Abstract
Acquisition of tamoxifen resistance (TR) during anti-estrogenic therapy using tamoxifen is a major obstacle in the treatment of estrogen receptor (ER)-positive breast cancer. As a biguanide derivative, metformin is commonly used to treat type II diabetes. It has recently emerged as a potential anticancer agent. The objective of the present study was to investigate the anticancer activity of metformin in relation to ERα expression and its signaling pathway in ERα-positive MCF-7 and MDA-MB-361 breast cancer cells as well as TR MCF-7 breast cancer cells. Metformin inhibited both protein and mRNA levels of ERα in the presence or absence of estrogen (E2) in the MCF-7, TR MCF-7 and MDA-MB-361 cells. Metformin repressed E2-inducible estrogen response element (ERE) luciferase activity, protein levels and mRNA levels of E2/ERα-regulated genes [including c-Myc, cyclin D1, progesterone receptor (PR) and pS2] to a greater degree than tamoxifen, resulting in inhibition of cell proliferation of MCF-7, TR MCF-7 and MDA-MB-361 cells. Collectively, our results suggest that one of the anticancer mechanisms of metformin could be attributable to the repression of expression and transcriptional activity of ERα. Metformin may be a good therapeutic agent for treating ERα-positive breast cancer by inhibiting the expression and function of ERα. In addition, metformin may be useful to treat tamoxifen-resistant breast cancer.
Keywords: estrogen receptor, tamoxifen resistance, metformin, estrogen response element, breast cancer, anti-estrogen therapy
Introduction
Estrogen receptor (ER) is an important prognostic marker and therapeutic target of breast cancer. There are two classes of ER: ERα and ERβ (1). ERα is predominantly expressed in breast ductal epithelial cells. It plays a crucial role in both mammary carcinogenesis and breast cancer progression (2,3). ERα is a member of the nuclear receptor superfamily of transcription factors whose activity is primarily regulated by estrogen (E2) binding. It regulates the transcription of target genes (4,5). ERα-positive breast cancer accounts for 70% of all breast cancer cases. Patients with these tumors are candidates for anti-estrogen therapy after surgical treatment. Such therapy is through blockage of binding of E2/ERα with selective ER modulators (SERMs) such as tamoxifen or by inhibiting E2 biosynthesis using aromatase inhibitors (AIs) (6). Only 60% of all ERα-positive breast cancers are responsive to tamoxifen. Unfortunately, the majority of these patients who do respond well initially often develop resistance to tamoxifen therapy and have relapse during their clinical courses (7). Although acquisition of tamoxifen resistance (TR) is due to a variety of factors, the mechanisms underlying this phenomenon remain poorly understood.
As a biguanide derivative, metformin (1,1-dimethylbiguanide hydrochloride) can suppress insulin levels (8), but increase insulin sensitivity of peripheral tissues (9). Accordingly, it has been approved to treat type II diabetes mellitus. Notably, several meta-analyses recently confirmed that metformin therapy could reduce the incidence of cancers, including breast and colorectal cancer, hepatocarcinoma and cancer-related mortality (10–14). Moreover, metformin has been reported to be able to inhibit proliferation and induce apoptosis in triple-negative breast cancer cell lines (15,16). The antitumor properties of metformin have been ascribed to its ability to activate adenosine monophosphate kinase (AMPK), thus, inhibiting the mammalian target of rapamycin (mTOR), a promoter of cell growth and proliferation (8,17,18). Based on these properties, metformin has gained increasing attention as a potential anticancer agent (19). Metformin has been shown to be able to reduce ER expression in endometrial tumors of women with type II diabetes mellitus (20). However, its effect on the expression and function of ERα in ERα-positive breast cancers regardless of diabetes is currently unclear. Therefore, the objective of the present study was to investigate the anticancer activity of metformin in relation to ERα expression and its signaling pathway in ERα-positive MCF-7 and MDA-MB-361 breast cancer cells, and TR MCF-7 breast cancer cells. Notably, it was found that metformin may be more effective at inhibiting ERα signaling by estrogenic stimulation compared to tamoxifen for ERα-positive breast cancers and that metformin may be an effective therapeutic agent for treating tamoxifen-resistant breast cancer.
Materials and methods
Cell lines and reagents
Human breast cancer cell lines MCF-7 and MDA-MB-361 were purchased from the American Type Culture Collection (ATCC; Manassas, VA, USA). MCF-7 cells were cultured in RPMI-1640 medium supplemented with 10% fetal bovine serum (FBS), 100 U/ml penicillin and 100 µg/ml streptomycin (Gibco, Grand Island, NY, USA). MDA-MB-361 cells were cultured in Leibovitz's L-15 medium (Gibco) supplemented with 20% FBS at 37°C in a 5% CO2 humidified incubator. Metformin, 17β-estradiol (E2) and 4-hydroxytamoxifen (4-OHT) were purchased from Sigma (St. Louis, MO, USA). Metformin was dissolved in sterile water. E2 and 4-OHT were dissolved in ethanol. They were immediately stored at −80°C.
Establishment of the tamoxifen-resistant (TR) MCF-7 cell line
MCF-7 cells were cultured in phenol red-free RPMI-1640 medium supplemented with 10% charcoal stripped FBS (PAA Laboratories, Morningside, Australia) to deplete estrogen. The tamoxifen-resistant (TR) MCF-7 cell line was established from MCF-7 cells following continuous exposure to 10−6 M 4-OHT, an active metabolite of tamoxifen (21,22). Under these conditions, the growth rates of MCF-7 cells were reduced. However, after ~2 months, cell growth was gradually increased, indicating an acquisition of resistance to growth inhibition of 4-OHT. Designated TR MCF-7 cells were cultured for an additional 4 months in medium containing 4-OHT before characterization studies.
Isolation of RNA and quantitative real-time RT-PCR (RT-qPCR)
Total RNA was isolated using the RNeasy Mini kit (Qiagen, Hilden, Germany). For cDNA synthesis, 1 µg of total RNA was subjected to reverse transcription-polymerase chain reaction (RT-PCR) assay using CycleScript RT PreMix kit (Bioneer Corporation, Daejeon, Korea). RT-qPCR was performed with Power SYBR-Green PCR Master Mix on an ABI 7300 real-time PCR system (both from Applied Biosystems, Warrington, UK) using the following cycling conditions: 50°C for 2 min, 95°C for 5 min, followed by 40 cycles of 95°C for 30 sec, 55°C for ERα and pS2 or 60°C for cyclin D1 for 30 sec, 72°C for 30 sec. The following primers were used: 5′-AGCACCCAGTGAAGCTACT-3′ (ERα-forward) and 5′-TAGGGCACACAAACTCCT-3′ (ERα-reverse); 5′-TATGAATCACTTCTGCAGTGAG-3′ (pS2-forward) and 5′-GAGCGTTAGATAACATTTGCC-3′ (pS2-reverse); 5′-CGCCCCACCCCTCCAG-3′ (cyclin D1-forward) and 5′-CCGCCCAGACCCTCAGACT-3′ (cyclin D1-reverse); and 5′-ATCATCCCTGCCTCTACTGG-3′ (forward) and 5′-CCCTCCGACGCCTGCTT-CAC-3′ (reverse) for GAPDH as internal standard. Cycle threshold values were normalized to those of GAPDH. The relative fold-change was calculated using the 2−ΔΔCt method.
Western blot analysis
Protein lysates were prepared with RIPA buffer (20 mM Tris-HCl pH 7.5, 2 mM EDTA, 150 mM NaCl, 1 mM sodium vanadate, 10 mM NaF, 2.5 mM sodium pyrophosphate, 1% sodium deoxycholate, 0.1% SDS, 1% NP-40) supplemented with protease inhibitor cocktail (Roche, Mannheim, Germany). Protein concentrations were determined using a BCA protein assay kit (Thermo Scientific, Rockford, IL, USA). Protein samples (30 µg) were resolved by SDS-PAGE and transferred onto polyvinylidene fluoride (PVDF) membranes (Bio-Rad Laboratories). Membranes were blocked with skim milk and incubated with the primary antibodies. Following washing, the membranes were incubated with horseradish peroxidase-conjugated anti-mouse or anti-rabbit secondary antibody and developed with ECL Plus Western Blot Detection System reagent (GE Healthcare Biosciences, Piscataway, NJ, USA). Rabbit anti-ERα (1:2,000) antibody was purchased from Millipore (Billerica, MA, USA). Mouse anti-cyclin D1 (1:1,000), rabbit anti-TFF1/pS2 (1:1,000), rabbit anti-phospho-AMPKα (Thr172, 1:1,000) and rabbit anti-AMPKα (1:1,000) antibodies were purchased from Cell Signaling Technology Inc. (Beverly, MA, USA). Mouse anti-c-Myc (1:1,000) and rabbit anti-progesterone receptor (PR) (1:1,000) antibodies were purchased from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA). A monoclonal anti-β-actin (1:5,000) antibody obtained from Sigma was used to determine protein loading. Protein levels were quantified using ImageJ software (NIH, Bethesda, MD, USA).
Cell proliferation assay
Cells were seeded into 12-well plates at a density of 5×104 cells/well (500 µl/well). After incubation for 24 h, the cells were treated with metformin, 4-OHT and E2 in estrogen-depleted RPMI-1640 medium and incubated for an additional 72 h. After that, the cells were trypsinized and counted after staining with trypan blue dye solution using the TC10™ Automated Cell Counter (Bio-Rad Laboratories). The number of viable cells in each well was calculated. Results are presented as relative percentage to the control of each group from three independent experiments in triplicates.
Luciferase assay
The transcriptional activity of ERα was analyzed by luciferase assay using pGL2-3X ERE TATA luc plasmid (Addgene, Cambridge MA, USA). Cells were seeded into 12-well plates and grown to confluency. After co-transfection with pGL2-3X ERE TATA luc and pRL-TK-luc control plasmid (Promega, Madison, WI, USA) using Lipofectamine 2000 reagent (Invitrogen, Carlsbad, CA, USA) for 24 h, the cells were treated with metformin, 4-OHT and E2 in estrogen-depleted RPMI-1640 medium. After an additional incubation for 24 h, luciferase activity was measured using the Dual-Luciferase reporter assay system (Promega) and normalized to pRL-TK-luc activity to correct for differences in transfection efficiency. Results are presented as fold-change relative to the control of each group from three independent experiments in triplicates.
Statistical analysis
Each experiment was performed independently at least three times. Data are presented as mean ± standard deviation for each experiment. Comparisons between two groups were performed using the Student's t-test. P<0.05 and P<0.01 were considered to indicate a statistically significant result.
Results
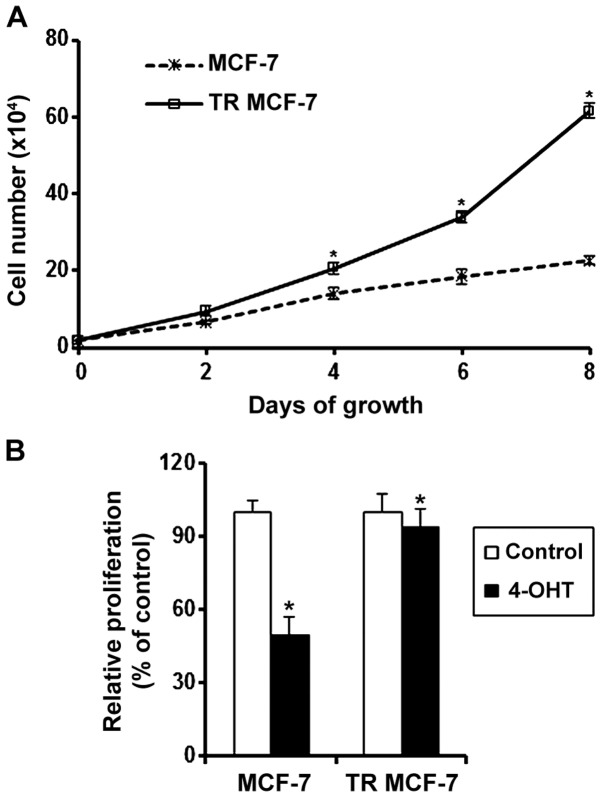
Effect of 4-OHT on the proliferation of MCF-7 and TR MCF-7 cells
To evaluate the acquisition of resistance to the anti-estrogenic action of 4-OHT, we measured the cell proliferation rate of proliferation MCF-7 and the TR MCF-7 cells every 2 days by counting cell numbers. The proliferation rate of proliferation TR MCF-7 cells was significantly higher than that of the MCF-7 cells in the presence of 4-OHT (Fig. 1A). We also determined the proliferation of MCF-7 and TR MCF-7 cells treated with 4-OHT or the control vehicle (Ctrl) for 5 days. The proliferation of the 4-OHT-treated MCF-7 cells was inhibited by 50% compared to that of the Ctrl cells. A slight decrease in the proliferation was observed in the 4-OHT-treated TR MCF-7 cells (Fig. 1B).
Figure 1.
Effect of 4-OHT on the proliferation of MCF-7 and TR MCF-7 cells. (A) MCF-7 and TR MCF-7 cells were seeded into 6-well plates at a density of 2×104 cells/well in estrogen-depleted RPMI-1640 medium in the presence of 4-OHT (10−6 M). Cell number was counted every 2 days by trypan blue staining. Data represent the mean ± SD of three independent experiments conducted in triplicates. P-value was calculated compared to the MCF-7 cells; *P<0.05. (B) MCF-7 and TR MCF-7 cells were treated with or without 4-OHT in estrogen-depleted RPMI-1640 medium for 5 days. Cell proliferation was determined by trypan blue staining. Data represent the mean ± SD of three independent experiments conducted in triplicates. P-value was calculated compared to the untreated Ctrl cells; *P<0.05.
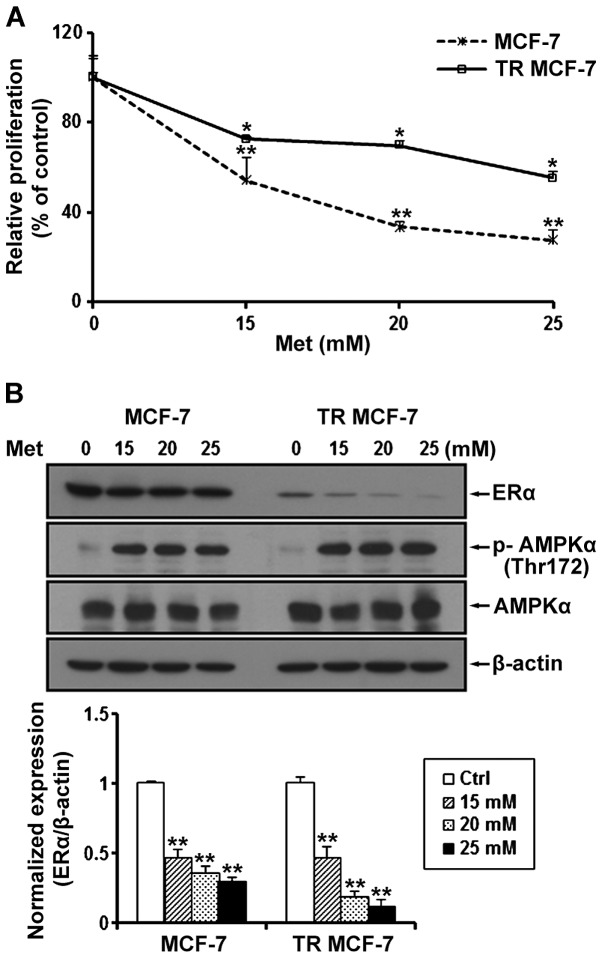
Metformin inhibits cell proliferation and ERα protein levels in MCF-7 and TR MCF-7 cells
We determined the proliferation of MCF-7 and TR MCF-7 cells treated with metformin at a concentration of 15, 20 and 25 mM for 72 h. Compared to the untreated control cells, metformin inhibited the cell proliferation of the MCF-7 and TR MCF-7 cells in a dose-dependent manner (Fig. 2A). Compared to the untreated cells, the cell proliferation of the MCF-7 and TR MCF-7 cells was inhibited 70 and 50%, respectively, by 25 mM metformin, indicating that the TR MCF-7 cells were less sensitive at the same concentration of metformin compared to the MCF-7 parental cells for the antiproliferative effect of metformin. Next, we performed western blot analysis to evaluate the effect of metformin on ERα protein levels. We found that the protein levels of ERα were reduced in a dose-dependent manner by treatment with 15, 20 and 25 mM metformin in both cell lines (Fig. 2B). The concentrations of metformin used in the present study are high, but to focus on the anticancer effects of metformin on TR MCF-7 cells, based on these results, subsequent experiments were carried out using 25 mM metformin. We also determined AMPKα phosphorylation (Thr172) and total AMPKα levels to demonstrate that metformin was present and active during our experiments.
Figure 2.
Metformin (Met) inhibits cell proliferation and expression of ERα in MCF-7 and TR MCF-7 cells. (A) Cells were treated with Met at a concentration of 15, 20 and 25 mM for 72 h in each culture medium supplemented with 3% FBS. Cell proliferation was measured by cell counting using trypan blue staining. (B) The expression levels of ERα, phospho(p)-AMPKα (Thr172) and total AMPKα were examined by western blotting. β-actin was evaluated as a loading control. All data represent the mean ± SD of three independent experiments conducted in triplicates. P-value was calculated compared to the untreated Ctrl cells; *P<0.05 and **P<0.01.
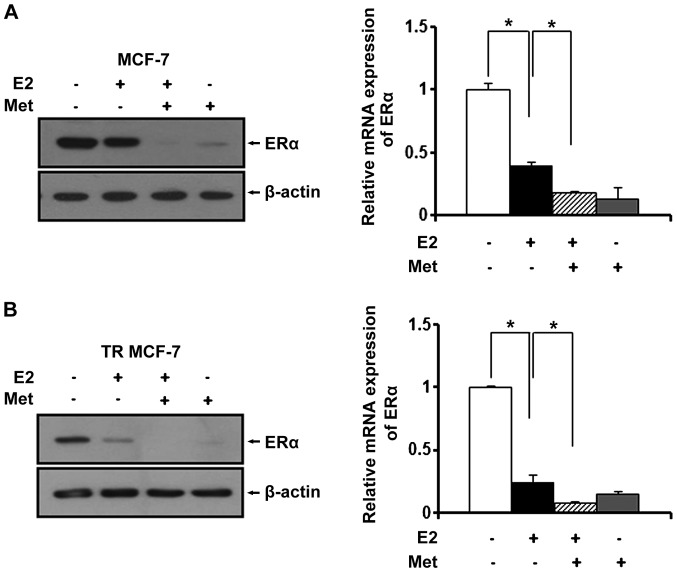
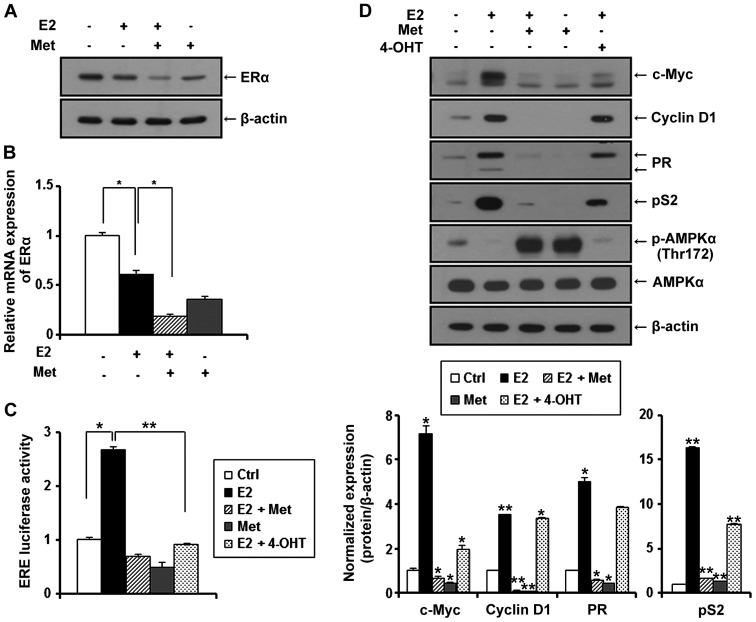
Metformin inhibits the expression of ERα in MCF-7 and TR MCF-7 cells under E2
Since estrogen (E2) is a stimulatory signal for breast cancer development and progression, we treated the MCF-7 and TR MCF-7 cells with metformin in an E2-exposed physiological condition. After treatment with E2, changes in the ERα protein levels were evaluated by western blot analysis. E2 has been reported to be able to rapidly reduce the levels of ERα protein transiently expressed in cells (23). As shown in Fig. 3A and B (left panels), the E2-treated cells had decreased ERα protein levels compared to these levels in the untreated control cells. The protein levels of ERα were decreased more significantly after treatment with metformin. Based on RT-qPCR, we found that metformin also repressed the E2-induced mRNA level of ERα in the MCF-7 cells (0.6-fold decrease compared to E2-treated only cells) and the TR MCF-7 cells (0.7-fold decrease compared to E2-treated only cells) (Fig. 3A and B, right panels).
Figure 3.
Metformin (Met) inhibits expression of ERα in the MCF-7 and TR MCF-7 cells under E2. (A) MCF-7 and (B) TR MCF-7 cells were treated with Met (25 mM) in the presence of E2 (100 nM) for 48 h in estrogen-depleted RPMI-1640 medium containing 3% charcoal stripped FBS. Immunoblots were probed with the anti-ERα antibody (left panels). β-actin was evaluated as a loading control. ERα mRNA levels were determined by RT-qPCR after treatment of Met and E2 for 24 h (right panels). Data represent the mean ± SD of three independent experiments conducted in triplicates; *P<0.05.
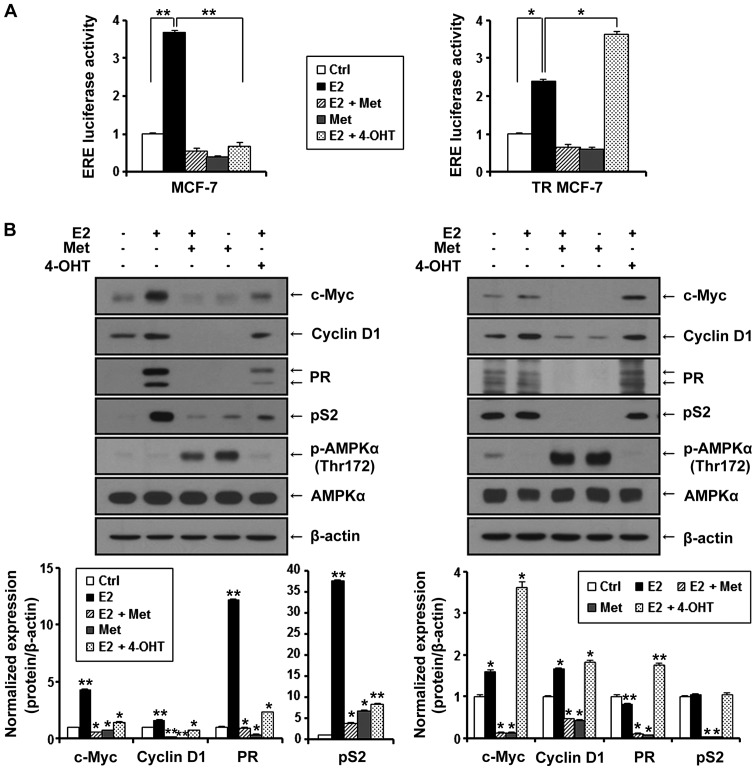
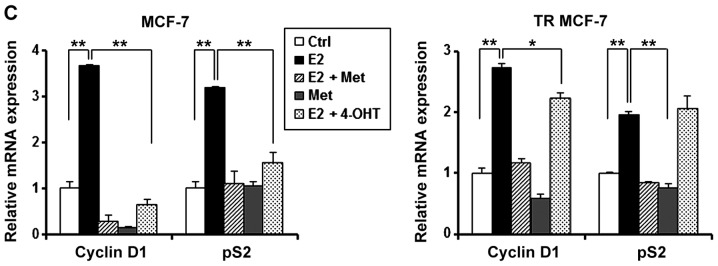
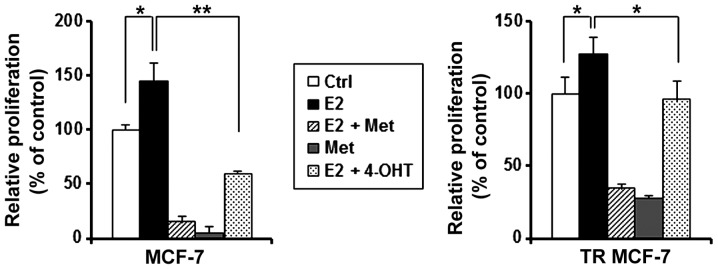
Metformin inhibits E2-inducible ERE luciferase activity and the expression of ERα target genes in MCF-7 and TR MCF-7 cells
ERα is known to interact with the estrogen response element (ERE) site of target genes and activate the transcription of regulated genes in response to E2. Therefore, we evaluated the effect of metformin on the transcriptional activity of ERα compared to anti-estrogenic agent 4-OHT. MCF-7 and TR MCF-7 cells were transiently co-transfected with E2-inducible luciferase reporter gene (pGL2-3X ERE TATA luc) and pRL-TK-luc control plasmid. Transfected cells were treated with metformin and 4-OHT under stimulation of E2 or with only metformin for 24 h. As shown in Fig. 4A, E2-induced ERE luciferase activity was inhibited by the treatment of metformin in both the MCF-7 and TR MCF-7 cells. Compared to the E2 only-treated cells, metformin (85% decrease) was as effective as 4-OHT (81% decrease) in regulating the transcriptional activity of ERα in MCF-7 cells. However, 4-OHT stimulated the ERE luciferase activity in the TR MCF-7 cells. Consequently, we compared the inhibitory effect of metformin and 4-OHT on cellular levels of proteins encoded by E2/ERα-regulated genes, including c-Myc, cyclin D1, PR and pS2 in both the MCF-7 (Fig. 4B, left) and the TR MCF-7 (Fig. 4B, right) cells. Metformin inhibited the protein levels of E2-induced c-Myc, cyclin D1, PR and pS2 to a greater extent than 4-OHT. However, 4-OHT exhibited no inhibitory effect on the expression of these target genes in the TR MCF-7 cells. AMPKα phosphorylation (Thr172) and total AMPKα levels were also examined by western blotting. In addition, then we proceeded for RT-qPCR. E2-induced mRNA levels of ERα target genes, cyclin D1 and pS2 were inhibited by the treatment of metformin (Fig. 4C). These results suggest that metformin inhibited ERα-mediated transcription levels of its target genes through inhibiting the transcriptional activity of ERα activated by E2 in both the MCF-7 and TR MCF-7 cells.
Figure 4.
Metformin (Met) inhibits E2-inducible ERE luciferase activity and expression of ERα target genes in MCF-7 and TR MCF-7 cells. (A) Transfected cells were treated with Met (25 mM) and 4-OHT (10−6 M) in the presence of E2 (100 nM) and ERE luciferase assay was performed. (B) MCF-7 (left) and TR MCF-7 (right) cells were treated with Met and 4-OHT in the presence of E2 for 48 h in estrogen-depleted RPMI-1640 medium containing 3% charcoal stripped FBS. The protein levels of c-Myc, cyclin D1, PR, pS2, phospho(p)-AMPKα (Thr172) and total AMPKα were examined by western blotting. β-actin was evaluated as a loading control. Protein expression levels normalized to β-actin are presented. Data represent the mean ± SD of three independent experiments. P-value was calculated compared to untreated Ctrl or E2-treated cells; *P<0.05 and **P<0.01. (C) RT-qPCR was conducted to assess the mRNA levels of ERα target genes, cyclin D1 and pS2. All data represent the mean ± SD of three independent experiments conducted in triplicates; *P<0.05 and **P<0.01.
Metformin inhibits E2-stimulated cell proliferation of the MCF-7 and TR MCF-7 cells
Cell counting using trypan blue staining was performed to compare the antiproliferative effect of metformin and 4-OHT on E2-treated MCF-7 and TR MCF-7 cells. As shown in Fig. 5, metformin inhibited the cell proliferation stimulated by estrogen in both the MCF-7 and TR MCF-7 cells compared to the E2 only-treated cells. Metformin inhibited cell proliferation of MCF-7 cells (90 vs. 60% decrease compared to E2 only-treated cells) and TR MCF-7 cells (74 vs. 25% decrease compared to E2 only-treated cells) to a greater extend than 4-OHT. These results suggest that metformin is likely to have an inhibitory effect on the proliferation of MCF-7 and TR MCF-7 cells through the inhibitory function of ERα.
Figure 5.
Metformin (Met) inhibits E2-induced cell proliferation in MCF-7 and TR MCF-7 cells. MCF-7 and TR MCF-7 cells were treated with Met (25 mM) and 4-OHT (10−6 M) in the presence of E2 (100 nM) for 72 h in estrogen-depleted RPMI-1640 medium containing 3% charcoal stripped FBS. Cell proliferation assay by cell counting using trypan blue staining was performed. Data represent the mean ± SD of three independent experiments conducted in triplicates; *P<0.05 and **P<0.01.
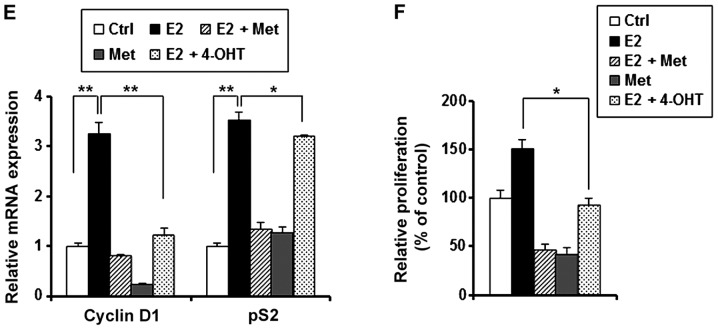
Metformin inhibits E2-induced expression, function of ERα and cell proliferation of MDA-MB-361 breast cancer cells
In general, ERα and HER2 co-expression in breast cancer may result in the treatment failure of tamoxifen therapy. To properly evaluate the clinical potential of metformin in ERα- and HER2-positive breast cancer (luminal B subtype), we investigated the anticancer effect of metformin using the MDA-MB-361 (ERα+/HER2+) cell line. Similar to our results in the MCF-7 and TR MCF-7 cells, metformin reduced the ERα protein (Fig. 6A) and mRNA levels (Fig. 6B). As shown in Fig. 6C, metformin and 4-OHT resulted in a 75 and 67% decrease in E2-induced ERE luciferase activity, respectively. In addition, E2-induced expression of c-Myc, cyclin D1, PR and pS2 were inhibited by the treatment of metformin. Moreover, we showed AMPKα phosphorylation (Thr172) and total AMPKα levels to demonstrate that metformin was present and active during our experiments (Fig. 6D). Next, we performed RT-qPCR. It was found that E2-induced mRNA levels of cyclin D1 and pS2 were inhibited by the treatment of metformin (Fig. 6E). Metformin resulted in 70% inhibition of the proliferation of MDA-MB-361 cells compared to cells treated by E2 only (Fig. 6F).
Figure 6.
Metformin (Met) inhibits E2-induced expression, function of ERα and cell proliferation in MDA-MB-361 breast cancer cells. (A) The protein levels of ERα were examined by western blotting. β-actin was evaluated as a loading control. (B) ERα mRNA levels were determined by RT-qPCR. (C) ERE luciferase assay was performed. (D) The protein levels of c-Myc, cyclin D1, PR, pS2, phospho(p)-AMPKα (Thr172) and total AMPKα were examined by western blotting. β-actin was evaluated as a loading control. Protein expression levels normalized with β-actin are presented. Data represent the mean ± SD of three independent experiments. P-value was calculated compared to the untreated Ctrl cells or E2-treated cells; *P<0.05 and **P<0.01. (E) RT-qPCR was conducted to assess mRNA levels of cyclin D1 and pS2. (F) Cell proliferation was measured by trypan blue staining. All data represent the mean ± SD of three independent experiments conducted in triplicates; *P<0.05, **P<0.01.
Discussion
Estrogen (E2) plays a vital role in the pathogenesis of breast cancer through estrogen receptor α (ERα) (24). Blocking the E2/ERα signaling pathway is the first-line therapeutic strategy for patients with ERα-positive breast cancer. Although anti-estrogenic therapy using tamoxifen is still an important and major modality to manage ERα-positive breast cancer (25), its usefulness is greatly limited by de novo and acquired resistance (26). Therefore, new therapeutic strategies are required to overcome tamoxifen resistance (TR). In the present study, we showed the effectiveness of metformin by targeting ERα using ERα-positive as well as tamoxifen-resistant breast cancer cells, thus providing a possible mechanism underlying the anticancer effect of metformin.
Numerous in vitro and in vivo studies have demonstrated that metformin treatment can result in the inhibition of cancer cell growth (27–30). A variety of mechanisms have been invoked to explain the antitumor effect of metformin, including activation of AMPK and inhibition of mTOR (31,32). We focused on research related to the expression and signaling pathway of ERα. Our results revealed that metformin inhibited E2-induced expression, ERE luciferase activity, expression of ERα target genes, and cell proliferation of MCF-7 and TR MCF-7 cells. Collectively, our data indicated that the anticancer effect of metformin could be due to the repression of expression and transcriptional function of ERα.
In addition to MCF-7 and TR MCF-7 breast cancer cells, we also assessed the antiproliferative effect of metformin on MDA-MB-361 (ERα+/HER2+) breast cancer cells. HER2 is a transmembrane tyrosine kinase and a member of the human epidermal growth factor receptor (EGFR) family. It leads to the activation of the signaling pathway that promotes cell proliferation, migration, and survival. HER2 amplification and/or overexpression in breast cancer are correlated to poor patient survival or resistance to tamoxifen therapy (33–37). Consistent with our results in the MCF-7 and TR MCF-7 breast cancer cells, metformin also inhibited E2-induced expression and function of ERα as well as the cell proliferation of MDA-MB-361 cells. E2-induced ERE luciferase activity, expression of ERα target genes, and cell proliferation were also inhibited by tamoxifen in MCF-7 cells, although the effect of tamoxifen was less than that of metformin. Overall, metformin inhibited the ERE luciferase activity, the expression of ERα target genes, and the cell proliferation to a greater extend than 4-OHT in the MCF-7, TR MCF-7 and MDA-MB-361 cells. These effects could be due to the fact that 4-OHT blocked the binding of E2/ERα without suppressing the expression of ERα itself, suggesting that treatment with metformin may be useful for patients with ERα-positive breast cancer.
In conclusion, these results suggest that metformin exhibited a superior antiproliferative effect by inhibiting ERα signaling than tamoxifen in ERα-positive MCF-7, TR MCF-7 and MDA-MB-361 cells. Currently, there is no alternative standard treatment for tamoxifen-resistant breast tumors except aromatase inhibitors. Therefore, we suggest that metformin may be one of the effective therapeutic agents for treating tamoxifen-resistant breast cancer. Moreover, combination strategies with metformin may be useful for enhancing the treatment efficacy of other cytotoxic chemotherapies or targeted therapies (38). Further experiments including animal studies and clinical trials are warranted.
Acknowledgments
The present study was supported by a grant (HI14C3405) from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare (MOHW), Republic of Korea.
References
- 1.Ali S, Coombes RC. Estrogen receptor alpha in human breast cancer: Occurrence and significance. J Mammary Gland Biol Neoplasia. 2000;5:271–281. doi: 10.1023/A:1009594727358. [DOI] [PubMed] [Google Scholar]
- 2.Hall JM, Couse JF, Korach KS. The multifaceted mechanisms of estradiol and estrogen receptor signaling. J Biol Chem. 2001;276:36869–36872. doi: 10.1074/jbc.R100029200. [DOI] [PubMed] [Google Scholar]
- 3.Couse JF, Korach KS. Estrogen receptor null mice: What have we learned and where will they lead us? Endocr Rev. 1999;20:358–417. doi: 10.1210/edrv.20.3.0370. [DOI] [PubMed] [Google Scholar]
- 4.Colditz GA. Relationship between estrogen levels, use of hormone replacement therapy, and breast cancer. J Natl Cancer Inst. 1998;90:814–823. doi: 10.1093/jnci/90.11.814. [DOI] [PubMed] [Google Scholar]
- 5.Hankinson SE, Colditz GA, Willett WC. Towards an integrated model for breast cancer etiology: The lifelong interplay of genes, lifestyle, and hormones. Breast Cancer Res. 2004;6:213–218. doi: 10.1186/bcr921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uray IP, Brown PH. Clinical Cancer Prevention. Springer; 2011. Chemoprevention of hormone receptor-negative breast cancer: New approaches needed; pp. 147–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osborne CK. Tamoxifen in the treatment of breast cancer. N Engl J Med. 1998;339:1609–1618. doi: 10.1056/NEJM199811263392207. [DOI] [PubMed] [Google Scholar]
- 8.Shaw RJ, Lamia KA, Vasquez D, Koo SH, Bardeesy N, Depinho RA, Montminy M, Cantley LC. The kinase LKB1 mediates glucose homeostasis in liver and therapeutic effects of metformin. Science. 2005;310:1642–1646. doi: 10.1126/science.1120781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bailey CJ, Turner RC. Metformin. N Engl J Med. 1996;334:574–579. doi: 10.1056/NEJM199602293340906. [DOI] [PubMed] [Google Scholar]
- 10.Bowker SL, Majumdar SR, Veugelers P, Johnson JA. Increased cancer-related mortality for patients with type 2 diabetes who use sulfonylureas or insulin. Diabetes Care. 2006;29:254–258. doi: 10.2337/diacare.29.02.06.dc05-1558. [DOI] [PubMed] [Google Scholar]
- 11.Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD. Metformin and reduced risk of cancer in diabetic patients. BMJ. 2005;330:1304–1305. doi: 10.1136/bmj.38415.708634.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Decensi A, Puntoni M, Goodwin P, Cazzaniga M, Gennari A, Bonanni B, Gandini S. Metformin and cancer risk in diabetic patients: A systematic review and meta-analysis. Cancer Prev Res. 2010;3:1451–1461. doi: 10.1158/1940-6207.CAPR-10-0157. [DOI] [PubMed] [Google Scholar]
- 13.Bosco JLF, Antonsen S, Sørensen HT, Pedersen L, Lash TL. Metformin and incident breast cancer among diabetic women: A population-based case-control study in Denmark. Cancer Epidemiol Biomarkers Prev. 2011;20:101–111. doi: 10.1158/1055-9965.EPI-10-0817. [DOI] [PubMed] [Google Scholar]
- 14.Beck E, Scheen AJ. Metformin, an antidiabetic molecule with anti-cancer properties. Rev Med Liege. 2013;68:444–449. In French. [PubMed] [Google Scholar]
- 15.Liu B, Fan Z, Edgerton SM, Deng XS, Alimova IN, Lind SE, Thor AD. Metformin induces unique biological and molecular responses in triple negative breast cancer cells. Cell Cycle. 2009;8:2031–2040. doi: 10.4161/cc.8.13.8814. [DOI] [PubMed] [Google Scholar]
- 16.Jiralerspong S, Gonzalez-Angulo AM, Hung M-C. Expanding the arsenal: Metformin for the treatment of triple-negative breast cancer? Cell Cycle. 2009;8:2681–2684. doi: 10.4161/cc.8.17.9502. [DOI] [PubMed] [Google Scholar]
- 17.Marx J. Medicine. Cancer-suppressing enzyme adds a link to type 2 diabetes. Science. 2005;310:1259–1259. doi: 10.1126/science.310.5752.1259a. [DOI] [PubMed] [Google Scholar]
- 18.Goodwin PJ, Pritchard KI, Ennis M, Clemons M, Graham M, Fantus IG. Insulin-lowering effects of metformin in women with early breast cancer. Clin Breast Cancer. 2008;8:501–505. doi: 10.3816/CBC.2008.n.060. [DOI] [PubMed] [Google Scholar]
- 19.Dowling RJ, Goodwin PJ, Stambolic V. Understanding the benefit of metformin use in cancer treatment. BMC Med. 2011;9:33. doi: 10.1186/1741-7015-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Markowska A, Pawałowska M, Filas V, Korski K, Gryboś M, Sajdak S, Olejek A, Bednarek W, Spiewankiewicz B, Lubin J, et al. Does Metformin affect ER, PR, IGF-1R, β-catenin and PAX-2 expression in women with diabetes mellitus and endometrial cancer? Diabetol Metab Syndr. 2013;5:76. doi: 10.1186/1758-5996-5-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoo YA, Kim YH, Kim JS, Seo JH. The functional implications of Akt activity and TGF-beta signaling in tamoxifen-resistant breast cancer. Biochim Biophys Acta. 2008;1783:438–447. doi: 10.1016/j.bbamcr.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 22.Knowlden JM, Hutcheson IR, Jones HE, Madden T, Gee JM, Harper ME, Barrow D, Wakeling AE, Nicholson RI. Elevated levels of epidermal growth factor receptor/c-erbB2 heterodimers mediate an autocrine growth regulatory pathway in tamoxifen-resistant MCF-7 cells. Endocrinology. 2003;144:1032–1044. doi: 10.1210/en.2002-220620. [DOI] [PubMed] [Google Scholar]
- 23.Dauvois S, Danielian PS, White R, Parker MG. Antiestrogen ICI 164,384 reduces cellular estrogen receptor content by increasing its turnover. Proc Natl Acad Sci USA. 1992;89:4037–4041. doi: 10.1073/pnas.89.9.4037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clark GM, Osborne CK, McGuire WL. Correlations between estrogen receptor, progesterone receptor, and patient characteristics in human breast cancer. J Clin Oncol. 1984;2:1102–1109. doi: 10.1200/JCO.1984.2.10.1102. [DOI] [PubMed] [Google Scholar]
- 25.Honig SF. Tamoxifen for the reduction in the incidence of breast cancer in women at high risk for breast cancer. Ann NY Acad Sci. 2001;949:345–348. doi: 10.1111/j.1749-6632.2001.tb04043.x. [DOI] [PubMed] [Google Scholar]
- 26.Osborne CK, Schiff R. Mechanisms of endocrine resistance in breast cancer. Annu Rev Med. 2011;62:233–247. doi: 10.1146/annurev-med-070909-182917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zakikhani M, Dowling R, Fantus IG, Sonenberg N, Pollak M. Metformin is an AMP kinase-dependent growth inhibitor for breast cancer cells. Cancer Res. 2006;66:10269–10273. doi: 10.1158/0008-5472.CAN-06-1500. [DOI] [PubMed] [Google Scholar]
- 28.Dowling RJ, Zakikhani M, Fantus IG, Pollak M, Sonenberg N. Metformin inhibits mammalian target of rapamycin-dependent translation initiation in breast cancer cells. Cancer Res. 2007;67:10804–10812. doi: 10.1158/0008-5472.CAN-07-2310. [DOI] [PubMed] [Google Scholar]
- 29.Ben Sahra I, Laurent K, Loubat A, Giorgetti-Peraldi S, Colosetti P, Auberger P, Tanti JF, Le Marchand-Brustel Y, Bost F. The antidiabetic drug metformin exerts an antitumoral effect in vitro and in vivo through a decrease of cyclin D1 level. Oncogene. 2008;27:3576–3586. doi: 10.1038/sj.onc.1211024. [DOI] [PubMed] [Google Scholar]
- 30.Buzzai M, Jones RG, Amaravadi RK, Lum JJ, DeBerardinis RJ, Zhao F, Viollet B, Thompson CB. Systemic treatment with the antidiabetic drug metformin selectively impairs p53-deficient tumor cell growth. Cancer Res. 2007;67:6745–6752. doi: 10.1158/0008-5472.CAN-06-4447. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez-Angulo AM, Meric-Bernstam F. Metformin: A therapeutic opportunity in breast cancer. Clin Cancer Res. 2010;16:1695–1700. doi: 10.1158/1078-0432.CCR-09-1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, et al. Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest. 2001;108:1167–1174. doi: 10.1172/JCI13505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gullick WJ, Berger MS, Bennett PL, Rothbard JB, Waterfield MD. Expression of the c-erbB-2 protein in normal and transformed cells. Int J Cancer. 1987;40:246–254. doi: 10.1002/ijc.2910400221. [DOI] [PubMed] [Google Scholar]
- 34.King CR, Kraus MH, Aaronson SA. Amplification of a novel v-erbB-related gene in a human mammary carcinoma. Science. 1985;229:974–976. doi: 10.1126/science.2992089. [DOI] [PubMed] [Google Scholar]
- 35.Riese DJ, II, van Raaij TM, Plowman GD, Andrews GC, Stern DF. The cellular response to neuregulins is governed by complex interactions of the erbB receptor family. Mol Cell Biol. 1995;15:5770–5776. doi: 10.1128/MCB.15.10.5770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235:177–182. doi: 10.1126/science.3798106. [DOI] [PubMed] [Google Scholar]
- 37.Ross JS, Fletcher JA. The HER-2/neu oncogene in breast cancer: Prognostic factor, predictive factor, and target for therapy. Stem Cells. 1998;16:413–428. doi: 10.1002/stem.160413. [DOI] [PubMed] [Google Scholar]
- 38.Kim J, Lee J, Kim C, Choi J, Kim A. Anti-cancer effect of metformin by suppressing signaling pathway of HER2 and HER3 in tamoxifen-resistant breast cancer cells. Tumour Biol. 2015 Nov 18; doi: 10.1007/s13277-015-4440-9. Epub ahead of print. [DOI] [PubMed] [Google Scholar]