Abstract
BACKGROUND:
Adults with childhood-onset epilepsy experience poorer adult social outcomes than their peers. The relative roles of seizures over time versus learning and psychiatric problems are unclear.
METHODS:
We examined independent influences of psychiatric and learning disorders and of seizure course in 241 young adults (22–35 years old) with uncomplicated epilepsy in a longitudinal community-based cohort study. Social outcomes were ascertained throughout the study. A history of psychiatric and learning problems was ascertained ∼9 years after study entry. Seizure course was: “Excellent,” no seizures after the first year, in complete remission at last contact (N = 95, 39%); “Good,” seizures occurred 1 to 5 years after diagnosis, in complete remission at last contact (N = 56, 23%); “Fluctuating,” more complicated trajectories, but never pharmacoresistant (N = 70, 29%); “Pharmacoresistant,” long-term pharmacoresistant (N = 20, 8%). Multiple logistic regression was used to identify contributors to each social outcome.
RESULTS:
Better seizure course predicted college completion, being either employed or pursuing a degree, and driving, but was not substantially associated with other social outcomes. Poorer seizure course was associated with a greater likelihood of having offspring, particularly in women without partners. Learning problems, psychiatric disorders, or both negatively influenced all but 2 of the social outcomes.
CONCLUSIONS:
In young adults with uncomplicated epilepsy, the course of seizures contributed primarily to education, employment, and driving. A history of learning problems and psychiatric disorders adversely influenced most adult outcomes. These findings identify potential reasons for vocational and social difficulties encountered by young adults with childhood epilepsy and areas to target for counseling and transition planning.
What’s Known on This Subject:
Previous studies suggest a lasting pervasive negative impact on social outcomes in adults with onset of epilepsy in childhood. Reasons were unclear.
What This Study Adds:
Poorer seizure course as well as history of psychiatric and learning disorders independently influence social outcomes in adults with childhood epilepsy who have otherwise uncomplicated (“normal”) neurologic presentations.
Several longitudinal studies of children with epilepsy have demonstrated poorer than expected prognosis for attaining benchmark social outcomes in adulthood. These outcomes include completing secondary education, obtaining a college degree, employment, marriage, and driving.1–5 Some of this is due to individuals whose epilepsies occur in association with brain insults and other conditions, particularly when associated with intellectual disability.3,5–7 Evidence from these studies, however, still suggests that young people with uncomplicated epilepsy fail to achieve the same levels of success in life as their peers. In children with uncomplicated epilepsy, there is also ample evidence demonstrating an increased level of subtle cognitive as well as psychiatric and behavioral problems relative to healthy controls, which could also influence adult outcomes.8–13 The respective impacts of seizure course versus learning and psychiatric problems on adult outcomes have not been distinguished. Understanding what places a child with epilepsy at risk for poorer outcomes in adulthood might contribute to management of childhood epilepsy, determining the need for early educational and psychiatric/psychological services, and planning pediatric to adult transition and transfer of care.
In young adults studied from the initial diagnosis of uncomplicated childhood epilepsy, we examined the relation of adult social outcomes to the course of seizure control as well as psychiatric disorders and learning problems.
Methods
Data came from a prospective, longitudinal, community-based study of children with newly diagnosed epilepsy recruited from the office of 16 of the 17 child neurologists practicing in Connecticut (1993–1997). Eligible individuals had onset of epilepsy between 0 and 15 years of age and received their initial diagnosis of epilepsy by participating physicians (ie, they were not referred for other concerns after diagnosis and treatment elsewhere).14 Participants were followed until the study’s conclusion in 2014. At ∼9 and ∼15 years after initial recruitment, they participated in extensive reassessments involving structured interviews and several standardized instruments. Yearly, we updated information about education, living arrangements, driving, and employment. At the exit interview (1–5 years after the 15-year interview), social outcomes were updated with the same questions from the 15-year interview.
Parents originally provided written, informed consent. Children who were old enough provided oral or written assent as appropriate. As participants attained majority, they were recruited to participate as young adults and provided written consent. Approval for this study was obtained from the institutional review boards of all institutions involved in this research.
The analytic sample was limited to those with uncomplicated epilepsy presentations (normal neurologic examination, normal brain imaging, absence of intellectual disability, and no history of insults accounting for the epilepsy) to allow focus on young adults who, apart from epilepsy, did not have any other neurologic conditions that might independently affect social outcomes. In addition, to target long-term outcomes in young adults, only those followed ≥10 years and who were ≥22 years old when social outcomes were last assessed were included.
Seizure Course
Detailed seizure and antiseizure medication (ASM) histories were obtained via phone contact with the family every 3 to 4 months and medical records were reviewed periodically. From these data, periods of remission, relapse, seizure occurrence, and time off ASMs were prospectively determined.
Based on a previous analysis,15 we developed a 4-category composite seizure course variable: (1) “Excellent” meant no seizures after the first year after diagnosis and in complete remission when social outcomes were ascertained. Complete remission required being both seizure-free and ASM-free16 for 5 years and corresponds closely to the “smooth sailing” epilepsy previously described.17 (2) “Good” identified those with seizures beyond the first year and up through 5 years after diagnosis, but no further seizures since that time and in complete remission at last contact. (3) “Fluctuating” included more complicated trajectories with seizures occurring >5 years after diagnosis, often with multiple periods of remission and relapse, and rarely in complete remission at last contact, but never meeting the criteria for pharmacoresistance (failure of ≥2 ASM trials18). (4) “Pharmacoresistant” referred to those who were long-term pharmacoresistant.
Psychiatric and Learning Problems
Psychiatric diagnoses and learning problems were identified ∼9 years after the initial epilepsy diagnosis and were based on parent interviews and medical record reviews.19,20 Psychiatric disorders were analyzed in groups for externalizing disorders (attention-deficit/hyperactivity, conduct, and oppositional-defiant) and internalizing disorders (depression, anxiety, obsessive-compulsive, and bipolar). Learning problems, including developmental delay, language problems, and dyslexia, were also grouped into a single dichotomous variable.
Young Adult Social Outcomes
Social outcomes included living and family arrangements (living on one’s own or in a dorm versus with parents, ever married or with a partner, and having any children), education (high school graduate, college graduate, or currently in a degree program), employment (employed ≥20 hours/week), having a driver’s license, and trouble with law enforcement. Because being in a degree program and being employed represent comparable forms of productivity for young adults, we created a composite variable, “productive engagement”: either employed ≥20 hours/week or in a degree program versus neither.
Parent Education
As a proxy for socioeconomic status, we included an indicator for whether at least 1 parent had completed college as assessed at the time of initial study recruitment (1993–1997).
Analysis
Bivariate analyses first examined associations of social outcomes with seizure outcomes and histories of psychiatric disorders and learning problems. χ2 tests and Mantel–Hansel χ2 tests for trend were used. Seizure course was tested against each social outcome. We also compared categorical and ordinal representations of the seizure variable. For each outcome, test for lack of fit of the monotonic trend versus the categorical representation was accomplished by determining the difference in the model χ2s with respect to the change in degrees of freedom (df) for each pair of models (1 with the categorical on 3 df and 1 with the monotonic with 1 df). When there was no significant lack of fit of the ordinal versus categorical representation of seizure outcome, we used the Aikake Information Criterion (AIC) to select the better model based on the lower model AIC.21
With multiple logistic regression analyses, each social outcome was modeled as a function of the seizure course and history of psychiatric disorders and learning problems. Adjustment was made for age, gender, and parent education when these significantly contributed to an outcome. Because the odds ratio (OR) exaggerates (away from the null value) the relative risk for common outcomes, we also obtained point estimates of the relative risk by using proportional hazards models.22 All P values are 2-tailed. Analyses were done in SAS 9.3 (SAS Institute, Inc, Cary, NC).
Results
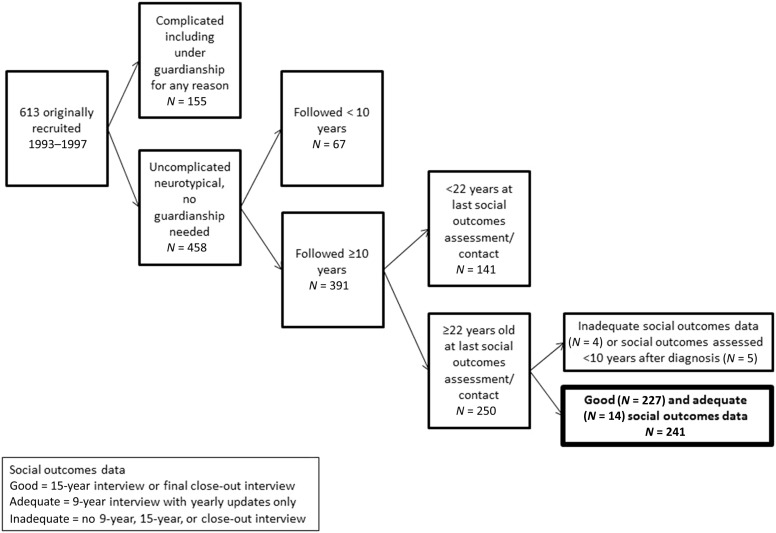
Of the original 613 participants, 458 had uncomplicated presentations of whom 391 (82%) were followed ≥10 years. After exclusions, 241 were eligible for analysis (Fig 1). The median length of follow-up for social outcomes was 18 years (interquartile range 17–19 years).
FIGURE 1.
Derivation of the study sample.
The sample consisted of 127 (52.7%) women and 114 (47.3%) men. The average age at first seizure was 7.1 years (SD = 3.4) and at time of assessment was 26.1 years (SD = 3.3). The epilepsy diagnoses were determined at initial study entry and revised as additional information required.14,23 For this analysis, epilepsies were grouped as nonsyndromic epilepsies with focal features (N = 99, 41.1%), generalized genetic epilepsies (N = 87, 36.1%, primarily childhood absence, juvenile absence, and juvenile myoclonic epilepsy), focal self-limited epilepsy (N = 43, 17.8%, mostly benign epilepsy with centrotemporal spikes), and other, mostly uncharacterized, epilepsies (N = 12, 4.9%).
Seizure course was: excellent, N = 95 (39.4%); good, N = 56 (23.2%); fluctuating, N = 70 (29.1%); and pharmacoresistant, N = 20 (8.3%).
Age, Gender, and Parent’s Education Versus Social Outcomes
Women were more likely than men to have a partner and children and to have graduated from college. Men were more likely than women to have had some trouble with the law (21.1% versus 8.7%, P = .006; Supplemental Table 4). Living on one’s own, having a partner or children, and graduation from college were strongly correlated with older age at the time that social outcome data were collected (Supplemental Table 5). These outcomes were correlated with epilepsy onset age. Because everyone was followed for roughly the same time, age at onset and at last contact were strongly correlated (r = 0.80, P < .0001); any independent effects of the 2 could not be distinguished. Having a college graduate parent was associated with a modestly lower likelihood of still living at home and having children. However, it was strongly associated with receiving a college degree (65.7% vs 25.0%, P < .0001) and being productively engaged (93.3% vs 77.9%, P = .001; Supplemental Table 6).
Seizure Course and Social Outcomes
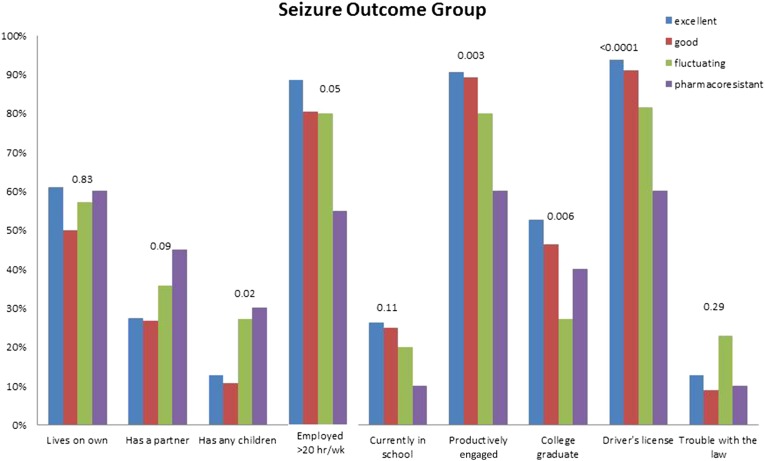
For bivariate analyses, seizure course was a strong predictor of finishing college (P = .006), being productively engaged (P = .009), and having a driver’s license (P < .0001) (Fig 2, Supplemental Table 7). Being employed and being in a degree program were negatively associated with each other; 17.7% of those who were employed were in school versus 40.4% of those who were unemployed (P = .0004). Living independently of parents, living with a partner, and having trouble with law enforcement were not associated with seizure course. Unexpectedly, a poorer seizure course was associated with a greater likelihood of having offspring (P = .007). This led to an exploratory analysis described below. For all comparisons, the monotonic trend provided adequate fit to the data and its AIC was also lower (better) than for the categorical representation of seizure course.
FIGURE 2.
Association between seizure course and each of the benchmark social outcomes studied.
Learning Problems and Social Outcomes
Participants with a history of learning problems compared to those without were less likely to be employed (63.2% vs 80.1%, P = .009), to have completed college (22.4% vs 49.2%, P = .0003), to be productively engaged (74.1% vs 88%, P = .01), or to have a driver’s license (74.1% vs 90.7%, P = .001) (Table 1). A history of learning disorders was not associated with living on one’s own, having a partner, having children, or having had trouble with the law.
TABLE 1.
Association Between Young Adult Outcomes and Learning Problems That Were Ascertained at the 9-y Follow-up Assessment
| Learning Problems Ascertained at 9-y Assessment | |||
|---|---|---|---|
| None (N = 183) | Present (N = 58) | P Value | |
| Living arrangements | |||
| Lives with parents | 75 (41.0%) | 27 (46.6%) | .45 |
| Lives on own or in dorm | 108 (59.0%) | 31 (53.5%) | |
| Ever married or lives with partner | |||
| No | 127 (69.4%) | 39 (67.2%) | .76 |
| Yes | 56 (30.6%) | 19 (32.8%) | |
| Any children | |||
| No | 153 (83.6%) | 45 (77.6%) | .30 |
| Yes | 30 (16.4%) | 13 (22.4%) | |
| Employed ≥20 h/wka | |||
| No | 36 (19.9) | 21 (36.8) | .009 |
| Yes | 145 (80.1) | 36 (63.2) | |
| Graduated high school/GEDb | |||
| No | 3 (1.6%) | 1 (1.7%) | .96 |
| Yes | 180 (98.4%) | 57 (98.3%) | |
| Graduated from a 4-y college | |||
| No | 93 (50.8%) | 45 (77.6%) | .0003 |
| Yes | 90 (49.2%) | 13 (22.4%) | |
| Currently pursuing a degree in college, graduate school, or technical training | |||
| No | 142 (77.6%) | 44 (75.9%) | .78 |
| Yes | 41 (22.4%) | 14 (24.1%) | |
| Productively engaged | |||
| Neither in a degree program nor employed ≥20 h/wk | 22 (12.0%) | 15 (25.9%) | .01 |
| Either in a degree program or employed ≥20 h/wk* | 161 (88.0%) | 43 (74.1%) | |
| Driver’s license | |||
| No | 15 (8.2%) | 15 (25.9%) | .0004 |
| Yes | 168 (91.8%) | 43 (74.1%) | |
| Any encounters with law enforcement | |||
| No | 159 (86.9%) | 47 (81.0%) | .27 |
| Yes | 24 (13.1%) | 11 (19.0%) | |
Three missing number of hours per week.
GED, Graduate Equivalency Degree.
Psychiatric Disorders and Social Outcomes
Differences between those with and without a history of psychiatric disorders were seen for completion of college (26.9% vs 48.6%, P = .002) and encounters with law enforcement (25.4% vs 10.3%, P = .003) (Table 2). The associations for these 2 social outcomes were especially strong for externalizing disorders. People with versus people without internalizing disorders were more likely to have offspring (P = .008) and less likely to be employed (P = .02). Psychiatric disorders (overall and by type) were not associated with living and family arrangements, or having a driver’s license.
TABLE 2.
Association Between Psychiatric Diagnoses as Ascertained at the 9-y Interview With Young Adult Social Outcomes
| Psychiatric Disorders Ascertained at the 9-y Assessment | ||||
|---|---|---|---|---|
| No Reported Psychiatric Disorders (N = 175)a | Internalizing Disorders (N = 41) | Externalizing Disorders (N = 43) | Any Psychiatric Disorder (N = 67)b | |
| Living arrangements | ||||
| Lives with parents | 68 (39.4) | 16 (39.0%) | 24 (55.8%) | 34 (50.8%) |
| Lives on own or in dorm | 106 (60.6%) | 25 (61.0%) | 19 (44.2%) | 33 (49.3%) |
| P value | .96 | .05 | .10 | |
| Ever married or lives with partner | ||||
| No | 11 (68.08%) | 24 (58.5%) | 33 (76.7%) | 48 (71.6%) |
| Yes | 56 (32.0%) | 17 (41.5%) | 10 (23.3%) | 19 (28.4%) |
| P value | .25 | .26 | .57 | |
| Any children | ||||
| No | 147 (84.0%) | 27 (65.9%) | 34 (79.1%) | 52 (77.6%) |
| Yes | 28 (16.0%) | 14 (34.2%) | 9 (20.9%) | 15 (22.4%) |
| P value | .008 | .44 | .25 | |
| Employed ≥20 h/wk | ||||
| No | 37 (21.4) | 16 (39.0) | 11 (26.2) | 20 (30.3) |
| Yes | 136 (78.6) | 25 (61.0) | 31 (73.8) | 46 (69.7) |
| P value | .02 | .50 | .15 | |
| Graduated high school/GEDc | ||||
| No | 2 (1.1%) | 1 (2.4%) | 1 (2.3%) | 2 (3.0%) |
| Yes | 173 (98.9%) | 40 (97.6%) | 42 (97.7%) | 65 (97.0%) |
| P value | .52 | .55 | .32 | |
| Graduated from a 4-y college | ||||
| No | 90(51.4%) | 28 (68.3%) | 35 (81.4%) | 49 (73.1%) |
| Yes | 85 (48.6%) | 13 (31.7%) | 8 (18.6%) | 18 (26.9%) |
| P value | .05 | .0004 | .002 | |
| Currently pursuing a degree in college, graduate school, or technical training | ||||
| No | 134 (76.6%) | 33 (80.5%) | 33 (76.7%) | 52 (77.6%) |
| Yes | 40 (23.4%) | 8 (19.5%) | 10 (23.3%) | 15 (22.4%) |
| P value | .59 | .98 | .92 | |
| Productively engaged | ||||
| Neither in a degree program nor employed ≥20 h/week | 23 (13.1%) | 11 (26.8%) | 7 (16.3%) | 14 (20.9%) |
| Either in a degree program or employed ≥20 h/week | 152 (86.9%) | 30 (73.2%) | 36 (83.7%) | 53 (79.1%) |
| P value | .03 | .59 | .14 | |
| Driver’s license | ||||
| No | 19 (10.9%) | 5 (12.2%) | 9 (20.9%) | 12 (17.9%) |
| Yes | 156 (89.1%) | 36 (87.8%) | 34 (79.1%) | 55 (82.1%) |
| P value | .81 | .08 | .11 | |
| Any encounters with law enforcement | ||||
| No | 157(89.7%) | 32 (78.1%) | 29 (67.4%) | 50 (74.6%) |
| Yes | 18 (10.3%) | 9 (22.0%) | 14 (32.6%) | 17 (25.4%) |
| P value | .04 | .0002 | .003 | |
Reference group to which each of the other columns is compared.
These participants are also included in the groups for internalizing and for externalizing disorders.
GED, Graduate Equivalency Degree (in the United States, an alternative to a high school diploma).
Multivariable Analyses: Independent Prognostic Factors for Social Outcomes
In a series of logistic regression analyses, each social outcome was modeled as a function of the seizure course, learning problems, and psychiatric disorders (overall, internalizing, and externalizing) (Table 3). Adjustment was made for age, gender, and parent education when they significantly contributed to prediction of a specific outcome.
TABLE 3.
Results of Multiple Logistic Regression Analyses to Identify Independent Predictors of Key Social Outcomes
| Predictive Factors | OR (95% CI) | Risk Ratioa | P Valueb |
|---|---|---|---|
| Living and family arrangement social outcomes | |||
| Living on one’s own including in a dormitoryc,d | |||
| Any psychiatric disorder | 0.47 (0.25–0.88) | 0.51 | .02 |
| Ever married or lives with a partnerc,e | |||
| No predictors | |||
| Has childrend,e | |||
| Worse seizure outcome | 1.46 (1.03–2.06)f | 1.32 | .03 |
| History of internalizing disorders | 2.89 (1.26–6.64) | 2.05 | .01 |
| Employment and educational attainment outcomes | |||
| Employed ≥20 h/weekc | |||
| Learning problems | 0.43 (0.22–0.82) | 0.55 | .01 |
| Currently pursuing a post–high school degree or certificationc | |||
| No predictors | |||
| Either employed ≥20 h/wk or actively pursuing education beyond high schoold | |||
| Worse seizure outcome | 0.57 (0.39–0.83) | 0.92 | .004 |
| Learning problems | 0.45 (0.21–0.98) | 0.87 | .04 |
| Graduated from 4-y collegec,d,e | |||
| Worse seizure outcome | 0.62 (0.45–0.86) | 0.84 | .004 |
| Learning problems | 0.35 (0.15–0.81) | 0.59 | .01 |
| Any psychiatric disorder | 0.32 (0.15–0.71) | 0.60 | .005 |
| Other outcomes | |||
| Has a driver’s licensec | |||
| Worse seizure outcome | 0.42 (0.27–0.66) | 0.91 | .0002 |
| Learning disorder | 0.35 (0.15–0.78) | 0.84 | .01 |
| Encounters with law enforcemente | |||
| Externalizing disorders | 3.27 (1.45–7.35) | 2.51 | .01 |
CI, confidence interval.
Estimates are adjusted for
Based on approximations using proportional hazards modeling.
P values are based on logistic regression.
age,
parental education, and
gender, and where these were statistically significant predictors of a specific outcome.
A secondary analysis revealed this association was almost completely restricted to women who did not have a partner.
Living and Family Arrangements
People with a history of psychiatric disorders were less likely to be living on their own (OR = 0.47, P = .02). Having children was seen more often in those with a history of internalizing disorders (OR= 2.89, P = .01) and was also independently increased in association with poor seizure course (OR = 1.46 for each successively poorer seizure outcome category, P = .03). No factor considered was associated with having a partner. The association between seizure outcome and having offspring was examined more carefully by stratifying on gender and having a partner. Almost all of the effect was due to woman who did not have partners (from best to worst seizure outcome group, 2.9%, 10.5%, 27.8%, and 40% of women without partners had children, P = .002 for trend). Similar trends were absent in men and in women with partners.
Employment and Education
Worse seizure course and learning problems independently contributed to a lower likelihood of college completion and productive engagement. Psychiatric disorders (OR = 0.32, P = .005) were associated with a lower chance of completing college. Learning problems were also associated with a lower chance of being employed (OR = 0.43, P = .01).
Driving and Trouble With Law Enforcement
Worse seizure course (P = .0002) and learning problems (OR = 0.35, P = .01) were each independently associated with a lower likelihood of driving. Externalizing disorders were the only predictor of trouble with law enforcement (OR = 3.27, P = .01).
Discussion
Earlier studies suggest something beyond seizures affects success in young adulthood.1,3,4,24–26 Epilepsy is often associated with neurologic conditions and deficits that themselves impact adult outcomes. We therefore focused on young adults with uncomplicated childhood epilepsy and examined the unique contributions of seizure course over 10 to 20 years, learning problems, and psychiatric disorders to achieving social outcomes. Although some important outcomes are influenced by seizure control, a history of learning problems and psychiatric disorders had more pervasive influences.
The employment and educational outcomes examined are key to lifelong success and independence. Seizure course influences completion of college, employment, and driving, which itself impacts employment. The independent role of seizure course over time in influencing these types of outcomes has not been fully appreciated previously, but may explain why people who had benign epilepsy with centrotemporal spikes, an epilepsy that usually has a “smooth-sailing” course,15 have better social outcomes than young adults with other forms of uncomplicated childhood epilepsy.25–27
Notably, seizure course was not associated with living independently of parents, having a partner, or trouble with law enforcement. The unexpected finding concerning poorer seizure course and offspring may reflect several factors. Anecdotally, some young women reported that having children gave them a feeling of being successful at something. This fits well with our exploratory analysis showing that virtually all of the association was in young women without partners. It would require separate, targeted research efforts to understand this finding better in contemporary society.
Beyond seizures, learning problems and psychiatric disorders influenced social outcomes. Learning problems are common in school-aged children; however, they occur more often in children with uncomplicated epilepsy than in healthy peer controls.9,11–13 In fact, before diagnosis of epilepsy11,28 or shortly thereafter,9 children with uncomplicated epilepsy are already more likely to be receiving special education services compared with similar-aged controls. Before initiation of ASMs, adults with newly diagnosed seizures display evidence of relatively poorer memory function and processing speed compared with healthy controls.29 Studies focused on specific forms of childhood epilepsy also implicate verbal processing and attentional networks as being subtly altered, perhaps explaining the relative impairment in those functions.30,31 In fact, learning problems were discussed as possibly contributing to poorer outcomes in 1 study.32 They were also associated with adverse social outcomes in the Canadian cohort, although receipt of special education services was considered a poor outcome in that study.1 Independent of seizure course, learning problems appear to impact several important adult outcomes.
The relative strengths and weaknesses of this study must be considered. Our cohort had an average age of 26 years when social outcomes were assessed. This may be too young for outcomes such as marriage and having children. Nonetheless, our results are relevant to young adults in their twenties, and we suspect that the trends with outcomes at this age will track with later outcomes.
Of families approached to participate in the initial study, ∼80% agreed.14 Of subjects followed ≥10 years and who were ≥22 years old at the end of the study, 74% were included in these analyses. Although this is good retention for such a long-term study, it leaves room for selective attrition, which could affect our overall assessment of these outcomes. For example, almost all individuals in our study sample completed secondary education. This is high compared with Connecticut overall, where graduation rate percentages are currently in the low- to mid-80s.33 Our sample excluded those with the most severe disabilities who might be less likely to graduate. We do not have graduation rates for individuals who, like our cases, are free of neurologic or intellectual disability; we suspect it is higher than average. Notably, other studies found no difference in completing secondary education in young people with epilepsy but without neurologic disability versus population controls.2,3
In the 1990s and 2000s, Connecticut had a high penetration of special education services. We cannot address the role that the high level of special resources received by young people in this cohort may have played in their social successes. Our findings should not be used to argue against the need for these additional resources for young people with epilepsy. In addition, there have been major changes in societal attitudes toward individuals with extra challenges. In the United States, we marked the 25th anniversary of the Americans with Disabilities Act, which changed opportunities for people with all types of medical conditions and related challenges. The discrimination and stigma traditionally attached to epilepsy may be decreasing thanks to efforts to improve understanding of epilepsy and decrease stigma nationally34 and globally35 and the increasing emphasis on accommodating individuals with disabilities or special medical needs.36,37 We have no way of assessing the impact of these factors in our or other cohorts; however, the possibility that differences between findings in earlier cohorts or different settings and ours might be because of improvements in attitudes cannot be ignored.
Assessment of psychiatric and learning disorders was based on medical record reviews and parent reports rather than standardized assessment, and it is likely that disorders, such as attention-deficit/hyperactivity disorder, have substantial variation in diagnosis across providers. We note that the assessments were made several years before outcomes were assessed, limiting the likelihood of diagnostic suspicion bias.38 We were generally not able to determine the onset of psychiatric problems relative to the onset of epilepsy, although learning problems clearly did precede the onset of epilepsy in many school-aged children.28
We also did not compare our cohort to the general population as done in some of the older studies,2,5,32 which demonstrated differences in people with and without epilepsy. Our purpose was to distinguish the roles of seizures from behavioral and learning problems and identify factors within young people with epilepsy that might influence adult outcomes.
Conclusions
In children with uncomplicated epilepsy, poorer seizure outcomes over many years appear to impact attainment of education and employment-related outcomes as well as driving; however, seizures seem to have less, if any, negative impact on other social functions that were considered. Learning problems and psychiatric disorders, by contrast, have pervasive influences across most social outcomes. Improved understanding of the course of epilepsy and its associated learning and behavioral difficulties as young people grow up could help prepare individuals to address, compensate for, and even overcome potential difficulties they may encounter entering adulthood.
Acknowledgments
We thank the many young people and their families whose participation over the years has made this study possible. We also thank Barry Russman, MD, who helped to make this study happen in the first place and Eugene Shapiro, MD, who helped it to continue.
Glossary
- AIC
Aikake Information Criterion
- ASM
antiseizure medication
- df
degrees of freedom
- OR
odds ratio
Footnotes
Dr Berg conceptualized and designed the study, supervised all data collection, planned, oversaw, and interpreted the analyses, and drafted and revised the manuscript; Drs Baca, Vickrey, and Caplan participated in planning and interpretation of the analyses and in critically reviewing and revising the manuscript; Ms Rychlik performed the analyses and participated in critical review and revision of the manuscript; and Drs Testa and Levy participated in reviewing clinical data for the study over the years as well as in critically reviewing and revising the manuscript.
FINANCIAL DISCLOSURE: The authors have indicated they no financial relationships relevant to this article to disclose.
FUNDING: This study was funded by grant R37-NS31146 from the National Institute of Neurologic Disorders and Stroke. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Camfield C, Camfield P, Smith B, Gordon K, Dooley J. Biologic factors as predictors of social outcome of epilepsy in intellectually normal children: a population-based study. J Pediatr. 1993;122(6):869–873 [DOI] [PubMed] [Google Scholar]
- 2.Sillanpää M, Jalava M, Kaleva O, Shinnar S. Long-term prognosis of seizures with onset in childhood. N Engl J Med. 1998;338(24):1715–1722 [DOI] [PubMed] [Google Scholar]
- 3.Geerts A, Brouwer O, van Donselaar C, et al. Health perception and socioeconomic status following childhood-onset epilepsy: the Dutch study of epilepsy in childhood. Epilepsia. 2011;52(12):2192–2202 [DOI] [PubMed] [Google Scholar]
- 4.Shackleton DP, Kasteleijn-Nolst Trenité DGA, de Craen AJM, Vandenbroucke JP, Westendorp RGJ. Living with epilepsy: long-term prognosis and psychosocial outcomes. Neurology. 2003;61(1):64–70 [DOI] [PubMed] [Google Scholar]
- 5.Chin RFM, Cumberland PM, Pujar SS, Peckham C, Ross EM, Scott RC. Outcomes of childhood epilepsy at age 33 years: a population-based birth-cohort study. Epilepsia. 2011;52(8):1513–1521 [DOI] [PubMed] [Google Scholar]
- 6.Sillanpää M, Schmidt D. Long-term employment of adults with childhood-onset epilepsy: a prospective population-based study. Epilepsia. 2010;51(6):1053–1060 [DOI] [PubMed] [Google Scholar]
- 7.Camfield C, Camfield P. Twenty years after childhood-onset symptomatic generalized epilepsy the social outcome is usually dependency or death: a population-based study. Dev Med Child Neurol. 2008;50(11):859–863 [DOI] [PubMed] [Google Scholar]
- 8.Austin JK, Harezlak J, Dunn DW, Huster GA, Rose DF, Ambrosius WT. Behavior problems in children before first recognized seizures. Pediatrics. 2001;107(1):115–122 [DOI] [PubMed] [Google Scholar]
- 9.Hermann B, Jones J, Sheth R, Dow C, Koehn M, Seidenberg M. Children with new-onset epilepsy: neuropsychological status and brain structure. Brain. 2006;129(pt 10):2609–2619 [DOI] [PubMed] [Google Scholar]
- 10.Jones JE, Watson R, Sheth R, et al. Psychiatric comorbidity in children with new onset epilepsy. Dev Med Child Neurol. 2007;49(7):493–497 [DOI] [PubMed] [Google Scholar]
- 11.Oostrom KJ, Smeets-Schouten A, Kruitwagen CLJJ, Peters ACB, Jennekens-Schinkel A; Dutch Study Group of Epilepsy in Childhood . Not only a matter of epilepsy: early problems of cognition and behavior in children with “epilepsy only”–a prospective, longitudinal, controlled study starting at diagnosis. Pediatrics. 2003;112(6 pt 1):1338–1344 [DOI] [PubMed] [Google Scholar]
- 12.Caplan R, Siddarth P, Gurbani S, Ott D, Sankar R, Shields WD. Psychopathology and pediatric complex partial seizures: seizure-related, cognitive, and linguistic variables. Epilepsia. 2004;45(10):1273–1281 [DOI] [PubMed] [Google Scholar]
- 13.Caplan R, Siddarth P, Stahl L, et al. Childhood absence epilepsy: behavioral, cognitive, and linguistic comorbidities. Epilepsia. 2008;49(11):1838–1846 [DOI] [PubMed] [Google Scholar]
- 14.Berg AT, Shinnar S, Levy SR, Testa FM. Newly diagnosed epilepsy in children: presentation at diagnosis. Epilepsia. 1999;40(4):445–452 [DOI] [PubMed] [Google Scholar]
- 15.Berg AT, Rychlik K. The course of childhood-onset epilepsy over the first two decades: a prospective, longitudinal study. Epilepsia. 2015;56(1):40–48 [DOI] [PubMed] [Google Scholar]
- 16.Berg AT, Rychlik K, Levy SR, Testa FM. Complete remission of childhood-onset epilepsy: stability and prediction over two decades. Brain. 2014;137(pt 12):3213–3222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Camfield P, Camfield C. Epileptic syndromes in childhood: clinical features, outcomes, and treatment. Epilepsia. 2002;43(suppl 3):27–32 [DOI] [PubMed] [Google Scholar]
- 18.Kwan P, Arzimanoglou A, Berg AT, et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia. 2010;51(6):1069–1077 [DOI] [PubMed] [Google Scholar]
- 19.Baca CB, Vickrey BG, Caplan R, Vassar SD, Berg AT. Psychiatric and medical comorbidity and quality of life outcomes in childhood-onset epilepsy. Pediatrics 2011;128(6). Available at: www.pediatrics.org/cgi/content/full/128/6/e1532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berg AT, Caplan R, Hesdorffer DC. Psychiatric and neurodevelopmental disorders in childhood-onset epilepsy. Epilepsy Behav. 2011;20(3):550–555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu S. Center for Research in Computation. Akaike Information Criterion. Available at: http://www4.ncsu.edu/∼shu3/Presentation/AIC.pdf. Accessed March 3, 2015
- 22.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706 [DOI] [PubMed] [Google Scholar]
- 23.Berg AT, Shinnar S, Levy SR, Testa FM, Smith-Rapaport S, Beckerman B. How well can epilepsy syndromes be identified at diagnosis? A reassessment 2 years after initial diagnosis. Epilepsia. 2000;41(10):1269–1275 [DOI] [PubMed] [Google Scholar]
- 24.Sillanpää M, Haataja L, Shinnar S. Perceived impact of childhood-onset epilepsy on quality of life as an adult. Epilepsia. 2004;45(8):971–977 [DOI] [PubMed] [Google Scholar]
- 25.Camfield CS, Camfield PR. The adult seizure and social outcomes of children with partial complex seizures. Brain. 2013;136(pt2):593–600 [DOI] [PubMed] [Google Scholar]
- 26.Camfield P, Camfield C. Idiopathic generalized epilepsy with generalized tonic-clonic seizures (IGE-GTC): a population-based cohort with >20 year follow up for medical and social outcome. Epilepsy Behav. 2010;18(1-2):61–63 [DOI] [PubMed] [Google Scholar]
- 27.Camfield CS, Camfield PR. Rolandic epilepsy has little effect on adult life 30 years later: a population-based study. Neurology. 2014;82(13):1162–1166 [DOI] [PubMed] [Google Scholar]
- 28.Berg AT, Hesdorffer DC, Zelko FAJ. Special education participation in children with epilepsy: what does it reflect? Epilepsy Behav. 2011;22(2):336–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor J, Kolamunnage-Dona R, Marson AG, Smith PEM, Aldenkamp AP, Baker GA; SANAD study group . Patients with epilepsy: cognitively compromised before the start of antiepileptic drug treatment? Epilepsia. 2010;51(1):48–56 [DOI] [PubMed] [Google Scholar]
- 30.Masur D, Shinnar S, Cnaan A, et al. ; Childhood Absence Epilepsy Study Group . Pretreatment cognitive deficits and treatment effects on attention in childhood absence epilepsy. Neurology. 2013;81(18):1572–1580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lillywhite LM, Saling MM, Harvey AS, et al. Neuropsychological and functional MRI studies provide converging evidence of anterior language dysfunction in BECTS. Epilepsia. 2009;50(10):2276–2284 [DOI] [PubMed] [Google Scholar]
- 32.Geerts A, Arts WF, Stroink H, et al. Course and outcome of childhood epilepsy: a 15-year follow-up of the Dutch Study of Epilepsy in Childhood. Epilepsia. 2010;51(7):1189–1197 [DOI] [PubMed] [Google Scholar]
- 33.National Center for Education Statistics. Digest of Education Statistics. Averaged freshman graduation rates for public secondary schools, by state or jurisdiction: Selected years 1990-91 through 2009-2010. Available at: http://nces.ed.gov/programs/digest/d12/tables/dt12_124.asp. Accessed March 3, 2015
- 34.Institute of Medicine Epilepsy Across the Spectrum: Promoting Health and Understanding. Washington, DC: National Academies Press; 2012 [PubMed] [Google Scholar]
- 35.International League Against Epilepsy , International Bureau for Epilepsy, World Health Organization. Global Campaign Against Epilepsy: Out of the Shadows. Heemstede, Netherlands: International Bureau for Epilepsy; 2003
- 36.US Department of Justice, Civil Rights Division. Americans With Disability Act. Available at: www.ada.gov. Accessed March 3, 2015
- 37.US Department of Education, Office of Special Education and Rehabilitation Services. Thirty-five Years of Progress in Educating Children With Disabilities Through IDEA Washington, DC: US Department of Education; 2010 [Google Scholar]
- 38.Haynes RB, Sackett DL, Guyatt GH, Tugwell P. Clinical Epidemiology: How To Do Clinical Practice Research. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006 [Google Scholar]