Abstract
Pregnant and parenting adolescents often experience high rates of intimate partner violence (IPV) and its sequelae posttraumatic stress disorder (PTSD) and depression. Narrative Exposure Therapy (NET) is an innovative intervention that has demonstrated strong preliminary evidence in improving mental health. The specific aims of this article are threefold: a) provide a brief background about IPV-related PTSD and depression among pregnant and parenting adolescents, b) describe NET’s theoretical principals, its therapeutic process, and provide review of existing evidence and c) to discuss NET as a potential treatment to address that mental health burden among adolescents experiencing IPV-related PTSD and depression.
Keywords: Narrative Exposure Therapy, posttraumatic stress disorder, depression, adolescents, intimate partner violence
Adolescent parents of both genders and pregnant adolescents experience high rates of intimate partner violence (IPV).1,2 Despite this, there are a paucity of evidence-based, developmentally appropriate interventions to treat subsequent posttraumatic stress disorder (PTSD) and depression. Narrative Exposure Therapy (NET) is an innovative, individual, therapeutic intervention that has demonstrated strong preliminary evidence in improving mental health outcomes in people experiencing multiple traumas, particularly war, torture and mass disasters. Specifically, researchers and clinicians developed NET for their clients facing crisis and unstable situations, such as persistent war and conflict resultant trauma.3 While it has been modified and tested in children and adolescents,4–8 to date, we found no published studies testing NET’s impact on adolescents experiencing IPV-related PTSD. Therefore, the purpose of this paper is to propose utilizing NET with a new population, parenting adolescents (male and female) and pregnant adolescents (herein referred to as pregnant or parenting adolescents) who experience IPV-related PTSD and depression. While IPV-involved adolescents experience depression and PTSD, many of these youth have lifetime trauma histories, which also result in a lasting mental health burden. Yet, these diagnoses remain unidentified, untreated, and burdensome, often leading to additional violence experiences and the intergenerational transmission of violence. The specific aims of this article are to: a) provide a brief background about IPV-related PTSD and depression among adolescents, particularly those parenting and pregnant; b) describe NET’s theoretical principals, its therapeutic process, and provide review of existing evidence and c) to discuss NET as a potential community-based treatment to address the mental health burden associated with IPV.
Background
IPV among adolescents
Rates of IPV are unacceptably high among both male and female adolescents; 10% of adolescents report being purposefully hit, slapped, or physically hurt by a partner in the past 12 months9 and almost 3% have experienced a serious form of IPV in their lifetime.10 Intimate partner violence is defined as physical, sexual, or psychological/emotional violence (including stalking) within a current or former dating relationship, face-to-face and/or electronically.11 Experiencing IPV in adolescents is often the start of the cycle of violence; 7% of adolescents will experience persistent IPV victimization in young adulthood.12 Adolescent IPV is bilateral, often with females reporting higher rates of violence perpetration.2,13,14
PTSD and depression are the most common mental health co-morbidities related to adolescent IPV.10,15 PTSD is classified anxiety disorder lasting at least four weeks, based on the Diagnositc Statistical Manual (Version Four) (DSM-IV).16 Children and adolescents can develop PTSD following exposure to a traumatic event such as interpersonal violence and sexual abuse. PSDT describes the clustering of symptoms after the event including re-experiencing the trauma, avoidance behaviors, and excessive arousal.16 PTSD is also associated with significant academic and social impairments.17 Depression is classified by depressed mood or loss of interest or pleasure present over the same two weeks.18 Depression in adolescents has been linked to poor functioning, lifetime depressive episodes, suicide behavior, poor physical health and engagement in risk behavior.19
An adolescent reporting IPV is 3.6 times more likely to experience PTSD and 3.7 times more likely to experience a major depressive episode than a peer reporting no IPV and cumulative IPV exposure increases these risks.10,20 Furthermore, adolescents suffering from PTSD symptoms have an increased risk of IPV revictimization and injury severity.21,22 Many statistics of IPV are among those accessing shelter or other services; still among a community sample of young women who have experienced IPV, over half of them met criteria for PTSD (57%) or depression (56%).23
Pregnancy and adolescent IPV
Adolescents experiencing either past or current physical abuse were almost 3–6 more likely to become pregnant.24,25 Among pregnant adolescents, IPV prevalence rates range from 1–38%; consistently higher than in their adult counterparts.26–31
The consequences of prenatal violence are serious. Adolescents exposed to prenatal violence, including IPV, are at higher risk for poor birth outcomes including preterm births, second trimester bleeding, and low birth weight babies.31,32 Furthermore, pregnant adolescents experiencing IPV are at a much greater risk for PTSD, depression, and suicidal thinking than their non-pregnant peers or their pregnant peers not experiencing violence.33,34
Parenting adolescents and IPV
Among adolescent parenting couples, 44% (69 of 158) reported IPV.35 Parenting adolescents often experience a rise in violence severity with a prevalence of 40% in the 3rd postpartum month increasing to 62% by the 2nd year.36 Adolescent mothers experiencing IPV are at a much higher risk for PTSD and depression than their nonparenting counterparts.37–39 Rates of positive screens for postpartum depression nearly doubled for those experiencing recent IPV in a sample of predominantly young, urban mothers.37 The effects of adolescent IPV on continued abuse and mental health are long-lasting. Adolescent mothers who report IPV are more likely to have continued IPV exposure through adulthood and concomitant depression.40 Among young adult mothers (ages 18–21), IPV was signficantly associated with depression and anxiety.41
Effect of IPV exposure on children
IPV during pregnancy and during the post-partum period contributes to the intergenerational cycle of violence, as children exposed to adult IPV are at increased risk for experiencing IPV, engaging in behavior risks and poor mental health, including PTSD.42–45 Among adolescent parents, IPV was related to poor infant temperament and lower parenting competence, mediated by depression.46 Children of parents experiencing violence are at risk for relational PTSD, which predicts that a child’s response to trauma is heightened because the parents’ responses are not well regulated.47 Nearly half of the infants that have been exposed to parental IPV in their first year experienced at least one trauma symptom as reported by their mother.48 Infants whose mothers’ experienced physical IPV reported their infants to have poorer health then their peers.49 Adolescent mothers who have experienced IPV have a decreased level of parental engagement and more likely to endorse corporal punishment and harsh intrusive parenting and less likely to exhibit sensitive supportive parenting.39,50 Witnessing parent experiences of IPV is associated with neglect and the impact extends throughout the lifespan of the child increasing risk for mental health issues and risk behaviors, including substance abuse.51
IPV and socioeconomic risk factors among pregnant and parenting youth
Notably, the risk of IPV-related PTSD and depression increases for young pregnant or parenting youth from urban, low-resourced neighborhoods52,53 and those who experience childhood family violence, disorder, and traumatic stressors.22,54 A recent study of low-income pregnant Latinas; reports of physical violence were 44%.2 Another study of low-income adolescents demonstrated that of those reporting violence (16%), almost 60% reported severe violence and were significantly more likely to report multiple episodes of violence.32,55 Intraparental violence and having peers in violent dating relationships increases the odds that adolescents will engage in IPV.56 However, all adolescents who experience lifetime trauma, including IPV, will not develop PTSD or depression. Factors that predict vulnerability to PTSD include social-ecological factors such as poverty, lack of family support, and family distress.53 Homeless youth report low levels of connectedness (low to average), high rates of emotional trauma (74%), physical abuse (70%), and sexual abuse (55%) increasing their susceptibility to PTSD and depression.57 Furthermore, multiple traumas can have a cumulative effect on PTSD severity.3,58 Many adolescents who have been victimized in dating relationship have experienced multiple traumas, life stressors, and other types of victimization.10,59
Gaps in adolescent IPV research
Research in adolescent IPV has focused predominantly in two areas. First, researchers have been successful in identifying social determinants related to risk of experiencing IPV and determining it’s physical and mental health consequences, including depression, suicidal ideation, and substance use.58,60 Second, intervention research has focused on testing primary prevention strategies, including effective interventions such as Safe Dates61 and Start Strong.62
Despite making strides in primary prevention, evidence-based interventions for adolescents experiencing IPV and its mental health correlates are very limited. Little evidence exists to support effective treatment for adolescents who have already experienced IPV and related mental health outcomes. The majority of literature on the topic of adolescent IPV and mental health interventions is focused on treatment of children who have witnessed parental IPV.63,64 Furthermore, existing interventions for adolescents experiencing IPV, target only the disruption of IPV rather than providing treatments for mental health issues related to trauma experience. Cunningham and colleagues (2013) report that a brief motivational interview with adolescents in an emergency department can significantly decrease the severity of dating violence one-year post intervention. However, data were not collected on mental health symptoms at the time of the intervention or at the follow-ups. There is considerably more evidence for treatment for postpartum depression not related to trauma.65 Yet still, there is a lack of effective interventions that target treatment for postpartum depression among adolescents.54
Narrative Exposure Therapy (NET)- Innovative Ideas to Treat PTSD
NET: Theoretical principles
Stress predominantly activates the two body systems that target the brain: 1) the hippocampus (responsible for memory) and the hypothalamic-pituitary-adrenal (HPA) axis (regulates cortisol) and the 2) amygdala (develops and processes emotions).3 Characterized as a disorder of hyperbolic defensive physiological arousal, PTSD sensitizes individuals to subsequent stress and prolongs extreme emotional dispensation across several physiological spheres.66,67 Specifically, studies relate PTSD and trauma to differences in norepinephrine, dopamine, emotional regulation, which are all activated by stress.68 Excessive and prolonged activation of the stress system as with individuals that suffer from PTSD, however, might lead to enduring psychopathology and physical complications.69 Particularly affected in PTSD are the HPA axis where persistent, invasive memories and impaired memory retrieval develops.3 The cognitive processing model postulates that PTSD results from a fragmented narrative maintained through distorted and detached autobiographic memory of trauma.3,70 The emotional processing theory of PTSD postulates that the repeated assault impairs the amygdala responsible for emotional regulation.3 As a result, emotional and autobiographic memory become fragmented and leads to impaired functioning, hyperarousal, dissociation, flashbacks, avoidance and depression.
Adolescents are more vulnerable to trauma than adults due to their malleable endocrine systems during puberty; the HPA axis influences the gonadal, growth hormone, and thyroid axis. Trauma during adolescence could have irreversible effects on growth and development, particularly brain.69 Ongoing exposure to traumatic events is also associated with more severe and chronic PTSD and increased morbidity rates like depression.71–74
Individuals with PTSD exist in a state of hyperarousal as evidenced by sleep difficulties, hypervigilence, and startle response.75 In a study using magnetoencepholagraphy, Adenauer and colleagues (2010) demonstrated that patients with PTSD had a biphasic response to adverse pictures not present in neutral pictures. They hypothesized that the early prefrontal increased cortex response represents the enhanced alarm response and the secondary decreased activation of the parieto-occipital areas represented the emotional disengagement common in PTSD patients.76
A particularly promising intervention to treat PTSD and depression related to experiencing multiple traumas is NET,3,77,78 which is an exposure therapy emphasizing the importance of documentation of past trauma endured as told by the client to a therapist.77 NET is rooted in Cognitive Based Therapy (CBT) and Testimony Therapy.3 Specifically, NET aims to reconstruct memories and associated emotional regulation, including traumatic events, by providing meaningful linkages and sensory integration. The reconstruction of these memories in the safety of a therapeutic relationship is theorized to treat depressive and PTSD symptoms.3 While trauma-focused CBT has the strongest evidence base for treatment of adolescents with PTSD,79,80 the integration of Testimony Therapy provides symptomatic relief from PTSD through a therapeutic narration and documentation of trauma experiences.81
NET, following CBT principals, aims to change behavior and affect by addressing dysfunctional thinking through the reconstruction of the autobiographical memory.3 Specifically, it seeks to reduce PTSD by reconstructing how the person thinks about and reacts to the trauma and trauma cues. NET is based on the cognitive processing model, therefore the therapist guides the client to correct the fragmented narrative maintained through distorted and detached autobiographic memory of trauma.3,70 It is also based on emotional processing theory and maintains that repeated exposure would habituate emotional responses thereby decreasing PTSD.82 NET takes a relatively new treatment focus on the patients’ lifetime, as it was developed to reduce the symptoms of PTSD caused by multiple traumas.3 Individual therapy sessions allow the client to review all the significant positive and negative events in their life and slow down for active exposure during the most pressing traumatic memories. The therapist assists the patient in integrating fragmented memories into a coherent, contextualized autobiography in concordance with an adaptive emotional response.3
Only one study to date has examined biomedical or neurological mechanisms by which NET is effective. Adenauer and colleagues (2011) examined brain activity directed towards adverse stimuli examining neurophysiological indicators of attention using magnetoencephlographic technology measuring steady state visual-evoked fields (ssVEF) before and after completion of NET therapy. Only in the NET group, parietal and occipital activity towards threatening pictures increased significantly after therapy. This response represents a reassessment of current danger thereby reducing PTSD symptoms.83 Participants in the NET group had a corresponding decrease in PTSD and depression symptoms.
The NET Therapeutic Process
NET is a standardized and manualized treatment.3 All of the studies referenced the standardized manual or KidNET (based on the manual). (see table 1). KidNET the NET modified for children to include multiple illustrative strategies, including drawings and role-play and a focus on future appeared to be the only significant modification of the manual. However, some successful NET modifications included adding particular psychological modalities including biofeedback, which alone did not significantly reduce PTSD symptoms),84 or grief session.7
Table 1.
Table of Studies Examining effects of Narrative Exposure Therapy (NET)
| Study | Purpose | Design
& comparison group |
Sample (N) Setting |
Intervention/ Interventionists / Fidelity/ Treatment condition |
Main Results (within treatment effect sizes) (Cohen’s d) |
|---|---|---|---|---|---|
| Adenauer, H., Catani, C., Gola, H., Keil, J., Ruf, M., Schauer, M., & Neuner, F. (2011). Narrative exposure therapy for PTSD increases top-down processing of aversive stimuli--evidence from a randomized controlled treatment trial. BMC Neuroscience, 12, 127. A3 | To examine whether NET causes changes in affective stimulus processing in patients with chronic PTSD | RCT: ET compared to WLC |
Sample: N=34 Refugees with PTSD.
History of organized violence, persecution & current PTSD
diagnosis (ages 16–56) Setting: University of Konstanz, Germany Psychological Research and Outpatient Clinic for Refugees. |
Intervention: NET: (standardized
manual) 12 therapy sessions, weekly or bi weekly (M=108 min SD 1M7 min) Interventionists: Clinical psychologists with expertise in NET & PTSD. Therapeutic competence & treatment fidelity: Regular supervision. Testimonies were checked for vividness and consistency to ensure proper application- no major deviations noted. Treatment completion: NET: 16/18 (Deportation) WLC 16/18 (Deportation) |
In treatment completers, time ×
treatment interaction revealed difference in decreased PTSD symptoms [(F
(1,17)=34.99, p<.001) and decreased depression rating [F (1,
17)=13.2), p<.005) for those in NET group as compared to WLC at
4 months follow-up NET within group effect sizes were d=2.21 for PTSD and d=1.56 for depression. Only in the NET group, parietal and occipital activity towards threatening pictures increased significantly after therapy (NET: t= −3.35, p = .007). (WLC: t = 0.58, p = .58). |
| Bichescu, D., Neuner, F., Schauer, M., &Elbert, T. (2007). Narrative exposure therapy for political imprisonment-related chronic posttraumatic stress disorder and depression. Behaviour Research and Therapy, 45(9), 2212–2220. | To compare NET with Psychoeducation (PED) effectiveness of decreasing PTSD and depression among political detainees | RCT: NET compared to PED (nature and prevalence of PTSD) |
Sample: N=18 political detainees
with significant trauma in remote
past Setting: Romania at subsidiaries of the Association of Former Political Detainees in Iasi and Brosov and at the University |
Intervention: NET: 5 sessions
(ca. 120 min per session weekly/biweekly) or PED: 1
session Interventionists: 1 female PhD psychology student from University of Konstanz trained in NET. Therapeutic competence & treatment fidelity: Supervision by documentations by email Treatment completion: NET 9/9 PED 9/9 |
Time × treatment interaction revealed
difference in decreased PTSD symptoms [(F(1, 16)= 20.80, p<.001,
n2=.60]and for depression scores [(F(1, 16)= 6.50,
p<.05, n2=.35] for those in NET compared to
PED. NET effect sizes were d=3.15 for PTSD and d=0.97 for depression (6 months) |
| Catani, C., Kohiladevy, M., Ruf, M., Schauer, E., Elbert, T., & Neuner, F. (2009). Treating children traumatized by war and Tsunami: A comparison between exposure therapy and meditation-relaxation in North-East Sri Lanka. BMC Psychiatry, 9, 22. | To examine, whether highly affected children with a preliminary diagnosis of PTSD would profit more from KIDNET or from a mediation-relaxation protocol. | RCT: KIDNET compared to mediation-relaxation protocol (MED-RELAX) |
Sample: N=31 children (ages
8–14) with PTSD who have experienced recent mass disaster
(Tsunami) and also (ca. 120 min per session, weekly/biweekly) civil
war Setting: Sir Lanka newly erected refugee camp |
Intervention: KIDNET: 5 NET
sessions modified for children and adolescents MED-RELAX: 6 sessions. Both treatments 60–90 minutes within 2 weeks Interventionists: 6 female, trained local teachers (master counselors-76 training days (≈10 hours/day) with focus on NET, basic counseling, diagnostic tests, and MED-RELAX. 4 day refresher course. Therapeutic competence & treatment fidelity: Supervision by local trainers. Therapists completed detailed protocol after each session and 2 clinical psychologists (University of Konstanz) & local clinical supervisor carried out random observations of single therapy sessions. Regular supervision meetings were offered to therapist team. No major deviations noted Treatment completion: NET 16/16 MED-RELAX 15/15 |
Time × treatment interaction revealed
no significant differences between NET and
MED-RELAX. Both treatment conditions had significant decrease in PTSD symptoms and impairment in function at 1 month after and remained stable. NET effect size d=1.76 (post treatment) and d= 1.96 (6 month follow-up). MED-RELAX effect sizes d=1.83 and d= 2.20. |
| Ertl, V., Pfeiffer, A., Schauer, E., Elbert, T., & Neuner, F. (2011). Community-implemented trauma therapy for former child soldiers in northern Uganda: A randomized controlled trial. JAMA, 306(5), 503–512. | To assess the efficacy of a community-based intervention targeting symptoms of PTSD in formerly abducted individuals. | RCT: NET (N=29) compared to Academic Catch -up with supportive counseling (N=28) or wait list (N=28) |
Sample: N= 85 former Ugandan
child soldiers with PTSD (ages
12–25) Setting: 3 study areas in Uganda with varying distances from war exposure, internally displaced persons camps and new settlements. Treatment in patient homes |
Intervention: NET: 8 sessions
(90–120 minutes), 3 times weekly based on standardized manual
and KIDNET. Academic catch-up and supportive counseling: Intensive
educational catch-up training (55%) and psychoeducation plus
basic counseling. Interventionists: Intensively trained local counselors (7 woman &7 men) Therapeutic competence & treatment fidelity: case discussions in supervision meetings, observation and evaluation of treatment sessions via video recordings, and review of the obligatory treatment process notes for each session. NET testimonies were reviewed to check for trauma focus and data richness. No deviations from protocol noted. Treatment completion: NET: 28/29 Academic/Counseling: 27/28 Wait list: 28/28 |
Time × treatment interaction revealed
a superiority of NET compared with academic catch-up (F1,234.1 = 5.21, P
= .02) and wait-listing (F1,228.3 = 5.28, p = .02). NET effect size: d = 1.80 Academic catch-up effect size: d = 0.83 Wait-listing effect size: d = 0.81 (all 12 month) |
| Hijazi, A. M., Lumley, M. A., Ziadni, M. S., Haddad, L., Rapport, L. J., &Arnetz, B. B. (2014). Brief narrative exposure therapy for posttraumatic stress in Iraqi refugees: A preliminary randomized clinical trial. J Trauma Stress, 27(3), 314–322 | To test the efficacy of an adapted, culturally sensitive, brief NET in a sample of traumatized Iraqi refugees | RCT: Brief NET vs WLC |
Sample: N= 63 Iraqi refugees
exposed to violent or traumatic event related to refugee status and they
were bothered by it, though repeatedly about it or felt they had not
overcome it. Setting: Southeast Michigan community refugee settings with services provided but no intense therapy |
Intervention: Brief NET: 3
sessions in Arabic from structured
manual Interventionists: 2 doctoral students in clinical psychology. Trained and supervised (weekly) by clinical psychologist with expertise in exposure therapy. Therapeutic competence & treatment fidelity: Trained and weekly supervision by clinical psychologist with expertise in exposure therapy. Treatment completion: NET: 39/41 |
Time × treatment interactions revealed NET had significantly greater posttraumatic growth (d = 0.83) and well-being (d = 0.54) through 4 months than controls. |
| Halvorsen, J. O., &Stenmark, H. (2010). Narrative exposure therapy for posttraumatic stress disorder in tortured refugees: A preliminary uncontrolled trial. Scand J Psychol, 51(6), 495–502 | To examine the effectiveness of NET specifically among tortured refugees residing in a Western country. | Quasi-experimental (no control) |
Sample: N=16 adult torture
survivors, refugee and asylum seekers with
PTSD Setting: Psychiatric outpatient clinics in Mid-Norway health region. |
Intervention: NET: 10 sessions
based on standardized NET manual (90 minutes). 9 NET sessions had
professional interpreter present, 3 professional phone
interpreters. Interventionists: 15 Mental health professionals. Experts from the University of Konstanz and the aid organization VIVO trained the mental health professionals during a 5-day workshop plus 2-day workshops twice every 6th month to maintain their skills. Therapeutic competence & treatment fidelity: Therapists received individual supervision after 4, spaced, sessions and self-report measure if used main NET ingredients. No deviations noted Treatment completion: NET: 16/16 |
Decrease in PTSD scores (F (2,30)=13.72, p
=000). Decrease in depressive symptoms [F (2,30)= 6.94),
p=0.003) NET effect size = 1.16 for PTSD and 0.84 for depression |
| Hensel-Dittmann, D., Schauer, M., Ruf, M.,
Catani, C., Odenwald, M., Elbert, T., &Neuner, F. (2011).
Treatment of traumatized victims of war and torture: A randomized
controlled comparison of narrative exposure therapy and stress
inoculation training. PsychotherPsychosom, 80(6), 345–352 |
To compare the outcome of 2 active treatments for PTSD as a consequence of war and torture: NET and stress inoculation training (SIT) | RCT: NET compared to stress inoculation training (SIT) |
Sample: N=28 Refugees and asylum
seekers with PTSD Setting: Research & Outpatient Clinic for Refugees in Konstanz, Germany |
Intervention: NET: 10 sessions based on
standardized manual (90 minutes). Ave 9 days before treatments. 17 cases
professional interpreter. Interventionists: Trained staff from Research and Outpatient Clinic for Refugees. Therapeutic competence & treatment fidelity: Treatment sessions were videotaped and randomly analyzed. Treatment implementation discussed in team sessions. Treatment completion: NET: 12/15 SIT: 11/13 |
Time × treatment interactions revealed
NET had significantly symptom reduction [F (3,52)= 3.08;
p<.05]. NET effect size=1.42 &1.59 for PTSD symptoms (6 months, & 1 year) STI effect size for PTSD symptoms = 0.12–0.19 for (6 months, 1 year) No change for depression or other co-morbid conditions |
| Morina, N., Maier, T., Bryant, R., Knaevelsrud, C., Wittmann, L., Rufer, M., … Muller, J. (2012). Combining biofeedback and Narrative Exposure Therapy for persistent pain and PTSD in refugees: A pilot study. Eur J, Psychotraumatol, 3. | To present data on a pilot treatment [NET and biofeedback (BF)] study conducted with 15 traumatised refugees with persistent pain and PTSD | Pilot study: NET and biofeedback (no control) |
Sample: N=15 Refugees with
experience of war/torture persistent pain and
PTSD Setting: Outpatient Unit for Victims of Torture and Ware in the Department of Psychiatry and Psychotherapy (University Hospital of Zurich) |
Intervention: Combined 10-session
BF program followed by 10-session trauma-focused NET
protocol Interventionists: 4 postgraduate clinical psychologists who had received special training in NET Therapeutic competence & treatment fidelity: Weekly supervision Treatment completion: BF+ NET 15/18 |
Objective was to provide information on
feasibility, acceptance and safety. Findings indicated intervention to
be feasible, well accepted, tolerated &
safe. Time × treatment interaction revealed significance in PTSD [F (1.3, 18.39) = 22.01, p < .001] BF +NET Effect sizes: 0.1, 1.43, −.0.01 for PTSD |
| Neuner, F., Onyut, P. L., Ertl, V., Odenwald, M., Schauer, E., & Elbert, T. (2008). Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 76(4), 686–694. | To examine whether trained lay counselors can carry out effective treatment of PTSD in a refugee settlement | RCT: NET compared to flexible trauma counseling (TC) and non-treatment group. |
Sample: N= 277 Rwandan and
Somalian refugees who were diagnosed with
PTSD Setting: African refugee settlement in Uganda |
Intervention: NET: 6 sessions
based on standardized manual. Usually 2 sessions per week, 1–2
hours) Interventionists: Trained local, lay counselors (9 refugees from community with literacy (English & mother tongue, empathy & motivation)- 6 week course, general counseling skills and NET & trauma training) Therapeutic competence & treatment fidelity: Case and personal supervision weekly. Treatment adherence discussed by case in supervision meetings, direct observation of treatment and review of testimonies and treatment protocols. No major deviation noted. Treatment completion: NET: 86/111 TC: 85/111 |
Time × treatment interaction for NET
and non treatment group revealed significance in PTSD [F (1, 112)=8.2,
p=.005]. No significant difference between NET and TC NET effect sizes: d= 1.4 and 1.4 in PTSD (post-test & 6 month Follow-up |
| Onyut, L. P., Neuner, F., Schauer, E., Ertl, V., Odenwald, M., Schauer, M., & Elbert, T. (2005). Narrative Exposure Therapy as a treatment for child war survivors with posttraumatic stress disorder: two case reports and a pilot study in an African refugee settlement. BMC Psychiatry, 5, 7. | To created and evaluated the efficacy of KIDNET, a child-friendly version of Narrative Exposure Therapy (NET), as a short-term treatment for children | Pilot study: no control |
Sample: N=6 Somali refugee
children suffering from PTSD aged 12–17
years Setting: Uganda refugee settlement |
Intervention: KIDNET: 4–6
sessions of child-friendly version of NET lasting 1–2
hours Interventionists: Expert clinicians experienced with NET Therapeutic competence & treatment fidelity: none indicated Treatment completion: NET: 6/6 |
Time × treatment effect: F (2,5)= 15.45, p< 0.01. PTSD symptom reduction (post test and 9 month follow-up) |
| Pabst, A., Schauer, M., Bernhardt, K., Ruf, M., Goder, R., Rosentraeger, R., … Seeck-Hirschner, M. (2012). Treatment of patients with borderline personality disorder and comorbid posttraumatic stress disorder using narrative exposure therapy: a feasibility study. Psychotherapy and Psychosomatics, 81(1), 61–63 | To test the feasibility of narrative exposure therapy (NET), a trauma-focused therapy suitable for both in- and outpatient settings which can be taught to clinically experienced therapists in a short-term training program and implemented in a comprehensive treatment for borderline personality disorder (BPD) patients with comorbid PTSD. | Feasibility study |
Sample: N= 10 woman (ages
19–45) with BPD and PTSD Setting: Center for Integrative Psychiatry in Kiel, Germany |
Intervention: NET sessions (average 14
based on severity and amount of trauma) standardized manual, 90 minutes,
1–2 times weekly Interventionists: Expert clinicians with 2-day NET training by NET multi-professional team Therapeutic competence & treatment fidelity: Weekly team meetings and biannual supervision to assurance adherence to manual guidelines Treatment completion: NET: 10/10 |
NET: significant reduction in PTSD symptoms
(p< .05) and depression (p<.05) NET effect size (Hedges’g)= 0.92 (PTSD) and .89 (depression) (6 months) |
| Ruf, M., Schauer, M., Neuner, F., Catani, C., Schauer, E., & Elbert, T. (2010). Narrative exposure therapy for 7- to 16-year-olds: a randomized controlled trial with traumatized refugee children | To examine the effectiveness of narrative exposure therapy for children (KIDNET) in treating posttraumatic stress disorder (PTSD) in refugee children living in exile | RCT: NET compared to WLC |
Sample: N=26 refugee children
(ages 7–16) traumatized by organized violence and diagnosed with
PTSD Setting: Research-Outpatient clinic for Refugees at the University of Konstanz, Germany |
Intervention: KIDNET: ≈8
sessions, 90–120 minutes,
weekly Interventionists: 8 clinical psychologists (4 PhD students, 2 senior researches at PhD-level and 2 professors of clinical psychology with experience in treatment of war and organized violence survivors). Professional translators in 7 cases Therapeutic competence & treatment fidelity: not indicated Treatment completion: NET; 13/13 |
Time × treatment [F91,24)= 7.56,
p=.01) NET effect size: 1.9, p= .001 (6 month follow-up) |
| Schaal, S., Elbert, T., &Neuner, F. (2009). Narrative exposure therapy versus interpersonal psychotherapy. A pilot randomized controlled trial with Rwandan genocide orphans. PsychotherPsychosom, 78(5), 298–306. | To evaluate the efficacy of treatment modules for trauma spectrum disorders in a sample of Rwandan genocide orphans | RCT: NET compared to interpersonal therapy (IPT) in group |
Sample: N=26 youth (ages
14–28) living in child-headed households or orphanages in
Kigali, Rwanda. Setting: Rwanda |
Intervention: NET: 3 sessions + I
grief session, weekly, 2–2.5 hours. Based on standardized
modules IPT; Group (3–4 people), 4 sessions. Both treatments with professional interpreters. Interventionists: 2 female counselors from University of Konstanz with experience in the applied treatment modules Therapeutic competence & treatment fidelity: Weekly supervision meetings Treatment completion: NET 12/12 IPT 14/14 |
Between group differences: PTSD: F (1,23)=7.68; p<0.01 Depression: F (1,23)= 5.20, p< .05 NET effect sizes 0.39, 0.71 IPT effect size: 0.23, 0.00 (3, 6 month follow-up) |
| Zang, Y., Hunt, N., & Cox, T. (2013). A randomised controlled pilot study: The effectiveness of narrative exposure therapy with adult survivors of the Sichuan earthquake. BMC Psychiatry, 13, 41. | To evaluate the efficacy of Narrative Exposure Therapy (NET) as a short-term treatment for PTSD using Chinese earthquake survivors | RCT pilot: NET compared to WLC |
Sample: N=22 adults recently
diagnosed with PTSD site of Sicuan earthquake in
China Setting: Beichaun County, China |
Intervention: NET: 4 sessions
based on manual, 60–90 minutes over 2
weeks Interventionists: 3 female master level psychologist therapists, native Chines speakers, trained in NET Therapeutic competence & treatment fidelity: Tutored under supervision, case and personal supervision were maintained on weekly basis. Treatment adherence direct observation of treatment, case discussion in supervision meetings, and a review of records and treatment protocols Treatment completion: NET: 11/11 |
Time × treatment comparison revealed
significant differences for 3 subscales of PTSD [F (1,19)= 28.99, 22.20,
& 57.30; p<.001] NET effect sizes 1.09, 1.35, 1.30 for 3 subgroups, WLC effect sizes 0.09, 0.35, 0.16. |
Key:
RCT= Randomized Control Trial
WLC= Waitlist Control
PTSD: Posttraumatic Stress Disorder
Fidelity measures included observing sessions live, video taped or checking session transcripts for NET components (e.g. trauma focus, data richness) as detailed in the manual.4,8,83,85–88. One study used a therapist self-report measure of main NET ingredients (e.g. psychoeducation, lifeline exercise, and prolonged exposure to traumatic memories.89 However, the fidelity measures used in the studies have not been published yet.
NET is a short-term treatment; typically NET has been completed in 8–12 sessions.3 However, one modification made by researchers has been to decrease the session numbers (3–6 sessions).7,86,88,90,91 The shortened sessions has been supported by the documentation of Initial relief has been documented within 3 sessions of NET3 and effectiveness in shortened studies. For example, a study examining a brief modification of NET (3 sessions) determined increase of well-being and symptoms reduction in a sample of Iraqi refugees.90 Notably, the authors attributed the therapy’s modest effect as compared to other studies to the short-term therapy. However in the original NET, the therapist determines the number of sessions based on the severity and number of traumatic events.3 Additionally, participant age may impact the number of sessions needed. KidNET, developed for adolescents and children, is conducted within 4–10 sessions.92 Most frequently, KidNET has been tested with 4–6 sessions.4,5,7 NET Sessions were developed to typically last 90–120 minutes, supported by studies examined.3
NET was developed and has been tested predominantly with intervention delivered by clinical psychologists or master-level clinicians with expertise in NET and PTSD.6,83,84,87,88 Other studies indicated doctoral or psychology students delivered the intervention6,90,91 or expert clinicians or mental health professionals5,7,85,87,89 but did not detail level of education or training. However, to improve access to transient populations, implementation studies have been conducted with NET using trained lay counselors.4,8,86 Lay counselors completed advanced training over 6–8 weeks that included basic counseling, diagnostic testing and NET. The trainings were lead by expert NET and trauma therapists. Three studies supported evidence that these trained lay therapists were able to administer effective treatment with intense training4,8,86 demonstrating that a clinical psychotherapist is not necessary to provide effective treatment. The efficacy of NET delivered by trained local counselors was supported in populations of children experiencing PTSD as well.4 This supports the fact that NET is amenable and sustainable to IPV-involved adolescents in community agencies with mental health staff that are well trained and supervised. Adolescents in community agencies have developed a relationship with the counselors there and may be more likely to share such intimate details of painful experiences; thereby increasing the opportunities for follow through with the therapy until completion. Developing the trust in the therapist/client relationship is an important component for the successful implementation of NET.93
Treatment participation is a critical component to effectiveness of NET. The majority of studies documented high therapy completion rates from 88%–100%. Frequent reasons for not completing therapy were unrelated to therapy effects, but rather deportation or asylum procedural difficulties or requiring inpatient hospitalization.83,85 Treatment adherence is one critical measurement of both client acceptance and treatment fidelity.94 Evidence of high rates of treatment completion is a promising feature for an intervention aimed at a population notorious for low rates of treatment adherence associated with increased morbidity and medical complications.95
NET: The evidence
The unique results of NET on PTSD and/or additional mental health conditions have been published in 14 papers (see table 1). The majority of studies (N=9) were randomized controlled trials (RCTs) and the remaining studies were quasi-experimental (no control), pilots or feasibility studies (N=5). (see table 1)
Sample sizes were generally small ranging from 1891 to 858 not including pilot or feasibility study sample sizes. However, one study had a sample size of 277.86 Trauma affected all participants, which included refugees and asylum seekers,6,83,84,86,89,90 political detainees and torture and genocide survivors,85,89,91 survivors of mass disasters and war,4,5,7,85,88 and child soldiers.8 All participants met criteria for PTSD. Samples included children,4–6,8, adolescents and young adults,6–8,83 and adults.83–91 Samples also included participants years removed from the trauma. Bichescu and colleagues (2007) demonstrated NET’s efficacy in decreasing PTSD and depression symptoms in political detainees whose traumatic events included political detention and tortured that occurred over 40 years ago.91 The effect size of 5 sessions of NET on PTSD symptoms was 3.15 and on depression symptoms was .97, both significantly larger as compared to effect sizes of one session of psychoeducation.
Settings
Most of the trials were set in the psychiatric outpatient clinics or government services targeting refugees6,83–85,87,89,91 or refugee or resettlement camps or sites of recent war, violence or mass disaster.4,5,7,8,86,88 Only one study was set in the United States.90 Hijazi and colleagues (2014) recruited at community agencies providing comprehensive services for refugees. However, intensive therapy was not included in such services. Treatment sessions were conducted at the clients preferred site (e.g home, church or community center).
Children and adolescents
Published studies have examined the effect of NET on mental outcomes in children and adolescents (N=5).4–8 The majority of the studies that included children have used KIDNET, a modified version of NET that includes the use of illustrative materials including drawings and role-play to help the children reconstruct the memories. Additionally, the therapist extends the narration beyond the present to discuss future hopes and aspirations.5 Studies have supported positive outcomes in children and adolescents as well.4–8 In studies conducting NET in children and adolescents, NET has demonstrated 67% and 83% remission of PTSD symptoms4–6. In a study of orphans ages 14–28 (N=26), NET was compared to interpersonal psychotherapy. Six months after their intervention, only 25% of the group receiving NET fulfilled PTSD criteria but 71% of those receiving IPT met criteria.7 Ertl and colleagues (2011) demonstrated that NET was more effective in treating PTSD symptoms as compared to academic catch-up intervention in former children soldiers (ages 12–25).
Strengths of the studies
As a group, one of the predominant of the studies’ strengths is that NET as been used in multiple countries and diverse cultures. Therapists and participants have not always spoken the same language and multiple studies have been effective in their use of interpreters.6,7,85,89 However, interventions that trained local therapists have also demonstrated positive outcomes.4,8,86
Studies have also compared NET with other therapies, and generally NET has shown greater efficacy in refugee and political prisoner populations than comparable therapeutic treatments of supportive, trauma counseling86, psychoeducation91 or group interpersonal training7 in decreasing posttraumatic symptoms and depression scores. Furthermore, tortured victims of war receiving NET had significantly greater reduction in PTSD severity scored as compared to their peers treated with stress inoculation treatment (SIT) (effect sizes: NET: d=1.42 vs SIT d=.12).85 In studies including children and adolescents, NET has also shown superiority to other treatment therapies. In children experiencing PTSD, NET has also demonstrated a significant group difference in PTSD severity as compared to an intervention of academic catch-up and supportive counseling for a group of former child soldiers.8 NET had significant larger effects sizes when compared to group interpersonal therapy for children ages 12–25.7 However, in another comparison study in children with PTSD after a mass disaster, both treatments (NET and a mediation-relaxation protocol) demonstrated a decrease in PTSD symptoms and improved functioning; however the differences between the groups were not significant.4
Weakness of studies
Some general study weaknesses emerge from the literature. As discussed, the publications did not detail study fidelity or treatment competence measures. The study samples were also small, with the expectation of Neuner and colleagues (2008) in a refugee settlement (N=277). Therefore larger scale trials are needed.
Three reviews of published and unpublished research has shown that NET is a promising treatment for PTSD and depression, even in insecure settings.77,78,96 NET has shown an average moderate to strong effect size (approximate .40–.65) in treating PTSD in vulnerable populations of refugees.96 Furthermore, Robjant and Fazel’s (2010) systematic review of the literature found NET effective in low-income and middle-resourced (Cohen’s d= 1.29–3.15 at follow-up) (11 RCTs) as well as high resourced areas, transferability across cultures, in children and adolescents (6 RCTs), and in continued volatile situations.77 This supports the potential for NET to be effective in community health agencies that provide social services to residentially unstable adolescents.
Critics of NET may suggest the danger of asking participants to retell their experience will increase stress and chances of or re-experiencing the trauma97. However, the psychotherapy modalities that involve exposure of the patient to trauma-related cues in a safe environment to decrease PTSD symptoms have the most empirical support.98 Therefore, NET, relies on the retelling of one’s narrative in coherent autobiographic memory, as guided by a trained therapist.97 This method of reflection is in congruent with evidence-based treatment of PTSD as determined by the National Institutes of Health and Care Excellence (NICE).99
It is recommended that the effectiveness of NET be examined being in larger scale randomized controlled studies.77,78 Furthermore, NET is being tested in additional populations experiencing PTSD and NET’s impact on other mental health disorders and behaviors,93 including patients with borderline personality disorders87 and chronic pain related to PTSD.84 It has currently not been tested in either IPV-related PTSD or specifically in pregnant or parenting adolescents or adults.
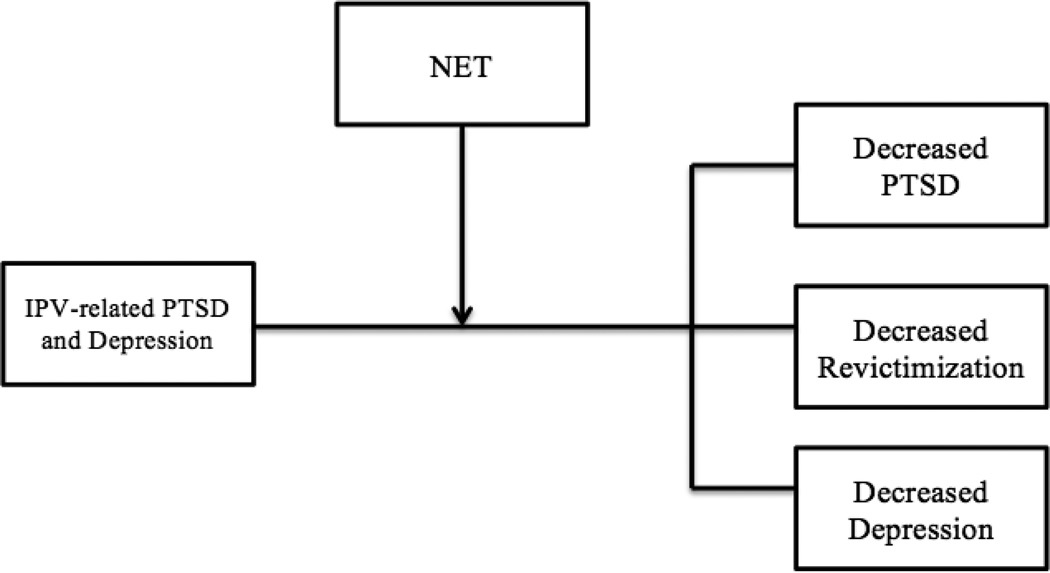
The Proposed Model: NET for IVP-related PTSD pregnant and parenting teens
Because IPV can cause or exacerbate mental health symptoms, and mental health burden is linked to increased risk for IPV, particularly in pregnant and parenting adolescents, we suggest that NET is a potential, innovative intervention to address adolescents’ comorbid issues, thus reducing morbidity and mortality. This notion is based on the current evidence presented supporting the following NET characteristics: 1) effectiveness of NET for adolescents in decreasing PTSD symptoms and depression, in low-resourced and unstable communities and 2) NET is amenable to training community agency staff familiar with the adolescents and unique issues they face. This is hypothesized to improve treatment adherence and consequently effectiveness since building strong relationships between adolescent and therapist has been demonstrated to increase treatment adherence.95 Therefore, future research to test this model has been proposed in community-based agencies and with their dedicated staff, trained and supervised by experts in trauma and NET.
Conclusion
This paper’s objective was to provide an overview of adolescent IPV and mental health, and explore the potential benefits of offering NET, a suitable evidence-based treatment, to pregnant and parenting adolescents exposed to IPV in partnership with community-based agencies. To best meet the needs of adolescents, they must be at the table for the design, implementation and testing of interventions to target their health and wellness.100,101 Community-based participatory research (CBPR) methodology, which has been used with vulnerable populations, is an excellent vehicle to explore the potential of NET with IPV-involved adolescents; in a community setting, with providers they trust. CBPR is a methodology and approach to research which draws on the intervention target as an expert in his or her life and that expertise lends itself to all aspects of intervention testing.100,101 The intervention target, in this case – adolescents – are considered equal partners in all stages of the intervention development, with feedback loops and constant monitoring of the therapeutic process for benefits and unintended consequences. It is possible that researchers shy away from testing novel interventions with this population to institutional review board and human subject concerns regarding vulnerability. Adolescents are considered children under the federal research regulations and because clients of this intervention would also likely be victims of abuse and from lower socioeconomic life courses, they are even more vulnerable. However, with careful planning and interdisciplinary teams that include community-engaged experts who work with adolescents, and the teens themselves, it is possible. The statutory processes designed to protect youth should not be barriers to helping them overcome their adversities with evidence-based interventions
The time is now to move away from prevalence studies and begin to examine how to treat these youth to recover from their lived experiences so that they might continue to live lives that are healthy and begin new trajectories for their children: violence-free.
Figure 1.
NET for IVP-related PTSD pregnant and parenting teens
Acknowledgments
The authors would like to thank our funder, Patricia H. Garman Behavior Health Nursing Fund.
We would like to acknowledge our community partners, Center for Youth, Mercy Community Services, and Alternatives for Battered Woman all of Rochester, New York and the adolescents they serve.
Footnotes
None of the authors have any financial conflict of interest to report.
Contributor Information
Ellen M. Volpe, University at Buffalo, State University of New York, School of Nursing, 3435 Main St, Buffalo, New York 14214, emvolpe@buffalo.edu.
Camille R. Quinn, Department of Psychiatry, School of Medicine & Dentistry, University of Rochester Medical Center, 300 Crittenden Boulevard, Rochester, NY 14642, Camille_Quinn@urmc.rochester.edu.
Kathryn Resch, Department of Psychiatry, School of Medicine & Dentistry, University of Rochester Medical Center, 300 Crittenden Boulevard, Rochester, NY 14642, Kathryn_Resch@urmc.rochester.edu.
Marilyn S. Sommers, Medical-Surgical Nursing, University of Pennsylvania School of Nursing, 418 Curie Boulevard, Fagin Hall, Room 402, Philadelphia, PA 19104 (w) 215-746-8320, ssommer@nursing.upenn.edu.
Elizabeth Wieling, Family Social Science, University of Minnesota, 293 McNH, 1985 Buford Avenue, St Paul, MN 55108, lwieling@umn.edu.
Catherine Cerulli, Director of Susan B. Anthony Center for Woman’s Leadership, Department of Psychiatry, School of Medicine & Dentistry, University of Rochester Medical Center, 300 Crittenden Boulevard, Rochester, NY 14642, Catherine_Cerulli@urmc.rochester.edu.
References
- 1.Kulkarni S, Lewis C, Rhodes D. Clinical Challenges in Addressing Intimate Partner Violence (IPV) with Pregnant and Parenting Adolescents. [2011/11/01];Journal of family violence. 2011 26(8):565–574. [Google Scholar]
- 2.Newman BS, Campbell C. Intimate partner violence among pregnant and parenting Latina adolescents. J Interpers Violence. 2011 Sep;26(13):2635–2657. doi: 10.1177/0886260510388281. [DOI] [PubMed] [Google Scholar]
- 3.Schauer M, Neuner F, Elbert T. Narrative Exposure Therapy: A Short-Term Treatment for Traumatic Stress Disorders. 2n ed. Cambridge, MA: Hogrefe; 2011. [Google Scholar]
- 4.Catani C, Kohiladevy M, Ruf M, Schauer E, Elbert T, Neuner F. Treating children traumatized by war and Tsunami: a comparison between exposure therapy and meditation-relaxation in North-East Sri Lanka. BMC psychiatry. 2009;9:22. doi: 10.1186/1471-244X-9-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Onyut LP, Neuner F, Schauer E, et al. Narrative Exposure Therapy as a treatment for child war survivors with posttraumatic stress disorder: two case reports and a pilot study in an African refugee settlement. BMC psychiatry. 2005;5:7. doi: 10.1186/1471-244X-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ruf M, Schauer M, Neuner F, Catani C, Schauer E, Elbert T. Narrative exposure therapy for 7- to 16-year-olds: a randomized controlled trial with traumatized refugee children. Journal of traumatic stress. 2010 Aug;23(4):437–445. doi: 10.1002/jts.20548. [DOI] [PubMed] [Google Scholar]
- 7.Schaal S, Elbert T, Neuner F. Narrative exposure therapy versus interpersonal psychotherapy. A pilot randomized controlled trial with Rwandan genocide orphans. Psychotherapy and psychosomatics. 2009;78(5):298–306. doi: 10.1159/000229768. [DOI] [PubMed] [Google Scholar]
- 8.Ertl V, Pfeiffer A, Schauer E, Elbert T, Neuner F. Community-implemented trauma therapy for former child soldiers in northern uganda: A randomized controlled trial. JAMA : the journal of the American Medical Association. 2011;306(5):503–512. doi: 10.1001/jama.2011.1060. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Youth risk behavior surveillance—United States, 2011. 2012 [Google Scholar]
- 10.Wolitzky-Taylor KB, Ruggiero KJ, Danielson CK, et al. Prevalence and correlates of dating violence in a national sample of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2008 Jul;47(7):755–762. doi: 10.1097/CHI.0b013e318172ef5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Understanding Teen Dating Violence. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2014. [Google Scholar]
- 12.Halpern CT, Spriggs AL, Martin SL, Kupper LL. Patterns of Intimate Partner Violence Victimization from Adolescence to Young Adulthood in a Nationally Representative Sample. J Adolesc Health. 2009;45(5):508–516. doi: 10.1016/j.jadohealth.2009.03.011. 11// [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Volpe EM, Hardie TL, Cerulli C. Associations among depressive symptoms, dating violence, and relationship power in urban, adolescent girls. J Obstet Gynecol Neonatal Nurs. 2012 Jul-Aug;41(4):506–518. doi: 10.1111/j.1552-6909.2012.01384.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams JR, Ghandour RM, Kub JE. Female perpetration of violence in heterosexual intimate relationships: adolescence through adulthood. Trauma, violence & abuse. 2008 Oct;9(4):227–249. doi: 10.1177/1524838008324418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lehrer JA, Buka S, Gortmaker S, Shrier LA. Depressive symptomatology as a predictor of exposure to intimate partner violence among US female adolescents and young adults. Archives of Pediatric Adolescent Medicine. 2006 Mar;160(3):270–276. doi: 10.1001/archpedi.160.3.270. [DOI] [PubMed] [Google Scholar]
- 16.Pervanidou P. Biology of post-traumatic stress disorder in childhood and adolescence. Journal of neuroendocrinology. 2008 May;20(5):632–638. doi: 10.1111/j.1365-2826.2008.01701.x. [DOI] [PubMed] [Google Scholar]
- 17.Giaconia RM, Reinherz HZ, Silverman AB, Pakiz B, Frost AK, Cohen E. Traumas and posttraumatic stress disorder in a community population of older adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34(10):1369–1380. doi: 10.1097/00004583-199510000-00023. [DOI] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5) Fifth Edition ed. American Psychiatric Association; 2013. [Google Scholar]
- 19.Lewandowski RE, Acri MC, Hoagwood KE, et al. Evidence for the management of adolescent depression. Pediatrics. 2013 Oct;132(4):e996–e1009. doi: 10.1542/peds.2013-0600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cisler JM, Begle AM, Amstadter AB, et al. Exposure to interpersonal violence and risk for PTSD, depression, delinquency, and binge drinking among adolescents: data from the NSA-R. Journal of traumatic stress. 2012 Feb;25(1):33–40. doi: 10.1002/jts.21672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perez S, Johnson DM. PTSD compromises battered women's future safety. Journal of Interpersonal Violence. 2008 May 1;23(5):635–651. doi: 10.1177/0886260507313528. 2008. [DOI] [PubMed] [Google Scholar]
- 22.Kuijpers KF, van der Knaap LM, Lodewijks IA. Victims' influence on intimate partner violence revictimization: a systematic review of prospective evidence. Trauma, violence & abuse. 2011 Oct;12(4):198–219. doi: 10.1177/1524838011416378. [DOI] [PubMed] [Google Scholar]
- 23.Nathanson AM, Shorey RC, Tirone V, Rhatigan DL. The Prevalence of Mental Health Disorders in a Community Sample of Female Victims of Intimate Partner Violence. Partner abuse. 2012 Jan;3(1):59–75. doi: 10.1891/1946-6560.3.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roberts TA, Auinger P, Klein JD. Intimate partner abuse and the reproductive health of sexually active female adolescents. J Adolesc Health. 2005 May;36(5):380–385. doi: 10.1016/j.jadohealth.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 25.Silverman JG, Raj A, Mucci LA, Hathaway JE. Dating violence against adolescent girls and associated substance use, unhealthy weight control, sexual risk behavior, pregnancy, and suicidality. Jama-J Am Med Assoc. 2001 Aug 1;286(5):572–579. doi: 10.1001/jama.286.5.572. [DOI] [PubMed] [Google Scholar]
- 26.Chambliss LR. Intimate partner violence and its implication for pregnancy. Clinical Obstetrics & Gynecology. 2008;51(2):385–397. doi: 10.1097/GRF.0b013e31816f29ce. [DOI] [PubMed] [Google Scholar]
- 27.Heaman MI. Relationships Between Physical Abuse During Pregnancy and Risk Factors for Preterm Birth Among Women in Manitoba. J Obstet Gynecol Neonatal Nurs. 2005;34(6):721–731. doi: 10.1177/0884217505281906. [DOI] [PubMed] [Google Scholar]
- 28.Gessner BD, Perham-Hester KA. Experience of violence among teenage mothers in Alaska. J Adolesc Health. 1998 May;22(5):383–388. doi: 10.1016/s1054-139x(97)00257-7. [DOI] [PubMed] [Google Scholar]
- 29.Wiemann CM, Agurcia CA, Berenson AB, Volk RJ, Rickert VI. Pregnant adolescents: experiences and behaviors associated with physical assault by an intimate partner. Matern Child Health J. 2000 Jun;4(2):93–101. doi: 10.1023/a:1009518220331. [DOI] [PubMed] [Google Scholar]
- 30.Covington DL, Justason BJ, Wright LN. Severity, manifestations, and consequences of violence among pregnant adolescents. J Adolesc Health. 28(1):55–61. doi: 10.1016/s1054-139x(00)00154-3. [DOI] [PubMed] [Google Scholar]
- 31.Curry MA, Perrin N, Wall E. Effects of abuse on maternal complications and birth weight in adult and adolescent women. Obstet Gynecol. 1998 Oct;92(4 Pt 1):530–534. doi: 10.1016/s0029-7844(98)00258-0. [DOI] [PubMed] [Google Scholar]
- 32.Covington DL, Justason BJ, Wright LN. Severity, manifestations, and consequences of violence among pregnant adolescents. J Adolesc Health. 2001 Jan;28(1):55–61. doi: 10.1016/s1054-139x(00)00154-3. [DOI] [PubMed] [Google Scholar]
- 33.Ely GE, Nugent WR, Cerel J, Vimbba M. The relationship between suicidal thinking and dating violence in a sample of adolescent abortion patients. Crisis. 2011;32(5):246–253. doi: 10.1027/0227-5910/a000082. [DOI] [PubMed] [Google Scholar]
- 34.Rodriguez MA, Valentine J, Ahmed SR, et al. Intimate partner violence and maternal depression during the perinatal period: A longitudinal investigation of Latinas. Violence against women. 2010 May;16(5):543–559. doi: 10.1177/1077801210366959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moore DR, Florsheim P, Butner J. Interpersonal behavior, psychopathology, and relationship outcomes among adolescent mothers and their partners. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53. 2007 Oct-Dec;36(4):541–556. doi: 10.1080/15374410701662709. [DOI] [PubMed] [Google Scholar]
- 36.Harrykissoon SD, Rickert VI, Wiemann CM. Prevalence and patterns of intimate partner violence among adolescent mothers during the postpartum period. Arch Pediat Adol Med. 2002 Apr;156(4):325–330. doi: 10.1001/archpedi.156.4.325. [DOI] [PubMed] [Google Scholar]
- 37.Kornfeld BD, Bair-Merritt MH, Frosch E, Solomon BS. Postpartum depression and intimate partner violence in urban mothers: Co-occurrence and child healthcare utilization. J Pediatr. 2012 Aug;161(2):348.e342–353.e342. doi: 10.1016/j.jpeds.2012.01.047. [DOI] [PubMed] [Google Scholar]
- 38.Rodriguez MA, Heilemann MV, Fielder E, Ang A, Nevarez F, Mangione CM. Intimate partner violence, depression, and PTSD among pregnant Latina women. Annals of family medicine. 2008 Jan-Feb;6(1):44–52. doi: 10.1370/afm.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gustafsson HC, Cox MJ the Family Life Project Key I. Relations Among Intimate Partner Violence, Maternal Depressive Symptoms, and Maternal Parenting Behaviors. Journal of marriage and the family. 2012 Oct;74(5):1005–1020. doi: 10.1111/j.1741-3737.2012.01010.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lindhorst T, Oxford M. The long-term effects of intimate partner violence on adolescent mothers' depressive symptoms. Soc Sci Med. 2008 Mar;66(6):1322–1333. doi: 10.1016/j.socscimed.2007.11.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leaman SC, Gee CB. Intimate partner violence among adolescent and young adult mothers. [2008/08/01];Journal of family violence. 2008 23(6):519–528. [Google Scholar]
- 42.Becker KD, Stuewig J, McCloskey LA. Traumatic stress symptoms of women exposed to different forms of childhood victimization and intimate partner violence. J Interpers Violence. 2010;25(9):1699–1715. doi: 10.1177/0886260509354578. [DOI] [PubMed] [Google Scholar]
- 43.Bensley L, Van Eenwyk J, Wynkoop Simmons K. Childhood family violence history and women's risk for intimate partner violence and poor health. Am J Prev Med. 2003 Jul;25(1):38–44. doi: 10.1016/s0749-3797(03)00094-1. [DOI] [PubMed] [Google Scholar]
- 44.Bair-Merritt MH, Blackstone M, Feudtner C. Physical health outcomes of childhood exposure to intimate partner violence: a systematic review. Pediatrics. 2006 Feb;117(2):e278–e290. doi: 10.1542/peds.2005-1473. [DOI] [PubMed] [Google Scholar]
- 45.Moretti MM, Obsuth I, Odgers CL, Reebye P. Exposure to maternal vs. paternal partner violence, PTSD, and aggression in adolescent girls and boys. Aggressive Behavior. 2006;32(4):385–395. [Google Scholar]
- 46.Gibson C, Callands TA, Magriples U, Divney A, Kershaw T. Intimate Partner Violence, Power, and Equity Among Adolescent Parents: Relation to Child Outcomes and Parenting. Matern Child Health J. 2014 Apr 30; doi: 10.1007/s10995-014-1509-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Scheering MS, Zeanah CH. A relational perspective on PTSD in early childhood. Journal of traumatic stress. 2001 Oct;14(4):799–815. doi: 10.1023/A:1013002507972. [DOI] [PubMed] [Google Scholar]
- 48.Bogat GA, DeJonghe E, Levendosky AA, Davidson WS, von Eye A. Trauma symptoms among infants exposed to intimate partner violence. Child Abuse Neglect. 2006 Feb;30(2):109–125. doi: 10.1016/j.chiabu.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 49.Burke JG, Lee LC, O'Campo P. An exploration of maternal intimate partner violence experiences and infant general health and temperament. Matern Child Health J. 2008 Mar;12(2):172–179. doi: 10.1007/s10995-007-0218-z. [DOI] [PubMed] [Google Scholar]
- 50.Postmus JL, Huang C-C, Mathisen-Stylianou A. The impact of physical and economic abuse on maternal mental health and parenting. Children and Youth Services Review. 2012;34(9):1922–1928. 9// [Google Scholar]
- 51.Dube SR, Anda RF, Felitti VJ, Edwards VJ, Williamson DF. Exposure to abuse, neglect, and household dysfunction among adults who witnessed intimate partner violence as children: implications for health and social services. Violence and victims. 2002 Feb;17(1):3–17. doi: 10.1891/vivi.17.1.3.33635. [DOI] [PubMed] [Google Scholar]
- 52.Benson ML, Fox GL. When violence hits home: How economics and neighborhood play a role. Washington DC: US Department of Justice; 2004. [Google Scholar]
- 53.DiGangi JA, Gomez D, Mendoza L, Jason LA, Keys CB, Koenen KC. Pretrauma risk factors for posttraumatic stress disorder: a systematic review of the literature. Clin Psychol Rev. 2013 Aug;33(6):728–744. doi: 10.1016/j.cpr.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 54.Kleiber BV, Dimidjian S. Postpartum depression among adolescent mothers: A comprehensive review of prevalence, course, correlates, consequences, and interventions. Clinical Psychology: Science and Practice. 2014;21(1):48–66. [Google Scholar]
- 55.Wiemann CM, Agurcia CA, Berenson AB, Volk RJ, Rickert VI. Pregnant adolescents: Experiences and behaviors associated with physical assault by an intimate partner. Maternal and child health journal. 2000 Jun;4(2):93–101. doi: 10.1023/a:1009518220331. [DOI] [PubMed] [Google Scholar]
- 56.Arriaga XB, Foshee VA. Adolescent dating violence: do adolescents follow in their friends', or their parents', footsteps? J Interpers Violence. 2004 Feb;19(2):162–184. doi: 10.1177/0886260503260247. [DOI] [PubMed] [Google Scholar]
- 57.Rew L. Caring for and Connecting With Homeless Adolescents. Family & Community Health. 2008;31:S42–S51. doi: 10.1097/01.FCH.0000304017.13255.12. [DOI] [PubMed] [Google Scholar]
- 58.Callahan MR, Tolman RM, Saunders DG. Adolescent Dating Violence Victimization and Psychological Well-Being. J Adolescent Res. 2003 Nov 1;18(6):664–681. 2003. [Google Scholar]
- 59.Hamby S, Finkelhor D, Turner H. Teen dating violence: Co-occurrence with other victimizations in the National Survey of Children's Exposure to Violence (NatSCEV) Psychology of Violence. 2012;2(2):111–124. [Google Scholar]
- 60.Exner-Cortens D, Eckenrode J, Rothman E. Longitudinal Associations Between Teen Dating Violence Victimization and Adverse Health Outcomes. Pediatrics. 2012 Dec 10; doi: 10.1542/peds.2012-1029. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Foshee VA, Bauman KE, Greene WF, Koch GG, Linder GF, MacDougall JE. The Safe Dates program: 1-year follow-up results. American journal of public health. 2000 Oct;90(10):1619–1622. doi: 10.2105/ajph.90.10.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.RTI Internationa. Start Strong: Building healthy teen relationships. 2013 [Google Scholar]
- 63.Cohen JA, Mannarino AP, Iyengar S. Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: a randomized controlled trial. Arch Pediat Adol Med. 2011 Jan;165(1):16–21. doi: 10.1001/archpediatrics.2010.247. [DOI] [PubMed] [Google Scholar]
- 64.Smith P, Yule W, Perrin S, Tranah T, Dalgleish T, Clark DM. Cognitive-behavioral therapy for PTSD in children and adolescents: a preliminary randomized controlled trial. J Am Acad Child Psy. 2007 Aug;46(8):1051–1061. doi: 10.1097/CHI.0b013e318067e288. [DOI] [PubMed] [Google Scholar]
- 65.Yozwiak JA. Postpartum Depression and Adolescent Mothers: A Review of Assessment and Treatment Approaches. Journal of Pediatric and Adolescent Gynecology. 2010;23(3):172–178. doi: 10.1016/j.jpag.2009.09.003. 6// [DOI] [PubMed] [Google Scholar]
- 66.Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. The American journal of psychiatry. 1999 Jun;156(6):902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- 67.McTeague LM, Lang PJ, Laplante MC, Cuthbert BN, Shumen JR, Bradley MM. Aversive imagery in posttraumatic stress disorder: trauma recurrence, comorbidity, and physiological reactivity. Biol Psychiat. 2010 Feb 15;67(4):346–356. doi: 10.1016/j.biopsych.2009.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.De Bellis MD, Keshavan MS, Shifflett H, et al. Brain structures in pediatric maltreatment-related posttraumatic stress disorder: a sociodemographically matched study. Biol Psychiat. 2002 Dec 1;52(11):1066–1078. doi: 10.1016/s0006-3223(02)01459-2. [DOI] [PubMed] [Google Scholar]
- 69.Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response. Annual review of physiology. 2005;67:259–284. doi: 10.1146/annurev.physiol.67.040403.120816. [DOI] [PubMed] [Google Scholar]
- 70.Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behaviour research and therapy. 2000 Apr;38(4):319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- 71.Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: A revisit with new data and methods. Science. 2006 Aug 18;313(5789):979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Follette VM, Polusny MA, Bechtle AE, Naugle AE. Cumulative trauma: The impact of child sexual abuse, adult sexual assault, and spouse abuse. Journal of traumatic stress. 1996 Jan;9(1):25–35. doi: 10.1007/BF02116831. [DOI] [PubMed] [Google Scholar]
- 73.Green BL, Goodman LA, Krupnick JL, et al. Outcomes of single versus multiple trauma exposure in a screening sample. Journal of traumatic stress. 2000 Apr;13(2):271–286. doi: 10.1023/A:1007758711939. [DOI] [PubMed] [Google Scholar]
- 74.Kar N, Bastia BK. Post-traumatic stress disorder, depression and generalised anxiety disorder in adolescents after a natural disaster: a study of comorbidity. Clinical practice and epidemiology in mental health : CP & EMH. 2006;2:17. doi: 10.1186/1745-0179-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Briere JN, Elliott DM. Immediate and long-term impacts of child sexual abuse. The Future of children / Center for the Future of Children, the David and Lucile Packard Foundation. 1994 Summer-Fall;4(2):54–69. [PubMed] [Google Scholar]
- 76.Adenauer H, Pinosch S, Catani C, et al. Early processing of threat cues in posttraumatic stress disorder-evidence for a cortical vigilance-avoidance reaction. Biol Psychiat. 2010 Sep 1;68(5):451–458. doi: 10.1016/j.biopsych.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 77.Robjant K, Fazel M. The emerging evidence for Narrative Exposure Therapy: A review. Clinical psychology review. 2010 Dec;30(8):1030–1039. doi: 10.1016/j.cpr.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 78.McPherson J. Does Narrative Exposure Therapy Reduce PTSD in Survivors of Mass Violence? Research on Social Work Practice. 2011 Jul 6; 2012. [Google Scholar]
- 79.Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S. Psychological treatments for chronic post-traumatic stress disorder. Systematic review and metaanalysis. The British journal of psychiatry : the journal of mental science. 2007 Feb;190:97–104. doi: 10.1192/bjp.bp.106.021402. [DOI] [PubMed] [Google Scholar]
- 80.Gillies D, Taylor F, Gray C, O'Brien L, D'Abrew N. Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents. The Cochrane database of systematic reviews. 2012;12:CD006726. doi: 10.1002/14651858.CD006726.pub2. [DOI] [PubMed] [Google Scholar]
- 81.Cienfuegos AJ, Monelli C. The testimony of political repression as a therapeutic instrument. The American journal of orthopsychiatry. 1983 Jan;53(1):43–51. doi: 10.1111/j.1939-0025.1983.tb03348.x. [DOI] [PubMed] [Google Scholar]
- 82.Foa EB, Steketee G, Rothbaum BO. Behavioral/cognitive conceptualizations of posttraumatic stress disorder. Behavior Therapy. 1989 Spring;20(2):155–176. // [Google Scholar]
- 83.Adenauer H, Catani C, Gola H, et al. Narrative exposure therapy for PTSD increases top-down processing of aversive stimuli--evidence from a randomized controlled treatment trial. BMC neuroscience. 2011;12:127. doi: 10.1186/1471-2202-12-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Morina N, Maier T, Bryant R, et al. Combining biofeedback and Narrative Exposure Therapy for persistent pain and PTSD in refugees: a pilot study. European journal of psychotraumatology. 2012;3 doi: 10.3402/ejpt.v3i0.17660. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 85.Hensel-Dittmann D, Schauer M, Ruf M, et al. Treatment of traumatized victims of war and torture: A randomized controlled comparison of narrative exposure therapy and stress inoculation training. Psychotherapy and psychosomatics. 2011;80(6):345–352. doi: 10.1159/000327253. [DOI] [PubMed] [Google Scholar]
- 86.Neuner F, Onyut PL, Ertl V, Odenwald M, Schauer E, Elbert T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomized controlled trial. Journal of consulting and clinical psychology. 2008 Aug;76(4):686–694. doi: 10.1037/0022-006X.76.4.686. [DOI] [PubMed] [Google Scholar]
- 87.Pabst A, Schauer M, Bernhardt K, et al. Treatment of patients with borderline personality disorder and comorbid posttraumatic stress disorder using narrative exposure therapy: a feasibility study. Psychotherapy and psychosomatics. 2012;81(1):61–63. doi: 10.1159/000329548. [DOI] [PubMed] [Google Scholar]
- 88.Zang Y, Hunt N, Cox T. A randomised controlled pilot study: The effectiveness of narrative exposure therapy with adult survivors of the Sichuan earthquake. BMC psychiatry. 2013;13:41. doi: 10.1186/1471-244X-13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Halvorsen JO, Stenmark H. Narrative exposure therapy for posttraumatic stress disorder in tortured refugees: A preliminary uncontrolled trial. Scandinavian journal of psychology. 2010 Dec;51(6):495–502. doi: 10.1111/j.1467-9450.2010.00821.x. [DOI] [PubMed] [Google Scholar]
- 90.Hijazi AM, Lumley MA, Ziadni MS, Haddad L, Rapport LJ, Arnetz BB. Brief narrative exposure therapy for posttraumatic stress in Iraqi refugees: a preliminary randomized clinical trial. Journal of traumatic stress. 2014 Jun;27(3):314–322. doi: 10.1002/jts.21922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bichescu D, Neuner F, Schauer M, Elbert T. Narrative exposure therapy for political imprisonment-related chronic posttraumatic stress disorder and depression. Behaviour research and therapy. 2007;45(9):2212–2220. doi: 10.1016/j.brat.2006.12.006. 9// [DOI] [PubMed] [Google Scholar]
- 92.Neuner F, Catani C, Ruf M, Schauer E, Schauer M, Elbert T. Narrative exposure therapy for the treatment of traumatized children and adolescents (KidNET): from neurocognitive theory to field intervention. Child and adolescent psychiatric clinics of North America. 2008 Jul;17(3):641–664. x. doi: 10.1016/j.chc.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 93.Neuner F, Schauer M, Elbert T. On the efficacy of Narrative Exposure Therapy: A reply to Mundt et al. Intervention. 2014;12(2):267–297. [Google Scholar]
- 94.Schoenwald SK, Garland AF. A review of treatment adherence measurement methods. Psychol Assess. 2013 Mar;25(1):146–156. doi: 10.1037/a0029715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Taddeo D, Egedy M, Frappier JY. Adherence to treatment in adolescents. Paediatrics & child health. 2008 Jan;13(1):19–24. doi: 10.1093/pch/13.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gwozdziewycz N, Mehl-Madrona L. Meta-analysis of the use of narrative exposure therapy for the effects of trauma among refugee populations. The Permanente journal. 2013 Winter;17(1):70–76. doi: 10.7812/TPP/12-058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mundt A, Wunsche P, Heinz A, Pross C. Trauma therapy in crisis and disaster areas- -a critical review of standardized interventions such as narrative exposure therapy. Psychiatrische Praxis. 2011 Aug;38(6):300–305. doi: 10.1055/s-0030-1266096. [DOI] [PubMed] [Google Scholar]
- 98.Rothbaum BO, Davis M. Applying learning principles to the treatment of post-trauma reactions. Annals of the New York Academy of Sciences. 2003 Dec;1008:112–121. doi: 10.1196/annals.1301.012. [DOI] [PubMed] [Google Scholar]
- 99.National Institutes for Health and Clinical Excellence(NICE) Post-traumatic stress disorder (PTSD): The treament of PTSD in adults and children. London: 2005. [Google Scholar]
- 100.Sormanti M, Pereira L, El-Bassel N, Witte S, Gilbert L. The role of community consultants in designing an HIV prevention intervention. AIDS education and prevention : official publication of the International Society for AIDS Education. 2001 Aug;13(4):311–328. doi: 10.1521/aeap.13.4.311.21431. [DOI] [PubMed] [Google Scholar]
- 101.Israel BA, Schulz AJ, Parker EA, Becker AB Community-Campus Partnerships for H. Community-based participatory research: policy recommendations for promoting a partnership approach in health research. Education for health. 2001;14(2):182–197. doi: 10.1080/13576280110051055. [DOI] [PubMed] [Google Scholar]