Abstract
Acetabular intraosseous cysts are frequently encountered in patients with dysplasia or femoroacetabular impingement. Small cysts are typically addressed by removing the cyst lining and stimulating healing via microfracture or abrasion chondroplasty. In contrast, larger cysts involving 1-3 cm3 frequently require additional fortification with bone graft material to facilitate osseous ingrowth and cyst healing. Previous arthroscopic reports have described the use of rim trimming to access the extra-articular side of the cyst, with subsequent use of straight metal cannulas for delivery of bone graft material. The downsides of this technique include the requirement for rim trimming, which may be ill advised in patients with normal coverage or dysplasia, as well as the creation of a second breach in the cyst wall, precluding pressurization of the bone graft material. We describe an arthroscopic technique using a curved delivery device allowing for deeper penetration into the cyst cavity through the articular side and greater delivery of bone graft material.
Acetabular intraosseous cysts are frequently encountered in patients with femoroacetabular impingement (FAI) and dyslasia.1 With few exceptions,2, 3 most of cysts are considered pathologic and a source of pain warranting treatment at the time of surgery.1, 4, 5 The prevailing approach for smaller cysts (< 1 cm3) entails evacuating the cystic contents, removing the lining, and stimulating osseous healing via abrasion chondroplasty or microfracture.4, 5 Larger cysts (> 1 cm3) have been addressed exclusively with “outside-in” drilling using open4 and arthroscopic techniques,5 necessitating the creation of a second, extra-articular, breach into the cyst contents.
To address the aforementioned shortcomings, we present an arthroscopic technique using a curved delivery device allowing for deeper and more precise penetration into the cyst cavity through the articular side and greater delivery of bone graft material.
Surgical Technique
Preoperative and Intraoperative Evaluation
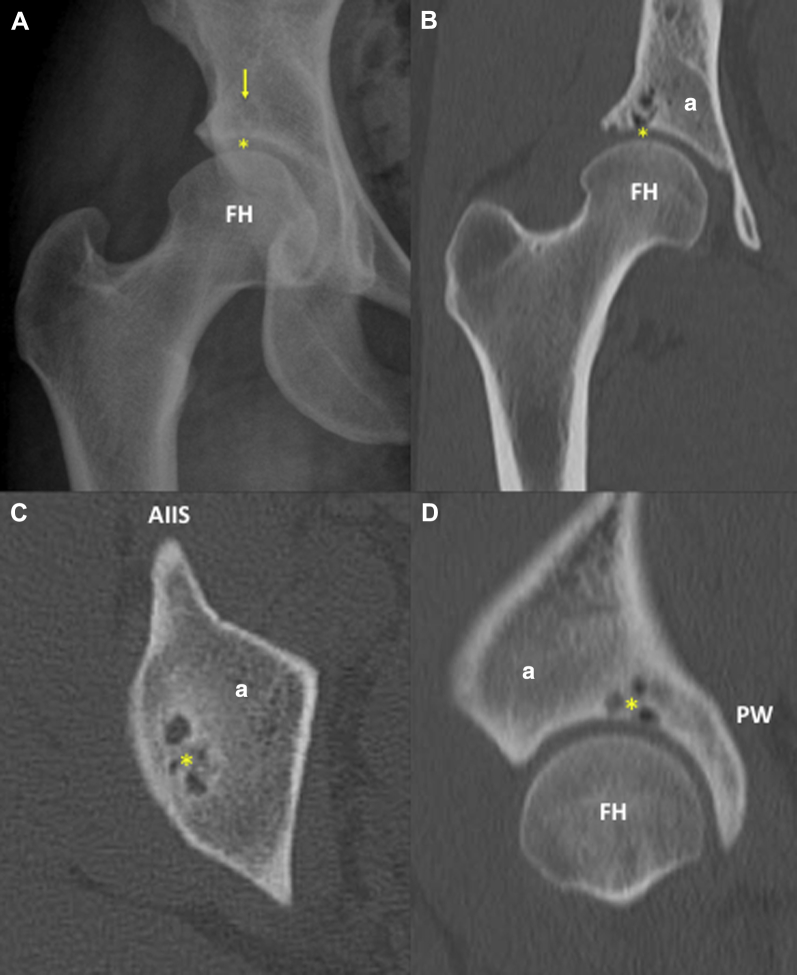
Preoperative evaluation of the painful hip includes a thorough history, physical examination, and radiographic studies aiming to identify underlying impingement and/or instability characteristics (Fig 1A). Acetabular intraosseous cysts may be identified on contrast and noncontrast MRI and should be evaluated for size, consistency, and location. A computed tomography scan provides greater bony detail to allow for more accurate sizing and localization of the cyst and because of its higher resolution may reveal the intra-articular breach (Fig 1 B-D). In dysplastic patients, these cysts may be assumed to communicate directly with the joint space,1 even if an intra-articular breach is not clearly visible. Heterogeneous cysts in atypical locations should be evaluated for malignancy by an orthopaedic oncologist. Incidental and benign appearing (non mechanical) cysts in asymptomatic hips are observed with close follow-up.
Fig 1.
Preoperative radiographic studies. (A) AP radiograph of the right hip demonstrating a large acetabular bone cyst (yellow arrow) with articular communication (yellow asterisk). (B) Coronally reformatted computed tomography (CT) scan of the right hip demonstrating a loculated acetabular cyst with clear articular communication (yellow asterisk). (C) Axial CT scan of the right hip demonstrating an acetabular bone cyst with loculated appearance (yellow asterisk). (D) Sagitally reformatted CT scan of the right hip demonstrating a loculated acetabular bone cyst in the superior weight-bearing region (yellow asterisk). (a, acetabulum; AIIS, anterior inferior iliac spine; FH, femoral head; PW, posterior wall.)
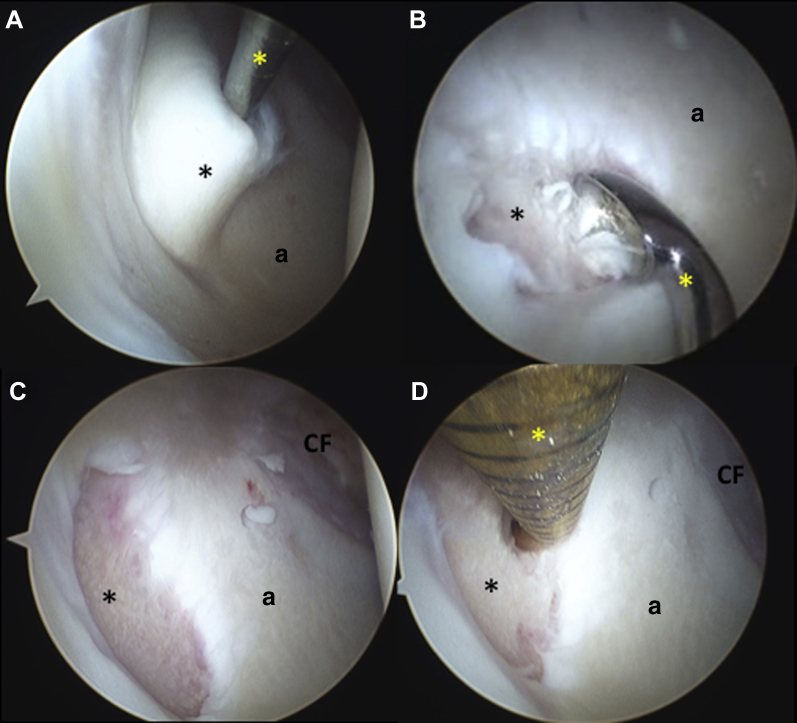
Hip arthroscopy is carried out in a standard fashion using a previously described technique.6 During central compartment evaluation, the area of the suspected intra-articular breach is inspected for change in color or texture, keeping in mind that most of such lesions are visually unimpressive and seemingly innocuous. The area is gently probed with a blunt instrument (Fig 2A) to reveal an unstable cartilage flap or wave delamination, signifying accurate localization of the intra-articular breach. FAI pathology is then addressed with labral repair, femoral osteoplasty, and rim trimming performed as indicated, before turning attention to the treatment of the cyst.
Fig 2.
Intraoperative arthroscopic images corresponding to the right hip in Figure 1. (A) Viewing through the mid-trochanteric portal with a 30° arthroscope, the full-thickness articular cartilage flap (black asterisk) is gently elevated with a probe (yellow asterisk) inserted through the mid-anterior portal. The articular cartilage flap covers the underlying acetabular bone cyst. (B) Viewing through the mid-anterior portal with a 30° arthroscope, an angled curette (yellow asterisk) is inserted through the mid-trochanteric portal to remove the calcified cartilage layer from the articular cartilage defect and to establish a stable rim. The articular communication of the cystic contents (black asterisk) is seen adjacent to the curette. (C) Viewing through the mid-trochanteric portal with a 30° arthroscope, the well-contained articular cartilage defect is seen (black asterisk) after removal of the overlying full-thickness cartilage flap. (D) Viewing through the mid-trochanteric portal with a 30° arthroscope, an angled microfracture awl (yellow asterisk) is inserted through the mid-anterior portal to gently probe and excavate the mucinous contents from the cystic cavity, adjacent to the articular cartilage defect (black asterisk). (a, acetabulum; CF, cotyloid fossa.)
Cyst Decompression and Bone Grafting
The damaged cartilage is sharply excised using angled curettes (Bruns Bone Curette Angled #1, Sklar Instruments, West Chester, PA) and shavers (Fig 2 B and C), and the underlying articular breach is exposed with an appropriately angled microfracture awl (XL Microfracture Awl, Smith & Nephew, Andover, MA) (Fig 2D, Video 1). Mucinous cystic contents may be seen draining from the cyst cavity during this step (Video 1). A curved arthroscopic shaver (4.5 mm 30° angled double-bite, Stryker, Kalamazoo, MI) is then inserted through either the mid-trochanteric portal or the mid-anterior portal, and bluntly introduced into the opening of the cyst cavity to completely evacuate the contents. The shaver, curette, and microfracture awl are used in an alternating fashion to prepare the defect for bone grafting. Care is taken to ensure that all soft tissue contents have been evacuated from the cyst cavity. Microfracture may be carried out in the remainder of the bony defect to stimulate healing adjacent to the cystic breach. We recommend the additional use of a fluted drill for more accurate placement of microfracture holes into the cystic cavity (Micro FX, Stryker). Fluoroscopy may be used to assess the depth and adequacy of device penetration into the cyst cavity.
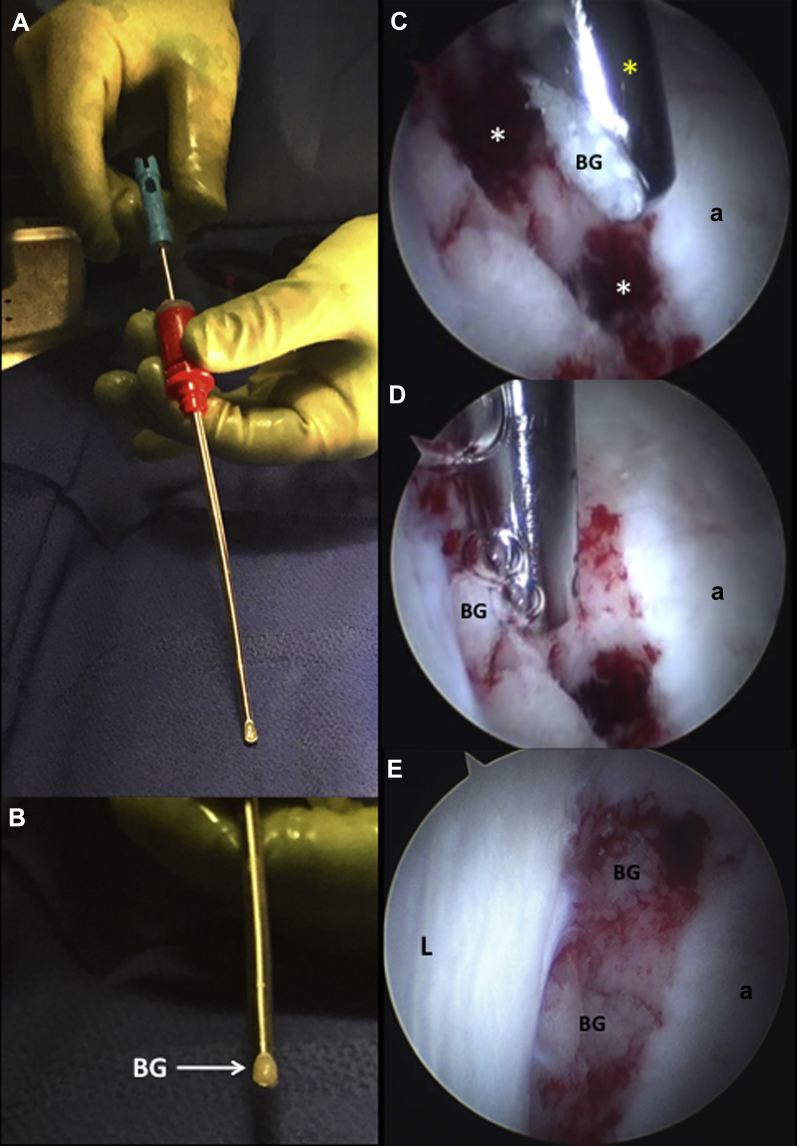
The arthroscopic shaver is then disassembled into an inner cutting sleeve, to be used as a plunger, and an outer sheath, to be used as the curved delivery device (Fig 3 A and B). This is accomplished by firmly applying manual pressure on the curved portion of the shaver against the sterile back table to slightly reduce the angle of curvature. This allows the inner sleeve to be removed with relative ease (Fig 3A). The outer sleeve is cleaned with a cotton swab and used as a curved cannula for delivery of bone graft material into the cyst (Fig 3 B-E). The bone graft of choice (DBX, Synthes, West Chester, PA) is loaded antegrade into the outer sleeve by using the inner sleeve and/or blunt switching stick as a plunger until the material is seen at the aperture on the opposite end (Fig 3 B and C). The plunger is gently depressed while the surgeon occludes the aperture with his thumb, to pack the bone graft within the sheath, before introducing the sheath into the joint. The outer sheath may then be manipulated against the back table to the desired degree of curvature before inserting into the joint for bone graft application. A switching stick is used to assess the best portal for optimal trajectory to the cyst. A slotted cannula is then inserted over the switching stick, which is replaced by the curved shaver sleeve with bone graft inside. The aperture of the shaver sleeve is positioned at the opening of the cystic cavity, establishing a seal (Fig 3D). This is made possible by the “side opening” design of the sleeve, as compared with an “end opening” design of a typical cannula. The inner sleeve is used as a plunger to gently fill the cyst with bone graft. Turning the sheath 180° enables the surgeon to use its convex side to gently compact the bone graft. For larger cysts, the steps above are repeated to deliver more bone graft. After compacting the bone graft placed inside the cyst, excess graft is evacuated from the joint using a shaver placed away from the cyst region and traction is released. Table 1 outlines some important “technical pearls” for successful execution of this technique.
Fig 3.
Sheath disassembly and intraoperative arthroscopic images corresponding to the right hip in Figure 1. (A) The curved shaver is disassembled by applying pressure against the sterile back table until the angle of curvature is slightly reduced. This allows the inner sleeve (blue) to be removed from the outer sheath (red) with relative ease. (B) The outer sheath is loaded with bone graft (BG), and the inner sleeve is used as a plunger until the bone graft can be seen exiting the side-opening. The outer sheath may then be manipulated against the back table to the desired degree of curvature before inserting into the joint for bone graft application. (C) Viewing through the mid-trochanteric portal with a 30° arthroscope, a curved shaver sleeve (yellow asterisk) loaded with bone graft is inserted through the mid-anterior portal in preparation for bone grafting of the cystic cavities (white asterisks). (D) Viewing through the mid-trochanteric portal with a 30° arthroscope, a curved shaver sleeve (yellow asterisk) is placed with the side-opening of the shaver sleeve facing the cystic cavity to deliver the bone graft. Air bubbles are seen as the inner sleeve of the curved shaver is deployed as a plunger to deliver the bone graft and pressurize the cystic cavity. (E) Viewing through the mid-anterior portal with a 30° arthroscope, a well-positioned bone graft can be seen within the loculated cystic cavity in the well-contained articular cartilage defect. (a, acetabulum; L, labrum.)
Table 1.
Indications, Contraindications, and Technical Pearls for Inside Out Bone Grafting of Acetabular Intraosseous Cysts
| Indications |
| • Symptomatic hip instability or femoroacetabular impingement (FAI) with magnetic resonance imaging (MRI) and or computed tomography (CT) evidence of an acetabular intraosseous cyst |
| Contraindications |
| • Coxarthrosis (Tonnis grade 3 or 4)—Consider total hip arthroplasty |
| Technical pearls |
| • Use a blunt probe to gently expose the cyst by manipulating overlying delaminated articular cartilage |
| • Take time to completely excise the membranous cyst lining to prevent recurrence and failure of bony healing |
| • Use the portal that gives the best trajectory for delivering bone graft |
| • Perform grafting in stages and use multiple loads, if necessary, to adequately pressurize cyst |
| • Meticulously lavage and suction excess bone graft material from the joint |
| • Appropriately address all underlying pathomechanical contributors to cyst formation including femoroacetabular impingement and dysplasia |
| Potential risks |
| • Extravasation of bone graft material, possibly resulting in heterotopic ossification (HO) |
Postoperative Management
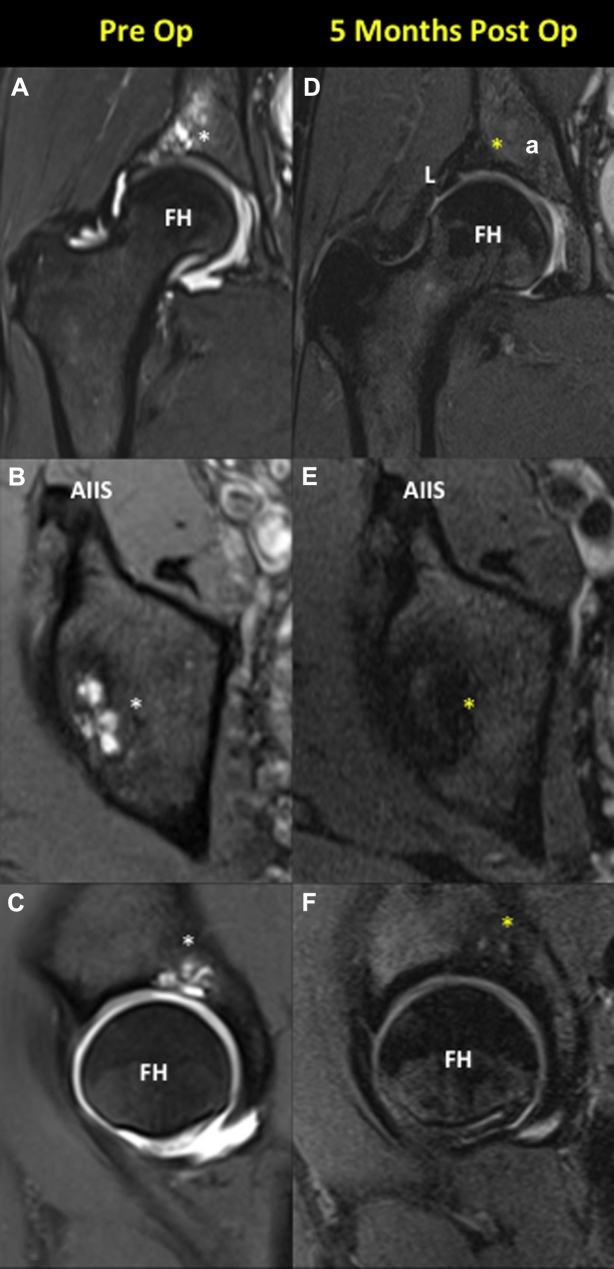
Postoperative precautions are predicated on the size and location of the cyst as well as any underlying dysplastic characteristics. We recommend limiting weight bearing to “toe-touch” for 4 to 6 weeks in patients with dysplasia or cysts > 1 cm3. Smaller cysts in patients with FAI may be treated with weight bearing as tolerated using crutches for stability for 2 weeks, provided that extensive microfracture was not performed. Standard hip arthroscopy rehabilitation is then commenced with return to play allowed 4 to 6 months postoperatively, depending on the duration of limited weight bearing and ability to regain muscle strength and control. Follow-up MRI may be obtained to ensure adequate cyst healing (Fig 4), especially if a staged realignment procedure, such as a periacetabular osteotomy, is planned.
Fig 4.
Pre- and postoperative magnetic resonance imaging (MRI) scans of the right hip, previously shown in Figure 1. (A) Preoperative coronal T2 MRI arthrogram demonstrating an acetabular bone cyst (white asterisk) in the superior weight-bearing portion. (B) Preoperative axial T2 MRI arthrogram demonstrating an acetabular bone cyst (white asterisk) with the loculated pattern. (C) Preoperative sagittal T2 MRI arthrogram demonstrating an acetabular bone cyst (white asterisk) with articular cartilage breach. (D) Postoperative coronal T2 MRI scan demonstrating complete cyst healing and remodeling (yellow asterisk) with excellent fibrocartilage fill of articular cartilage defect. (E) Postoperative axial T2 MRI scan demonstrating complete cyst healing and remodeling (yellow asterisk) with resolution of loculations. (F) Postoperative sagittal T2 MRI scan demonstrating complete cyst healing and remodeling (yellow asterisk) with excellent fibrocartilage fill of articular cartilage defect. (a, acetabulum; AIIS, anterior inferior iliac spine; FH, femoral head; L, labrum.)
Discussion
In this article, we present an “inside-out” technique for bone grafting acetabular intraosseous cysts, using a curved delivery device. Some important advantages of this technique include preservation of the extra-articular cyst wall for more effective cyst pressurization with bone graft as well as obviating the need for concomitant rim trimming to afford cyst access. Given that these cysts are frequently encountered in patients with dysplasia, avoiding rim trimming for cyst access is highly beneficial. Potential risks associated with this technique include extravasation of bone graft material, possibly resulting in heterotopic ossification.
The prevailing approach for smaller cysts (< 1 cm3) entails evacuating the cystic contents, removing the lining, and stimulating osseous healing via abrasion chondroplasty or microfracture.4, 5 Larger cysts (> 1 cm3) have been addressed exclusively with “outside-in” drilling using open4 and arthroscopic techniques,5 necessitating the creation of a second, extra-articular, breach into the cyst contents.
In the arthroscopic technique by Jamali et al.,5 this “outside-in” approach necessitates rim trimming to allow extra-articular access to the cyst contents, which may be ill advised in patients with normal coverage or dysplasia. Field et al.4 describe a technique using fluoroscopic guidance with a drill guide placed through the ilium. The position of the guide may be intrapelvic and extrapelvic depending on the location of the cyst and best trajectory for access. This technique carries the added morbidity of using a second incision and intrapelvic placement of the drill guide. In addition, the technique relies on image guidance for appropriate cyst localization rather than direct visualization, which may result in incomplete decompression and suboptimal placement of bone graft. In general, “outside-in” techniques provide indirect access for cyst lining removal and may result in persistent pain or cyst recurrence.
The curved delivery device described in this article is unique in that, with the use of appropriate portals, it allows direct access to all acetabular bone cysts. In addition, the limited side-opening of the sheath may be nicely apposed to the cyst introitus to create a seal for superior pressurization, concomitantly limiting extravasation of bone graft material into the joint cavity.
In summary, the “inside-out” technique described in this article may be universally applied to decompress and bone graft large (> 1 cm3) acetabular bone cysts. The technique allows for direct visualization of cyst decompression, preservation of the extra-articular cyst wall, and pressurization of bone graft.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
A 30° 2.7-mm arthroscope (ConMed Linvatec, Utica, NY) is inserted into the central compartment through the mid-trochanteric portal. A probe is placed through the mid-anterior portal and diagnostic arthroscopy of the central compartment is performed. The probe is used to gently elevate the area of chondromalacia overlying the acetabular bone cyst, which can be localized with preoperative computed tomography scanning. The area of the full-thickness flap is debrided with the use of basket forceps and a grasper to remove the flap. Residual flap debris may be evacuated with a curved arthroscopic shaver (4.5-mm angled double-bite, Stryker). The margins of the articular cartilage defect are sharply delineated with an angled curette (Bruns Bone Curette Angled #1, Sklar Instruments, West Chester, PA), which may also be used to remove the calcified cartilage layer. Viewing and working portals are interchanged to allow for complete access to all aspects of the defect. A microfracture awl (XL Microfracture Awl, Smith & Nephew, Andover, MA) may be used to gently breach, enlarge, and excavate the cystic contents before using the curved shaver to suction and further debride the cyst. The microfracture awl and probe may also be used to pry out any residual soft tissue cyst lining to ensure complete cyst decompression before bone grafting. The remainder of the defect may be microfractured with the use of a fluted drill (Micro FX, Stryker) to stimulate healing. The curved shaver is then disassembled by gently straightening the curved portion against the back table, removing the inner cutting sleeve, and the outer sheath is cleaned with a cotton swab. Bone graft material (DBX, Synthes) is loaded into the outer sheath in an antegrade fashion until seen at the sheath opening. The inner cutting sleeve is used as a plunger while occluding the opening to compact the bone graft material within the sheath before inserting the sheath into the joint. Alternatively, a switching stick or blunt instrument may be used as a plunger. The sheath may be re-bent against the back table to the desired angle and inserted through the mid-anterior portal to be positioned with the side-opening facing the cyst. Effort is made to obtain a seal against the cystic opening before depressing the inner sleeve as a plunger to deliver the bone graft. Air bubbles can be seen as the bone graft is delivered, and the sheath is periodically repositioned to assess the extent of fill. The sheath may be removed and reloaded as needed to completely fill all cystic defects. The residual bone graft is then removed with the curved shaver positioned away from the area of the cyst and traction is released. Femoral osteoplasty, labral repair, and any other indicated procedures are performed and capsular closure is carried out with the use of the SpeedStitch suture passer (ArthroCare, Austin, TX).
References
- 1.Inui A., Nakano S., Yoshioka S. Subchondral cysts in dysplastic osteoarthritic hips communicate with the joint space: Analysis using three-dimensional computed tomography. Eur J Orthop Surg Traumatol. 2013;23:791–795. doi: 10.1007/s00590-012-1082-0. [DOI] [PubMed] [Google Scholar]
- 2.Register B., Pennock A.T., Ho C.P., Strickland C.D., Lawand A., Philippon M.J. Prevalence of abnormal hip findings in asymptomatic participants: A prospective, blinded study. Am J Sports Med. 2012;40:2720–2724. doi: 10.1177/0363546512462124. [DOI] [PubMed] [Google Scholar]
- 3.Tzaveas A.P., Villar R.N. Cyst-like lesion of the acetabular roof—An abnormal finding or an anatomical variant? Hip Int. 2010;20:258–260. doi: 10.1177/112070001002000219. [DOI] [PubMed] [Google Scholar]
- 4.Field R.E., Rajakulendran K., Strambi F. Arthroscopic grafting of chondral defects and subchondral cysts of the acetabulum. Hip Int. 2011;21:479–486. doi: 10.5301/HIP.2011.8583. [DOI] [PubMed] [Google Scholar]
- 5.Jamali A.A., Fritz A.T., Reddy D., Meehan J.P. Minimally invasive bone grafting of cysts of the femoral head and acetabulum in femoroacetabular impingement: Arthroscopic technique and case presentation. Arthroscopy. 2010;26:279–285. doi: 10.1016/j.arthro.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 6.Mei-Dan O., McConkey M.O., Young D.A. Hip arthroscopy distraction without the use of a perineal post: Prospective study. Orthopedics. 2013;36:e1–e5. doi: 10.3928/01477447-20121217-10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A 30° 2.7-mm arthroscope (ConMed Linvatec, Utica, NY) is inserted into the central compartment through the mid-trochanteric portal. A probe is placed through the mid-anterior portal and diagnostic arthroscopy of the central compartment is performed. The probe is used to gently elevate the area of chondromalacia overlying the acetabular bone cyst, which can be localized with preoperative computed tomography scanning. The area of the full-thickness flap is debrided with the use of basket forceps and a grasper to remove the flap. Residual flap debris may be evacuated with a curved arthroscopic shaver (4.5-mm angled double-bite, Stryker). The margins of the articular cartilage defect are sharply delineated with an angled curette (Bruns Bone Curette Angled #1, Sklar Instruments, West Chester, PA), which may also be used to remove the calcified cartilage layer. Viewing and working portals are interchanged to allow for complete access to all aspects of the defect. A microfracture awl (XL Microfracture Awl, Smith & Nephew, Andover, MA) may be used to gently breach, enlarge, and excavate the cystic contents before using the curved shaver to suction and further debride the cyst. The microfracture awl and probe may also be used to pry out any residual soft tissue cyst lining to ensure complete cyst decompression before bone grafting. The remainder of the defect may be microfractured with the use of a fluted drill (Micro FX, Stryker) to stimulate healing. The curved shaver is then disassembled by gently straightening the curved portion against the back table, removing the inner cutting sleeve, and the outer sheath is cleaned with a cotton swab. Bone graft material (DBX, Synthes) is loaded into the outer sheath in an antegrade fashion until seen at the sheath opening. The inner cutting sleeve is used as a plunger while occluding the opening to compact the bone graft material within the sheath before inserting the sheath into the joint. Alternatively, a switching stick or blunt instrument may be used as a plunger. The sheath may be re-bent against the back table to the desired angle and inserted through the mid-anterior portal to be positioned with the side-opening facing the cyst. Effort is made to obtain a seal against the cystic opening before depressing the inner sleeve as a plunger to deliver the bone graft. Air bubbles can be seen as the bone graft is delivered, and the sheath is periodically repositioned to assess the extent of fill. The sheath may be removed and reloaded as needed to completely fill all cystic defects. The residual bone graft is then removed with the curved shaver positioned away from the area of the cyst and traction is released. Femoral osteoplasty, labral repair, and any other indicated procedures are performed and capsular closure is carried out with the use of the SpeedStitch suture passer (ArthroCare, Austin, TX).