
References
- 1.Rabin C, Bock B. Desired features of smartphone applications’ promoting physical activity. Telemed J E Health. 2011;17(10):801–803. doi: 10.1089/tmj.2011.0055. [DOI] [PubMed] [Google Scholar]
- 2.Vansaun MN. Molecular pathways: adiponectin and leptin signaling in cancer. Clin Cancer Res. 2013;19(8):1926–1932. doi: 10.1158/1078-0432.CCR-12-0930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thompson HJ, Sedlacek SM, Paul D, Wolfe P, McGinley JN, et al. Effect of dietary patterns differing in carbohydrate and fat content on blood lipid and glucose profiles based on weight-loss success of breast cancer survivors. Breast Cancer Res. 2012;14(1):R1. doi: 10.1186/bcr3082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bender JL, Yue RY, To MJ, Deacken L, Jadad AR. A lot of action, but not in the right direction: systematic review and content analysis of smartphone applications for the prevention, detection, and management of cancer. J Med Internet Res. 2013;15(12):e287. doi: 10.2196/jmir.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fox S. Pew Internet and American Life Project. Washington, DC: Pew Internet and American Life Project; 2012. [Google Scholar]
- 6.Conroy DE, Yang CH, Maher JP. Behavior change techniques in top-ranked mobile apps for physical activity. Am J Prev Med. 2014;46(6):649–652. doi: 10.1016/j.amepre.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 7.Middelweerd A, van der Laan DM, van Stralen MM, Mollee JS, Stuij M, et al. What features do Dutch university students prefer in a smartphone application for promotion of physical activity? A qualitative approach. Int J Behav Nutr Phys Act. 2015;12:31. doi: 10.1186/s12966-015-0189-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bort-Roig J, Gilson ND, Puig-Ribera A, Contreras RS, Trost SG, et al. Measuring and influencing physical activity with smarphone technology: a systematic review. Sports Med. 2014;44(5):671–86. doi: 10.1007/s40279-014-0142-5. [DOI] [PubMed] [Google Scholar]
- 9.Wearing JR, Nollen N, Befort C, Davis AM, Agemy CK, et al. iPhone app adherence to expert-recommended guidelines for pediatric obesity prevention. Child Obes. 2014;10(2):132–144. doi: 10.1089/chi.2013.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs. 2013;28(4):320–329. doi: 10.1097/JCN.0b013e318250a3e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Casey M, Hayes PS, Glynn F, OLaighin G, Heaney D, et al. Patients’ experiences of using a smartphone application to increase physical activity: the SMART MOVE qualitative study in primary care. Br J Gen Pract. 2014;64(625):e500–8. doi: 10.3399/bjgp14X680989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vandelanotte C, Caperchione CM, Ellison M, George ES, Maeder A, et al. What kinds of website and mobile phone-delivered physical activity and nutrition interventions do middle-aged men want? J Health Commun. 2013;18(9):1070–1083. doi: 10.1080/10810730.2013.768731. [DOI] [PubMed] [Google Scholar]
- 13.Morrison LG, Hargood C, Lin SX, Dennison L, Joseph J, et al. Understanding usage of a hybrid website and smartphone app for weight management: a mixed-methods study. J Med Internet Res. 2014;16(10):e201. doi: 10.2196/jmir.3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kirwan M, Duncan MJ, Vandelanotte C, Mummery KW. Design, development, and formative evaluation of a smartphone application for recording and monitoring physical activity levels: the 10,000 Steps “iStepLog”. Health Educ Behav. 2012;40(2):140–151. doi: 10.1177/1090198112449460. [DOI] [PubMed] [Google Scholar]
- 15.Gasser R, Brodbeck D, Degen M, Luthiger Jürg, Wyss Remo, et al. Persuasiveness of a mobile lifestyle coaching application using social facilitation. Lecture Notes Comput Sci. 2006;3692:27–38. [Google Scholar]
- 16.Glynn LG, Hayes PS, Casey M, Glynn F, Alvarez-Iglesias A, et al. Effectiveness of a smartphone application to promote physical activity in primary care: the SMART MOVE randomized controlled trial. Br J Gen Pract. 2014;64(624):e384–91. doi: 10.3399/bjgp14X680461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allen JK, Stephens J, Dennison Himmelfarb CR, Stewart KJ, Hauck S, et al. Randomized controlled pilot study testing use of smartphone technology for obesity treatment. J Obes. 2013;2013:151597. doi: 10.1155/2013/151597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carter MC, Burley VJ, Nykjaer C, Cade JE. Adherence to a smartphone application for weight loss compared to website and paper diary: pilot randomized controlled trial. J Med Internet Res. 2013;15(4):e32. doi: 10.2196/jmir.2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duncan M, Vandelanotte C, Kolt GS, Rosenkranz RR, Caperchione CM, et al. Effectiveness of a web- and mobile phone-based intervention to promote physical activity and healthy eating in middle-aged males: randomized controlled trial of the ManUp study. J Med Internet Res. 2014;16(6):e136. doi: 10.2196/jmir.3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turner-McGrievy G, Tate D. Tweets, apps, and pods: results of the 6-month Mobile Pounds off Digitally (Mobile POD) randomized weight-loss intervention among adults. J Med Internet Res. 2011;13:e120. doi: 10.2196/jmir.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turner-McGrievy GM, Beets MW, Moore JB, Kaczynski AT, Barr-Anderson DJ, et al. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J Am Med Inform Assoc. 2013;20(3):513–518. doi: 10.1136/amiajnl-2012-001510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin CK, Miller AC, Thomas DM, Champagne CM, Han H, et al. Efficacy of Smart Loss, a smartphone-based weight loss intervention: results from a randomized controlled trial. Obesity (Silver Spring) 2015;23(5):935–942. doi: 10.1002/oby.21063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fukuoka Y, Vittingh off E, Jong SS, Haskell William. Innovation to motivation: pilot study of a mobile phone intervention to increase sedentary behavior among sedentary women. Prev Med. 2010;51(3–4):287–289. doi: 10.1016/j.ypmed.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kirwan M, Duncan MJ, Vandelanotte C, Mummery WK. Using smartphone technology to monitor physical activity in the 10,000 steps program: a matched case-control trial. J Med Internet Res. 2012;14(2) doi: 10.2196/jmir.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Middelweerd A, Mollee JS, van der Wal CN, Brug J, Te Velde SJ, et al. Apps to promote physical activity among adults: a review and content analysis. Int J Behav Nutr Phys Act. 2014;11:97. doi: 10.1186/s12966-014-0097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Knight E, Stuckey MI, Prapavessis H, Petrella RJ. Public health guidelines for physical activity: is there an app for that?A review of android and apple app stores. JMIR Mhealth Uhealth. 2015;3(2):e43. doi: 10.2196/mhealth.4003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glynn LG, Hayes PS, Casey M, Glynn F, Alvarez-Iglesias A, et al. SMART MOVE—a smartphone-based intervention to promote physical activity in primary care: study protocol for a randomized controlled trial. Trials. 2013;29:157. doi: 10.1186/1745-6215-14-157. [DOI] [PMC free article] [PubMed] [Google Scholar]


