Abstract
Histone deacetylases (HDACs) are highly expressed in intrahepatic cholangiocarcinoma (ICC) and are associated with poor prognosis of these patients. The aim of the present study was to explore the inhibitory effects of HDAC inhibitors on ICC cells and identify effective and sensitive drugs for ICC. Effects of 34 HDAC inhibitors were screened through two rounds of cell viability assays, and HC toxin, a cyclic tetrapeptide first isolated from the secondary metabolite of Helminthosporium carbonum, exhibited an antitumor activity superior to that of the other HDAC inhibitors and gemcitabine. The mechanisms involved in the inhibitory effects of HC toxin on CCLP-1 cells were investigated by cell counting, colony formation assay, cell morphological observation, real-time PCR, western blotting and flow cytometry. It was demonstrated that HC toxin inhibited the cell proliferation and clone formation ability of the CCLP-1 cells. HC toxin increased the acetyl-histone H4 level and this was associated with the inhibitory effect of HC toxin on the CCLP-1 cells. We also found that HC toxin reduced the level of HDAC1 protein in a post-transcriptional manner. Morphological observation showed multiple morphological changes and indicated the possibility of cell differentiation owing to HC toxin. With increasing concentration of HC toxin, the cell cycle was gradually arrested at the G0/G1 stage and the percentage of apoptotic cells increased which was not mainly through the caspase-3-dependent ways. These results indicated that HC toxin was the most effective among the various HDAC inhibitors with multiple functions in the suppression of ICC in vitro. Thus, HC may be a potential chemotherapeutic for ICC.
Keywords: HC toxin, intrahepatic cholangiocarcinoma, histone deacetylase inhibitor, cell proliferation, apoptosis, cell cycle, cell differentiation
Introduction
Intrahepatic cholangiocarcinoma (ICC) is an epithelial cell malignancy arising from cholangiocytes within the liver. Although ICC is rare, the morbidity and mortality rates have markedly increased over the last three decades, particularly in European and American countries (1). Unlike hepatic cellular carcinoma and hilar cholangiocarcinoma, the dormant clinical symptoms and ambiguous imaging features make it even harder for ICC to be diagnosed at an early stage (2,3). Thus, the chance for curative resection is generally limited, and patients with ICC are also not suitable for liver transplantation (4). Moreover, owing to its desmoplastic character, complicated tumor microenvironment and rich genetic heterogeneity, ICC is consistenly resistant to traditional chemotherapeutics (5,6). Various targeted therapeutics and combined chemotherapy do not demonstrate desired results except for the protocol of gemcitabine plus cisplatin which achieves a median survival time of only 11.7 months for patients who do not receive surgery (7,8). Therefore, new sensitive therapeutics are urgently needed.
Histone deacetylases (HDACs) are responsible for the removal of acetyl groups from the lysine residues on the N-terminal part of core histones (H2A, H2B, H3 and H4) and maintain a balance with histone acetylase in normal organisms. When overexpressed, HDACs may give rise to the formation of heterochromatin without DNA binding by associated transcription factors. As a result, it may silence various key genes, which play important roles in transcriptional regulation, cell cycle progression and developmental events. In the occurrence and development of ICC, HDACs play an oncogene role (9). Expression of HDAC1 was found to be significantly correlated with lymph node metastasis, high stage carcinoma and vascular invasion of ICC and was found to be negatively correlated with prognosis (10). Therefore, it is reasonable to regulate the expression and activity of HDACs for the treatment of ICC. Although studies have reported the effects of various HDAC inhibitors on bile duct cancer cells (11–13), to the best of our knowledge, no research concerning the effects of HDAC inhibitors on ICC has been reported to date.
HC toxin, a cyclic tetrapeptide first isolated from the secondary metabolite of Helminthosporium carbonum (14), is thought to be a type of HDAC inhibitor in plants, insects and mammals (15). It was found to exhibit antitumor activities in several types of human cancer cells with stronger antitumor activity than other HDAC inhibitors in neuroblastoma cells (16–18). In the present study, we explored the effects of 34 types of HDAC inhibitors on ICC cell lines in vitro, compared the anti-ICC activity of HC toxin with other HDAC inhibitors and investigated the mechanisms involved in the inhibitory effects of the HC toxin on ICC in vitro.
Materials and methods
Cell culture and HDAC inhibitors
ICC cell lines RBE and SSP-25 (obtained from Piken University, Japan) and CCLP-1 and TFK-1 (obtained from the University of Pittsburg, USA) were cultured in RPMI-1640 medium (Gibco, USA) containing 10% fetal calf serum (FCS) (HyClone, USA). All media contained 2 mM L-glutamine, 100 U/ml of penicillin G and streptomycin. The cell lines were passaged twice/week and maintained at 37°C in 5% CO2-95% air (vol/vol). Trichostatin A (TSA), suberohydroxamic acid (SAHA), gemcitabine (GEM), HC toxin and other HDAC inhibitors (Cayman 11076, no. 0466317) were dissolved in dimethyl sulfoxide (DMSO) at 10 mM ready for usage.
Cell viability assay
Cells were plated in 96-well plates (at 5×103 cells/well), and divided into trial control and blank groups co-cultured with HDAC inhibitors, solvent or nothing for 48 h in three replicates, respectively. Cell viability was verified by adding Cell Counting Kit-8 (CCK-8; Dojindo, Japan) into the well at a final concentration of 10% after discarding the previous supernatant and incubating for 2–4 h at 37°C. Then, the absorbance at 450 nm was examined using a microplate reader (Mithras LB 940; Berthold Technologies GmbH & Co., Bad Wildbad, Germany) and displayed as the optical density (OD). Cell viability = (trial group OD - blank group OD)/(control group OD - blank group OD) × 100%.
Cell counting
Cells were plated in 6-well plates (at 5×104 cells/well). After culturing with the HDAC inhibitors at different doses for 24–72 h with medium changed every 24 h, the cells were digested and dissolved using phosphate-buffered saline (PBS) as single-cell suspension. Cell number was examined using the Countess Cell Counting Chamber (Invitrogen, USA).
Colony formation assay
Single-cell suspensions were plated into 6-well plates at a density of 300–500 cells/well. After the cells became adherent, the medium was replaced and different doses of HC toxin were added. The cells were cultured for 10–14 days at 37°C and stained with Giemsa staining after being fixed with 4% paraformaldehyde (Sigma, USA). Viable colonies were counted. Colony formation rate = colony number/number of plated cells × 100%.
Giemsa staining and light microscopic observation
Cells were grown on coverslips placed in 6-well plates (at 5×104/well) in advance and cultured with HC toxin for two days. After being fixed with 4% paraformaldehyde and washing with PBS three times/5 min, the cells were stained by Giemsa staining (Xiangya, China) for 15–30 min and then placed on a microscopic slide. An upright metallurgical microscope (Euro immune; Germany) and an inverted microscope (Olympus, Japan) were used to observe the morphology of the cells with and without Giemsa staining, respectively. Images were captured and cells with apoptotic bodies were counted.
Flow cytometry
The cells were harvest after incubation with the HC toxin or solvent for 48 h. For apoptosis assessment, 7-AAD combined with FITC-conjugated Annexin V (both from BioLegend, USA) were used to treat the cells according to the manufacturer's protocols. For cell cycle analysis, the cells were collected in 0.001% Triton of PBS and stained with 7-AAD alone after being fixed in 5 ml of 70% cold ethanol for 24 h. Approximately 10,000–20,000 cells were analyzed with a FACSCalibur using CellQuest software (both from Becton-Dickinson, USA). FlowJo 7.6.1 was used to analyze the data.
Western blot analysis
Total proteins were extracted using the protein extraction kit (KeyGen Biotech, China) and were transferred onto a polyvinylidene fluoride membrane (Millipore, Germany) after being separated on 10% SDS-PAGE. Anti-bax, anti-bcl-2, anti-cytochrome c (Santa Cruz Biotechnology, Santa Cruz, CA, USA), anti-β-actin (Bioeasy, Korea), anti-caspase-3 (Abcam, USA), anti-HDAC1 (Cell Signaling Technology, USA), and anti-acetyl-histone H4 (Upstate) were used to detected proteins and the homologous secondary antibody conjugated with horseradish peroxidase were then used to detect the primary antibodies. Immunoreactive bands were cast to X-ray film (Carestream, China) after shining by a chemiluminescent substrate (Millipore, Germany). ImageJ software (National Institutes of Health, Bethesda, MA, USA) was used to calculate the relative expression of proteins.
Real-time PCR
Total RNA was extracted from the cells plated in 6-well plates after treatment with the HC toxin for 48 h using an RNA simple extracted kit (Tiangen China). Reverse transcription reaction was immediately performed using the PrimeScript RT reagent kit (Takara, Japan). Real-Time PCR was carried out in an ABI 7500 Real-Time PCR system (Life Technologies) using the SYBR II-Green PCR kit (Takara), and the data are shown in 2−ΔΔCt format. β-actin was used as inner reference. Primers for HDAC1 were: 5′-CTCCATCCGTCCAGATAAAT-3′ and 5′-GCCACAGAACCACCAGTAG-3′; and primers for β-actin were: 5′-GAGAAGGCGTGACATTAAG-3′ and 5′-GAAGGAAGGCTGGAAGAG-3′ (both from Sangon, China). All the processes were performed according to the manufacturer's protocols included in the kits, correspondingly.
Statistical analysis
Every experiment was performed at least three times in triplicate, and data are shown as the mean ± SD. Differences between groups were assessed using the Student's t-test (one sample or paired t-tests), and were considered as statistically significant at a P-value <0.05.
Results
Anti-ICC activity of HC toxin is superior to that of other HDAC inhibitors and gemcitabine (GEM)
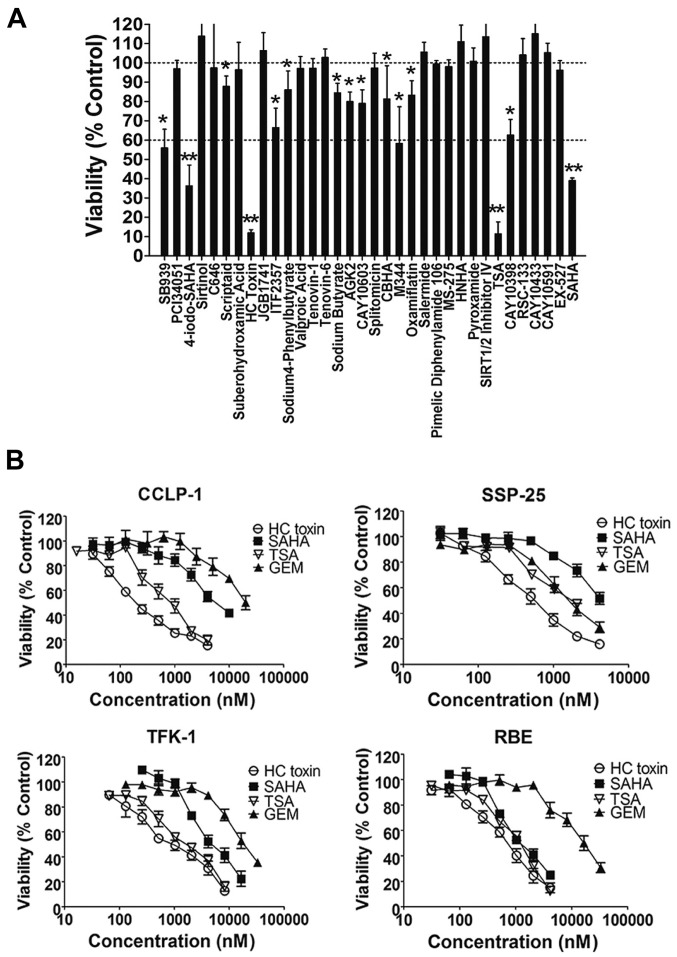
In the primary screening (Fig. 1A), all of the compounds at a concentration of 3 µM were co-cultured with the REB cells for 48 h and cell viability was assessed by the CCK-8 assay. The results revealed that 13 of the 34 types of HDAC inhibitors showed inhibitory activities with cell viability <100%. Among these, the inhibitory effects of HC toxin, TSA, SAHA and 4-iodo-SAHA were the most intensive with cell viability <60%.
Figure 1.
Results of the HDAC inhibitor screening in intrahepatic cholangiocarcinoma (ICC) cell lines by cell viability assays. (A) Cell viability of RBE cells after being co-cultured with 34 HDAC inhibitors for 48 h. All of the HDAC inhibitors were used at a final concentration of 3 µM. Differences were statistical significant at *P<0.05 compared with 100% and **P<0.05 compared with 60% viability. (B) Cell viability of four ICC cell lines after being co-cultured with HC toxin, SAHA, TSA or gemcitabine (GEM) for 48 h. The concentration gradient used increased from 30 nM to 30 µM with a common ratio of two.
To establish that the suppressive effects of the 13 HDAC inhibitors were not specific to the RBE cell line, we co-cultured four ICC cell lines (TFK-1, RBE, SSP-25 and CCLP-1) with three HDAC inhibitors (HC toxin, TSA or SAHA) or the positive control (GEM) for 48 h. In the secondary screening (Fig. 1B), HC toxin was the most effective followed by TSA, and all three HDAC inhibitors exhibited stronger anti-ICC activities in the four ICC cell lines than GEM except for SAHA in the SSP-25 cell line. The inhibitory activity of HC toxin was similar to that of TSA in the TFK-1 and RBE cell lines while it was superior to TSA in the SSP-25 and CCLP-1 cell lines from concentration from ~30 nM to 8 µM. These results indicated that the anti-ICC activity of HC toxin was superior to that of the other HDAC inhibitors and GEM.
We also calculated the IC50 values of the HC toxin. For the CCLP-1, SSP-25, TFK-1 and RBE cell lines, the IC50 values were ~297.6±80.4, 520.0±43.0, 854.6±86.9 and 713.7±27.3 nM, respectively. Thus, we chose HC toxin at a concentration ~400 nM to co-culture with the CCLP-1 cells in the following experiments.
HC toxin suppresses cell proliferation and colony formation of CCLP-1 cells
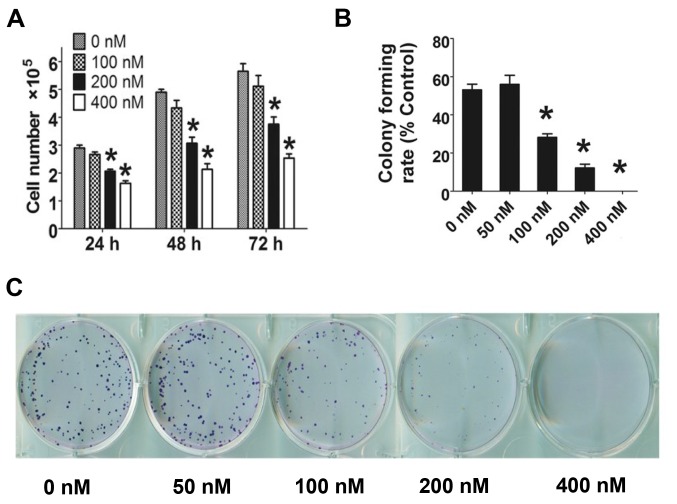
HC toxin (0–400 nM) was co-cultured with CCLP-1 cells, and cell number decreased with increasing concentration of HC toxin for 24–72 h (Fig. 2A). HC toxin at 100 nM did not significantly restrict the cell proliferation of the CCLP-1 cells at the three time points. At 48 h, the number of cells was reduced by 1.5- to 2.2-fold following treatment with HC toxin in a dose-dependent manner which was in line with the cell viability assay as determined by the CCK-8 assay.
Figure 2.
Effects of HC toxin on the cell proliferation and clone formation ability of CCLP-1 cells. *P<0.05, difference is statistically significant. (A) Cell counting of CCLP-1 cells after culturing with the indicated doses of HC toxin for 24–72 h. (B and C) Results of the colony formation assay.
In the colony formation assay (Fig. 2B and C), the colony formation rate of the CCLP-1 cells was decreased from ~53.1±5.2% in the control group (0 nM) to 0% in the 400 nM group. The rate of colony formation of the 50 nM group was modestly increased when compared with the 0 nM group, but the difference was not statistically significant.
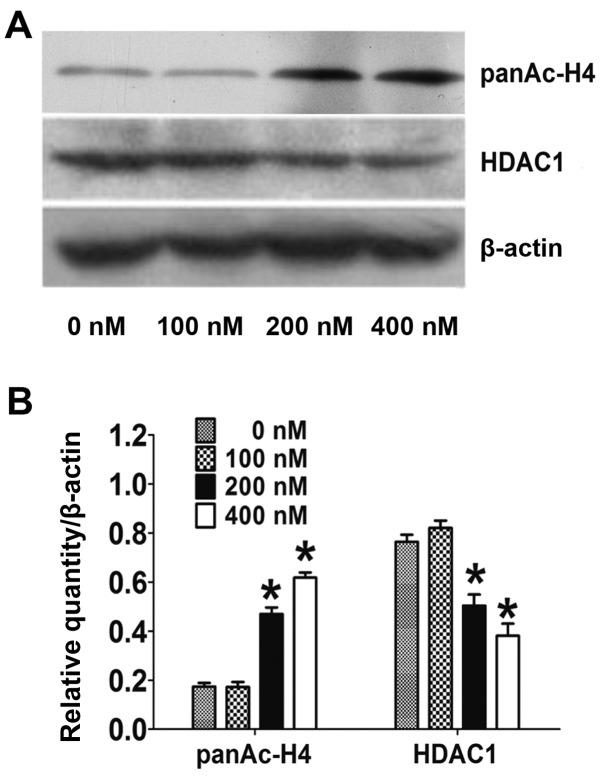
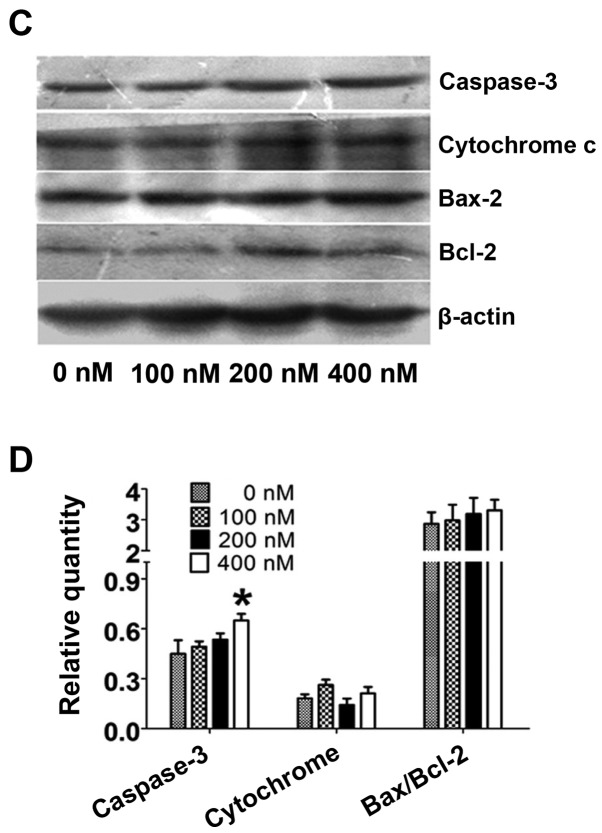
HC toxin downregulates the protein level of acetyl-histone H4 and HDAC1
The activity of HDAC was examined indirectly by checking the level of acetyl-histone H4. As shown in Fig. 3A and B, the acetyl-histone H4 level was markedly reduced by 2.5- to 3.3-fold following treatment with 200 and 400 nM of HC toxin, respectively, while the level did not obviously change following HC toxin treatment at 100 nM. This correlated with the inhibitory effects on the cell proliferation and colony ability in the CCLP-1 cells.
Figure 3.
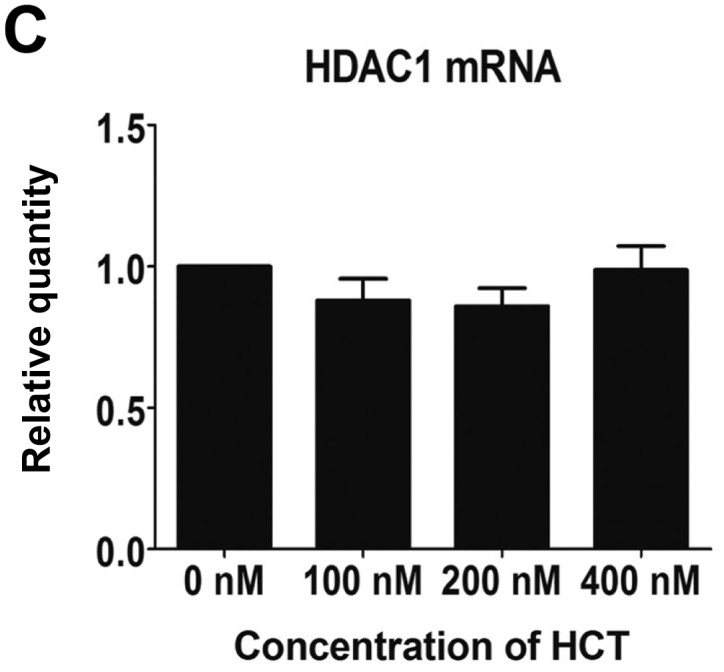
Effects of HC toxin on the level of acetyl-histone H4 and HDAC1 proteins, and HDAC1 mRNA in CCLP-1 cells. *P<0.05, difference is statistically significant. (A and B) Protein levels of acetyl-histone H4 and HDAC1 as examined by western blotting. (C) The mRNA level of HDAC1 as examined by real-time PCR.
We also examined the expression of HDAC1 in CCLP-1 cells. As shown in Fig. 3A and B, the expression of HDAC1 protein was markedly reduced 1.6- to 2.2-fold at 200 and 400 nM of HC toxin respectively while no change was obvious at 100 nM. However, the mRNA of HDAC1 examined by real-time PCR did not change at all of the three doses used (Fig. 3C).
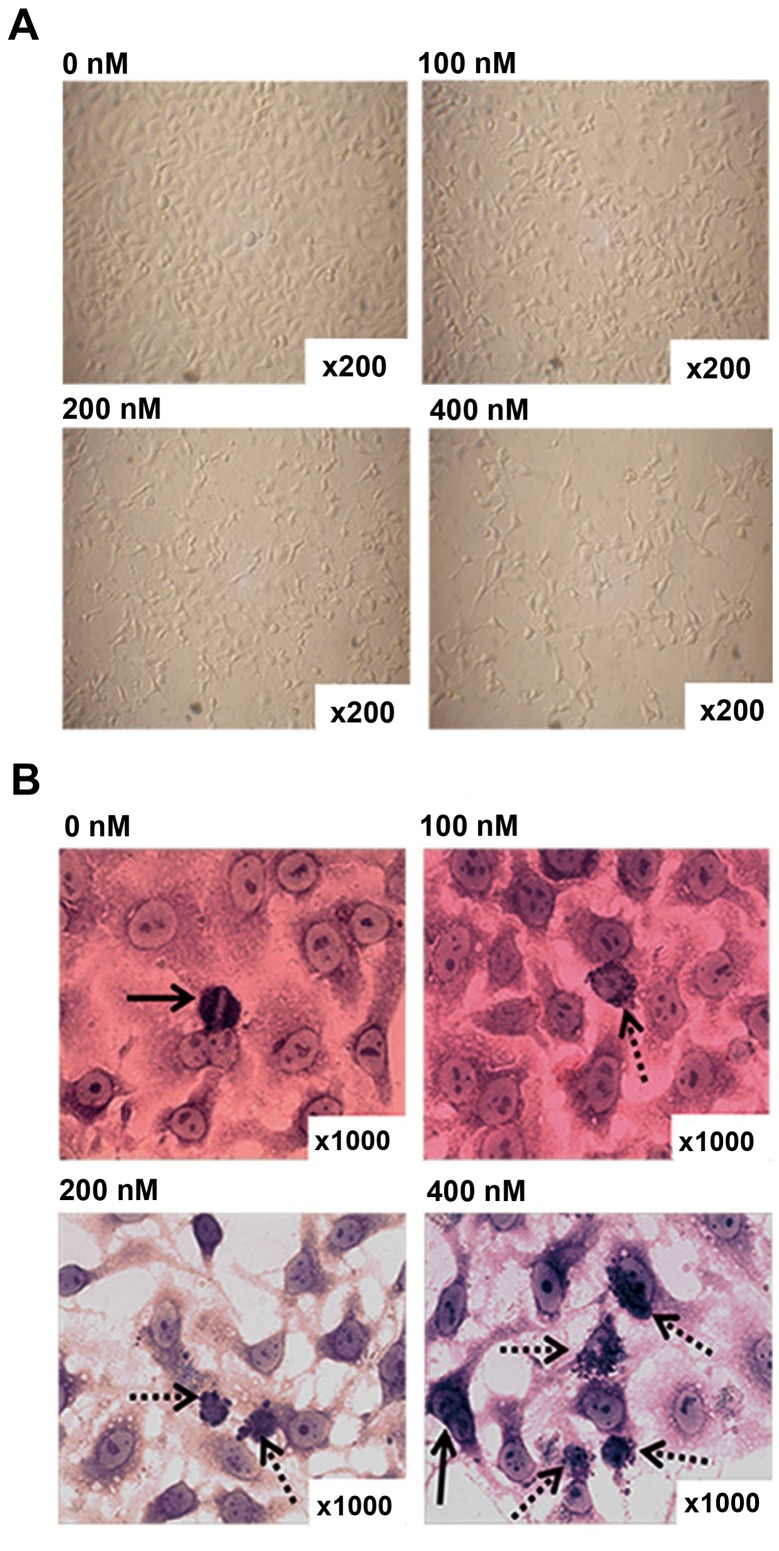
HC toxin induces multiple morphological changes under light microscopic observation
CCLP-1 cells were cultured with the different doses of HC toxin for 48 h. The morphology and growth features of the cells in each groups were observed by light microscopy before and after Giemsa staining. With increasing doses of HC toxin, the cells gradually decreased in density with single cells dwindling in size, dendrite-like structures appearing and gradually became longer (Fig. 4A).
Figure 4.
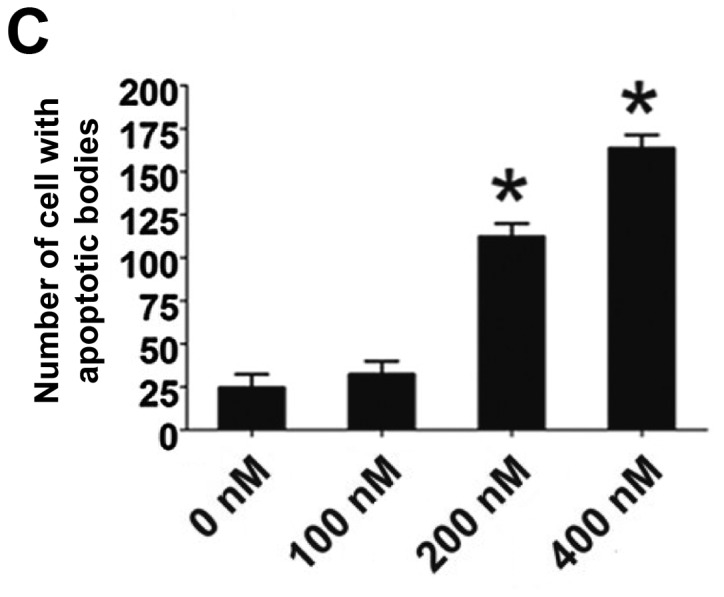
Effects of HC toxin on the morphology of CCLP-1 cells. (A) Cell morphology of CCLP-1 cells without Giemsa staining. (B) Cell morphology of CCLP-1 cells with Giemsa staining. Dotted arrows indicate cells with apoptotic bodies. Solid arrows indicate cells in meiosis. (C) Cell counting of cells with apoptotic bodies from 10 fields at a magnification of x200 by microscopy; 0, 100, 200 and 400 nM are the doses of HC toxin used. *P<0.05, difference is statistically significant.
In order to clearly observe cell nuclei, Giemsa staining was performed. As shown in Fig. 4B, multinucleated and cellular atypia were reduced, mitotic figures decreased, apoptotic bodies appeared and progressively increased with the increasing concentration of the HC toxin. We calculated the number of cells with apoptotic bodies from 10 fields with a magnification of x200. This showed that the number of cells with apoptotic bodies in the 200 and 400 nM groups was much higher than that in the 0 and 100 nM groups, and there was no difference between the latter two in terms of statistical significance (Fig. 4C).
Cell cycle is arrested at the G0/G1 stage
Cell cycle distribution was detected by flow cytometry with 7-AAD staining. After incubation with HC toxin for 48 h, the floating cells were removed to exclude the interference from apoptosis and dead cells. Compared with the 0 nM group, the 20 and 400 nM groups exhibited significantly higher percentages of cells in the G0/G1 stage and the percentages of cells in the G2/M stage were markedly deceased in a dose-dependent manner (Fig. 5A and B). No difference in the percentage of cells in the S stage was observed among the groups. This illustrated that HC toxin arrests the cell cycle in the G0/G1 stage.
Figure 5.
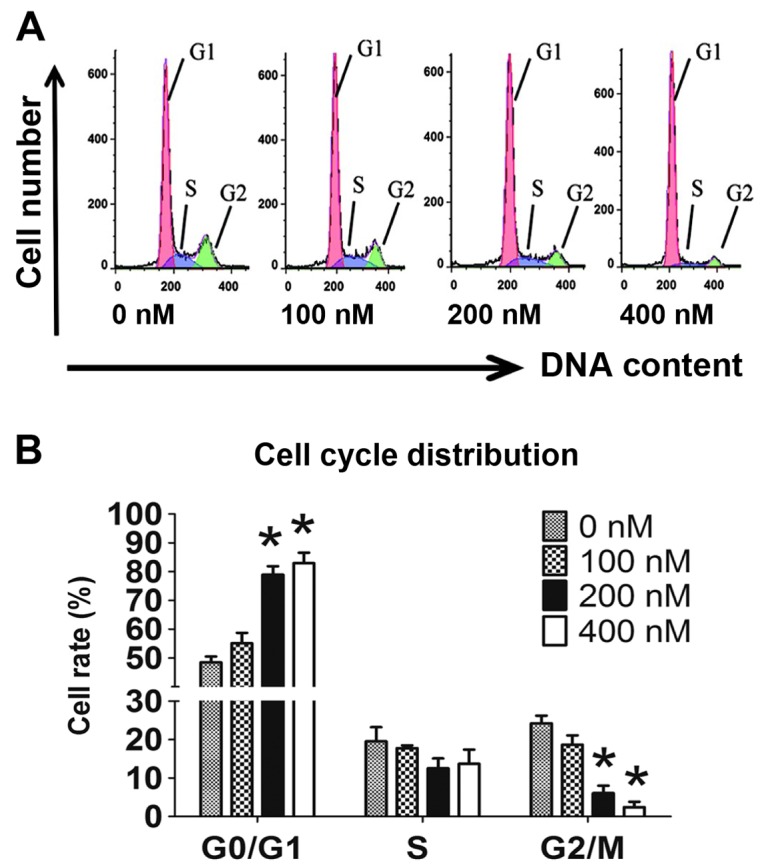
(A and B) Cell cycle distribution of CCLP-1 cells after treatment with HC toxin for 48 h; 0, 100, 200 and 400 nM are the doses of HC toxin used. *P<0.05, difference is statistically significant.
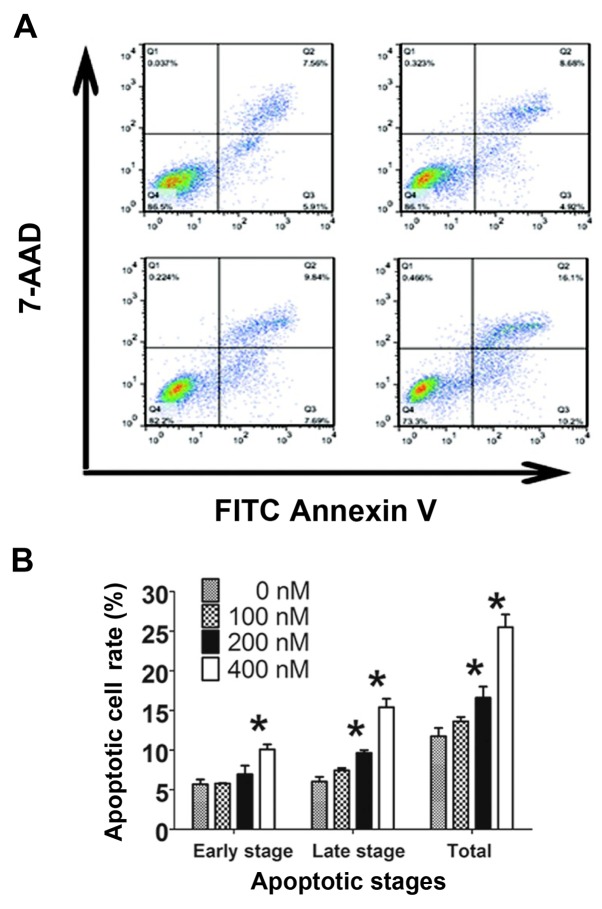
HC toxin induces cell apoptosis via the caspase-3-dependent and -independent pathways
The apoptotic effects of the HC toxin were examined by flow cytometry with staining of Annexin V-FITC combined with 7-AAD and by assessment of morphological changes with Giemsa staining. In the 200 and 400 nM groups, the numbers of cells with apoptotic bodies were significantly increased compared with the 0 nM group (Fig. 4C). The percentages of total apoptosis, early apoptosis and late apoptosis were increased with the increasing HC toxin concentration (Fig. 6A and B). Significant increases in the percentages of cells in the late and total stage of apoptosis were noted at 200 nM of HC toxin, but could not be observed in the early stage. This may be due to the binding capacity of Annexin V-FITC or the instrument noise.
Figure 6.
Effects of HC toxin on the apoptotic effect of CCLP-1 cells. (A and B) Apoptotic cell ratio of CCLP-1 cells as examined by flow cytometry. (C and D) Expression changes and relative quantification of apoptotic proteins examined by western blotting; 0, 100, 200 and 400 nM are the doses of HC toxin used. *P<0.05, difference is statistically significant.
We then explored the specific apoptosis pathways involved by assessing the expression changes in apoptotic proteins. The expression of caspase-3 did not show a significant increase until the concentration of HC toxin increased to 400 nM with only an increase of ~1.5-fold. The levels of bax/bcl-2 and cytochrome c did not change in our experimental environment (Fig. 6C and D). Therefore, it is reasonable to consider that the caspase-3-dependent pathway was not the major pathway which was involved in the HC toxin-mediated apoptosis while the caspase-3-independent pathway may play the major role.
Discussion
ICC is the second most common malignant tumor in the liver and its pathogenesis is still unclear. Late diagnosis and the high recurrence rate have limited the effects of surgical excision and lead to dismal overall 5- and 3-year survival rates even worse than HCC (19). Moreover, there is no effective chemotherapy regimens for ICC due to the high chemoresistance. Thus, discovery of novel sensitive therapeutics is warranted. In the present study, we carried out two rounds of screening for 34 types of HDAC inhibitors. HC toxin was the most effective in the suppression of growth of the ICC cell lines and the mechanisms were associated with cell apoptosis, cell cycle arrest and differentiation.
HDAC inhibitors are potential antitumor agents composed of hydroxamic acid, cyclotetrapeptides, benzamide, some short chain fatty acids and other molecular structure types (20). The 34 HDAC inhibitors used, which were chosen from an epigenetic library provided by Cayman Co., covered more molecular structure types of HDAC inhibitors than the previous study (16). In the primary screening, 13 HDAC inhibitors exhibited anti-ICC activity and four exhibited intensive activity (cell viability <60%). Among them, valproic acid (VPA), which was the earliest HDAC inhibitor, exhibited a weak antitumor activity in RBE cells in line with previous research on HuCCT1 (ICC cell line) and SUIT-2 (pancreas cancer cell line) cells (13). Yet, the significance of the primary screening was confined to only one cell line and one concentration was used. Therefore, we performed a secondary screening in four ICC cell lines with different doses of HDAC inhibitors. In the secondary screening, HC toxin showed an anti-ICC activity much stronger than that of gemcitabine which is currently one of the most important chemotherapeutic for the treatment of ICC (21,22). The effect of TSA was similar to that of HC toxin in RBE and TFK-1 cells but was obviously inferior to the latter in SSP-25 and CCLP-1 cells. This suggested that HC toxin may have a wider antitumor spectrum and may also work in the treatment of some tumor subtypes with chemoresistance. Hence, HC toxin could be a potential therapeutic for cancer treatment.
The mechanisms involved in the inhibitory effects of the HC toxin in ICC cell lines are various and are as follows.
Firstly, as a cell-permeable, reversible inhibitor of HDACs, HC toxin acts mainly by inhibiting the activities of HDACs to carry out H3 and/or H4 hyperacetylation in their promoter regions (15) and this is in line with the results shown in Fig. 3A and B. In our research, we also found that the protein expression of HDAC1 decreased by western blot analysis. However, the mRNA of HDAC1 did not change correspondingly. This illustrated that HC toxin downregulated the HDAC1 level depending on the post-transcriptional modification or the degradation acceleration of HDAC1 itself.
Secondly, the cell cycle was arrested at the G0/G1 stage which suggested that DNA replication or histone synthesis was blocked at the S stage. The results were in line with previous findings of HC toxin in neuroblastoma cells (16), but not breast cancer cells (T47D) in which the cell cycle was arrested at G2/M (17). This difference may be associated with the nature of the cell lines used. Cell cycle arrest at G0/G1 may rely on a change in p21waf1 and cyclin protein (23). As a cell cyclin kinase inhibitor, p21waf1 upregulation may suppress the activities of cyclin and reduce the phosphorylation level of Rb therefore resulting in the decrease in the E2F level and finally arresting the cell cycle at the G0/G1 stage. Suberoylanilide hydroxamic acid (SAHA), another type of HDAC inhibitor, induces a sharp rising in p21waf1 protein and mRNA of bladder carcinoma cells (T24) (24). Many other HDAC inhibitors have a similar functional mechanism (25–27), and this may also exist in the process of HC toxin function in CCLP-1 cells; yet this requires further experiments to verify. Additionally, HC toxin may play a role in cell cycle synchronization and may be a solution for drug-resistance in some cases; thus, the use of HC toxin in various combination chemotherapy protocols should be considered.
Thirdly, morphologic changes and flow cytometry demonstrated that HC toxin strongly induced the apoptosis of CCLP-1 cells. Cell apoptotic pathways can be simply divided into caspase-3-dependent and caspase-3-independent pathways (28). Bax/Bcl-2, cytochrome c and caspase-3 are the major apoptosis-related proteins in the former containing endogenous and exogenous pathways (29,30). In the caspase-3-independent pathway, AIF, Endo G are the primary functional proteins produced in mitochondria and transferred into the nucleus to cleave DNA directly (31). In the western blot assay, the caspase-3 level was not markedly increased until the concentration of the HC toxin increased to 400 nM which did not correlate with the results of the flow cytometry. In addition, the Bax/Bcl-2 ratio and the level of cytochrome c did not significantly change at all HC toxin doses used. In a previous study performed in breast cancer cells, HC toxin did not obviously change the level of caspase-3 as well (17). This demonstrated that HC toxin induced apoptosis by means of both the caspase-3-dependent and -independent pathways and the latter could be dominant.
Finally, it is likely that HC toxin may regulate the differentiation of CCLP-1 cells according to the morphologic changes consisting of the appearance of dendritic-like structures (32). In addition, it was confirmed that HC toxin promotes the differentiation of neuroendocrine cells (33). However, this finding should be further investigated at a molecular level to provide further evidence in order to establish whether or not HC toxin induces the differentiation of ICC cell lines.
In summary, HC toxin demonstrated anti-ICC activity superior to that of other HDAC inhibitors and GEM. It suppressed cell proliferation, arrested the cell cycle and induced apoptosis and may induce the differentiation of ICC cells in vitro. These findings provide the experimental basis for the treatment of ICC by HC toxin.
Acknowledgments
The present study was supported by grants from the Natural Science Foundation of China (no. 81071990), the Guangdong Province Natural Science Foundation (no. 2015A030313725), and the Guangdong Science Province and Technology Program projects (2012B03180411).
References
- 1.Everhart JE, Ruhl CE. Burden of digestive diseases in the United States Part III: Liver, biliary tract, and pancreas. Gastroenterology. 2009;136:1134–1144. doi: 10.1053/j.gastro.2009.02.038. [DOI] [PubMed] [Google Scholar]
- 2.Iavarone M, Piscaglia F, Vavassori S, Galassi M, Sangiovanni A, Venerandi L, Forzenigo LV, Golfieri R, Bolondi L, Colombo M. Contrast enhanced CT-scan to diagnose intrahepatic cholangiocarcinoma in patients with cirrhosis. J Hepatol. 2013;58:1188–1193. doi: 10.1016/j.jhep.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Kim SH, Lee CH, Kim BH, Kim WB, Yeom SK, Kim KA, Park CM. Typical and atypical imaging findings of intrahepatic cholangiocarcinoma using gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging. J Comput Assist Tomogr. 2012;36:704–709. doi: 10.1097/RCT.0b013e3182706562. [DOI] [PubMed] [Google Scholar]
- 4.Robles R, Figueras J, Turrión VS, Margarit C, Moya A, Varo E, Calleja J, Valdivieso A, Valdecasas JC, López P, et al. Spanish experience in liver transplantation for hilar and peripheral cholangiocarcinoma. Ann Surg. 2004;239:265–271. doi: 10.1097/01.sla.0000108702.45715.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tepsiri N, Chaturat L, Sripa B, Namwat W, Wongkham S, Bhudhisawasdi V, Tassaneeyakul W. Drug sensitivity and drug resistance profiles of human intrahepatic cholangiocarcinoma cell lines. World J Gastroenterol. 2005;11:2748–2753. doi: 10.3748/wjg.v11.i18.2748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiefer MV, Albert M, McNally M, Robertson M, Sun W, Fraker D, Olthoff K, Christians K, Pappas S, Rilling W, et al. Chemoembolization of intrahepatic cholangiocarcinoma with cisplatinum, doxorubicin, mitomycin C, ethiodol, and polyvinyl alcohol: A 2-center study. Cancer. 2011;117:1498–1505. doi: 10.1002/cncr.25625. [DOI] [PubMed] [Google Scholar]
- 7.Lee J, Park SH, Chang HM, Kim JS, Choi HJ, Lee MA, Jang JS, Jeung HC, Kang JH, Lee HW, et al. Gemcitabine and oxaliplatin with or without erlotinib in advanced biliary-tract cancer: A multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2012;13:181–188. doi: 10.1016/S1470-2045(11)70301-1. [DOI] [PubMed] [Google Scholar]
- 8.Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, Madhusudan S, Iveson T, Hughes S, Pereira SP, et al. ABC-02 Trial Investigators: Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362:1273–1281. doi: 10.1056/NEJMoa0908721. [DOI] [PubMed] [Google Scholar]
- 9.Sriraksa R, Limpaiboon T. Histone deacetylases and their inhibitors as potential therapeutic drugs for cholangiocarcinoma - cell line findings. Asian Pac J Cancer Prev. 2013;14:2503–2508. doi: 10.7314/APJCP.2013.14.4.2503. [DOI] [PubMed] [Google Scholar]
- 10.Morine Y, Shimada M, Iwahashi S, Utsunomiya T, Imura S, Ikemoto T, Mori H, Hanaoka J, Miyake H. Role of histone deacetylase expression in intrahepatic cholangiocarcinoma. Surgery. 2012;151:412–419. doi: 10.1016/j.surg.2011.07.038. [DOI] [PubMed] [Google Scholar]
- 11.Zhang P, Guo Z, Wu Y, Hu R, Du J, He X, Jiao X, Zhu X. Histone deacetylase inhibitors inhibit the proliferation of gallbladder carcinoma cells by suppressing AKT/mTOR signaling. PLoS One. 2015;10:e136193. doi: 10.1371/journal.pone.0136193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kitamura T, Connolly K, Ruffino L, Ajiki T, Lueckgen A, DiGiovanni J, Kiguchi K. The therapeutic effect of histone deacetylase inhibitor PCI-24781 on gallbladder carcinoma in BK5.erbB2 mice. J Hepatol. 2012;57:84–91. doi: 10.1016/j.jhep.2012.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iwahashi S, Ishibashi H, Utsunomiya T, Morine Y, Ochir TL, Hanaoka J, Mori H, Ikemoto T, Imura S, Shimada M. Effect of histone deacetylase inhibitor in combination with 5-fluorouracil on pancreas cancer and cholangiocarcinoma cell lines. J Med Invest. 2011;58:106–109. doi: 10.2152/jmi.58.106. [DOI] [PubMed] [Google Scholar]
- 14.Islam MN, Islam MS, Hoque MA, Kato T, Nishino N, Ito A, Yoshida M. Bicyclic tetrapeptides as potent HDAC inhibitors: Effect of aliphatic loop position and hydrophobicity on inhibitory activity. Bioorg Med Chem. 2014;22:3862–3870. doi: 10.1016/j.bmc.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 15.Walton JD. HC-toxin. Phytochemistry. 2006;67:1406–1413. doi: 10.1016/j.phytochem.2006.05.033. [DOI] [PubMed] [Google Scholar]
- 16.Deubzer HE, Ehemann V, Kulozik AE, Westermann F, Savelyeva L, Kopp-Schneider A, Riester D, Schwab M, Witt O. Anti-neuroblastoma activity of Helminthosporium carbonum (HC)-toxin is superior to that of other differentiating compounds in vitro. Cancer Lett. 2008;264:21–28. doi: 10.1016/j.canlet.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 17.Joung KE, Kim DK, Sheen YY. Antiproliferative effect of trichostatin A and HC-toxin in T47D human breast cancer cells. Arch Pharm Res. 2004;27:640–645. doi: 10.1007/BF02980164. [DOI] [PubMed] [Google Scholar]
- 18.Kamitani H, Taniura S, Ikawa H, Watanabe T, Kelavkar UP, Eling TE. Expression of 15-lipoxygenase-1 is regulated by histone acetylation in human colorectal carcinoma. Carcinogenesis. 2001;22:187–191. doi: 10.1093/carcin/22.1.187. [DOI] [PubMed] [Google Scholar]
- 19.Khan SA, Davidson BR, Goldin RD, Heaton N, Karani J, Pereira SP, Rosenberg WM, Tait P, Taylor-Robinson SD, Thillainayagam AV, et al. British Society of Gastroenterology: Guidelines for the diagnosis and treatment of cholangiocarcinoma. An update Gut. 2012;61:1657–1669. doi: 10.1136/gutjnl-2011-301748. [DOI] [PubMed] [Google Scholar]
- 20.Jung M. Inhibitors of histone deacetylase as new anticancer agents. Curr Med Chem. 2001;8:1505–1511. doi: 10.2174/0929867013372058. [DOI] [PubMed] [Google Scholar]
- 21.Weber SM, Ribero D, O'Reilly EM, Kokudo N, Miyazaki M, Pawlik TM. Intrahepatic cholangiocarcinoma: Expert consensus statement. HPB. 2015;17:669–680. doi: 10.1111/hpb.12441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, Pawlik TM, Gores GJ. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60:1268–1289. doi: 10.1016/j.jhep.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 23.Richon VM, Sandhoff TW, Rifkind RA, Marks PA. Histone deacetylase inhibitor selectively induces p21WAF1 expression and gene-associated histone acetylation. Proc Natl Acad Sci USA. 2000;97:10014–10019. doi: 10.1073/pnas.180316197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yamaguchi J, Sasaki M, Sato Y, Itatsu K, Harada K, Zen Y, Ikeda H, Nimura Y, Nagino M, Nakanuma Y. Histone deacetylase inhibitor (SAHA) and repression of EZH2 synergistically inhibit proliferation of gallbladder carcinoma. Cancer Sci. 2010;101:355–362. doi: 10.1111/j.1349-7006.2009.01387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sachweh MC, Drummond CJ, Higgins M, Campbell J, Laín S. Incompatible effects of p53 and HDAC inhibition on p21 expression and cell cycle progression. Cell Death Dis. 2013;4:e533. doi: 10.1038/cddis.2013.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Emori T, Kitamura K, Okazaki K. Nuclear Smad7 overexpressed in mesenchymal cells acts as a transcriptional corepressor by interacting with HDAC-1 and E2F to regulate cell cycle. Biol Open. 2012;1:247–260. doi: 10.1242/bio.2012463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li L, Dai HJ, Ye M, Wang SL, Xiao XJ, Zheng J, Chen HY, Luo YH, Liu J. Lycorine induces cell-cycle arrest in the G0/G1 phase in K562 cells via HDAC inhibition. Cancer Cell Int. 2012;12(49) doi: 10.1186/1475-2867-12-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Porter AG, Jänicke RU. Emerging roles of caspase-3 in apoptosis. Cell Death Differ. 1999;6:99–104. doi: 10.1038/sj.cdd.4400476. [DOI] [PubMed] [Google Scholar]
- 29.Laulier C, Lopez BS. The secret life of Bcl-2: Apoptosis-independent inhibition of DNA repair by Bcl-2 family members. Mutat Res. 2012;751:247–257. doi: 10.1016/j.mrrev.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 30.Sinha K, Das J, Pal PB, Sil PC. Oxidative stress: The mitochondria-dependent and mitochondria-independent pathways of apoptosis. Arch Toxicol. 2013;87:1157–1180. doi: 10.1007/s00204-013-1034-4. [DOI] [PubMed] [Google Scholar]
- 31.Candé C, Cohen I, Daugas E, Ravagnan L, Larochette N, Zamzami N, Kroemer G. Apoptosis-inducing factor (AIF): A novel caspase-independent death effector released from mitochondria. Biochimie. 2002;84:215–222. doi: 10.1016/S0300-9084(02)01374-3. [DOI] [PubMed] [Google Scholar]
- 32.Scott RE. Differentiation, differentiation/gene therapy and cancer. Pharmacol Ther. 1997;73:51–65. doi: 10.1016/S0163-7258(96)00120-9. [DOI] [PubMed] [Google Scholar]
- 33.Deubzer HE, Ehemann V, Westermann F, Heinrich R, Mechtersheimer G, Kulozik AE, Schwab M, Witt O. Histone deacetylase inhibitor Helminthosporium carbonum (HC)-toxin suppresses the malignant phenotype of neuroblastoma cells. Int J Cancer. 2008;122:1891–1900. doi: 10.1002/ijc.23295. [DOI] [PubMed] [Google Scholar]