Abstract
BACKGROUND:
Six million US children are uninsured, despite two-thirds being eligible for Medicaid/Children’s Health Insurance Program (CHIP), and minority children are at especially high risk. The most effective way to insure uninsured children, however, is unclear.
METHODS:
We conducted a randomized trial of the effects of parent mentors (PMs) on insuring uninsured minority children. PMs were experienced parents with ≥1 Medicaid/CHIP-covered child who received 2 days of training, then assisted families for 1 year with insurance applications, retaining coverage, medical homes, and social needs; controls received traditional Medicaid/CHIP outreach. The primary outcome was obtaining insurance 1 year post-enrollment.
RESULTS:
We enrolled 237 participants (114 controls; 123 in PM group). PMs were more effective (P< .05 for all comparisons) than traditional methods in insuring children (95% vs 68%), and achieving faster coverage (median = 62 vs 140 days), high parental satisfaction (84% vs 62%), and coverage renewal (85% vs 60%). PM children were less likely to have no primary care provider (15% vs 39%), problems getting specialty care (11% vs 46%), unmet preventive (4% vs 22%) or dental (18% vs 31%) care needs, dissatisfaction with doctors (6% vs 16%), and needed additional income for medical expenses (6% vs 13%). Two years post-PM cessation, more PM children were insured (100% vs 76%). PMs cost $53.05 per child per month, but saved $6045.22 per child insured per year.
CONCLUSIONS:
PMs are more effective than traditional Medicaid/CHIP methods in insuring uninsured minority children, improving health care access, and achieving parental satisfaction, but are inexpensive and highly cost-effective.
What’s Known on This Subject:
Six million US children are uninsured, despite two-thirds being Medicaid/CHIP eligible; minority children are at high risk. Few trials have evaluated interventions to insure uninsured children, and none has assessed the effectiveness of parent mentors in insuring uninsured minority children.
What This Study Adds:
Parent mentors are more effective and faster than traditional methods in insuring uninsured minority children, renewing coverage, improving health care and dental access, reducing unmet needs, and achieving parental satisfaction, but are inexpensive and highly cost-effective, saving $6045 per child.
Over 5.9 million American children (8%) lack health insurance.1 Among uninsured US children, 62% to 72% (3.7–4.3 million) are eligible for but not enrolled in Medicaid or the Children’s Health Insurance Program (CHIP).2–5 For uninsured, low-income children (with family incomes <200% of federal poverty threshold), 84% are eligible for but not enrolled in Medicaid/CHIP.6
Racial/ethnic disparities exist in insurance coverage for US children. Compared with an uninsured rate of 5% for white children, 12% of Latino, 8% of African-American, and 8% of Asian/Pacific Islander children are uninsured.1 Latino and African-American children comprise 57% of uninsured children, although constituting only 42% of US children.7
Although millions of US children continue to be uninsured, not enough is known about the most effective interventions for insuring uninsured children. Parent mentors (PMs) are a special category of community health workers for children in which parents who have children with particular health conditions/risks leverage their relevant experience, along with additional training, to assist, counsel, and support other parents of children with the same health conditions/risks. Although PMs have been found to be effective in improving outcomes for minority asthmatic children,8 they have not been evaluated as an intervention to insure uninsured children. We therefore conducted a randomized controlled trial (RCT) of the effects of PMs on insuring uninsured minority children.
Methods
Trial Design
The Kids’ Health Insurance by Educating Lots of Parents (Kids’ HELP) RCT was conducted from June 2011 to April 2015 in Dallas County, TX, communities with high proportions of uninsured minority and low-income children. The study design/rationale are described in detail elsewhere.9
Informed written consent was obtained in English or Spanish from primary caregivers by using protocols approved by the UT Southwestern Institutional Review Board.
Recruitment
Eligibility criteria included the primary caregiver had ≥1 child 0 to 18 years old who lacked health insurance but was Medicaid/CHIP eligible (only 1 child/family was enrolled, to avoid clustering in analyses), and the primary caregiver self-identified the child as Latino/Hispanic or African-American. Using information from caregivers, researchers verified children’s Medicaid/CHIP eligibility, based on Texas criteria.10
Participants were recruited from Dallas communities with the highest proportions of low-income, minority families with uninsured children.11 Bilingual researchers recruited participants at 97 community sites, including supermarkets, department stores, Goodwill stores, restaurants, libraries, community centers, food banks, health fairs, YMCAs, churches, schools, community clinics, day-care establishments, laundromats, apartment complexes, homeless shelters, and Special Supplemental Nutrition Program for Women, Infants, and Children centers. Participants received honoraria of $50 at enrollment, $5 for monthly follow-ups, and $10 for 6- and 12-month surveys.
Intervention
PMs were parents with ≥1 child covered by Medicaid/CHIP for ≥1 year. PMs were recruited from June 2011 to August 2013 at a hospital-based Resident Continuity Clinic, charter school, and via established PM referrals (see https://vimeo.com/95286928). Interviews were conducted to identify optimal candidates, characterized by reliability, timeliness, persistence, and desire to help families with uninsured children. From 31 candidates interviewed, 15 PMs were chosen. PMs received monthly stipends for each family mentored. PMs and intervention participants were matched by race/ethnicity and zip code (whenever possible). Latino families were matched with fluently bilingual Latino PMs.
PMs participated in 2-day training sessions (see: https://vimeo.com/95286929). Session content was based on training provided to community case managers in the research team’s previous successful RCT,12 and addressed 9 topics: Why health insurance is so important for US children; the Kids’ HELP trial; being a successful PM; PM responsibilities; Medicaid and CHIP programs; Medicaid/CHIP application process; next steps after obtaining Medicaid/CHIP; importance of medical homes and taking an active role in pediatric care; and study paperwork. Training session content was detailed in the PM’s manual (available in English and Spanish), which PMs carried in the field. Post-training, overall test scores (0–100 scale) significantly increased, from a mean = 62 (range: 39–82) to 88 (67–100; P < .01), and wrong answers decreased (mean reduction = 8; P < .01). Significant improvements occurred in 6 of 9 topics, and 100% of PMs reported being very satisfied (86%) or satisfied (14%) with the training. Full details on the manual and training session outcomes are available elsewhere.13
PMs performed the following functions for intervention-group children and families: (1) education about insurance programs and application processes; (2) education/assistance regarding Medicaid/CHIP eligibility; (3) completing insurance applications together with caregivers and submission assistance; (4) expediting coverage decisions by early, frequent contact with Medicaid/CHIP representatives; (5) advocating for families by liaising between families and Medicaid/CHIP programs; (6) contacting Medicaid/CHIP representatives to remedy situations in which children incorrectly were deemed ineligible or had insurance inappropriately discontinued; (7) assistance with renewal application completion/submission; and (8) teaching caregivers how to renew Medicaid/CHIP or reapply after losing coverage. PMs followed up to 10 families at a time. Data document high levels of PM engagement with families, with means of 19.8 home visits and 161.4 phone/e-mail/text-message contacts/family. Complete details on PM functions are available elsewhere.9,13
Control Group
Controls received no intervention, given access to standard-of-care outreach/enrollment by Texas Medicaid/CHIP. The Texas Health and Human Services Commission (HHSC), which oversees Texas Medicaid/CHIP, launched a 2006–2007 outreach/education campaign to raise families’ CHIP/Medicaid awareness and “…emphasize the importance of health insurance and regular preventive care, explain how to apply for coverage and encourage families to complete the renewal process on time to avoid gaps in coverage for their children.”14 This campaign included bilingual radio, television, and newspaper advertisements; bus and bus-bench messages; Web sites with application links and order forms/materials for community-based organizations; and daycare-center outreach.14
Randomization
Computer-generated randomization was performed to allocate eligible participants in a 1:1 ratio to the intervention or control group. Randomization was performed by using permuted blocks stratified by child race/ethnicity.
Outcomes
The primary outcome was the child obtaining health insurance. Parents initially reported when children obtained coverage, with verification by parents providing copies or photos of insurance cards or HHSC letters documenting coverage and the effective date. HHSC provided second verifications for all participants. Other insurance-related outcomes included the number of days from study enrollment to obtaining insurance, sporadic coverage (obtained but then lost insurance), insurance renewal, insurance coverage 1 and 2 years post-intervention cessation, and parental satisfaction with the process of obtaining coverage.
Secondary outcomes were evaluated for all children (whether or not they obtained insurance) by using validated questions derived from national, state, and regional surveys and previously published work,12,15–27 and included health status, health-related quality of life, health care access, unmet medical and dental needs, use of health services, out-of-pocket costs, parental ratings of quality of the child’s health care, parental satisfaction with care, family financial burden, and missed school and work days because of the child’s illness. Outcomes and survey items are described in detail elsewhere.9
Data Collection
Outcomes were monitored by a researcher blinded to group allocation. The primary outcome and other insurance-related outcomes were assessed monthly; other outcomes were evaluated 6 and 12 months post-enrollment, except parental satisfaction with the coverage process, which was assessed 12 months post-enrollment. For participants agreeing to long-term follow-up after completing the 12-month follow-up, we administered questionnaires every 3 months for up to 2 years.
Analysis
The sample size was calculated by using a power of 80% to detect an intergroup difference of 20 percentage points in children’s insurance rates, at an α = 0.05. Accounting for up to 40% attrition, at least 216 participants (108 in each group) needed to be enrolled. Intention-to-treat intergroup comparisons were performed by using the Wilcoxon test, Pearson’s χ2 test, analysis of variance, stepwise multivariable logistic regression with generalized estimating equations, and an adjusted cumulative incidence curve; all tests were 2-sided. The trial’s clinicaltrials.gov identifier is NCT01264718.
Cost-Effectiveness Analysis
The cost-effectiveness analysis (CEA) used methodological principles detailed by the US Public Health Services Panel on Cost-Effectiveness in Health and Medicine.28,29 Cost items monitored and evaluated included direct health care costs, health insurance enrollment fees, intervention costs, and indirect costs.
Direct health care costs were calculated by using monthly parental reports (given access to medical records from multiple facilities was not feasible) of out-of-pocket costs and health services use in the past month, consistent with validated methods used in a recent CEA.30 Costs of health services (including emergency department [ED] visits, hospitalizations, and ICU stays) were derived from mean Texas Medicaid/CHIP reimbursements for specific services in the year of receipt.
Insurance enrollment fees were assessed by collecting information about coverage obtained and any associated enrollment fee.
Intervention costs were calculated by summing all intervention program costs, including PM payments, supplies, honoraria, and travel. PMs maintained detailed activity and time logs, permitting assessment of both total time spent per family and per activity.
Indirect costs included missed parental work days and parental time costs while seeking health insurance. Parents reported time spent seeking insurance information, completing paperwork, and calling/visiting state offices or private insurers. Time costs were converted to dollars by using wage rates. For employed parents, actual self-reported wage rates were used.
The incremental cost-effectiveness ratio (ICER) was calculated by using standard methods28,29: the difference in total costs between the intervention group and controls was divided by the intergroup difference in the proportion of insured children.
Results
Participants
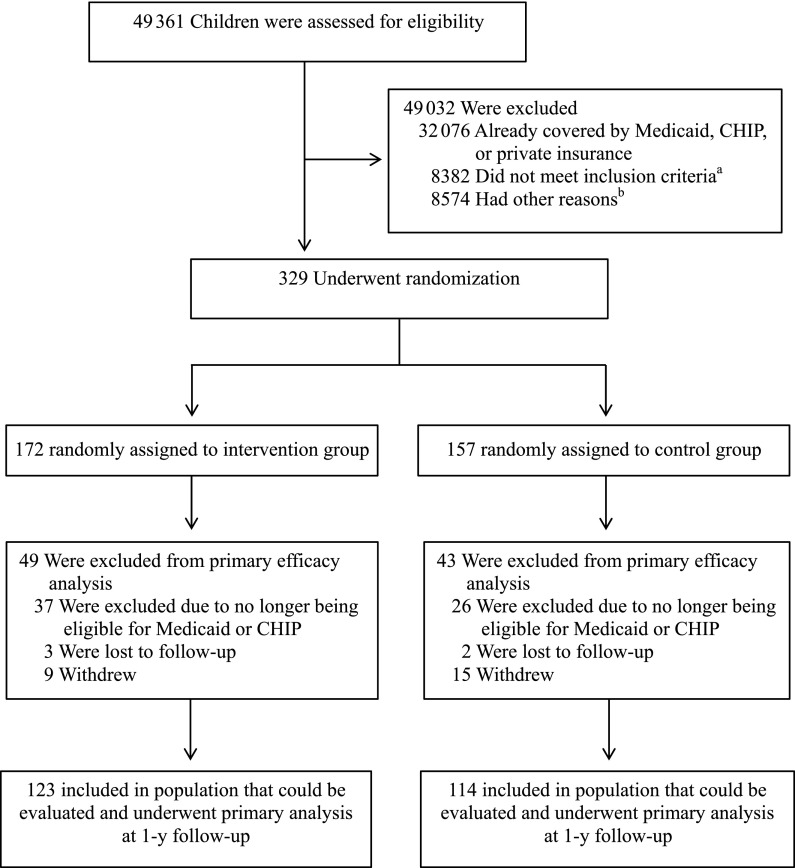
A total of 329 participants were randomly assigned to the PM intervention (N = 172) or control group (N = 157; Fig 1). After exclusions for subsequent Medicaid/CHIP ineligibility, losses to follow-up, and withdrawals, 123 pm-group participants and 114 controls comprised the final evaluable populations. These groups had similar characteristics (Table 1), except gender, for which adjustments were made in multivariable analyses. The median child age was 7 years old; approximately two-thirds of participants were Latino and one-third were African-American. The median annual family income was approximately $21 000, and children had been uninsured for a median of 7 months.
FIGURE 1.
Enrollment, randomization, and follow-up. aIncluding had no child, child > 18 years old, did not reside in target community, and family income above qualifying threshold for Medicaid/CHIP. bIncluding not interested, took information without further follow-up, legal custody issues, and language barrier.
TABLE 1.
Baseline Characteristics of Participants
| Characteristica | Control Group (N = 114) | PM Group (N = 123) |
|---|---|---|
| Selected sociodemographic characteristics | ||
| Median child age (IQR), y | 7 (4–12) | 7 (3–10) |
| Female child gender, n (%)b | 47 (41) | 72 (58) |
| Child race/ethnicity, n (%)c | ||
| Latino | 75 (66) | 80 (65) |
| African-American | 39 (34) | 43 (35) |
| Mean caregiver age, y | 37.5 ± 10.9 | 35.7 ± 9.4 |
| Female caregiver gender, n (%) | 110 (96) | 117 (95) |
| Primary caregiver’s relationship to child, n (%) | ||
| Biological mother | 101 (89) | 114 (93) |
| Biological father | 3 (3) | 5 (4) |
| Other | 10 (9) | 4 (3) |
| Caregiver not high-school graduate | 36 (32) | 49 (40) |
| Caregiver unemployed | 82 (72) | 97 (79) |
| Primary caregiver born in US | 51 (45) | 63 (51) |
| Primary caregiver US citizen | 59 (52) | 64 (52) |
| Median annual combined family income (IQR) | $21 300 ($13 100–$29 000) | $20 800 ($14 000–$30 000) |
| Median months child uninsured (IQR) | 8 (3–24) | 6 (4–12) |
| Health status and health-related quality of life | ||
| Child’s health status not excellent or very good, n (%)c | 50 (44) | 43 (35) |
| PedsQL total score | 89.7 ± 11.6 | 88.3 ± 14.6 |
| Access to care and unmet needs, n (%) | ||
| Child has no PCP | 75 (66) | 75 (61) |
| Child has no usual source of preventive care | 52 (46) | 43 (35) |
| Child has no usual source of sick care | 20 (18) | 21 (17) |
| Different source of sick care and preventive care | 65 (57) | 62 (50) |
| Never/sometimes gets immediate care from PCP | 13 (27) | 9 (16) |
| Has problems getting care from specialistsd | 12 (46) | 7 (41) |
| Delayed or did not get needed health care in past year | 85 (75) | 85 (69) |
| Did not receive all needed preventive care in past year | 44 (54) | 44 (50) |
| Did not receive all needed acute care in past year | 43 (81) | 62 (82) |
| Did not receive all needed dental care in past year | 57 (63) | 60 (59) |
| Did not receive all needed prescription medications in past year | 15 (24) | 9 (13) |
| Use of health services and out-of-pocket costse | ||
| Doctor visits in past year | 3.2 ± 0.4 | 3.0 ± 0.2 |
| Out-of-pocket cost per doctor visit | $161.31 ± 71.3 | $121.90 ± 27.7 |
| Preventive-care visits in past year | 1.0 ± 0.1 | 0.9 ± 0.1 |
| Out-of-pocket cost per preventive-care visit | $64.32 ± 26.8 | $29.11 ± 7.8 |
| Sick visits in past year | 1.7 ± 0.3 | 1.6 ± 0.2 |
| Out-of-pocket cost per sick visit | $201.39 ± 99.7 | $188.84 ± 61.2 |
| ED visits in past year | 1.0 ± 0.3 | 0.7 ± 0.1 |
| Out-of-pocket cost per ED visit | $351.19 ± 194.4 | $499.58 ± 163.3 |
| Hospitalizations in past year | 0.2 ± 0.1 | 0.1 ± 0.1 |
| Out-of-pocket cost per hospitalization | $1500 ± 1250 | $633 ± 535.20 |
| Quality of caref | ||
| Quality rating of child’s well-child care | 8.2 ± 2.1 | 8.5 ± 1.9 |
| Quality rating of child’s PCP | 8.7 ± 2.2 | 9.1 ± 1.6 |
| Quality rating of child’s acute care | 8.7 ± 2.2 | 8.6 ± 2.0 |
| Quality rating of child’s specialty care | 8.6 ± 0.5 | 7.7 ± 4.0 |
| Parental satisfaction with care, n (%) | ||
| Doctor never/sometimes takes time to understand child’s specific needs | 25 (22) | 27 (22) |
| Doctor never/sometimes respects you are expert on your child | 17 (15) | 20 (16) |
| Doctor never/sometimes understands how you prefer to raise child | 34 (30) | 34 (28) |
| Doctor did not spend enough time with child | 17 (15) | 19 (16) |
| Did not ask all questions I wanted to ask | 16 (17) | 14 (14) |
| Would not recommend child’s health care provider to friends | 32 (28) | 23 (19) |
| Family financial burden and missed school and work days due to child’s illness, n (%) | ||
| Need additional income to cover child’s medical expenses | 51 (45) | 51 (42) |
| Child’s health caused financial problems for family | 40 (35) | 44 (36) |
| Family cut down on work hours to obtain health care for child | 26 (23) | 25 (21) |
| Median no. of missed school days in past year (IQR) | 2 (1–5) | 2 (1–5) |
| Median no. of missed work days in past year due to child’s illness (IQR) | 0 (0–1) | 0 (0–2) |
| Median caregiver wage loss due to missed work days to care for sick child (IQR) | $155 ($75–$276) | $208 ($100–$324) |
| Median other costs related to taking care of sick child (IQR) | $70 ($20–$200) | $45 ($25–$87.50) |
IQR, interquartile range; PedsQL, Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales.
baseline characteristics, except where noted.
Plus-minus values are means ± SD, except where noted. There were no significant intergroup differences in
P = .02.
By caregiver report.
Among those who reported that their child needed specialty care.
Plus-minus values are means ± SE.
By caregiver report, using a scale of 0 to 10, in which 0 = worst possible rating and 10 = best possible rating.
Primary Outcome
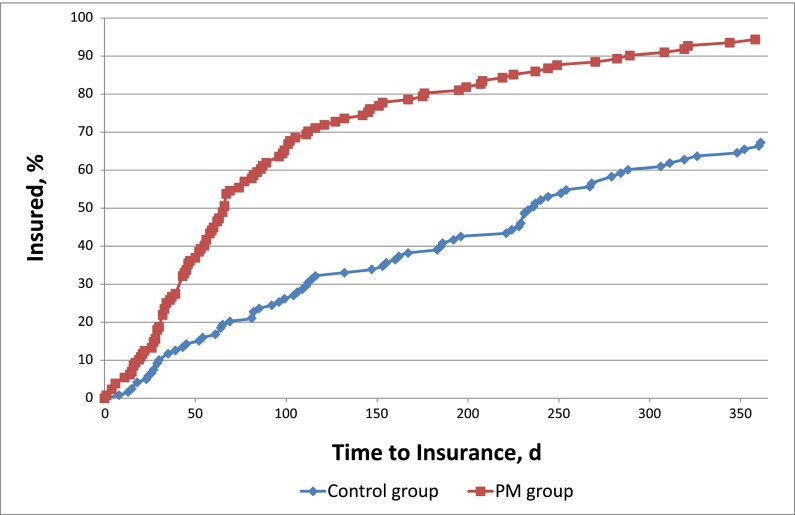
At 1-year follow-up, the PM group was more likely than controls to obtain health insurance, at 95% vs 68% (P < .001; Table 2). After adjustment, the PM group had 1.30 times the relative risk (95% confidence interval [CI]: 1.21–1.32) and 2.93 times the odds (95% CI: 2.14–4.00) of controls of obtaining insurance. An adjusted incidence curve revealed a marked intergroup difference in coverage emerging by the 100th day of follow-up and sustained over the 1-year follow-up period (Fig 2).
TABLE 2.
Study Outcomes at 1-Year Follow-Up and for Long-Term Insurance Coverage
| Outcomea | Control Group (n = 114) | PM Group (n = 123) | P |
|---|---|---|---|
| Primary outcome: child obtained health insurance, n (%) | 78 (68) | 117 (95) | <.001 |
| Adjusted relative risk (95% CI)b | Referent | 1.30 (1.21–1.32) | <.001 |
| Adjusted odds ratio (95% CI)b | Referent | 2.93 (2.14–4.00) | <.001 |
| Median number of days to obtaining insurance (IQR) | 140 (61–236) | 62 (33–112) | <.001 |
| Sporadic insurance coverage, n (%)c | 39 (34) | 32 (26) | .21 |
| Renewed insurance, n (%)d | 42 (60) | 80 (85) | <.001 |
| Health-insurance coverage 1 y after cessation of PM intervention, n (%)e | 62 (76) | 73 (95) | <.001 |
| Health-insurance coverage 2 y after cessation of PM intervention, n (%)f | 32 (76) | 39 (100) | <.001 |
| Parental satisfaction with process of trying to obtain health insurance for child, n (%) | <.001 | ||
| Very satisfied | 28 (25) | 69 (57) | |
| Satisfied | 45 (40) | 33 (27) | |
| Uncertain | 17 (15) | 12 (10) | |
| Dissatisfied | 10 (9) | 5 (4) | |
| Very dissatisfied | 13 (12) | 2 (2) | |
| Health status and health-related quality of life | |||
| Health status not excellent/very good, n (%)g | 41 (36) | 31 (25) | .07 |
| PedsQL total score | 94.3 ± 9.3 | 94.0 ± 9.7 | .84 |
| Access to health care, n (%) | |||
| Child has no PCP | 45 (40) | 19 (16) | <.001 |
| Child has no usual source of preventive care | 8 (7) | 1 (1) | .013 |
| Child has no usual source of sick care | 8 (7) | 3 (2) | .09 |
| Different source of sick care and preventive care | 31 (27) | 19 (16) | .03 |
| Never/sometimes gets immediate care from PCP | 5 (19) | 0 (0) | .03 |
| Has problems getting care from specialistsh | 6 (46) | 2 (11) | .03 |
| Delayed or did not get needed health care in past year | 29 (25) | 16 (13) | .02 |
| Did not receive all needed preventive care in past year | 16 (22) | 4 (4) | <.001 |
| Did not receive all needed acute care in past year | 5 (20) | 1 (3) | .04 |
| Did not receive all needed dental care in past year | 27 (31) | 18 (18) | .03 |
| Did not receive all needed prescription medications in past year | 2 (4) | 1 (2) | .42 |
| Use of health services and out-of-pocket costsi | |||
| Doctor visits in past year | 2.6 ± 0.3 | 2.9 ± 0.3 | .24 |
| Out-of-pocket cost per doctor visit | $37.24 ± 7.5 | $32.87 ± 24.0 | <.001 |
| Preventive-care visits in past year | 0.9 ± 0.1 | 1.3 ± 0.1 | .01 |
| Out-of-pocket cost per preventive-care visit | $27.49 ± 9.0 | $4.63 ± 1.5 | .09 |
| Sick visits in past year | 1.6 ± 0.3 | 1.4 ± 0.2 | .64 |
| Out-of-pocket cost per sick visit | $42.74 ± 9.4 | $9.38 ± 3.1 | <.001 |
| ED visits in past year | 0.34 ± 0.1 | 0.33 ± 0.1 | .59 |
| Out-of-pocket cost per ED visit | $94.04 ± 92.5 | $80.74 ± 33.0 | .22 |
| Hospitalizations in past year | 0.03 ± 0.02 | 0.02 ± 0.03 | .35 |
| Out-of-pocket cost per hospitalization | $25.00 ± 22.5 | $0 ± 0 | .25 |
| Quality of carej | |||
| Quality rating of child’s well-child care | 8.6 ± 1.5 | 8.9 ± 1.4 | .03 |
| Quality rating of child’s PCP | 9.0 ± 1.7 | 9.2 ± 1.3 | .55 |
| Quality rating of child’s acute care | 8.8 ± 1.6 | 9.2 ± 1.2 | .07 |
| Quality rating of child’s specialty care | 8.1 ± 2.5 | 8.8 ± 1.7 | .22 |
| Parental satisfaction with care, n (%) | |||
| Doctor never/sometimes takes time to understand child’s specific needs | 27 (24) | 15 (12) | .02 |
| Doctor never/sometimes respects you are expert on your child | 26 (23) | 13 (11) | .01 |
| Doctor never/sometimes understands how you prefer to raise child | 42 (37) | 31 (25) | .04 |
| Doctor did not spend enough time with child | 12 (11) | 11 (9) | .68 |
| Did not ask all questions I wanted to ask | 9 (8) | 6 (5) | .34 |
| Would not recommend child’s health care provider to friends | 18 (16) | 7 (6) | .01 |
| Family financial burden and missed school and work days due to child’s illness, n (%) | |||
| Need additional income to cover child’s medical expenses | 15 (13) | 7 (6) | .04 |
| Child’s health caused financial problems for family | 16 (14) | 9 (7) | .09 |
| Family cut down on work hours to obtain health care for child | 9 (8) | 6 (5) | .34 |
| Median caregiver wage loss due to missed work days to care for sick child (IQR) | $200 ($135–300) | $240 ($125–408) | .18 |
| Median other costs related to taking care of sick child (IQR) | $324 ($30–600) | $150 ($80–1344) | .58 |
| Median number of missed school days in past year (IQR) | 2.0 (0–3) | 2.0 (0–4) | .83 |
| Median number of missed work days in past year due to child’s illness (IQR) | 0 (0–0) | 0 (0–0) | .65 |
IQR, interquartile range; PedsQL, Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales.
combined income below the federal poverty threshold.
CHIP in Texas require annual renewal).
control group and 77 in the PM group could be evaluated and were assessed for health-insurance coverage.
the control group and 39 in the PM group could be evaluated and were assessed for health-insurance coverage.
Plus-minus values are means ± SD, except where indicated.
Adjusted for child gender and age, citizenship and employment status of primary caregiver, and an annual
Child was insured but then lost health insurance at some point during the 1-y follow-up interval.
Among children covered by Medicaid who were required to renew coverage after 6 mo (children covered by
At the 2-y follow-up assessment, 1 y after cessation of the PM intervention, when a total of 82 children in the
At the 3-y follow-up assessment, 2 y after cessation of the PM intervention, when a total of 42 children in
By caregiver report.
Among those who reported that their child needed specialty care.
Plus-minus values are means ± SE.
By caregiver report, using a scale of 0 to 10, in which 0 = worst possible rating and 10 = best possible rating.
FIGURE 2.
Adjusted incidence curve of insurance coverage for study participants. Covariates adjusted for include child’s age and gender, parental citizenship and employment, and family income.
Secondary Outcomes
The PM group obtained insurance quicker (median = 62 vs 140 days; P < .001) than controls, and was more likely to renew coverage (Table 2) and be insured both 1 year and 2 years after intervention cessation. PM group caregivers were more likely to be very satisfied with the process of trying to obtain children’s insurance, and less likely to be dissatisfied or very dissatisfied. The PM group was less likely to have no primary care provider (PCP), no usual source of preventive care, different sources of sick and preventive care, to never/sometimes get immediate care from the PCP, and to have problems getting specialist care. PM children were less likely to delay/not obtain needed health care, and to not receive needed preventive, acute, or dental care.
The mean number of preventive care visits was higher for PM than control children (Table 2). Mean out-of-pocket costs were lower for PM children for doctor visits and sick visits. PM-group parents rated the quality of their children’s well-child care higher, and were less likely to report dissatisfaction with their child’s health care for several measures: the doctor never/only sometimes takes time to understand the child’s specific needs, respects you are the expert on your child, and understands how you prefer to raise your child, and the parent would not recommend the child’s health care provider to friends.
Costs/CEA
The mean monthly cost (±SD) per participant of the PM intervention was $53.05 ± 10.41. The most expensive item was PM stipends ($33.20 [±3.50]), followed by program personnel ($15.60 [±9.10], to identify/recruit uninsured children), PM travel ($2.13 [±1.42]), supplies ($1.07 [±0.35]), PM training sessions ($0.70 [±0.20]), and PM-program personnel meetings ($0.35 [±0.02]).
Controls had higher total costs than the PM group for ED visits, hospitalizations, ICU stays, and wage loss/other costs of caring for sick children (Table 3). Most subjects (98% in each group) experienced at least 1 of these events, but no specific event/condition accounted for intergroup cost differences. Overall costs were $454 647 for controls and $291 426 for PM-group children. ICERs revealed the PM intervention saved $6045.22 per child insured per year and $4185.15 for each percent increase in children obtaining insurance per year (Table 3).
TABLE 3.
Analysis of Costs and Cost Effectiveness of PM Intervention
| Itema | Control Group | PM Group |
|---|---|---|
| PM stipends—total cost | — | $53 838 |
| PM travel and supplies—total cost | — | $5195 |
| PM training sessions and meetings—total cost | — | $1411.61 |
| Program coordinator salary—total cost | — | $25 350 |
| ED visitsa—total cost | $62 730 | $60 885 |
| Hospitalizationsb—total cost | $81 234 | $58 431 |
| ICU staysc—total cost | $277 094 | $74 742 |
| Wage loss and other costs related to taking care of sick childd—total cost | $33 589 | $12 985 |
| Total for all costs | $454 647 | $291 426 |
| ICER per child insurede | — | –$6045.22 |
| ICER per each percent increase in children insurede | — | –$4185.15 |
Intervention parents (98.4%) experienced a total of 75 missed work days due to their child’s illness. —, N/A.
N = 39 ED visits for controls and 40 for the intervention group.
N = 2 hospitalizations for controls and 2 for the intervention group.
N = 4 ICU stays for controls and 1 for the intervention group.
N = 112 control parents (98.2%) experienced a total of 83.5 missed work days due to their child’s illness; N = 121
A negative value represents cost savings per year.
Discussion
In the Kids’ HELP trial, the PM intervention was more effective than traditional outreach/enrollment in insuring uninsured minority children, resulting in 95% of children obtaining insurance, versus 68% of controls. The PM intervention also insured children faster, and was more effective in renewing coverage, improving access to medical and dental care, reducing out-of-pocket costs, achieving parental satisfaction and quality of care, and sustaining insurance after intervention cessation. This is the first RCT, to our knowledge, to evaluate the effectiveness of PMs in insuring uninsured children. Two systematic reviews31,32 revealed only one previous RCT (by our team) of an intervention to insure uninsured children, which revealed that community-based case managers were more effective than traditional outreach/enrollment in insuring uninsured Latino children. This RCT, in contrast to Kids’ HELP, used case managers, focused only on Latinos, and did not examine health, health care outcomes, or cost-effectiveness.12
PMs were relatively inexpensive, at $53.05 per child per month, and saved $6045.22 per year per child insured. The relatively low mean monthly costs of approximately $33 for PM stipends and $16 for personnel to screen, identify, and assign uninsured children to PMs indicate that the costs of implementing Kids’ HELP on a larger scale would be reasonable. The relatively low overall cost of $53 per month for Kids’ HELP may also be attractive to hospitals and health systems, given that the higher rate of insuring previously uninsured children in Kids’ HELP has the potential to translate into Medicaid/CHIP revenue for ED visits and hospitalizations, rather than write-offs of charity-care losses.
One could hypothesize that cost savings might have accrued for Kids’ HELP children via greater access to early, timely outpatient care and medical homes, thereby potentially reducing the number, duration, and severity of preventable illnesses and concomitant sick visits, ED visits, and hospitalizations, but further research would be needed to confirm this. Although the cost findings are suggestive, given that additional research is needed on the effectiveness of the intervention in other settings and populations, the study results would seem to indicate that implementing PM interventions in health plans, state Medicaid and CHIP programs, or nationally might potentially result in considerable cost savings. For example, hypothesizing PM interventions might have a similar efficacy when implemented on a larger scale and in other regions, national implementation of Kids’ HELP could possibly save $12.1 to $14.1 billion (3 700 000–4 300 000 [uninsured US children eligible for but not enrolled in Medicaid/CHIP2–5] × 0.57 [proportion of uninsured Latino or African-American children7] × $6045.22 [savings per child insured by Kids’ HELP] × 0.95 [proportion of PM group children obtaining insurance]). Conditionally assuming that PMs could also potentially be effective for uninsured children of all races/ethnicities, similar calculations suggest that national implementation of PM interventions to insure all Medicaid/CHIP-eligible uninsured children might possibly save $21.2 to $24.7 billion.
PMs were more effective in improving access to primary, dental, and specialty care; reducing unmet needs; achieving parental satisfaction with care; and sustaining long-term coverage. We hypothesize that these benefits resulted from PM training specifically emphasizing educating parents on the importance of medical homes, how to obtain children’s dental and specialty care, taking an active role in pediatric care, and how to maintain and renew Medicaid/CHIP.
PMs resulted in lower out-of-pocket costs for doctor and sick visits, higher well-child care quality ratings, and higher levels of parental satisfaction and respect from children’s physicians. We hypothesize these benefits accrued from a combination of PM children being more likely to have medical homes (evidenced by their greater likelihood of having a PCP, usual source of preventive care, and same source of sick and preventive care) and the ability to get immediate care from the PCP, along with PM training emphasizing educating parents on the importance of medical homes and taking an active role in pediatric care. Higher out-of-pocket costs for control parents may also have occurred because their children were less likely to be insured, thereby requiring parents to pay larger out-of-pocket shares for doctor and sick visits for their uninsured children.
Certain study limitations should be noted. This trial was conducted in urban populations of Latinos and African-Americans in Texas, so findings may not necessarily generalize to non-urban populations or other regions or racial/ethnic groups. Parental-reported service use was not verified via health records, although research documents high correlations between parental reports and health records.30 Some cost differences were driven by high costs of ICU care, and only 4 controls and 1 PM group child had ICU admissions, so caution in interpretation is warranted. The study protocol may have resulted in control children attaining higher rates of insurance coverage than in the general population in non-research settings, as monthly contacts by research staff to assess outcomes may have regularly prompted parents to seek insurance for their children.
The results suggest several potential implications for policy and practice. First, the largely passive mechanisms of traditional Medicaid/CHIP outreach and enrollment (such as media and public transportation advertisements and posting toll-free telephone numbers) appear to be less effective than a PM intervention that is interactive, provides social support, connects parents of uninsured children with other parents who successfully insured their own children and come from the same neighborhoods and similar racial/ethnic backgrounds, and includes PM training on providing assistance with obtaining pediatric care and addressing social determinants of health. Second, evidence suggests that PMs result in multiple benefits, including insuring more uninsured children, reducing families’ out-of-pocket costs of care, employing parents seeking work, increasing earnings in low-income minority communities, and saving money. Third, PMs and analogous peer mentors for adults might prove to be highly cost-effective interventions for reducing or eliminating insurance disparities and insuring all Americans.
Conclusions
PMs were more effective than traditional methods in insuring uninsured minority children; obtaining insurance faster; renewing coverage; improving access to primary, dental, and specialty care; reducing unmet needs and out-of-pocket costs; achieving parental satisfaction and care quality; and sustaining long-term coverage. The PM intervention was inexpensive, and saved $6045.22 per insured child. These findings suggest that PMs and analogous peer mentors for adults might prove to be highly cost-effective interventions for reducing or eliminating insurance disparities and insuring all Americans.
Acknowledgments
We thank the Kids’ HELP participants, parent mentors, and community partners for their valuable contributions.
Glossary
- CEA
cost-effectiveness analysis
- CHIP
Children’s Health Insurance Program
- CI
confidence interval
- ED
emergency department
- HHSC
Texas Health and Human Services Commission
- ICER
incremental cost-effectiveness ratio
- Kids’ HELP
Kids’ Health Insurance by Educating Lots of Parents
- PCP
primary care provider
- PM
parent mentors
- RCT
randomized, controlled trial
Footnotes
Dr Flores conceptualized and designed the study; designed the data-collection instruments; drafted the initial manuscript; provided administrative, technical, and material support; provided study supervision; and reviewed and revised the manuscript. Drs Lin, Walker, and Currie conceptualized and designed the study, designed the data-collection instruments, drafted the initial manuscript, and reviewed and revised the manuscript. Drs Lee and Allgeyer, Misters Fierro, Portillo, and Massey, and Ms Henry participated in the acquisition, analysis, and interpretation of data; drafted the initial manuscript; and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted.
The funding organization had no role in study design; data collection, analysis, or interpretation; or writing of the report. The corresponding author had full access to all study data and final responsibility for the decision to submit for publication. The views expressed in this article are solely those of the authors and do not represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01264718).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This study was funded by grant R01HD066219 (principal investigator: Dr Flores) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Smith JC, Medalia C; US Census Bureau Health insurance coverage in the United States: 2013. Washington, DC: US Government Printing Office, 2014 (Current Population Reports, P60-250). Available at: www.census.gov/content/dam/Census/library/publications/2014/demo/p60-250.pdf. Accessed June 9, 2015
- 2.Hudson JL, Selden TM. Children’s eligibility and coverage: recent trends and a look ahead. Health Aff (Millwood). 2007;26(5):w618–w629 [DOI] [PubMed] [Google Scholar]
- 3.Horner D, Guyer J, Mann C, Alker J. The Children’s Health Insurance Program Reauthorization Act of 2009. Washington, DC: Center for Children and Families, Georgetown University Health Policy Institute; 2009 [Google Scholar]
- 4.American Academy of Pediatrics Fact sheet. Children’s health insurance. Available at: www.aap.org/research/factsheet.pdf. Accessed June 10, 2015
- 5.Kenney GM, Lynch V, Haley JM, Huntress M, Resnick D, Coyer C. Gains for children: increased participation in Medicaid and CHIP in 2009. Washington, DC: Urban Institute; 2011. Available at: www.urban.org/UploadedPDF/412379-Gains-for-Children.pdf. Accessed June 10, 2015 [Google Scholar]
- 6.Holahan J, Dubay L, Kenney GM. Which children are still uninsured and why. Future Child. 2003;13(1):55–79 [PubMed] [Google Scholar]
- 7.US Census Bureau, Current Population Survey Table HI08. Health insurance coverage status and type of coverage by selected characteristics for children under 18 (all children): 2013. Available at: www.census.gov/hhes/www/cpstables/032014/health/toc.htm. Accessed June 9, 2015
- 8.Flores G, Bridon C, Torres S, et al. Improving asthma outcomes in minority children: a randomized, controlled trial of parent mentors. Pediatrics. 2009;124(6):1522–1532 [DOI] [PubMed] [Google Scholar]
- 9.Flores G, Walker C, Lin H, et al. Design, methods, and baseline characteristics of the Kids’ Health Insurance by Educating Lots of Parents (Kids’ HELP) trial: a randomized, controlled trial of the effectiveness of parent mentors in insuring uninsured minority children. Contemp Clin Trials. 2015;40:124–137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.CHIP/Children’s Medicaid Can I Get It? Austin, TX: Texas Health and Human Services Commission, 2015. Available at: http://chipmedicaid.org/en/Can-I-Get-It. Accessed May 6, 2015
- 11.The J. McDonald Williams Institute Research Arm of the Foundation for Community Empowerment The Cost of Not Addressing Concentrated Poverty: How Much Can Dallas Afford to Pay? Dallas, TX: Foundation for Community Empowerment; 2006 [Google Scholar]
- 12.Flores G, Abreu M, Chaisson CE, et al. A randomized, controlled trial of the effectiveness of community-based case management in insuring uninsured Latino children. Pediatrics. 2005;116(6):1433–1441 [DOI] [PubMed] [Google Scholar]
- 13.Flores G, Walker C, Lin H, et al. A successful program for training parent mentors to provide assistance with obtaining health insurance for uninsured children. Acad Pediatr. 2015;15(3):275–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Texas Health and Human Services Commission Children’s health insurance outreach and education campaign (news release). Austin, TX: Texas Health and Human Services Commission; April 11, 2006
- 15.Health Resources and Services Administration, Maternal and Child Health Bureau, Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. National Survey of Children’s Health, 2003. Interview sections 1-11. Atlanta, GA: Centers for Disease Control and Prevention. Available at: www.cdc.gov/nchs/data/slaits/NSCH_Questionnaire.pdf. Accessed June 10, 2015
- 16.Magee JC, Ritterband LM, Thorndike FP, Cox DJ, Borowitz SM. Exploring the relationship between parental worry about their children’s health and usage of an internet intervention for pediatric encopresis. J Pediatr Psychol. 2009;34(5):530–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39(8):800–812 [DOI] [PubMed] [Google Scholar]
- 18.Szilagyi PG, Zwanziger J, Rodewald LE, et al. Evaluation of a state health insurance program for low-income children: implications for state child health insurance programs. Pediatrics. 2000;105(2):363–371 [DOI] [PubMed] [Google Scholar]
- 19.Moreno L, Hoag SD. Covering the uninsured through TennCare: does it make a difference? Health Aff (Millwood). 2001;20(1):231–239 [DOI] [PubMed] [Google Scholar]
- 20.Szilagyi PG, Dick AW, Klein JD, Shone LP, Zwanziger J, McInerny T. Improved access and quality of care after enrollment in the New York State Children’s Health Insurance Program (SCHIP). Pediatrics. 2004;113(5). Available at: www.pediatrics.org/cgi/content/full/113/5/e395 [DOI] [PubMed] [Google Scholar]
- 21.Kempe A, Beaty BL, Crane LA, et al. Changes in access, utilization, and quality of care after enrollment into a state child health insurance plan. Pediatrics. 2005;115(2). Available at: www.pediatrics.org/cgi/content/full/115/2/364–371 [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention SLAITS National Survey of Children with Special Health Care Needs. Atlanta, GA: Centers for Disease Control and Prevention. Available at: www.cdc.gov/nchs/data/slaits/NSCSHCN%20Questionnaire%20(website)1.pdf. Accessed June 10, 2015
- 23.Holl JL, Szilagyi PG, Rodewald LE, et al. Evaluation of New York State’s Child Health Plus: access, utilization, quality of health care, and health status. Pediatrics. 2000;105(3 suppl E):711–718 [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention SLAITS: The State and Local Area Integrated Telephone Survey. National Survey of Early Childhood Health. Appendix III. Atlanta, GA: Centers for Disease Control and Prevention. Available at: www.cdc.gov/nchs/data/slaits/survey_sech00.pdf. Accessed June 10, 2015
- 25.Agency for Healthcare Research and Quality CAHPS Health Plan Survey 4.0. Version: Child Medicaid Questionnaire. Rockville, MD: Agency for Healthcare Research and Quality; 2008 [Google Scholar]
- 26.Lave JR, Keane CR, Lin CJ, Ricci EM, Amersbach G, LaVallee CP. Impact of a children’s health insurance program on newly enrolled children. JAMA. 1998;279(22):1820–1825 [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention Draft 2009 NHIS questionnaire–sample child. Atlanta, GA: Centers for Disease Control and Prevention, 2009. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2009/english/qchild.pdf. Accessed June 10, 2015
- 28.Gold M. Panel on cost-effectiveness in health and medicine. Med Care. 1996;34(suppl 12):DS197–DS199 [PubMed] [Google Scholar]
- 29.Gold MR, Siegel JE, Russell LB, Weinstein MC, eds. Cost-Effectiveness in Health and Medicine. New York, NY: Oxford University Press; 1996 [Google Scholar]
- 30.Noyes K, Bajorska A, Fisher S, Sauer J, Fagnano M, Halterman JS. Cost-effectiveness of the School-Based Asthma Therapy (SBAT) program. Pediatrics. 2013;131(3). Available at: www.pediatrics.org/cgi/content/full/131/3/e709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meng Q, Yuan B, Jia L, Wang J, Garner P. Outreach strategies for expanding health insurance coverage in children. Cochrane Database Syst Rev. 2010; (8):CD008194. [DOI] [PubMed] [Google Scholar]
- 32.Jia L, Yuan B, Huang F, Lu Y, Garner P, Meng Q. Strategies for expanding health insurance coverage in vulnerable populations. Cochrane Database Syst Rev. 2014;11:CD008194 10.1002/14651858.CD008194.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]