Abstract
Physician–scientists and scientists in all the health professions are vital members of the U.S. biomedical workforce, but their numbers at academic health centers are declining. Mentorship has been identified as a key component in retention of faculty members at academic health centers. Effective mentoring may promote the retention of clinician–scientists in the biomedical workforce. The authors describe a holistic institutional mentoring program to support junior faculty members engaged in clinical and translational science at the University of Utah. The clinical and translational scholars (CATS) program leverages the resources of the institution, including the Center for Clinical and Translational Science, to augment departmental resources to support junior faculty investigators and uses a multilevel mentoring matrix that includes self, senior, scientific, peer, and staff mentorship. Begun in the Department of Pediatrics, the program was expanded in 2013 to include all departments in the school of medicine and the health sciences. During the two-year program, scholars learn management essentials and have leadership training designed to develop principal investigators. Of the 86 program participants since fiscal year 2008, 92% have received extramural awards, 99% remain in academic medicine, and 95% remain at the University of Utah. The CATS program has also been associated with increased inclusion of women and underrepresented minorities in the institutional research enterprise. The CATS program manifests institutional collaboration and coordination of resources, which have benefited faculty members and the institution. The model can be applied to other academic health centers to support and sustain the biomedical workforce.
The physician–scientist was recognized as an endangered species more than three decades ago.1,2 A recent report of the National Institutes of Health (NIH) Physician–Scientist Workforce Working Group noted that the proportion of physician–scientists and other clinician–scientists in the biomedical workforce has decreased steadily since the 1970s.3 The loss of physician–scientists is disturbing in this period of unprecedented knowledge expansion in biomedical sciences. The clinician–scientist is uniquely positioned to translate basic science discoveries and knowledge generated through clinical investigation into evidence-based treatments for patients.
Mentorship is recognized as vital in the development of physician–scientists. However, a simple dyadic model is not a solution for all investigators4 and may be particularly challenging for translational scientists whose work crosses disciplinary and departmental boundaries. Finding quality mentoring is also difficult for women and members of underrepresented minority (URM) groups given the relative paucity of these individuals at senior levels in academic health centers.5–8 Solutions to the decline in physician–scientists include developing a robust infrastructure for mentorship and training to support those engaged in clinical and translational science.9
We describe the holistic clinical and translational scholars (CATS) mentoring program to develop principal investigators at the University of Utah. In this article, we provide the program framework, describe the Matrix Mentoring Model (MMM), and report outcomes for junior faculty participants.
Description of the CATS Mentoring Program
The CATS program offers two years of holistic mentorship that supports junior faculty members engaged in biomedical research in transitioning to principal investigators.
The CATS program was developed in the Department of Pediatrics in fiscal year (FY) 2008 and also supported child health investigators in the departments of obstetrics–gynecology and surgery and in the college of nursing. The program resulted in an increase in the award rate for career development grants for these child health scholars from 10/14 (71%) of those who applied for grants in FYs 2004–2007 to 29/30 (97%) of those who applied in FYs 2008–2015 (P = .03 by chi-square).
On the basis of the success of the pediatric CATS program, in FY 2013 we extended the program to include all departments in the school of medicine and the health sciences including the school of dentistry and colleges of health, nursing, and pharmacy, with a total of 1,830 faculty members, 693 in the tenure line.
The program is housed in the health sciences office of academic affairs and faculty development (AA/FD) and supported through the senior vice president. There is no charge for scholar participation. The AA/FD collaborates with academic departments, University of Utah Human Resources, and the Utah Center for Clinical and Translational Science (CCTS), which is part of the national Clinical and Translational Science Awards consortium, to provide comprehensive support for junior faculty investigators.
Annually, faculty members, at the ranks of instructor or assistant professor in their initial three years of faculty appointment, are nominated by their chairs or deans to participate. Annually, 30 to 40 faculty members are eligible. To participate, at least 30% of their effort must be for research, though the majority of accepted scholars have 40% to 60% effort dedicated to research. Senior mentors in the AA/FD office review and select scholars. The selection process is competitive, with a maximum of 20 scholars selected annually. Once scholars are selected, the MMM is used to create an individualized and holistic mentoring and development plan for each scholar.
Description of the MMM
The MMM was developed to support the CATS scholars and is a holistic framework that includes five levels of mentorship (Figure 1). The different types of mentorship are synergistic and create a nurturing environment that fosters accountability, communication, and skills development to create empowered principal investigators. The senior mentors and program staff define the activity of each mentor. Monitoring of effectiveness is ongoing through progress reports and senior mentor meetings with the mentees, scientific mentors, peers, staff, and department chairs or division chiefs.
Figure 1.
The five mentoring levels of the Matrix Mentoring Model (MMM), of the clinical and translational scholars (CATS) mentoring program, University of Utah. The MMM is a holistic multilevel approach for mentoring clinical and translational investigators at an academic health center.
Self-mentorship
The first, and central, component of the model is self-mentorship. Investigators are taught to be their own best mentors. Each scholar is asked to engage in a period of self-reflection to determine professional priorities and goals. Scholars are provided with tools to direct self-reflection, including a career strategic planning tool. Understanding their priorities is critical as they enter the faculty role and must make decisions regarding the investment of their time across a variety of valuable academic endeavors.
Senior mentorship
The second level of mentorship is termed senior mentorship, which is provided through the AA/FD. Senior mentors dedicate approximately 10% effort to the CATS program and are compensated by the AA/FD office up to the NIH salary cap. Each mentor is assigned three or four junior faculty scholars. Senior mentors are experienced grant-funded investigators who are recommended by their department chairs or dean and are interviewed and selected by the CATS program director. Senior mentors receive mentor training through the AA/FD and human resources. They understand the retention, tenure, and promotion process, are familiar with institutional resources, and have developed expertise in motivational communication.
Senior mentors meet regularly with scholars during the academic year, both individually and in small groups. A minimum of two career planning meetings is required annually at the beginning and end of each academic year. These meetings include the scholar, the scientific mentor(s), AA/FD staff, and the division chief or chair. The team creates a timeline for the academic year that includes priorities and milestones that are aligned with the career goals of the scholar. The academic goals and timeline are codified as a contract signed by the scholar, senior mentor, and the division chief, chair, or dean. The senior mentor is responsible for regularly evaluating the alignment of time in effort with the stated scholar priorities. An important advantage of the CATS program is the role of the senior mentor in ensuring accountability of all parties to the goals set forth in the timeline. The senior mentors are not in the same department or discipline as the scholar and can intervene with division chiefs or scientific mentors when conflicts arise. Senior mentors are expected to read and edit all research proposals developed by the scholars and to be strong advocates for the scholars during the two-year program.
Scientific mentorship
Senior mentors and program staff assist the scholar in identifying appropriate scientific mentors. The scholar ultimately chooses the members of the scientific mentoring team with input from other stakeholders. Each scholar is required to have a scientific mentorship team, ideally with three members. One individual serves as the primary mentor. Potential mentors are drawn from the full complement of faculty members at the University of Utah and are chosen to provide specific skills in research methodology or clinical expertise.
The primary scientific mentor is expected to meet frequently with the mentee, preferably weekly and no less than monthly. The entire scientific mentoring team is expected to meet at least quarterly to assess mentee progress. Biannual written mentor team reports are submitted to the senior mentor. The scientific mentors are not compensated financially for the time spent with the scholar because they have the opportunity to advance their own scientific interests through collaboration with the scholar through publication and grant applications. Additionally, excellence in mentorship is a criterion for promotion and tenure at the University of Utah, allowing scientific mentors to reference their mentorship of CATS trainees to support their own professional advancement.
Peer mentorship
Peer mentoring groups are developed through a training program for all scholars developed with the assistance of the University of Utah Human Resources entitled Management Essentials for Principal Investigators, which spans the full two years of the CATS program. Table 1 outlines the course content. Content is designed to improve knowledge and skills in scientific career development, grant writing, preaward and postaward grants management, and leadership.
Table 1.
Elements of the Management Essentials for Principal Investigators Course, Clinical and Translational Scholars (CATS) Mentoring Program, University of Utah
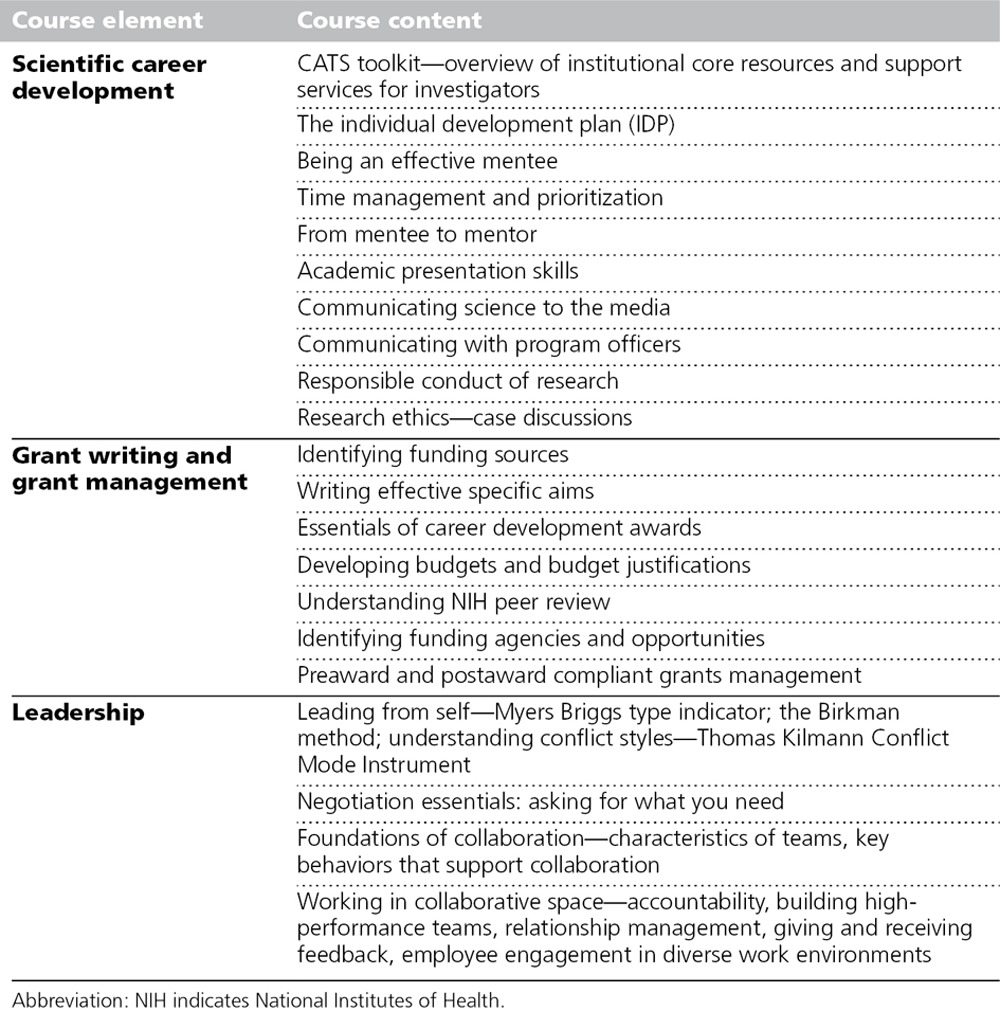
All scholars are brought together for a two-day orientation at the start of the program and for regular conferences and workshops thereafter. Scholars develop skills such as hiring, providing and receiving feedback, and managing team performance through human resources. They practice skills including communicating science with the media and negotiation, and participate in role-plays such managing conflict related to authorship and balancing clinical and research activities. Each scholar also receives an analysis of his/her personality type using the Myers-Briggs type indicator10 and an analysis of his/her conflict style using the Thomas Kilmann Conflict Mode Instrument.11 The scholars also have access to individual coaching for interpersonal skills on request.
Many productive peer relationships have developed as a result of participation. Individuals from different divisions, departments, and disciplines have supported each other in manuscript and grant review, and many have undertaken joint research projects that have resulted in publications and grant funding. During the interactions, scholars are also provided with resources to help them identify other appropriate peer groups to enlarge their networks.
Staff mentorship
A unique aspect of the MMM is AA/FD staff mentorship. Nonfaculty staff members include individuals with expertise in grants and contracts as well as individuals with analytic and data management skills. Staff members are present at all senior mentor meetings and participate and help teach the Management Essentials curriculum. Each scholar works closely with the AA/FD staff before and during grant preparation and submission. Throughout the process of grant submission, the scholars have a contextual training experience. Working closely with AA/FD staff, scholars learn research compliance at the local and national level. The scholars better appreciate the time and resources required for a successful grant submission and understand the indispensable roles staff members will have in their ultimate success as principal investigators. The AA/FD staff collaborate with the staff in each scholar’s home department to increase capacity and create a stronger infrastructure to support the scholar following completion of the CATS program.
Program direction and evaluation of mentorship
The senior mentors and AA/FD staff define the activity of each mentor type. Monitoring is ongoing throughout the year through progress reports, senior mentor and peer meetings, and feedback solicited from all program participants, staff, mentors, and departments. The effectiveness of senior mentors is measured through their contributions to program training and activities, participation with, and outcomes of assigned scholars.
Program Participants and Outcomes
Program participants
The pediatric CATS program began in FY 2008 and focused on child health investigators. The pediatric program enrolled 46 child health scholars. Of these there are 40 graduates and 6 active scholars in FY 2015. The health sciences CATS program began in FY 2013 and has had 40 participants with 9 graduates by FY 2015 (Table 2). In addition to the Department of Pediatrics, the Departments of Family and Preventive Medicine, Internal Medicine, Neurology, Neurosurgery, Obstetrics and Gynecology, Orthopaedics, Pathology, Surgery, and the Colleges of Health, Nursing, and Pharmacy have all had more than one CATS scholar.
Table 2.
Characteristics of the Clinical and Translational Scholars (CATS) Mentoring Program, University of Utah, 2008 to 2015
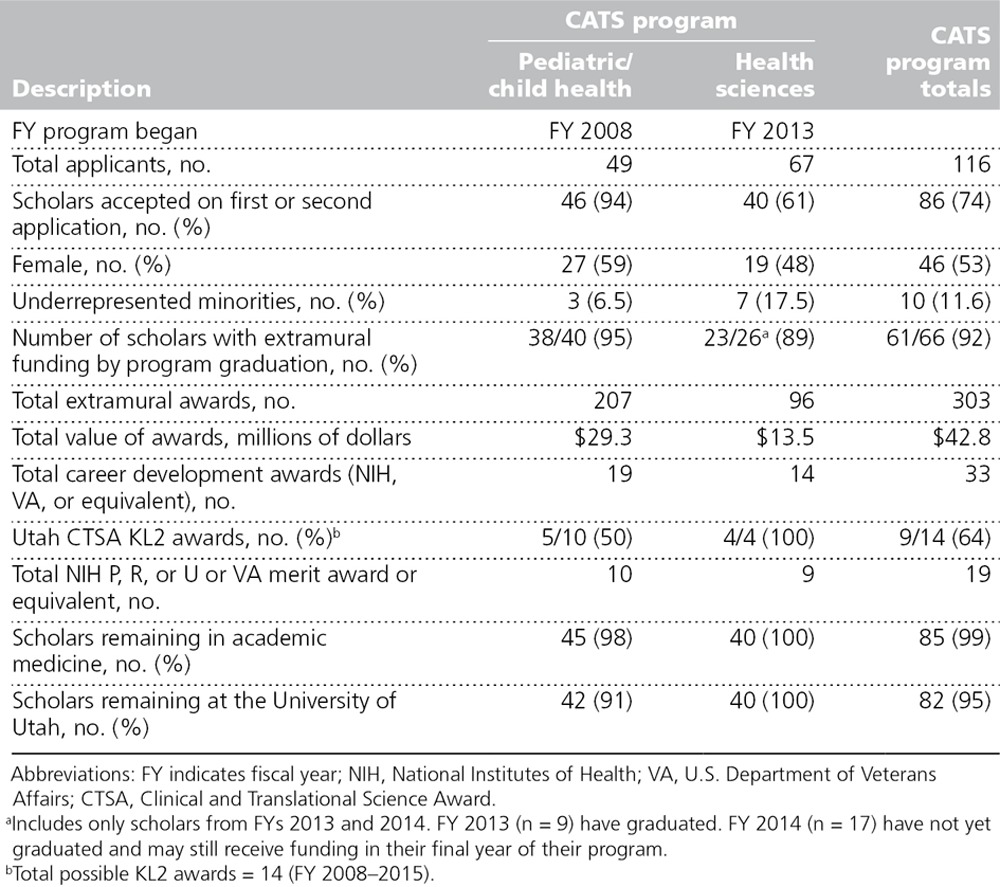
Overall, nearly 75% of applicants were accepted to the CATS programs, though the acceptance rate of applicants was higher for the pediatric program (94%) when compared with the health sciences program (61%), P < .001 (Table 2). Of the 30 CATS applicants not accepted initially, 13 did not reapply; all remain at the institution and are engaged primarily in clinical activities.
Grant support of CATS participants
The outcomes, including grant support of the CATS program scholars, are shown in Table 2. The majority of CATS scholars (92%), none of whom have grant support at the time of program entry, have achieved the goal of becoming principal investigators of at least one award by completion of the program. Awards continue to accrue after participation in the program. Participants have been awarded more than 300 grants valued at $42.8 million during and after their participation.
Longer-term outcomes are available for the pediatric CATS program. Of these scholars, 38/40 (95%) graduates have received extramural funding, and 2/6 (33%) of currently enrolled scholars have extramural awards. The 42 scholars who have received grant funding have received a total of 207 awards (4.9 per scholar) totaling $29.3 million in direct costs (mean $699,329 per scholar, range $25,000–$4,270,000) and generated $5.3 million in indirect costs. Thirty scholars (71%) have received awards of at least $100,000, 19 (45%) have received at least $500,000, and 9 (21%) have received at least $1 million.
The health sciences CATS scholars, 78% of whom have participated in the CATS program for less than two years, have submitted 71 applications for extramural funding and have received awards totaling $3.9 million as of quarter 2 FY 2015. Awards are similar to those obtained by child health investigators and include NIH, private foundations, and industry but also include Veteran’s Administration career development and merit awards.
Advancement and retention of CATS participants
The CATS program has produced additional positive outcomes for both the scholars and the institution. Of the 46 child health scholars, 23 (50%) have been promoted to assistant or associate professor, and 9 (20%) have received tenure. Importantly, 99% of all CATS participants remain in academic medicine, 95% at the University of Utah (Table 2). These retention rates are higher than for assistant professors in the health sciences, who overall had a retention rate of 60% for FYs 2008–2015 at our institution.
Inclusion and the CATS program
Inclusion of diversity in the faculty workforce was enhanced following the introduction of the CATS programs. For example, the proportion of women among child health investigators with career development awards increased from 1/10 (10%) from FYs 2004–2007 to 16/29 (55%) from FYs 2008–2015 (P = .02) following the implementation of the pediatric CATS program. The CATS scholars in both the child health and health sciences programs include a total of 86 individuals; 46 (53%) are women and 10 (11.6%) are from URM groups compared with the overall health sciences faculty in which 32% are women and 2% are from URM groups.
Costs associated with the CATS program
The CATS program leverages many institutional resources to create a structured mentoring program to benefit faculty in all departments, schools, and colleges. The inclusion and coordination of resources and personnel from the AA/FD office, the CCTS, and the University of Utah Human Resources increases the capacity of the faculty mentors and broadens the scope of services available while keeping costs low. The addition of senior mentors compensated for their participation, and dedicated staff represented new institutional costs. One program coordinator and one administrative director manage the CATS program within the context of the AA/FD office staff, which also manages several additional faculty development programs across the institution. There is a small annual cost for supplies and assessment tools used in the Management Essentials curriculum. The CATS program also contracts with the Utah CCTS to provide statistics and study design consultative services, grant writing workshops, and peer review during the scholars’ two-year participation in the program. For institutions planning to emulate the CATS program, costs will vary depending on the number of scholars and existing infrastructure. Direct financial costs for scholar time and resources directly related to research are borne by the departments. Based only on grants awarded, the return on investment of the CATS program is more than 20 to 1.
Interpretation and application
We have described an institutional mentoring program that coordinates and leverages the strengths of departments, the offices of faculty development and human resources, and the infrastructure of the NIH-supported CCTS to advance the careers of junior faculty members engaged in clinical and translational science. The integrated infrastructure supports the delivery of a holistic mentoring experience using the MMM and addresses many of the barriers facing the biomedical workforce.3 The CATS program has increased the research capacity of our institution and is generalizable to other academic health centers.
The MMM offers a new framework and moves away from dyadic mentoring toward mentoring networks where each mentor contributes unique skills.4 The model includes scientific and peer mentors12,13 recognized as essential for career development and present at many institutions. Unique aspects of the mentoring framework include a focus on self-mentoring and the investments in senior faculty and research staff mentors. Self-mentoring and skills development provide scholars with tools needed to thrive in academic medicine. Senior mentors provide objective career development support, facilitate accountability, and foster network development for each scholar. Research staff mentor and share knowledge that is vital to the growth of principal investigators. Coordinating these institutional investments has allowed us to develop efficiencies while increasing effectiveness and return.
Leadership training is an important aspect of the CATS program and the MMM. All faculty mentors, staff, and scholars participate in leadership training. The training improves individuals’ ability to communicate and to work in teams. These skills are critical for translational investigators.14,15 On completion of the CATS program, scholars are better equipped to understand their career goals and leadership and conflict styles and have developed management skills related to personnel and grants, which will enable them to better function as principal investigators and leaders.
We have identified multiple positive short-term outcomes of the CATS program. Of program participants, 92% transition to principal investigators with extramural awards during the mentored period. These scholars, over the 8-year course of the program’s life span to date, have been nearly uniformly retained in academic medicine and remain at the institution. Retention of 95% of junior faculty investigators in the CATS program contrasts with data from the Association of American Medical Colleges, which reported 50% attrition of assistant professors in clinical departments by 7.9 years16 and contrasts with the 60% retention rate from FY 2008–2015 for assistant professors at the University of Utah and similar or lower rates at other institutions.17–19 These data add support for the role of formal mentoring programs at academic health centers to support the biomedical research workforce.16,20
The CATS program also supports inclusion. The availability of the holistic program open to all faculty members may have facilitated the mentoring of women and URM investigators, who may struggle in academic medicine to access mentors.7,16,21 Following implementation of the CATS program, the proportion of women amongst all child heath investigators with career development awards increased significantly, and CATS scholars include more than 10% from URM backgrounds. The matrix of mentors may be particularly effective for groups with limited opportunities for dyadic mentoring. Additional longitudinal data will be required before we can evaluate the effect of the CATS program on URM faculty members’ retention and advancement.
Our observations are limited by reporting data for a single-center study and a short follow-up for each scholar (range of one to eight years). Nonetheless, we have demonstrated multiple benefits of the CATS program. Our findings contrast with national negative trends seen in the physician–scientist workforce and give us confidence in the program and in the institutional investment in structured mentoring for junior faculty engaged in clinical and translational science. We do not have sufficient data to fully assess the possibility of adverse effects that may have been experienced by those who did not participate in the CATS program. As the evidence increases regarding the effectiveness of the program, our goal is to support participation of all junior faculty members who aspire to be principal investigators. The CATS program and the MMM offer a successful model and a framework for institutional mentoring that can be applied in other academic health centers.
Acknowledgments: The authors acknowledge the clinical and translational scholars (CATS) program scholars who have been a source of inspiration and knowledge for the CATS mentors and staff.
Footnotes
Funding/Support: Dr. Byington received support through the Eunice Kennedy Shriver National Institute of Child Health and Human Development K24 HD047249 and the NIH/NCATS UL1 TR001067; Dr. Keenan received support through the NIH/Eunice Kennedy Shriver National Institute of Child Health and Human Development K24 HD072984.
Other disclosures: None reported.
Ethical approval: Reported as not applicable.
Previous presentations: Portions of this work were presented at the Association of American Medical Colleges Learn, Serve, Lead annual meeting, November 7–11, 2014, Chicago, Illinois.
References
- 1.Schafer AI. The vanishing physician–scientist? Transl Res. 2010;155:1–2. doi: 10.1016/j.trsl.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wyngaarden JB. The clinical investigator as an endangered species. N Engl J Med. 1979;301:1254–1259. doi: 10.1056/NEJM197912063012303. [DOI] [PubMed] [Google Scholar]
- 3.National Institutes of Health. Physician–Scientist Workforce Working Group Report. Bethesda, Md: National Institutes of Health; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeCastro R, Sambuco D, Ubel PA, Stewart A, Jagsi R. Mentor networks in academic medicine: Moving beyond a dyadic conception of mentoring for junior faculty researchers. Acad Med. 2013;88:488–496. doi: 10.1097/ACM.0b013e318285d302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tesch BJ, Wood HM, Helwig AL, Nattinger AB. Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA. 1995;273:1022–1025. [PubMed] [Google Scholar]
- 6.Jolliff L, Leadley J, Coakley E, Sloane R. Women in U.S. Academic Medicine and Science: Statistics and Benchmarking Report 2011–2012. Washington, DC: Association of American Medical Colleges; 2012. [Google Scholar]
- 7.Blood EA, Ullrich NJ, Hirshfeld-Becker DR, et al. Academic women faculty: Are they finding the mentoring they need? J Womens Health (Larchmt) 2012;21:1201–1208. doi: 10.1089/jwh.2012.3529. [DOI] [PubMed] [Google Scholar]
- 8.Beech BM, Calles-Escandon J, Hairston KG, Langdon SE, Latham-Sadler BA, Bell RA. Mentoring programs for underrepresented minority faculty in academic medical centers: A systematic review of the literature. Acad Med. 2013;88:541–549. doi: 10.1097/ACM.0b013e31828589e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meyers FJ, Begg MD, Fleming M, Merchant C. Strengthening the career development of clinical translational scientist trainees: A consensus statement of the Clinical Translational Science Award (CTSA) Research Education and Career Development Committees. Clin Transl Sci. 2012;5:132–137. doi: 10.1111/j.1752-8062.2011.00392.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Myers & Briggs Foundation. The MBTI instrument. http://www.myersbriggs.org/my-mbti-personality-type/. Accessed October 8, 2015.
- 11.Kilmann Diagnostics. Thomas-Kilmann TKI. 2015. http://www.kilmanndiagnostics.com/catalog/thomas-kilmann-conflict-mode-instrument. Accessed October 8, 2015.
- 12.Mayer AP, Blair JE, Ko MG, Patel SI, Files JA. Long-term follow-up of a facilitated peer mentoring program. Med Teach. 2014;36:260–266. doi: 10.3109/0142159X.2013.858111. [DOI] [PubMed] [Google Scholar]
- 13.Varkey P, Jatoi A, Williams A, et al. The positive impact of a facilitated peer mentoring program on academic skills of women faculty. BMC Med Educ. 2012;12:14. doi: 10.1186/1472-6920-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Research Council. Committee on the Science of Team Science, Board on Behavioral Cognitive and Sensory Sciences, Division of Behavioral and Social Sciences and Education. Chapter 5: Professional Development and Education for Team Science. In: Cooke NJ, Hilton ML, editors. In: Enhancing the Effectiveness of Team Science. Washington, DC: National Academies Press; 2015. [PubMed] [Google Scholar]
- 15.Dilmore TC, Moore DW, Bjork Z. Developing a competency-based educational structure within clinical and translational science. Clin Transl Sci. 2013;6:98–102. doi: 10.1111/cts.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu C, Morrison E. U.S. Medical School Full-Time Faculty Attrition. Washington, DC: Association of American Medical Colleges; 2014. [Google Scholar]
- 17.Bucklin BA, Valley M, Welch C, Tran ZV, Lowenstein SR. Predictors of early faculty attrition at one academic medical center. BMC Med Educ. 2014;14:27. doi: 10.1186/1472-6920-14-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ries A, Wingard D, Gamst A, Larsen C, Farrell E, Reznik V. Measuring faculty retention and success in academic medicine. Acad Med. 2012;87:1046–1051. doi: 10.1097/ACM.0b013e31825d0d31. [DOI] [PubMed] [Google Scholar]
- 19.Ries A, Wingard D, Morgan C, Farrell E, Letter S, Reznik V. Retention of junior faculty in academic medicine at the University of California, San Diego. Acad Med. 2009;84:37–41. doi: 10.1097/ACM.0b013e3181901174. [DOI] [PubMed] [Google Scholar]
- 20.Kashiwagi DT, Varkey P, Cook DA. Mentoring programs for physicians in academic medicine: A systematic review. Acad Med. 2013;88:1029–1037. doi: 10.1097/ACM.0b013e318294f368. [DOI] [PubMed] [Google Scholar]
- 21.Guevara JP, Adanga E, Avakame E, Carthon MB. Minority faculty development programs and underrepresented minority faculty representation at US medical schools. JAMA. 2013;310:2297–2304. doi: 10.1001/jama.2013.282116. [DOI] [PubMed] [Google Scholar]


