Abstract
A desirable vaccine against respiratory syncytial virus (RSV) should induce neutralizing antibodies without eliciting abnormal T cell responses to avoid vaccine-enhanced pathology. In an approach to deliver RSV neutralizing epitopes without RSV-specific T cell antigens, we genetically engineered chimeric influenza virus expressing RSV F262-276 neutralizing epitopes in the globular head domain as a chimeric hemagglutinin (HA) protein. Immunization of mice with formalin-inactivated recombinant chimeric influenza/RSV F262-276 was able to induce RSV protective neutralizing antibodies and lower lung viral loads after challenge. Formalin-inactivated RSV immune mice showed high levels of pulmonary inflammatory cytokines, macrophages, IL-4-producing T cells, and extensive histopathology. However, RSV-specific T cell responses and enhancement of pulmonary histopathology were not observed after RSV infection of inactivated chimeric influenza/RSV F262-276. This study provides evidence that an inactivated vaccine platform of chimeric influenza/RSV virus can be developed into a safe RSV vaccine candidate without priming RSV-specific T cells and immunopathology.
Keywords: Influenza virus, respiratory syncytial virus, recombinant, viral vector, F protein, neutralizing epitope vaccine
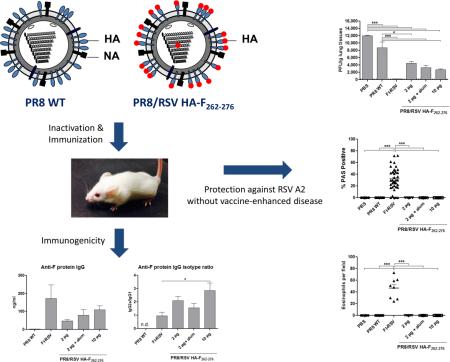
Graphical Abstract
In an approach to deliver respiratory syncytial virus (RSV) neutralizing epitopes without RSV-specific T cell antigens, we genetically engineered chimeric influenza virus expressing RSV F262-276 neutralizing epitopes in the globular head domain as a chimeric hemagglutinin (HA) protein. Intramuscular immunization of mice with formalin-inactivated recombinant chimeric influenza/RSV F262-276 induced IgG2a antibodies dominantly specific for RSV F protein. After RSV challenge, inactivated chimeric influenza/RSV F262-276 immune mice controlled lung viral loads and did not cause RSV-specific T cell responses and vaccine-enhanced pulmonary disease compared to formalin-inactivated RSV-immunized mice.
Background
Respiratory syncytial virus (RSV) is a major cause of respiratory tract illness in infants and young children and responsible for hundred thousands of annual deaths globally 1-2. RSV infection in early childhood has been linked to the recurrent wheezing later in life 3. Moreover, immunocompromised patients and the elderly are also at significant risk for severe RSV disease. This significant morbidity and mortality associated with RSV underscores the urgent need for the development of an RSV vaccine.
In the 1960s, clinical trials in infants using formalin-inactivated RSV (FI-RSV) formulated with alum resulted in severe vaccine-enhanced pulmonary disease severity upon subsequent RSV infection 4. Over the subsequent half century, previous studies about the pathogenesis of FI-RSV and the immune correlates of protection against RSV offer clues for development of a safe and effective RSV vaccine. A successful vaccine candidate will need to induce neutralizing antibodies, exclude immunosuppressive RSV proteins, and avoid the induction of undesirable T cell immune responses, which are known to be associated with vaccine-enhanced disease 5-7. Despite the extensive effort, there are no licensed RSV vaccines or therapeutic agents other than palivizumab (Synagis®; MedImmune).
Palivizumab is a humanized monoclonal antibody specific for the antigenic site II of RSV fusion (F) protein and is the only product approved for the prevention of severe RSV disease in high-risk pediatric patients 8. Passive transfer of monoclonal antibodies such as palivizumab and motavizumab suppresses viral replication in vivo and protects against RSV challenge in cotton rats without enhanced respiratory disease 9-10. It has been reported that palivizumab prophylaxis is effective in reducing the frequency of hospitalizations due to RSV infection in children who are at high risk of acquiring severe RSV infection 11. Nevertheless, due to the high cost of antibody prophylaxis, guidelines restrict recommendations for its use to the highest risk subgroups of infants.
Inactivated influenza vaccines have been safely used in humans. The reverse genetics system has provided a valuable tool for researchers to generate genetically manipulated influenza viruses expressing foreign antigens from different pathogens 12. Previously, we and others have reported that foreign epitopes could be presented to the immune system in the context of a chimeric influenza virus protein using a live vaccine platform 13-17. Here, we explored recombinant influenza virus as a safe inactivated vaccine for inducing neutralizing antibodies specific for the RSV F protein and avoiding RSV vaccine-induced abnormal immune responses. We generated recombinant influenza viruses carrying the RSV F262-276 neutralizing epitope within the globular head domain of hemagglutinin (HA) protein. Recombinant chimeric influenza/RSV F in an inactivated vaccine platform was investigated in regarding the immunogenicity, protective efficacy, cytokine and T cell responses as well as histopathology in comparison with FI-RSV.
Methods
Cells and viruses
HEp-2 cells and 293T cells were obtained from ATCC and propagated in Dulbecco's modified eagle media (DMEM) with 10% fetal bovine serum. Influenza A virus A/PR/8/1934 (H1N1, abbreviated PR8) virus was propagated in 10-day-old embryonated eggs. The RSV strain A2 was originally provided from Dr. Barney Graham. Purified inactivated viruses were produced by treating the virus with formalin at a final concentration of 1:4,000 (v/v) as previously described 15.
Construction of chimeric recombinant PR8/RSV HA-F
Plasmid pHW194-HA was previously described 18. By introducing silent mutations, a PstI restriction enzyme site was generated at nucleotide position 489 and removed at nucleotide position 74 of the PR8 HA gene. Moreover, new HindIII restriction enzyme site was introduced at nucleotide position 563 of the HA gene. The resulting plasmid was designated PR8-mHA. All silent mutations in the PR8-mHA were introduced by site-directed mutagenesis using the QuikChange Muli Site-Directed Mutagenesis Kit (Agilent Technologies, Böblingen, Germany) by use of a strategy similar to that employed by Li et al. 16-17. Three recombinant plasmids of chimeric HA-F constructs were generated by inserting the RSV F772-825, F784-828, and F784-819 nucleotide fragment (Genbank accession number FJ614814) into the PR8-mHA plasmid using PstI and HindIII restriction enzymes, respectively (Figure 1A).
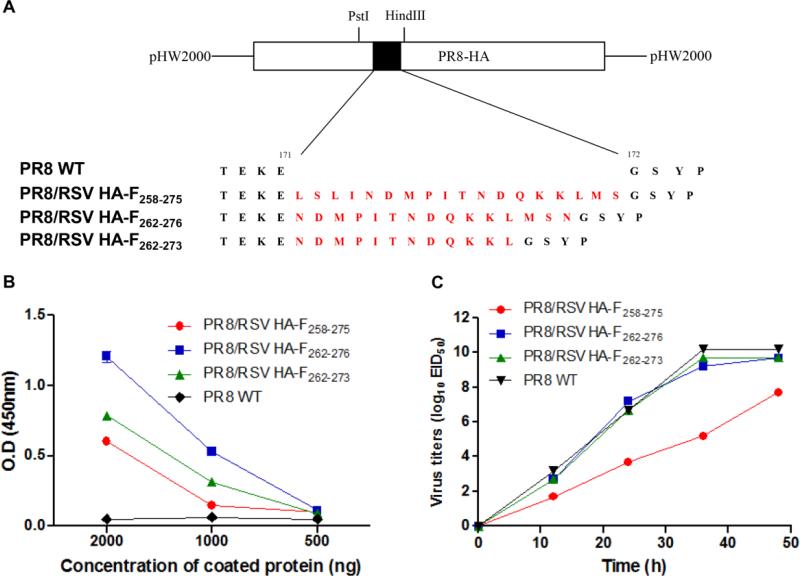
Figure 1. Recombinant PR8/RSV HA-F viruses show reactivity to palivizumab.
(A) Inserted sequences in the plasmids PR8/RSV HA-F258-275, PR8/RSV HA-F262-276, and PR8/RSV HA-F262-273. pHW194-HA-derived plasmids PR8/RSV HA-F258-275, PR8/RSV HA-F262-276, and PR8/RSV HA-F262-273 contains the amino acid (aa) sequence of the antigenic site II of the RSV F protein. The aa sequences forming the loop of site Sa of the mutated HA gene are shown. These plasmids contain 18- or 15- or 12-aa insertion in the HA gene between positions 171 and 172, as indicated by the black box, respectively. The inserted aa sequences are indicated by the red color. (B) Palivizumab reactivity. The presence and contents of RSV neutralizing epitopes in the chimeric recombinant viruses PR8 WT, PR8/RSV HA-F258-275, PR8/RSV HA-F262-276, and PR8/RSV HA-F262-273 were determined by ELISA using F protein monoclonal antibody (palivizumab). (C) In vitro growth kinetics. Eggs were infected at 15 EID50 (50% egg infective dose) of PR8 WT, PR8/RSV HA-F258-275, PR8/RSV HA-F262-276, and PR8/RSV HA-F262-273 virus. Samples were collected at 0, 12, 24, 36, and 48 h postinfection. The viral titer in the samples was determined by an egg infection assay.
Recombinant viruses PR8/RSV HA-F258-275, PR8/RSV HA-F262-276, and PR8/RSV HA-F262-273 were generated by reverse genetics using the pHW2000-based eight-plasmid system (kindly provided by R.G. Webster) as described by Hoffmann et al. 12. Briefly, 293T cells were cotransfected with eight pHW2000 plasmids containing eight influenza virus gene segments including the chimeric HA-F constructs (Figure 1A). After 48 h transfection, the supernatant was collected and further inoculated into embryonated chicken eggs. Seventy-two hours after inoculation, the presence of the recovered recombinant viruses was proved by hemagglutination of chicken red blood cells. To determine the incorporation of the antigenic site II of the RSV F protein into recombinant HA-F chimeric proteins, the reactivity to palivizumab (MedImmune, Gaithersburg, MD) was analyzed by enzyme-linked immunosorbent assay (ELISA).
Immunizations and RSV challenge of mice
For animal experiments, six- to eight-week-old female BALB/c mice (n = 5; Charles River Laboratories) were immunized intramuscularly with 10 μg of formalin-inactivated PR8/RSV HA-F262-276 virus or 2 μg of inactivated PR8/RSV HA-F262-276 virus alone or mixed with 50 μg of aluminum hydroxide (alum) adjuvant or 2 μg of inactivated PR8 wild-type (PR8 WT) virus. The FI-RSV control group was intramuscularly immunized with 2 μg of FI-RSV in alum adjuvant 19. Blood samples were obtained three weeks after each immunization. Immunized mice were challenged with RSV A2 strain (2 × 105 PFU) at 4 weeks after boost immunization. All animal experiments presented in this study were approved by the Georgia State University IACUC review boards (IACUC A14025).
Assays for antibody responses and virus titration
RSV F protein-specific antibodies (IgG, IgG1, and IgG2a) were determined in samples by enzyme-linked immunosorbent assay (ELISA) as previously described 20. To determine hemagglutination inhibition (HI) titers, serum samples were incubated with receptor destroying enzyme (RDE, Denka Seiken, Japan) and heated at 56 °C. In brief, HI titers were determined using inactivated PR8 virus and 1% chicken erythrocyte suspension with two-fold diluted serum samples after RDE treatment.
RSV-specific neutralizing antibody titers in immune sera were evaluated by a standard method as previously described 21. Briefly, the serum samples were heat-inactivated at 56°C and serially diluted two-fold in serum-free DMEM. Equal volumes of RSV (300 PFU/well) were mixed with diluted sera. A mixture of RSV with or without immune sera was incubated at 33°C, 5% CO2 for 1 h prior to incubation in the HEp-2 cell monolayers. The next steps were followed by an immune-plaque assay procedure as described previously 15. After fixing with 5% formaldehyde in PBS and blocked with 5% non-fat dry milk in PBST, anti-RSV F monoclonal antibody (131-2A, Millipore) and then HRP conjugated anti-mouse IgG antibody were used. Individual plaques were developed using 3,3’-diaminobenzidine tetrahydrochloride (DAB) substrate (Invitrogen, Camarillo, CA) and then counted.
Cytokine assay
Challenged mice were euthanized at 5 days post-infection (p.i.). Each lung was homogenized and centrifuged at 1400 × g at 4°C for 10 min. Cytokine and eotaxin levels in the lung extract were analyzed via ELISA according to the manufacturers’ instructions (eBioscience and R&D Systems) in duplicate against a standard curve.
Determination of F-specific T cell responses
Interferon (IFN)-γ- or IL-4-secreting cell spots were determined on Multi-screen 96 well plates (Millipore, Billerica, MA) coated with IFN-γ or IL-4 cytokine capture antibodies (BD Biosciences, San Diego, CA) as previously described 20. Briefly, spleen and lung cells were isolated from challenged mice and cultured on the plate with F85-93 peptide (KYKNAVTEL, 2 μg/ml) for 36 h, and then spots representing IFN-γ- or IL-4-secreting T cells were counted using an ELISpot reader (BioSys, Miami, FL).
Flow cytometric analysis
For bronchoalveolar lavage (BAL) cells, the diaphragms were dissected to allow free lung expansion and the lungs were lavaged by slowly instilling 1 ml of PBS and then gently aspirating as described 22. To perform cell phenotype analysis, immune cell surface marker antibodies including CD3, CD11b, CD11c, CD45, F4/80, MHC class II, and Siglec F (eBioscience or BD Pharmingen) were used to distinguish cell populations.
Pulmonary histology of RSV-infected mice
The lung tissues were fixed in 10% neutral buffered formalin for 24 hrs, transferred into 70% ethanol, and followed by routine processes. The lung tissues embedded in paraffin, sectioned into a thickness of 5 μm and stained with hematoxylin and eosin (H&E), periodic acid-Schiff stain (PAS) or hematoxylin and congo red (H&CR) as described previously 23-24. At least eight sections per mouse were obtained for histopathologic analysis. Tissue sections stained with H&E were scored blindly for the degree of inflammation around blood vessels, airways, or interstitial spaces, on a scale of 0 to 3, as previously described 25-26. For sections stained with PAS, the percentage of airways positive for PAS in ten individual airways of each mouse was scored.
Statistical analysis
All results are expressed as the mean ± standard error of the mean (SEM). To determine the statistical significance, 1-way or 2-way ANOVA was used where appropriate. P-values of less than or equal to 0.05 were considered statistically significant.
Results
Chimeric influenza viruses carrying an HA-F shows reactivity to RSV neutralizing antibody
The antigenic site B of influenza virus H3 protein and the antigenic site Sa of H1 protein virus is located at the head domain of the HA protein 27-28. It has been previously demonstrated that the 12-ammino-acid (aa) peptide can be inserted into the loop between the glycine and aspartic acid residues 16. The 18-aa peptide LSLINDMPITNDQKKLMS (F258-275), the 15-aa peptide NDMPITNDQKKLMSN (F262-276), and the 12-aa peptide NDMPITNDQKKL (F262-273), derived from the antigenic site II of RSV F protein, which is recognized by palivizumab (Synagis) 29, were selected for expression in the HA antigenic site Sa of PR8. Chimeric recombinant influenza viruses PR8/RSV HA-F258-275, PR8/RSV HA-F262-276, and PR8/RSV HA-F262-273 were generated using the reverse genetics system (Figure 1A).
All 3 recombinant chimeric influenza viruses were successfully rescued as confirmed by growth in eggs. The antigenic properties of the chimeric recombinant viruses were determined by ELISA using palivizumab (Figure 1B). The parental virus PR8 did not show any reactivity to palivizumab. The reactivity of palivizumab monoclonal antibody to the 15-aa PR8/RSV HA-F262-276 was estimated to be at least 1.7-fold higher than that to the 18-aa PR8/RSV HA-F258-275. Moreover, compared with that of the 12-aa PR8/RSV HA-F262-273, the reactivity of palivizumab antibody to the 15-aa PR8/RSV HA-F262-276 was approximately 1.4-fold higher. These data suggest that replication competent PR8 virus containing 18-aa RSV F foreign peptide in the antigenic site Sa of globular head domain can be rescued. However, the 18-aa PR8/RSV HA-F258-275, showed the lowest reactivity to palivizumab.
The 15-aa RSV F epitope-carrying recombinant influenza virus with highest palivizumab reactivity maintains an equal growth property in eggs
To compare in vitro viral growth kinetics, eggs were inoculated at a 15 EID50 (50% egg infective dose) of PR8 WT (wild type control), the 18-aa PR8/RSV HA-F258-275, the 15-aa PR8/RSV. A-F262-276, and the 12-aa PR8/RSV HA-F262-273. At various times after inoculation, virus titers in allantoic fluids were determined by an egg infection assay (Figure 1C). The growth kinetics of the 15-aa PR8/RSV HA-F262-276 or the 12-aa PR8/RSV HA-F262-273 except the 18-aa PR8/RSV HA-F258-275 in eggs was found to be comparable to that of PR8 WT. The insertion of an 18-aa epitope domain might have caused a conformational change on the head domain of HA protein, lowering the growth property of the chimeric HA-F virus.
Inactivated PR8/RSV HA-F262-276 vaccination is effective in inducing RSV neutralizing antibodies
For immunization studies, we selected a 15-aa recombinant PR8/RSV HA-F262-276 virus which showed the highest reactivity to palivizumab. Immunogenicity of recombinant PR8/RSV HA-F262-276 virus was determined in mice intramuscularly immunized with inactivated PR8/RSV HA-F262-276 or PR8 WT virus. Currently an approach to reduce vaccine dose is to increase immunogenicity by use of adjuvants 30. To determine potential dose sparing effects of adjuvants, inactivated PR8/RSV HA-F262-276 virus was mixed with alum. Three weeks after boost, RSV F-specific antibody responses were measured (Figure 2A-D).
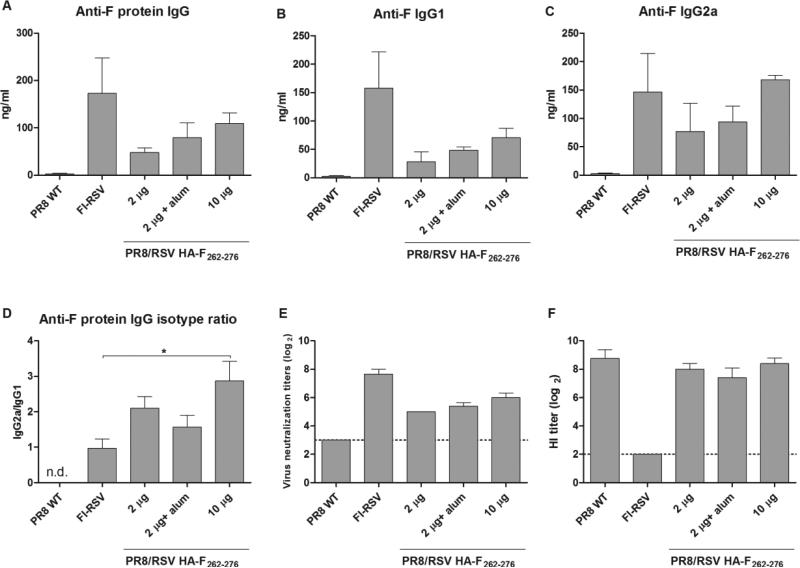
Figure 2. Inactivated PR8/RSV HA-F262-276 immunization induces RSV neutralizing antibodies without compromising virus immunogenicity.
Mice (n = 5) were immunized intramuscularly with 10 μg or 2 μg of inactivated PR8/RSV HA-F262-276 virus alone or mixed with alum or 2 μg of inactivated PR8 WT virus or 2 μg of FI-RSV in alum. Serum samples were obtained at 3 weeks after boost. IgG (A), IgG1 (B), and IgG2a (C) antibodies specific for RSV F protein in serum. ELISA was performed for F protein-specific serum antibodies using serially diluted serum samples. (D) Ratios of IgG2a/IgG1 isotype antibodies specific for RSV F protein. (E) RSV neutralization titers. The dashed lines denote limits of detection (a titer of 8). (F) Hemagglutination inhibition (HI) titers. HI titers were evaluated by standard methods using 4 HA units of inactivated A/PR8 virus and 1% chicken red blood cells. Error bars indicate mean ± SEM. n.d., not determined.
IgG antibodies specific for RSV F proteins were observed in sera from mice vaccinated with 10 μg of PR8/RSV HA-F262-276 (109.2 ± 50 ng/ml), 2 μg of PR8/RSV HA-F262-276 with alum (96.7 ± 63 ng/ml), and 2 μg of PR8/RSV HA-F262-276 (48.0 ± 16 ng/ml), respectively. A pattern of IgG antibody isotypes after immunization has been used as an indicator of Th1- or Th2-biased immune responses 31. Interestingly, the group with 10 μg of PR8/RSV HA-F262-276 showed significantly higher ratios of IgG2a/IgG1isotypes than the FI-RSV group (p < 0.05, Figure 2D), indicating a Th1-type immune response.
The FI-RSV group showed the highest mean neutralizing antibody titer of 7.7 ± 0.58 log2 against RSV (Figure 2C). In addition, mice vaccinated with recombinant PR8/RSV HA-F262-276 virus alone or mixed with alum showed higher neutralizing antibody titers against RSV than those of the PR8 WT control group. There was no significant difference in RSV neutralizing titers among the groups (Figure 2C). All mice immunized with recombinant or PR8 WT virus showed high titers of HI activity up to 8.75 ± 0.6 log2 (Figure 2D), indicating that there is no defect in virus immunogenicity of chimeric recombinant PR8/RSV HA-F262-276 virus.
Inactivated chimeric PR8/RSV HA-F262-276 vaccine significantly reduces RSV lung viral loads without inducing Th2 cytokines and RSV-specific T cell responses after challenge
To assess the protective efficacy of inactivated recombinant PR8/RSV HA-F262-276 vaccine, groups of mice were challenged with RSV A2 (2 × 105 PFU/mouse) at 4 weeks after boost. Mice vaccinated with FI-RSV showed complete protection against RSV A2 at 5 day p.i. Lung viral loads were significantly decreased in mice vaccinated with recombinant PR8/RSV HA-F262-276 virus alone or mixed with alum compared with PBS mock or PR8 WT controls (Figure 3A). These results indicate a pattern of inverse correlation between RSV lung viral titers and neutralizing antibodies.
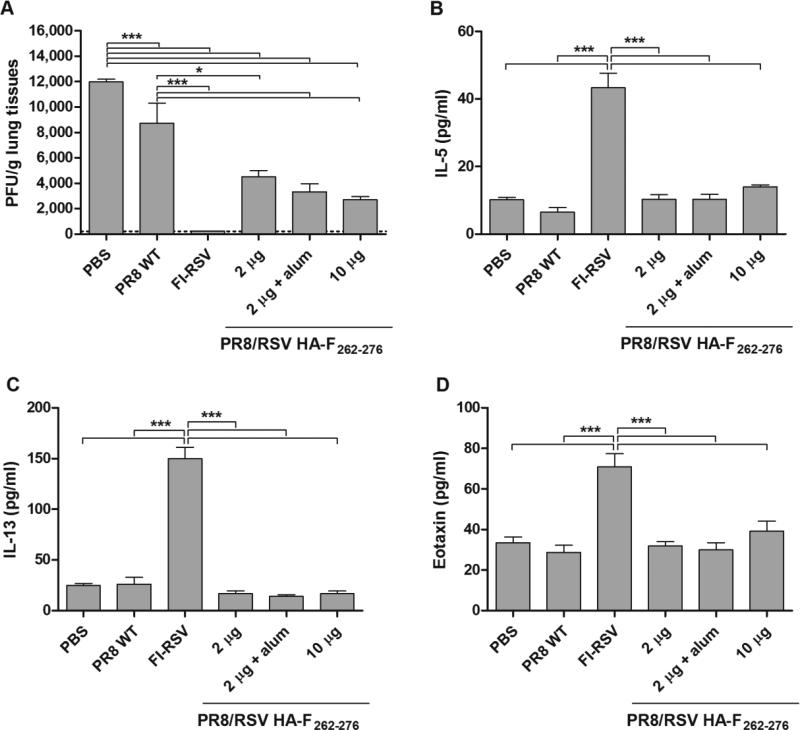
Figure 3. Inactivated PR8/RSV HA-F262-276 vaccine confers protection against RSV without inducing Th2 cytokines.
Mice that were immunized intramuscularly with PR8 WT or PR8/RSV HA-F262-276 virus or PBS were challenged with RSV A2 (n = 5). (A) Lung viral titers were determined by an immunoplaque assay at 5 days after RSV challenge. The levels of IL-5 (B), IL-13 (C) and eotaxin (D) were determined in the lung extracts from challenged mice by a cytokine ELISA at day 5 p.c.. Data represent mean ± SEM.
T helper type 2 (Th2) cytokines such as IL-5 and IL-13 have been shown to play an important role in RSV-induced pulmonary injury 32-33. In addition to the known roles for Th2 cytokines, studies have demonstrated that eotaxin is also a chemoattractant for eosinophils 34. The highest levels of cytokines and chemokine were observed in the lung extracts from the FIRSV group at day 5 p.c.. The levels of IL-5 (Figure 3B), IL-13 (Figure 3C) and eotaxin (Figure 3D) were significantly lower in mice immunized with recombinant PR8/RSV HA-F262-276 vaccines, PBS mock, and PR8 WT than those in the FI-RSV group.
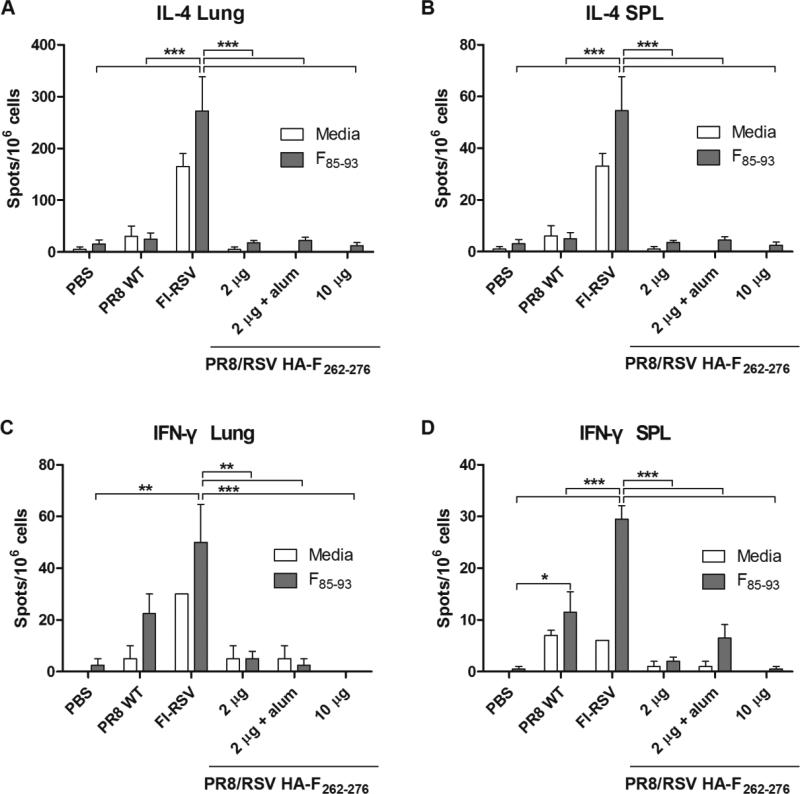
When compared to conventional cytokine ELISA, a cell-based assay of ELISpot is considered to be preferable for its higher sensitivity and epitope specificity 35. To determine whether recombinant PR8/RSV HA-F262-276 vaccination influenced antigen-specific T cell responses, we measured Th1 (IFN-γ) and Th2 (IL-4) cytokine-producing lung and spleen cell spots after in vitro stimulation with F85-93 peptide (Figure 4). The spot numbers of IL-4- or IFN-γ–secreting cells were detected at a significantly lower level in the lung from mice in the recombinant PR8/RSV HA-F262-276 vaccine groups and the PBS control group than those from the FI-RSV group. Interestingly, the PR8 WT group showed substantial levels of IFN-γ–secreting cells in lungs and spleens, but there was no significant difference.
Figure 4. Inactivated PR8/RSV HA-F262-276 immunization does not induce RSV-specific T cell responses.
IL-4- (A, B) secreting or IFN-γ– (C, D) secreting lung (A, C) or spleen (B, D) cells. Mice that were immunized intramuscularly with PR8 WT or PR8/RSV HA-F262-276 virus or PBS were challenged with RSV A2 (n = 5). At 5 day p.c., lung and spleen cells were harvested, stimulated with F85-93 peptides for 36 h. Cytokine-producing cell spots were counted by ELISPOT reader.
Inactivated PR8/RSV HA-F262-276 immunization does not induce eosinophil infiltration in the airways upon RSV infection
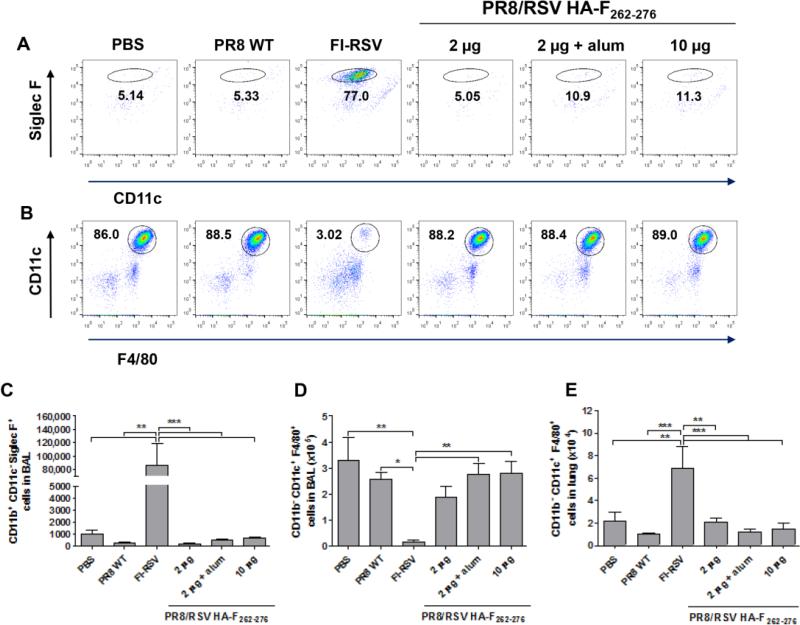
Pulmonary eosinophilia is known to be associated with FI-RSV-enhanced disease and correlated with the prominent production of Th2-derived cytokines 36-38. Moreover, eosinophils play a role in the reactive airway disease by producing proteins and enzymes that cause desquamation of airway epithelial cells, further contributing to airway obstruction 39. At day 5 p.i., eosinophils were significantly enhanced in BAL fluids from the FI-RSV group but not from other immunization groups (Figs. 5A and 5C). Notably, the PR8/RSV HA-F262-276 and PR8 WT groups did not reveal a distinct population of CD11b+CD11c−SiglecF+ cells in BAL fluids.
Figure 5. PR8/RSV HA-F immunization does not induce eosinophil infiltration in BAL fluids and macrophage infiltration in lung parenchyma upon RSV infection.
Cells in BAL samples obtained from challenged mice at 5 day p.c. were stained with anti-CD45, CD11b, CD11c, F4/80 and Siglec-F. (A) Representative dot plots of CD11b+CD11c−SiglecF+ cells (eosinophils). Number in the dot plots indicates percentages among CD45+CD11c− granulocytes. (B) Representative dot plots of CD11b−CD11c+F4/80+ cells (macrophages). Number in the dot plots indicates percentages among CD45+CD11b− granulocytes. (C) CD11b+CD11c−SiglecF+ cell counts in BAL fluids were determined. (D) CD11b−CD11c+F4/80+ cell counts in BAL were determined. (E) CD11b−CD11c+F4/80+ cell counts in lung parenchyma were determined. Data represent mean ± SEM.
By contrast, a reverse pattern was observed with CD11b−CD11c+F4/80+ macrophages in BAL fluids (Figs. 5B and 5D). The frequency and cellularity of CD11b−CD11c+F4/80+ macrophages in the BAL fluids were observed at significantly lower levels in the FI-RSV group than those in other groups. Interestingly, the cellularity of CD11b−CD11c+F4/80+ macrophages was significantly increased in the lung but not in BAL fluids from the FI-RSV group compared with other groups after challenge with RSV (Figure 5E). These results suggest that maintaining alveolar macrophages in the airways and preventing macrophage infiltration into the lung parenchyma tissues might be important for preventing vaccine-enhanced RSV disease.
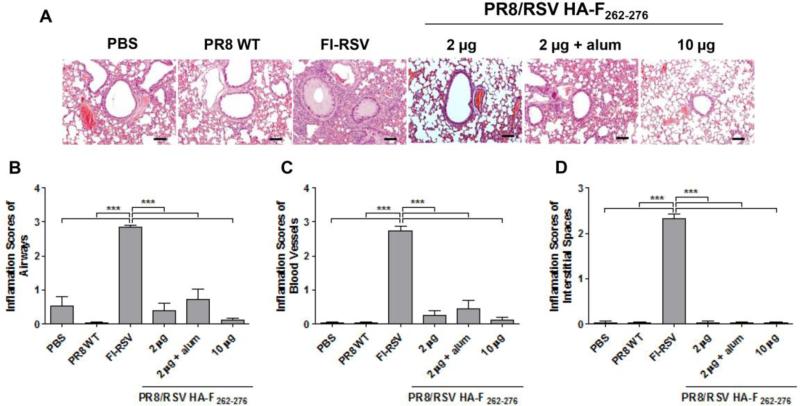
Inactivated PR8/RSV HA-F262-276 virus does not cause pulmonary histopathology
Developing a safe and effective RSV vaccine has been a challenge for over a half century. We examined pulmonary histopathology upon RSV infection for assessing the safety of RSV vaccine (Figure 6). FI-RSV immune mice showed highest inflammation around the airways (pathology score 2.9, Figure 6A, 6B), blood vessels (pathology score 2.7, Figure 6A, 6C), and interstitial spaces (pathology score 2.3, Figure 6A, 6D) after RSV challenge. Therefore, despite lung viral control, mice immunized with FI-RSV displayed severe vaccine-enhanced disease in the lung upon RSV infection. In contrast, lung tissues from the mice immunized with PR8/RSV HA-F262-276, PR8 WT and PBS did not reveal an obvious sign of inflammation around the airways, blood vessels, and interstitial spaces.
Figure 6. Histopathological changes in lungs are not observed in PR8/RSV HA-F262-276 immune mice upon RSV challenge.
Vaccinated mice were challenged with 2 × 105 PFU RSV A2 at 4 weeks after boost. Lungs were harvested at 4 day p.c., stained with H&E, and lung sections from each mouse were scored for inflammation on a scale of 0 to 3 as diagnostic criteria. (A) Representative sections are shown. Scale bars for H&E indicate 100 μm. (B) Inflammation scores around the airways (n = 5). (C) Inflammation scores around blood vessels (n = 5). (D) Inflammation scores around interstitial spaces (n = 5). Data represent mean ± SEM.
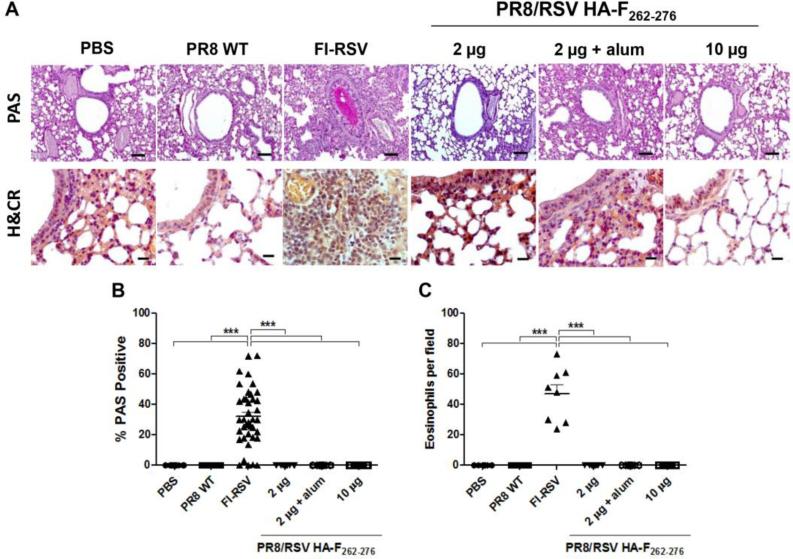
Abundant mucus production is another parameter of severe inflammatory RSV disease 40-41. The lung sections from mice were stained with PAS for visualization of mucus production (upper row, Figure 7A). These sections were quantitatively assessed for the percentage of airway linings showing PAS staining (Figure 7B). Inactivated PR8/RSV HA-F262-276 vaccine-immunized mice with or without alum adjuvant did not show PAS-positive airways (Figure 7B).
Figure 7. Periodic acid Schiff (PAS) and hematoxylin/Congo Red (H&CR) staining of lung tissues after RSV challenge.
Lung tissues were collected from challenged mice at day 5 p.c. and stained for analysis of mucus production and eosinophil infiltration (n = 5). (A) Photomicrographs of PAS (upper row), and H&CR (lower row) stained lung tissue sections from mice. Scale bars for PAS indicate 100 μm and for H&CR indicate 20 μm. (B) Inflammation scores of PAS staining. PAS-stained lung sections were scored as percentages of 10 individual airways in each mouse. Each dot symbolizes one airway. (C) Inflammation scores of H&CR staining. Eosinophils in lungs per 40× field counts in two different regions of each mouse. Data represent mean ± SEM.
The degrees of lung eosinophilia were estimated using H&CR staining to enumerate eosinophils and expressed as numbers of eosinophils present per 40× field (lower row, Figure 7A). Eosinophil accumulation in the lung was significantly greater in FI-RSV-immunized mice than that in the groups of mice that were vaccinated with the inactivated PR8/RSV HA-F262-276 vaccine or control PR8 WT (p < 0.001, Figure 7C).
Discussion
Influenza A virus has been examined for its suitability as a viral vector for the expression of foreign genes for vaccination since the reverse genetic system was developed 13. There are several approaches including the insertion of foreign proteins into the surface glycoproteins HA 16-17 and NA 42-43, and the manipulation of the nonstructural NS1 protein 44-45 or the PB2 protein 46-47. In previous studies, we engineered influenza A viruses expressing a conserved domain of the RSV G protein or the RSV F243-294 neutralizing epitope in the N-terminus of HA protein 14-15. These recombinant influenza viruses were capable of inducing neutralizing antibodies and conferring protection against RSV infection when mice were intranasally inoculated in a live virus platform. The size of foreign epitopes that are to be inserted into an antigenic site B head domain appears to be limited to 7 to 12 aa residues for the generation of recombinant live influenza viruses 16. We tested whether the insertion of an RSV neutralizing epitope into the antigenic site Sa of H1 HA protein could be more than 12 aa residues. To develop an effective chimeric virus for better exposure of RSV epitopes, we designed and constructed new chimeric recombinant influenza viruses expressing the palivizumab-recognized neutralizing epitope with 12, 15, and 18 aa on the antigenic site Sa of H1 protein, respectively. To the best of our knowledge, this is the first study to provide evidence that the antigenic site Sa of H1 can accommodate extra polypeptide segments up to 18 aa, still maintaining the HA functionality. Given the fact that the reactivity of palivizumab to the 15-aa PR8/RSV HA-F262-276 was higher than that to the 18-aa PR8/RSV HA-F258-275, it is possible that the insertion of 18-aa-polypeptide domain F258-275 into the antigenic site Sa caused conformational changes unfavorable to palivizumab reactivity in the head domain of HA protein as well as compromising HA functionality of reducing egg growth properties. The insertion of 15 aa of the RSV F262-276 neutralizing epitope into the antigenic site Sa of influenza virus HA was found to have the highest reactivity to palivizumab, indicating a favorable conformation for palivizumab recognition without causing a significant defect in the viral growth and HA immunogenicity (Figure 2). Our findings suggest that a foreign epitope up to 18 aa residues can be inserted into the antigenic site Sa of HA proteins and that 15-aa palivizumab epitope insertion has better exposure to palivizumab than either 18-aa epitope or 12-aa epitope. Thus, a chimeric virus with 15-aa palivizumab epitope insertion into HA can be a prospective vector platform for effectively delivering an RSV neutralizing epitope.
Influenza HI antibody titer are well known to correlate with influenza virus neutralizing antibodies and vaccine-induced protection 48. We confirmed that chimeric recombinant influenza virus vaccines did not compromise the induction of influenza virus specific antibody responses. All mice immunized with chimeric recombinant PR8/RSV or PR8 WT virus induced high titers of HI activity. Inactivated influenza vaccines are a current licensed platform for human vaccination. In a mouse model, it is well demonstrated that immunization with a prime boost regimen using inactivated influenza vaccines induces complete protection against lethal influenza virus challenge without displaying pulmonary histopathology 49-52. Vaccine-enhanced respiratory disease by FI-RSV immunization is a unique feature of an RSV pathogen, which has been a real challenge in developing a safe and effective RSV vaccine. Therefore, developing chimeric influenza/RSV viruses may provide an approach of vaccination against dual pathogens.
Following a disastrous outcome of alum-adjuvanted FI-RSV trials, a live-attenuated RSV vaccine platform is considered to be one of the promising RSV vaccine candidates. However, a difficult challenging factor for developing a live attenuated RSV vaccine is to find an appropriate balance of attenuation and immunogenicity between infants and sero-negative children 53-54. Also, it has been shown that purified full-length RSV F protein vaccines with alum adjuvant can cause vaccine-enhanced respiratory disease and Th2 type immune responses similar to FI-RSV upon RSV challenge despite their effective control of lung viral replication 55. In contrast, our results demonstrated that inactivated chimeric influenza/RSV HA-F vaccination elicited protective neutralizing antibodies but did not induce Th2 cytokines and eosinophil chemoattractant eotaxin. It has been reported that a restricted domain containing RSV neutralizing epitopes in a live viral vector can confer protection without vaccine-enhanced respiratory disease 14-15,42,44,56. Probably, recombinant vaccines have been preferentially investigated as a live viral vector platform due to the structural characteristics of location on the stalk region of the NA 42 and HA proteins 14-15 or the nature of intracellular expression of the NS1 protein 44,56. As far as we know, this is the first report of protection against RSV with an inactivated platform of recombinant influenza/RSV vaccine. The presentation of the RSV F neutralizing epitope on the head domain of HA protein was found to be effective in immunizing recombinant influenza/RSV virus as an inactivated vaccine platform. Inactivated or protein subunit vaccines are known to be usually safe and often the vaccine of choice for infants, immunocompromised patients, and pregnant women. Notably, inactivated influenza vaccination is approved for people ages 6 months or older and also recommended for all women who are or will be pregnant (in any trimester) during influenza season 57. Therefore, testing maternal immunization with inactivated influenza/RSV chimeric vaccines will be an objective of further studies, expecting to protect infants against RSV and influenza.
Vaccine safety is also an important issue to be considered when developing an RSV vaccine candidate. Therefore, it is worth noting that inactivated chimeric influenza/RSV vaccine induced protective neutralizing antibody against RSV without vaccine-enhanced disease. Vaccine-enhanced disease by FI-RSV was associated with elicitation of aberrant T cell responses 58, low-avidity antibodies 31, eosinophilic infiltration 4, and immune complex deposition in the small airways 59. Thus, an effective RSV vaccine should induce neutralizing antibodies, a balanced and controlled immune response but not cause disease upon RSV infection. Consistent with previous findings, the FI-RSV group induced high levels of Th2 cytokines, eotaxin, and eosinophils as well as both IFN-γ- and IL-4-producing T cells 14-15,20. Interestingly, alveolar macrophages from the FI-RSV group were found to be present at significantly lower levels in BAL fluids but at higher levels in lung parenchyma after RSV infection compared to other groups displaying no overt histopathology (Figure 5). Thus, it is likely that maintenance of alveolar macrophages in the airways but not in the lung parenchyma plays a role in preventing inflammatory RSV disease. Although RSV infection in the lower respiratory tract is likely to involve several cell types, the role of macrophages in the host response has been demonstrated 60-61. Recently, it has been reported that alternatively activated macrophages mediate the resolution of RSV-induced lung pathology 62. This study provides convincing evidence that differential distribution of alveolar macrophages between in the airways and in the lung parenchyma might play a role in the RSV-enhanced respiratory disease. Importantly, our study demonstrated the induction of neutralizing antibodies by immunization of mice with inactivated chimeric influenza/RSV vaccine without eliciting undesirable cellular responses such as Th2 cytokines and RSV-specific T cells following RSV challenge. Thus, this study reports a novel approach of delivering RSV neutralizing epitopes in the absence of RSV-specific T cell target antigens by engineering safe and immunogenic influenza virus as a vector.
In conclusion, this study demonstrates that inactivated chimeric influenza/RSV vaccine can confer protective immunity against RSV without the risk of potentially priming for enhanced lung pathology. Combinatory vaccination using other neutralizing epitopes of F or G protein may induce antisera with improved neutralization titers. As for a future direction, the safety and efficacy studies with the best candidate of chimeric vaccines that prevents lung inflammation will need to be carried out in a more relevant animal model such as cotton rats, which is a prerequisite for progressing to clinical testing. Our results underscore the considerable potential of influenza viral vector for the development of recombinant vaccines against different infectious agents. Taken together, these observations support that inactivated recombinant influenza/RSV vaccine represents a promising RSV vaccine candidate and need to be further developed, meeting on the priority of urgent medical needs.
Acknowledgements
This work was supported by NIH/NIAID grants AI105170 (S.M.K.), AI119366 (S.M.K.), and AI093772 (S.M.K.). The following reagent was obtained through BEI Resources, NIAID, NIH: Soluble Fusion Glycoprotein with C-Terminal Histidine Tag from Respiratory Syncytial Virus, A2, Recombinant Produced in 293F Cells, NR-28908.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
All authors declare no conflicts of interest.
References
- 1.Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med. 2005;352:1749–1759. doi: 10.1056/NEJMoa043951. [DOI] [PubMed] [Google Scholar]
- 2.Nair H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, O'Brien KL, Roca A, Wright PF, Bruce N, Chandran A, Theodoratou E, Sutanto A, Sedyaningsih ER, Ngama M, Munywoki PK, Kartasasmita C, Simoes EA, Rudan I, Weber MW, Campbell H. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375:1545–1555. doi: 10.1016/S0140-6736(10)60206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blanken MO, Rovers MM, Molenaar JM, Winkler-Seinstra PL, Meijer A, Kimpen JL, Bont L. Respiratory syncytial virus and recurrent wheeze in healthy preterm infants. N Engl J Med. 2013;368:1791–1799. doi: 10.1056/NEJMoa1211917. [DOI] [PubMed] [Google Scholar]
- 4.Kim HW, Canchola JG, Brandt CD, Pyles G, Chanock RM, Jensen K, Parrott RH. Respiratory syncytial virus disease in infants despite prior administration of antigenic inactivated vaccine. Am J Epidemiol. 1969;89:422–434. doi: 10.1093/oxfordjournals.aje.a120955. [DOI] [PubMed] [Google Scholar]
- 5.Collins PL GB. Viral and host factors in human respiratory syncytial virus pathogenesis. Journal of virology. 2008;82:2040–2055. doi: 10.1128/JVI.01625-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graham BS. Biological challenges and technological opportunities for respiratory syncytial virus vaccine development. Immunol Rev. 2011;239:149–166. doi: 10.1111/j.1600-065X.2010.00972.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Graham BS, Anderson LJ. Challenges and opportunities for respiratory syncytial virus vaccines. Current topics in microbiology and immunology. 2013;372:391–404. doi: 10.1007/978-3-642-38919-1_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romero JR. Palivizumab prophylaxis of respiratory syncytial virus disease from 1998 to 2002: results from four years of palivizumab usage. Pediatr Infect Dis J. 2003;22:S46–54. doi: 10.1097/01.inf.0000053885.34703.84. [DOI] [PubMed] [Google Scholar]
- 9.Johnson S, Oliver C, Prince GA, Hemming VG, Pfarr DS, Wang SC, Dormitzer M, O'Grady J, Koenig S, Tamura JK, Woods R, Bansal G, Couchenour D, Tsao E, Hall WC, Young JF. Development of a humanized monoclonal antibody (MEDI-493) with potent in vitro and in vivo activity against respiratory syncytial virus. J Infect Dis. 1997;176:1215–1224. doi: 10.1086/514115. [DOI] [PubMed] [Google Scholar]
- 10.Wu H, Pfarr DS, Johnson S, Brewah YA, Woods RM, Patel NK, White WI, Young JF, Kiener PA. Development of motavizumab, an ultra-potent antibody for the prevention of respiratory syncytial virus infection in the upper and lower respiratory tract. J Mol Biol. 2007;368:652–665. doi: 10.1016/j.jmb.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 11.Andabaka T, Nickerson JW, Rojas-Reyes MX, Rueda JD, Bacic Vrca V, Barsic B. Monoclonal antibody for reducing the risk of respiratory syncytial virus infection in children. Cochrane Database Syst Rev. 2013;4:CD006602. doi: 10.1002/14651858.CD006602.pub4. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann E, Neumann G, Kawaoka Y, Hobom G, Webster RG. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc Natl Acad Sci U S A. 2000;97:6108–6113. doi: 10.1073/pnas.100133697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garcia-Sastre A, Palese P. Influenza virus vectors. Biologicals. 1995;23:171–178. doi: 10.1006/biol.1995.0028. [DOI] [PubMed] [Google Scholar]
- 14.Lee YN, Hwang HS, Kim MC, Lee YT, Lee JS, Moore ML, Kang SM. Recombinant influenza virus expressing a fusion protein neutralizing epitope of respiratory syncytial virus (RSV) confers protection without vaccine-enhanced RSV disease. Antiviral Res. 2015;115:1–8. doi: 10.1016/j.antiviral.2014.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee YN, Suk Hwang H, Kim MC, Lee YT, Cho MK, Kwon YM, Seok Lee J, Plemper RK, Kang SM. Recombinant influenza virus carrying the conserved domain of respiratory syncytial virus (RSV) G protein confers protection against RSV without inflammatory disease. Virology. 2015;476:217–225. doi: 10.1016/j.virol.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li S, Polonis V, Isobe H, Zaghouani H, Guinea R, Moran T, Bona C, Palese P. Chimeric influenza virus induces neutralizing antibodies and cytotoxic T cells against human immunodeficiency virus type 1. J Virol. 1993;67:6659–6666. doi: 10.1128/jvi.67.11.6659-6666.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li SQ, Schulman JL, Moran T, Bona C, Palese P. Influenza A virus transfectants with chimeric hemagglutinins containing epitopes from different subtypes. J Virol. 1992;66:399–404. doi: 10.1128/jvi.66.1.399-404.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoffmann E, Krauss S, Perez D, Webby R, Webster RG. Eight-plasmid system for rapid generation of influenza virus vaccines. Vaccine. 2002;20:3165–3170. doi: 10.1016/s0264-410x(02)00268-2. [DOI] [PubMed] [Google Scholar]
- 19.Prince GA, Curtis SJ, Yim KC, Porter DD. Vaccine-enhanced respiratory syncytial virus disease in cotton rats following immunization with Lot 100 or a newly prepared reference vaccine. The Journal of general virology. 2001;82:2881–2888. doi: 10.1099/0022-1317-82-12-2881. [DOI] [PubMed] [Google Scholar]
- 20.Lee JS, Kwon YM, Hwang HS, Lee YN, Ko EJ, Yoo SE, Kim MC, Kim KH, Cho MK, Lee YT, Lee YR, Quan FS, Kang SM. Baculovirus-expressed virus-like particle vaccine in combination with DNA encoding the fusion protein confers protection against respiratory syncytial virus. Vaccine. 2014;32:5866–5874. doi: 10.1016/j.vaccine.2014.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson LJ, Bingham P, Hierholzer JC. Neutralization of respiratory syncytial virus by individual and mixtures of F and G protein monoclonal antibodies. J Virol. 1988;62:4232–4238. doi: 10.1128/jvi.62.11.4232-4238.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ko EJ, Kwon YM, Lee JS, Hwang HS, Yoo SE, Lee YN, Lee YT, Kim MC, Cho MK, Lee YR, Quan FS, Song JM, Lee S, Moore ML, Kang SM. Virus-like nanoparticle and DNA vaccination confers protection against respiratory syncytial virus by modulating innate and adaptive immune cells. Nanomedicine. 2015;11:99–108. doi: 10.1016/j.nano.2014.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meyerholz DK, Griffin MA, Castilow EM, Varga SM. Comparison of histochemical methods for murine eosinophil detection in an RSV vaccine-enhanced inflammation model. Toxicol Pathol. 2009;37:249–255. doi: 10.1177/0192623308329342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hwang HS, Kwon YM, Lee JS, Yoo SE, Lee YN, Ko EJ, Kim MC, Cho MK, Lee YT, Jung YJ, Lee JY, Li JD, Kang SM. Co-immunization with virus-like particle and DNA vaccines induces protection against respiratory syncytial virus infection and bronchiolitis. Antiviral Res. 2014;110:115–123. doi: 10.1016/j.antiviral.2014.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murawski MR, McGinnes LW, Finberg RW, Kurt-Jones EA, Massare MJ, Smith G, Heaton PM, Fraire AE, Morrison TG. Newcastle disease virus-like particles containing respiratory syncytial virus G protein induced protection in BALB/c mice, with no evidence of immunopathology. J Virol. 2010;84:1110–1123. doi: 10.1128/JVI.01709-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mok H, Lee S, Utley TJ, Shepherd BE, Polosukhin VV, Collier ML, Davis NL, Johnston RE, Crowe JE., Jr. Venezuelan equine encephalitis virus replicon particles encoding respiratory syncytial virus surface glycoproteins induce protective mucosal responses in mice and cotton rats. J Virol. 2007;81:13710–13722. doi: 10.1128/JVI.01351-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caton AJ, Brownlee GG, Yewdell JW, Gerhard W. The antigenic structure of the influenza virus A/PR/8/34 hemagglutinin (H1 subtype). Cell. 1982;31:417–427. doi: 10.1016/0092-8674(82)90135-0. [DOI] [PubMed] [Google Scholar]
- 28.Wiley DC, Wilson IA, Skehel JJ. Structural identification of the antibody-binding sites of Hong Kong influenza haemagglutinin and their involvement in antigenic variation. Nature. 1981;289:373–378. doi: 10.1038/289373a0. [DOI] [PubMed] [Google Scholar]
- 29.McLellan JS, Yang Y, Graham BS, Kwong PD. Structure of respiratory syncytial virus fusion glycoprotein in the postfusion conformation reveals preservation of neutralizing epitopes. J Virol. 2011;85:7788–7796. doi: 10.1128/JVI.00555-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hawken J, Troy SB. Adjuvants and inactivated polio vaccine: a systematic review. Vaccine. 2012;30:6971–6979. doi: 10.1016/j.vaccine.2012.09.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Delgado MF, Coviello S, Monsalvo AC, Melendi GA, Hernandez JZ, Batalle JP, Diaz L, Trento A, Chang HY, Mitzner W, Ravetch J, Melero JA, Irusta PM, Polack FP. Lack of antibody affinity maturation due to poor Toll-like receptor stimulation leads to enhanced respiratory syncytial virus disease. Nat Med. 2009;15:34–41. doi: 10.1038/nm.1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Collins PD, Marleau S, Griffiths-Johnson DA, Jose PJ, Williams TJ. Cooperation between interleukin-5 and the chemokine eotaxin to induce eosinophil accumulation in vivo. J Exp Med. 1995;182:1169–1174. doi: 10.1084/jem.182.4.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Castilow EM, Meyerholz DK, Varga SM. IL-13 is required for eosinophil entry into the lung during respiratory syncytial virus vaccine-enhanced disease. J Immunol. 2008;180:2376–2384. doi: 10.4049/jimmunol.180.4.2376. [DOI] [PubMed] [Google Scholar]
- 34.Johnson TR, Rothenberg ME, Graham BS. Pulmonary eosinophilia requires interleukin-5, eotaxin-1, and CD4+ T cells in mice immunized with respiratory syncytial virus G glycoprotein. J Leukoc Biol. 2008;84:748–759. doi: 10.1189/jlb.0907621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karlsson AC, Martin JN, Younger SR, Bredt BM, Epling L, Ronquillo R, Varma A, Deeks SG, McCune JM, Nixon DF, Sinclair E. Comparison of the ELISPOT and cytokine flow cytometry assays for the enumeration of antigen-specific T cells. J Immunol Methods. 2003;283:141–153. doi: 10.1016/j.jim.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 36.Kim HW, Canchola JG, Brandt CD, Pyles G, Chanock RM, Jensen K, Parrott RH. Respiratory syncytial virus disease in infants despite prior administration of antigenic inactivated vaccine. Am J Epidemiol. 1969;89:422–434. doi: 10.1093/oxfordjournals.aje.a120955. [DOI] [PubMed] [Google Scholar]
- 37.Chin J, Magoffin RL, Shearer LA, Schieble JH, Lennette EH. Field evaluation of a respiratory syncytial virus vaccine and a trivalent parainfluenza virus vaccine in a pediatric population. Am J Epidemiol. 1969;89:449–463. doi: 10.1093/oxfordjournals.aje.a120957. [DOI] [PubMed] [Google Scholar]
- 38.Castilow EM, Meyerholz DK, Varga SM. IL-13 is required for eosinophil entry into the lung during respiratory syncytial virus vaccine-enhanced disease. Journal of immunology. 2008;180:2376–2384. doi: 10.4049/jimmunol.180.4.2376. [DOI] [PubMed] [Google Scholar]
- 39.Ehlenfield DR, Cameron K, Welliver RC. Eosinophilia at the time of respiratory syncytial virus bronchiolitis predicts childhood reactive airway disease. Pediatrics. 2000;105:79–83. doi: 10.1542/peds.105.1.79. [DOI] [PubMed] [Google Scholar]
- 40.Aherne W, Bird T, Court SD, Gardner PS, McQuillin J. Pathological changes in virus infections of the lower respiratory tract in children. J Clin Pathol. 1970;23:7–18. doi: 10.1136/jcp.23.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lugo RA, Nahata MC. Pathogenesis and treatment of bronchiolitis. Clin Pharm. 1993;12:95–116. [PubMed] [Google Scholar]
- 42.De Baets S, Schepens B, Sedeyn K, Schotsaert M, Roose K, Bogaert P, Fiers W, Saelens X. Recombinant influenza virus carrying the respiratory syncytial virus (RSV) F85-93 CTL epitope reduces RSV replication in mice. J Virol. 2013;87:3314–3323. doi: 10.1128/JVI.03019-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Percy N, Barclay WS, Garcia-Sastre A, Palese P. Expression of a foreign protein by influenza A virus. J Virol. 1994;68:4486–4492. doi: 10.1128/jvi.68.7.4486-4492.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bian C, Liu S, Liu N, Zhang G, Xing L, Song Y, Duan Y, Gu H, Zhou Y, Zhang P, Li Z, Zhang K, Wang Z, Zhang S, Wang X, Yang P. Influenza virus vaccine expressing fusion and attachment protein epitopes of respiratory syncytial virus induces protective antibodies in BALB/c mice. Antiviral Res. 2014;104:110–117. doi: 10.1016/j.antiviral.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 45.Ferko B, Stasakova J, Sereinig S, Romanova J, Katinger D, Niebler B, Katinger H, Egorov A. Hyperattenuated recombinant influenza A virus nonstructural-protein-encoding vectors induce human immunodeficiency virus type 1 Nef-specific systemic and mucosal immune responses in mice. J Virol. 2001;75:8899–8908. doi: 10.1128/JVI.75.19.8899-8908.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fonseca W, Ozawa M, Hatta M, Orozco E, Martinez MB, Kawaoka Y. A recombinant influenza virus vaccine expressing the F protein of respiratory syncytial virus. Arch Virol. 2013 doi: 10.1007/s00705-013-1932-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Victor ST, Watanabe S, Katsura H, Ozawa M, Kawaoka Y. A replication-incompetent PB2-knockout influenza A virus vaccine vector. J Virol. 2012;86:4123–4128. doi: 10.1128/JVI.06232-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ohmit SE, Petrie JG, Cross RT, Johnson E, Monto AS. Influenza hemagglutination-inhibition antibody titer as a correlate of vaccine-induced protection. J Infect Dis. 2011;204:1879–1885. doi: 10.1093/infdis/jir661. [DOI] [PubMed] [Google Scholar]
- 49.Cox RJ, Hovden AO, Brokstad KA, Szyszko E, Madhun AS, Haaheim LR. The humoral immune response and protective efficacy of vaccination with inactivated split and whole influenza virus vaccines in BALB/c mice. Vaccine. 2006;24:6585–6587. doi: 10.1016/j.vaccine.2006.05.040. [DOI] [PubMed] [Google Scholar]
- 50.Brett IC, Johansson BE. Immunization against influenza A virus: comparison of conventional inactivated, live-attenuated and recombinant baculovirus produced purified hemagglutinin and neuraminidase vaccines in a murine model system. Virology. 2005;339:273–280. doi: 10.1016/j.virol.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 51.Kim YC, Quan FS, Compans RW, Kang SM, Prausnitz MR. Formulation and coating of microneedles with inactivated influenza virus to improve vaccine stability and immunogenicity. J Control Release. 2010;142:187–195. doi: 10.1016/j.jconrel.2009.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Quan FS, Kim YC, Yoo DG, Compans RW, Prausnitz MR, Kang SM. Stabilization of influenza vaccine enhances protection by microneedle delivery in the mouse skin. PLoS One. 2009;4:e7152. doi: 10.1371/journal.pone.0007152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Karron RA, Wright PF, Belshe RB, Thumar B, Casey R, Newman F, Polack FP, Randolph VB, Deatly A, Hackell J, Gruber W, Murphy BR, Collins PL. Identification of a recombinant live attenuated respiratory syncytial virus vaccine candidate that is highly attenuated in infants. J Infect Dis. 2005;191:1093–1104. doi: 10.1086/427813. [DOI] [PubMed] [Google Scholar]
- 54.Wright PF, Karron RA, Madhi SA, Treanor JJ, King JC, O'Shea A, Ikizler MR, Zhu Y, Collins PL, Cutland C, Randolph VB, Deatly AM, Hackell JG, Gruber WC, Murphy BR. The interferon antagonist NS2 protein of respiratory syncytial virus is an important virulence determinant for humans. J Infect Dis. 2006;193:573–581. doi: 10.1086/499600. [DOI] [PubMed] [Google Scholar]
- 55.Murphy BR, Sotnikov AV, Lawrence LA, Banks SM, Prince GA. Enhanced pulmonary histopathology is observed in cotton rats immunized with formalin-inactivated respiratory syncytial virus (RSV) or purified F glycoprotein and challenged with RSV 3-6 months after immunization. Vaccine. 1990;8:497–502. doi: 10.1016/0264-410x(90)90253-i. [DOI] [PubMed] [Google Scholar]
- 56.Zhang P, Gu H, Bian C, Liu N, Li Z, Duan Y, Zhang S, Wang X, Yang P. Characterization of recombinant influenza A virus as a vector expressing respiratory syncytial virus fusion protein epitopes. J Gen Virol. 2014;95:1886–1891. doi: 10.1099/vir.0.064105-0. [DOI] [PubMed] [Google Scholar]
- 57.General recommendations on immunization --- recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2011;60:1–64. [PubMed] [Google Scholar]
- 58.Castilow EM, Varga SM. Overcoming T cell-mediated immunopathology to achieve safe RSV vaccination. Future Virol. 2008;3:445–454. doi: 10.2217/17460794.3.5.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Polack FP, Teng MN, Collins PL, Prince GA, Exner M, Regele H, Lirman DD, Rabold R, Hoffman SJ, Karp CL, Kleeberger SR, Wills-Karp M, Karron RA. A role for immune complexes in enhanced respiratory syncytial virus disease. J Exp Med. 2002;196:859–865. doi: 10.1084/jem.20020781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pribul PK, Harker J, Wang B, Wang H, Tregoning JS, Schwarze J, Openshaw PJ. Alveolar macrophages are a major determinant of early responses to viral lung infection but do not influence subsequent disease development. J Virol. 2008;82:4441–4448. doi: 10.1128/JVI.02541-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reed JL, Brewah YA, Delaney T, Welliver T, Burwell T, Benjamin E, Kuta E, Kozhich A, McKinney L, Suzich J, Kiener PA, Avendano L, Velozo L, Humbles A, Welliver RC, Sr., Coyle AJ. Macrophage impairment underlies airway occlusion in primary respiratory syncytial virus bronchiolitis. J Infect Dis. 2008;198:1783–1793. doi: 10.1086/593173. [DOI] [PubMed] [Google Scholar]
- 62.Shirey KA, Lai W, Pletneva LM, Karp CL, Divanovic S, Blanco JC, Vogel SN. Role of the lipoxygenase pathway in RSV-induced alternatively activated macrophages leading to resolution of lung pathology. Mucosal Immunol. 2014;7:549–557. doi: 10.1038/mi.2013.71. [DOI] [PMC free article] [PubMed] [Google Scholar]