Abstract
In recent years, arthroscopic and arthroscopically assisted techniques have been increasingly used to reconstruct the lateral ligaments of the ankle. Besides permitting the treatment of several comorbidities, arthroscopic techniques are envisioned to lower the amount of surgical aggression and to improve the assessment of anatomic structures. We describe our surgical technique for arthroscopic, two-portal ankle ligament repair using an all-soft knotless anchor, which is made exclusively of suture material. This technique avoids the need for classic knot-tying methods. Thus it diminishes the chance of knot migration caused by pendulum movements. Moreover, it avoids some complications that have been related to the use of metallic anchors and some currently available biomaterials. It also prevents prominent knots, which have been described as a possible cause of secondary complaints.
Ankle sprain is the most frequent injury during sports activity. About 20% of cases eventually require surgical treatment for ankle instability after nonoperative treatment failure.1 The Broström procedure, with its several modifications, has been considered the gold standard of surgical treatment for several years.1, 2
Arthroscopic techniques have recently been described aiming to lower the amount of surgical aggression and shorten the rehabilitation process (Table 1).3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 These techniques have been linked to the development of anchor and fixation devices that have facilitated arthroscopic-assisted ligament repair.14 From large-diameter (5.5-mm) metal-based anchors4 to smaller (2.9-mm) biomaterial-based anchors,3, 14 several options have been proposed. More recently, all-suture anchors have also been proposed as a reliable fixation method while permitting even smaller drill holes (1.4 or 2.1 mm).15 This is advantageous when one is perforating a small bone or predicting the eventual need for a revision procedure. Moreover, if an additional implant is required (e.g., failure of anchors placed earlier), using large-diameter and “hard” implants, surgeons would face greater concerns or difficulties than those expected with a smaller and all-soft device.
Table 1.
Systematic Review of Clinical Publications (Including Technical Notes) on Topic of Ankle Instability Arthroscopic Repair
| Type of Study | Notes | |
|---|---|---|
| Takao et al.,5 2015 | Technical note | Repair of the lateral ligament alone using a lasso-loop stitch, which intends to avoid additional tightening of the inferior extensor retinaculum |
| Lui,6 2015 | Technical note | Modified Broström-Gould procedure; bone tunnels and transosseous sutures |
| Guillo et al.,7 2014 | Technical note | Hamstring autograft required |
| Guillo et al.,8 2014 | Technical note | Hamstring autograft required |
| Matsui et al.,9 2014 | Technical note | Modified Broström-Gould procedure |
| Vega et al.,3 2013 | Case series (n = 16) | Modified Broström-Gould procedure; 2.9-mm knotless anchor made of PEEK |
| Cottom and Rigby,10 2013 | Case series (n = 40) | Modified Broström-Gould procedure; bioabsorbable bone anchor (no further details available) |
| Acevedo and Mangone,11 2011 | Case series (n = 23) | Modified Broström-Gould procedure; bioabsorbable bone anchor, PLDLA based |
| Kim et al.,12 2011 | Case series (n = 28) | Modified Broström-Gould procedure; bioabsorbable bone anchor, PLDLA based (no further details available) |
| Nery et al.,13 2011 | Case series (n = 40) | Modified Broström-Gould procedure; 5.0-mm titanium bone anchor; mean follow-up, 9.8 yr |
| Corte-Real and Moreira,4 2009 | Case series (n = 31) | Modified Broström-Gould procedure; 5.0-mm titanium bone anchor |
NOTE. An electronic search was performed using the keywords “arthroscopic,” “ankle ligaments,” “repair,” “surgery,” and “reconstruction” in PubMed and ScienceDirect from 2009 to July 2015. The reference lists of identified publications and journals' electronic databases were also checked for the same period. This period was chosen based on when the first clinical experience on arthroscopic-assisted lateral ankle ligament repair took place, in 2009.4
PEEK, polyether ether ketone; PLDLA, poly-L/D-lactide.
All-suture anchors might also avoid complications related to metal or so-called biomaterials.16, 17 These range from foreign-body reactions to cyst formation, migration, or chondrolysis.
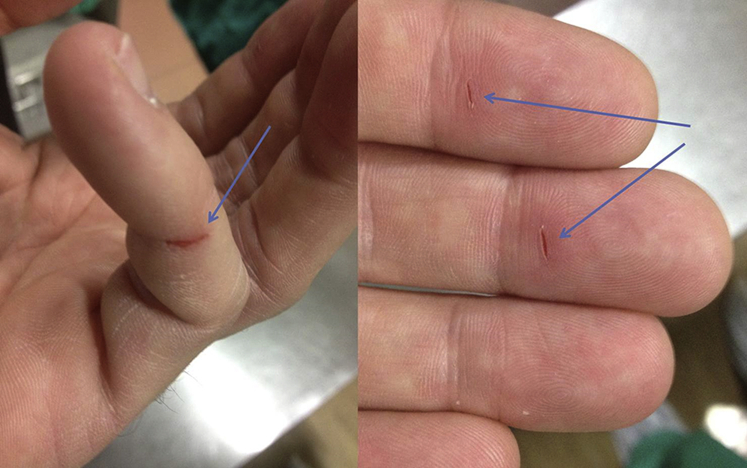
Over time, arthroscopy-related knot-tying techniques have been developed for use in shoulder procedures. These require consecutive training and have a somewhat demanding learning curve. Furthermore, such methods inherently have some risk of glove perforation and skin tears, which raises some safety concerns (Fig 1).18 In addition, movement-induced knot migrations have been described after repeated pendulum movements during knot tying.19 This phenomenon might cause changes in the direction and security of the knots.
Fig 1.
Skin tears caused by knot tying (arrows) after arthroscopic surgery.
For these reasons, we have decided to adjust our arthroscopic technique for lateral ankle ligament repair by adapting an implant recently developed primarily for shoulder surgery. This is an all-soft knotless anchor composed entirely of suture material: JuggerKnotless (Zimmer Biomet, Warsaw, IN). This technical note describes the surgical procedure step by step.
Surgical Technique
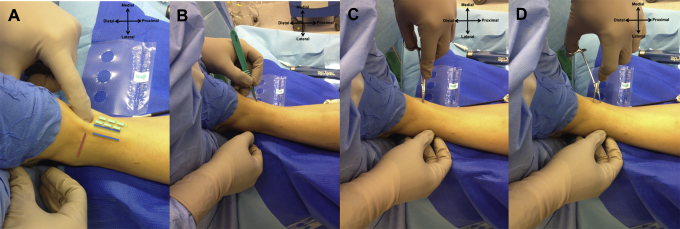
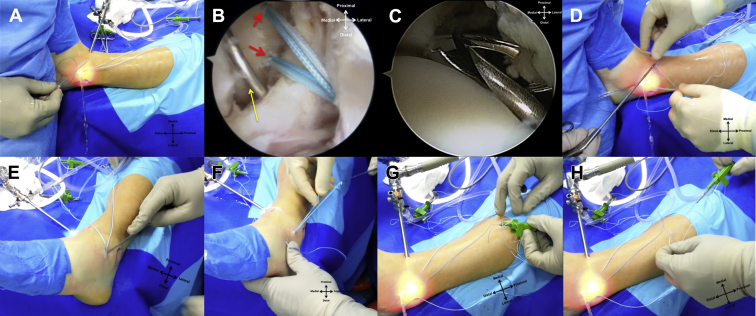
The patient is in the supine position with a pneumatic tourniquet around the thigh. A sandbag is placed under the ipsilateral buttock to rotate the hip internally (foot perpendicular to the ground) (Fig 2).
Fig 2.
Patient positioning showing left ankle surgery, with a sandbag under the ipsilateral buttock for internal rotation of the limb (A). Correct placement of the medial portal is a key to success. (B, C) The contour of the medial malleolus is drawn on the skin up to the joint line (yellow arrows). (B) In plantar flexion, the tibialis anterior tendon has a more medial position (entrapped between surgeon's fingers), whereas (C) in dorsiflexion, it slides to the center of the joint (between the red arrows).
Distraction should not be applied during this procedure.20 Distraction hinders inspection of the anterior talofibular ligament (ATFL) and fibula. It also diminishes the anterolateral working space.2 Lastly, distraction counteracts shortening of the ligaments.
The most important landmarks are the lateral malleolus (LM), medial malleolus, anterior joint line, and tibialis anterior tendon (TAT) (Fig 2, Fig 3). As shown in Video 1, the TAT is easily palpable. Its position is significantly more medial in plantar flexion compared with dorsiflexion (Fig 2, Fig 3). For this reason, a standard medial portal is made with the ankle in dorsiflexion, just medial to the TAT (as close as possible to the center of the joint).
Fig 3.
Creation of medial portal in a left ankle. (A) In dorsiflexion, at the level of the joint line (red line), a soft spot can be felt just medial to the tibialis anterior tendon (blue lines). Notice that in plantar flexion position the tendon is considerably more medial (dashed lines). The medial portal is created medial to the intersection of the tibialis anterior tendon and the joint line. (B) A surgical blade is used to cut the skin. (C, D) A mosquito clamp is used to bluntly dissect the soft tissue until reaching inside the joint. The ankle is kept in dorsiflexion at all times to open the anterior “working area,” diminish tension of the surrounding structures, and protect the joint cartilage.
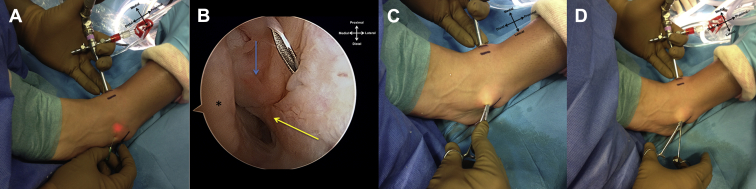
A 4.0-mm arthroscope is introduced through the medial portal, and serum inflow is provided by simple gravity. The joint is inspected and the ATFL identified (Fig 4), while the ankle is kept in dorsiflexion.21
Fig 4.
(A) As shown in a left ankle, a 22-gauge needle is used to assist in portal placement 1.0 to 1.5 cm anterior to the tip of the fibula while transillumination is used to protect the superficial peroneal nerve. (B) The tip of the lateral malleolus (blue arrow) and the remnant of the anterior talofibular ligament (yellow arrow) are identified. The talus is also visible (asterisk). (C, D) The surgical blade is used to cut the skin, and blunt dissection by a mosquito clamp is used to penetrate the joint, lowering the risk of iatrogenic injuries.
An accessory lateral portal (aLP) is created around 1.0 to 1.5 cm anterior to the tip of the fibula. It is recommended to achieve this with transillumination to protect the superficial peroneal nerve. A 22-gauge needle is used to assist in portal placement. In cases without comorbidities, this accessory portal can be used as a unique working portal (two-portal technique). If other concomitant procedures are required, we proceed as described elsewhere.20
The full course of the ATFL must be visible and accessible. The remnants of the ATFL are inspected, and a probe is used for palpation, tensioning, and judging the quality of the tissue (Fig 5). If the remnant is considered acceptable for the modified Broström-Gould procedure, the surgical procedure is completed as planned. If not, the procedure is interrupted and an alternative technique (which had previously been discussed with the patient) is performed.1, 8
Fig 5.
(A, B) Arthroscopic view of the lateral gutter of a left ankle through the anteromedial portal. The quality of the anterior talofibular ligament remnant (yellow arrows) must be inspected, and the contour of the tip of the medial malleolus (blue arrows) is identified. (C) A key to success is for the surgeon to prepare the tip of the lateral malleolus using a shaver blade until reaching bleeding bone before inserting the anchor (black arrow). (D) JuggerKnotless anchor (Zimmer Biomet) placement through the lateral portal. (E) Inside view of the anchor guide (the arthroscope is in the medial portal). (F) Introduction of the anchor. (G) Verification that both ends of the anchor are adequately sliding. (H) Confirmation of the pullout resistance of the anchor by raising the leg from the table while pulling through the anchor wires.
The surrounding tissue or synovitis can be removed, and the tip of the LM is prepared for anchor placement with a shaver or electrocoagulation device until bleeding bone is achieved. Both anchors are sequentially introduced through the aLP (Fig 5).
The surgeon places the first JuggerKnotless device more distally, aiming for the footprint of the ATFL. A blunt trocar is used inside a drill guide. The direction of the guide is placed with respect to the bone morphology of the LM and is usually directed anterior to posterior at approximately 45° to 60° of the longitudinal axis of the fibula and parallel to the plane of the lateral gutter. A 2.1-mm drill bit is used, creating a 17-mm-long tunnel (control is provided by a laser mark and safety stop). After tunnel creation, while the guide is maintained in the same position and direction, the anchor is introduced. The surgeon follows the course of the anchor using direct arthroscopic visualization. The anchor is fully introduced by gently tapping with a hammer until it reaches the safety stop. Once fully introduced, the guide is removed and both ends are pulled at the same time to ensure adequate fixation to bone. After this important step, the surgeon must ensure that both ends of the anchor are adequately sliding. With this device, a MaxBraid (polyethylene) suture (Zimmer Biomet) passes through a sleeve of braided polyester suture in a V-shaped configuration, which constitutes the anchoring mechanism to bone. Later, a second loop will also slide and finally lock the soft tissue in place by a similar mechanism.
The second anchor is placed around 5 mm more proximally and will be used to tension the inferior extensor retinaculum (IER). Each anchor has one solid-blue wire and a deployment device with a nitinol loop. Care should be taken to keep each solid-blue wire connected to its corresponding deployment device at all times.
An 18-gauge needle with a No. 3-0 nylon loop is introduced through the aLP and will serve as a suture passer (Fig 6). The needle will trespass the proximal half of the remnant of the ATFL from inferolateral to superomedial under direct arthroscopic visualization. Firm control of the needle with gentle progression is required to avoid iatrogenic articular damage.
Fig 6.
(A) An 18-gauge needle with a No. 3-0 nylon loop is introduced through the accessory lateral portal and serves as a suture passer. (B) Two anchors have been inserted in the lateral malleolus (red arrows). The needle (yellow arrow) trespasses the proximal half of the anterior talofibular ligament remnants. (C) A grasper is used to retrieve the nylon loop. (D) By use of the grasper, the nylon loop is retrieved outside the joint and the solid-blue wire from the first anchor is passed through. The nylon loop (including the solid-blue wire) is then pulled out through the skin. (E, F) Retrieval of the solid-blue wire through the accessory lateral portal with a hook probe. (G) The solid-blue wire of the anchor is passed through the nitinol loop of the deployment device of the anchor. (H) A second, blue-white loop is detached and slides over the solid-blue wire. Soft tissue is tensioned against the footprint by pulling the solid-blue wire. A small pull on the blue-white wire locks the mechanism.
By use of a grasper, the nylon loop is retrieved outside the joint by the aLP and the solid-blue wire from the first anchor is passed through. The nylon loop (including the first solid-blue wire) is subsequently pulled out through the skin. Blunt dissection of subcutaneous soft tissue is performed to avoid superficial peroneal nerve damage and to facilitate the soft-tissue sliding for later pants-over-vest IER reinforcement of the ATFL repair. The solid-blue wire is retrieved through the aLP with the hook probe (Video 1). This wire is connected to its corresponding deployment device by a mosquito clamp (to prevent confusion).
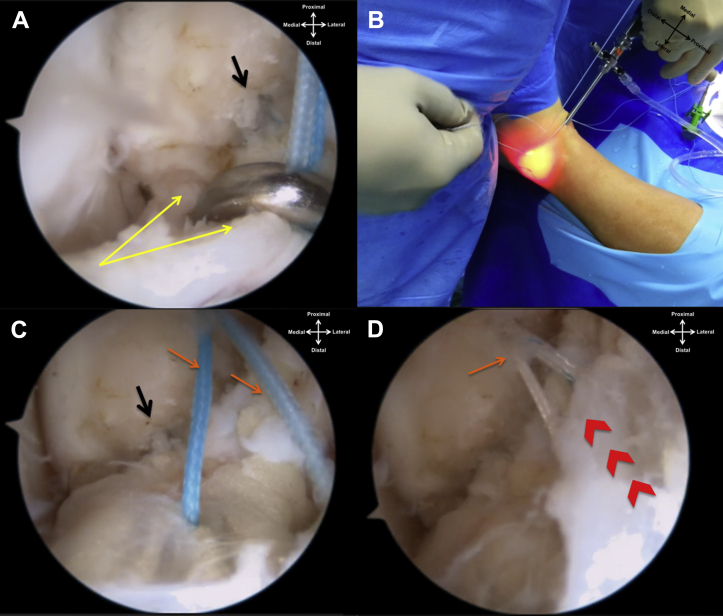
The nylon loop is reinserted (now penetrating more distal on the foot to trespass the IER), and a similar technique is used to retrieve the second solid-blue wire with the hook through the aLP. The foot is brought into a neutral position, and the first anchor is engaged by introducing 3 cm of the solid-blue wire through a nitinol loop on the deployment device. This device has a syringe-like embolus to be pressed, and another MaxBraid loop is detached (blue-white as opposed to the solid-blue wire). This second, blue-white loop is deployed and slides over the solid-blue wire. The surgeon pulls the solid-blue wire in a single continuous movement, making the blue-white loop slide and close, thus tensioning the soft tissue of the ATFL remnant against the footprint (Fig 7). A small pull on the blue-white end of the anchor finally blocks the mechanism.
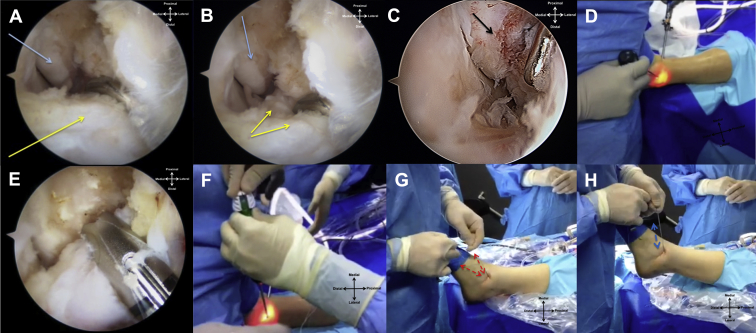
Fig 7.
Left ankle with the arthroscope through the medial portal. (A) The anterior talofibular ligament remnant (yellow arrows) is reattached to the footprint (black arrow) by the first anchor. (B) Final tensioning of the anterior talofibular ligament remnant is achieved in one single continuous movement. (C) The free space in the lateral gutter has diminished. There are no bulky knots around the anchor attachment (black arrow), and the two ends of the second anchor are visible (orange arrows). These are used to perform a pants-over-vest reinforcement with the inferior extensor retinaculum. (D) The second anchor (orange arrow) is also pulled in a continuous movement to tension the tissue of the inferior extensor retinaculum toward the lateral malleolus (red chevrons).
With the foot being kept in the neutral position, the second anchor is also armed using the previously described technique. At the end of the procedure, ankle stability and full range of motion are confirmed.
The mean tourniquet time in our first 10 consecutive cases was 37 minutes (range, 32 to 47 minutes). A compressive bandage and rigid splint or walker boot in neutral position are used for the first 2 weeks, and non–weight bearing is advised. The stitches are removed around 10 to 14 days.
Two weeks postoperatively, patients are allowed to start periods of active dorsiflexion–plantar flexion and partial weight bearing with a walker boot and crutches. Full weight bearing is achieved around 4 to 6 weeks after surgery.
Discussion
The presented technique enables effective repair of the lateral ankle ligaments in selected cases and if the technical rules are fulfilled (Table 2). However, the possible advantages and limitations of the technique must be considered (Table 3). Patient selection is not always obvious once there is a recognized need for a more objective method to evaluate the quality of the tissue of the ATFL remnant before the operation. The development of more specific instruments is also required to improve this technique in the future.
Table 2.
Pearls and Pitfalls of Procedure
| Pearls | Explanation |
|---|---|
| No distraction system is required. Ankle dorsiflexion during the procedure is a key to success. | The dorsiflexion method for anterior ankle arthroscopy creates an anterior working space and relaxes the anatomic structure during the procedure, thus lowering the rate of complications. |
| The surgeon should create the medial portal as close as possible to the center of the joint—just medial to the TAT—in full dorsiflexion at the level of the joint line. | This facilitates access to the lateral gutter. Most work is performed with the arthroscope in the medial portal, and the working instruments are inserted through the accessory lateral portal. |
| The surgeon should use the surgical blade only to cut the skin. | This prevents iatrogenic injuries. |
| The surgeon should use blunt dissection (our suggestion is to use a mosquito clamp) to create the portals and to prepare the subcutaneous tissue. | This prevents iatrogenic injuries. |
| The accessory lateral portal should be created under direct control with the arthroscope in the medial portal. | A needle is used to confirm that the portal will permit adequate instrument orientation before incision. Transillumination helps to reduce iatrogenic damage to the superficial nerves and vessels. |
| Inspection and dissection of the remnant of the ATFL comprise a key to success. | This is decisive for the outcome of the procedure. At this point, a final decision is made either to proceed as planned or to perform another repair or reconstruction technique. |
| The surgeon should debride the tip of the lateral malleolus until reaching bleeding bone before putting the anchors in place. | This step will enhance the biological reaction, thus facilitating the healing of the ligament. |
| The surgeon should take care to keep the anchor guide in place and in the same direction while drilling the bone tunnel and until the anchor is finally tapped in place. | If the direction of the guide changes during the procedure, it might result in failure of anchor deployment. |
| Immediately after putting the anchor in place, the surgeon should confirm pullout resistance and also that both ends of the anchor are adequately sliding. | If there is some problem impairing proper functioning of the anchor, this is the most adequate time to solve it. |
| The surgeon should make sure to keep both ends of each anchor always connected. | This prevents confusion and mistakes during the procedure, which could cause messing of the wires between both anchors and result in secondary errors. |
| The surgeon should avoid over-tensioning of the structures and always confirm that passive full dorsiflexion and plantar flexion are possible after ligament repair. | Excessive tension might cause secondary complaints after Broström-Gould repair. |
| Pitfalls | |
| The use of a needle as a suture passer can be considered a pitfall. | It might cause iatrogenic damage within the joint and to the ATFL remnant. More adequate instruments might be developed in the future. |
| The surgeon should avoid making multiple perforations when passing through the ATFL remnant with the 18-gauge needle. | This might cause iatrogenic damage to the remnant of the ligament. |
ATFL, anterior talofibular ligament; TAT, tibialis anterior tendon.
Table 3.
Advantages and Limitations of Procedure
| Advantages |
| Arthroscopy enables better tissue characterization. |
| Arthroscopy provides less postoperative swelling and discomfort. |
| Arthroscopic ligament repair provides better esthetic results. |
| There is a small amount of aggression to bone (2.1-mm drill tunnel). |
| There is a small risk of complications inherent to rigid anchors once these implants are made of all-soft, all-suture material. |
| The technique does not require experience in knot-tying techniques. |
| The technique diminishes the risk of bulky knots and knot migration. |
| The technique diminishes the risk of glove perforation and skin tears. |
| Limitations |
| Ankle ligament arthroscopic repair requires previous experience in ankle arthroscopy. |
| Few specific instruments have been developed for this specific purpose. This fact might create additional difficulties. |
| This procedure is not “universal.” It is only indicated when the remnant of the ATFL is considered suitable for repair. |
| Objective preoperative and perioperative criteria to define which ATFL remnants are suitable for repair are lacking. |
| The use of suture anchors increases the cost compared with some classic techniques. |
ATFL, anterior talofibular ligament.
Recent cadaveric studies have also been considered in the development of arthroscopic ankle instability repair.21, 22, 23, 24, 25, 26, 27 The described implant can be considered reliable and user-friendly. It also avoids bulky knots,4, 14 which are another possible source of complaints. The continuous single tensioning reduces complications associated with repeated pendulum movements of classic knot tying and minimizes the risk of glove perforation and skin tears.
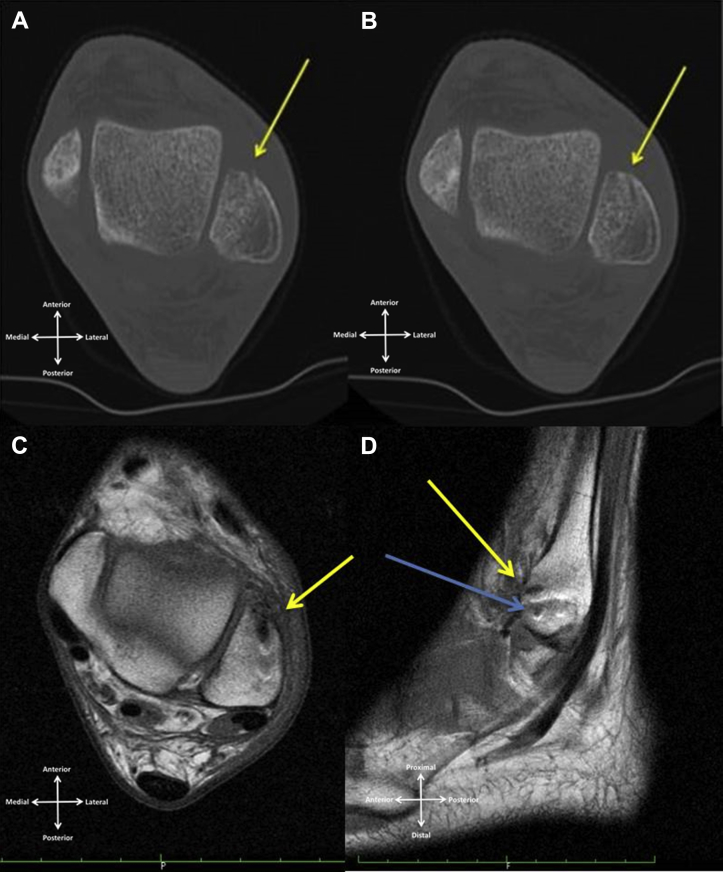
Early computed tomography and magnetic resonance imaging evaluation (Fig 8) confirmed that the defect induced in the bone can be considered minimal despite the high pullout resistance of the anchor that we used.28 It induces minimal bony aggression stating no limitation to any subsequent surgical approach to that area. Being an all-suture anchor, it minimizes the risk of articular damage attributable to implant migration or implant failure.
Fig 8.
(A, B) Computed tomography evaluation of a left ankle showing the small defects (yellow arrows) caused by the 2.1-mm anchors 2 months postoperatively. (C, D) Magnetic resonance imaging T1 evaluation of left ankle 2 months postoperatively. Some signal changes are explained by the short interval from surgery. (D) On the sagittal view, both tunnels can be identified (blue and yellow arrows).
Future studies are required concerning long-term follow-up. The advance of biomaterials and tissue engineering is fundamental in the development of surgery. However, surgeons must understand the advantages and limitations of every implant to adapt, progress, and improve the outcome.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Surgical technique for arthroscopic lateral ankle ligament repair using an anchor exclusively made of suture material. Two portals are required to accomplish a modified Broström-Gould repair. This anchor avoids the need for classic knot-tying techniques and diminishes the chance of knot migration, as well as the risk of glove perforation and skin tears. All images correspond to a left ankle.
References
- 1.de Vries J.S., Krips R., Sierevelt I.N., Blankevoort L. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011:CD004124. doi: 10.1002/14651858.CD004124.pub3. [DOI] [PubMed] [Google Scholar]
- 2.van Dijk C.N. Springer; Berlin: 2014. Ankle arthroscopy: Techniques developed by the Amsterdam Foot and Ankle School. [Google Scholar]
- 3.Vega J., Golano P., Pellegrino A., Rabat E., Pena F. All-inside arthroscopic lateral collateral ligament repair for ankle instability with a knotless suture anchor technique. Foot Ankle Int. 2013;34:1701–1709. doi: 10.1177/1071100713502322. [DOI] [PubMed] [Google Scholar]
- 4.Corte-Real N.M., Moreira R.M. Arthroscopic repair of chronic lateral ankle instability. Foot Ankle Int. 2009;30:213–217. doi: 10.3113/FAI.2009.0213. [DOI] [PubMed] [Google Scholar]
- 5.Takao M, Matsui K, Stone JW, et al. Arthroscopic anterior talofibular ligament repair for lateral instability of the ankle. Knee Surg Sports Traumatol Arthrosc in press, available online 16 May, 2015. doi:10.1007/s00167-015-3638-0. [DOI] [PMC free article] [PubMed]
- 6.Lui T.H. Modified arthroscopic Brostrom procedure. Foot Ankle Surg. 2015;21:216–219. doi: 10.1016/j.fas.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Guillo S., Cordier G., Sonnery-Cottet B., Bauer T. Anatomical reconstruction of the anterior talofibular and calcaneofibular ligaments with an all-arthroscopic surgical technique. Orthop Traumatol Surg Res. 2014;100:S413–S417. doi: 10.1016/j.otsr.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Guillo S., Archbold P., Perera A., Bauer T., Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014;3:e593–e598. doi: 10.1016/j.eats.2014.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matsui K., Takao M., Miyamoto W., Innami K., Matsushita T. Arthroscopic Broström repair with Gould augmentation via an accessory anterolateral port for lateral instability of the ankle. Arch Orthop Trauma Surg. 2014;134:1461–1467. doi: 10.1007/s00402-014-2049-x. [DOI] [PubMed] [Google Scholar]
- 10.Cottom J.M., Rigby R.B. The “all inside” arthroscopic Broström procedure: A prospective study of 40 consecutive patients. J Foot Ankle Surg. 2013;52:568–574. doi: 10.1053/j.jfas.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 11.Acevedo J., Mangone P.G. Arthroscopic lateral ankle ligament reconstruction. Tech Foot Ankle Surg. 2011;10:111–116. [Google Scholar]
- 12.Kim E.S., Lee K.T., Park J.S., Lee Y.K. Arthroscopic anterior talofibular ligament repair for chronic ankle instability with a suture anchor technique. Orthopedics. 2011;34273 doi: 10.3928/01477447-20110228-03. [DOI] [PubMed] [Google Scholar]
- 13.Nery C., Raduan F., Del Buono A., Asaumi I.D., Cohen M., Maffulli N. Arthroscopic-assisted Broström-Gould for chronic ankle instability: A long-term follow-up. Am J Sports Med. 2011;39:2381–2388. doi: 10.1177/0363546511416069. [DOI] [PubMed] [Google Scholar]
- 14.Wang J., Hua Y., Chen S., Li H., Zhang J., Li Y. Arthroscopic repair of lateral ankle ligament complex by suture anchor. Arthroscopy. 2014;30:766–773. doi: 10.1016/j.arthro.2014.02.023. [DOI] [PubMed] [Google Scholar]
- 15.Brown C.A., Hurwit D., Behn A., Hunt K.J. Biomechanical comparison of an all-soft suture anchor with a modified Broström-Gould suture repair for lateral ligament reconstruction. Am J Sports Med. 2014;42:417–422. doi: 10.1177/0363546513517873. [DOI] [PubMed] [Google Scholar]
- 16.Suchenski M., McCarthy M.B., Chowaniec D. Material properties and composition of soft-tissue fixation. Arthroscopy. 2010;26:821–831. doi: 10.1016/j.arthro.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 17.Pereira H., Correlo V.M., Silva-Correia J., Oliveira J.M., Reis R.L., Espregueira-Mendes J. Migration of “bioabsorbable” screws in ACL repair. How much do we know? A systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:986–994. doi: 10.1007/s00167-013-2414-2. [DOI] [PubMed] [Google Scholar]
- 18.Martinez A., Han Y., Sardar Z.M. Risk of glove perforation with arthroscopic knot tying using different surgical gloves and high-tensile strength sutures. Arthroscopy. 2013;29:1552–1558. doi: 10.1016/j.arthro.2013.05.022. [DOI] [PubMed] [Google Scholar]
- 19.Kim S.H., Crater R.B., Hargens A.R. Movement-induced knot migration after anterior stabilization in the shoulder. Arthroscopy. 2013;29:485–490. doi: 10.1016/j.arthro.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 20.van Dijk C.N., van Bergen C.J. Advancements in ankle arthroscopy. J Am Acad Orthop Surg. 2008;16:635–646. doi: 10.5435/00124635-200811000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Golano P., Vega J., de Leeuw P.A. Anatomy of the ankle ligaments: A pictorial essay. Knee Surg Sports Traumatol Arthrosc. 2010;18:557–569. doi: 10.1007/s00167-010-1100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Giza E., Whitlow S.R., Williams B.T. Biomechanical analysis of an arthroscopic Broström ankle ligament repair and a suture anchor-augmented repair. Foot Ankle Int. 2015;36:836–841. doi: 10.1177/1071100715576539. [DOI] [PubMed] [Google Scholar]
- 23.Giza E., Shin E.C., Wong S.E. Arthroscopic suture anchor repair of the lateral ligament ankle complex: A cadaveric study. Am J Sports Med. 2013;41:2567–2572. doi: 10.1177/0363546513500639. [DOI] [PubMed] [Google Scholar]
- 24.Lee KT, Kim ES, Kim YH, Ryu JS, Rhyu IJ, Lee YK. All-inside arthroscopic modified Broström operation for chronic ankle instability: A biomechanical study. Knee Surg Sports Traumatol Arthrosc in press, available online 4 July, 2015. doi:10.1007/s00167-014-3159-2. [DOI] [PubMed]
- 25.Clanton T.O., Campbell K.J., Wilson K.J. Qualitative and quantitative anatomic investigation of the lateral ankle ligaments for surgical reconstruction procedures. J Bone Joint Surg Am. 2014;96:e98. doi: 10.2106/JBJS.M.00798. [DOI] [PubMed] [Google Scholar]
- 26.Drakos M., Behrens S.B., Mulcahey M.K., Paller D., Hoffman E., DiGiovanni C.W. Proximity of arthroscopic ankle stabilization procedures to surrounding structures: An anatomic study. Arthroscopy. 2013;29:1089–1094. doi: 10.1016/j.arthro.2013.02.011. [DOI] [PubMed] [Google Scholar]
- 27.Neuschwander T.B., Indresano A.A., Hughes T.H., Smith B.W. Footprint of the lateral ligament complex of the ankle. Foot Ankle Int. 2013;34:582–586. doi: 10.1177/1071100712466851. [DOI] [PubMed] [Google Scholar]
- 28.Barber F.A., Herbert M.A., Hapa O. Biomechanical analysis of pullout strengths of rotator cuff and glenoid anchors: 2011 update. Arthroscopy. 2011;27:895–905. doi: 10.1016/j.arthro.2011.02.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique for arthroscopic lateral ankle ligament repair using an anchor exclusively made of suture material. Two portals are required to accomplish a modified Broström-Gould repair. This anchor avoids the need for classic knot-tying techniques and diminishes the chance of knot migration, as well as the risk of glove perforation and skin tears. All images correspond to a left ankle.