Abstract
Since their discovery in 2004, neutrophil extracellular traps (NETs) have been characterized as a fundamental host innate immune defense against various pathogens. Released in response to infectious and pro-inflammatory stimuli, NETs can immobilize invading pathogens within a fibrous matrix consisting of DNA, histones, and antimicrobial peptides. Conversely, excessive or dysregulated NET release may hold a variety of detrimental consequences for the host. A fine balance between NET formation and elimination is necessary to sustain a protective effect during infectious challenge. In recent years, a number of microbial virulence factors have been shown to modulate formation of NETs, thereby facilitating colonization or spread within the host. In this mini-review we summarize the contemporary research on the interaction of bacterial exotoxins with neutrophils that modulate NET production, focusing particular attention on consequences for the host. Understanding host–pathogen dynamics in this extracellular battlefield of innate immunity may provide novel therapeutic approaches for infectious and inflammatory disorders.
Keywords: phagocyte extracellular traps, neutrophils, macrophages, leukocidin, cell death
Neutrophil Extracellular Traps
The formation of neutrophil extracellular DNA traps (so called NETs) was first recognized as a host innate immune defense mechanism against infections by Brinkmann et al. (2004). This discovery altered the fundamental conception of the innate immune function of phagocytes against pathogenic microbes in a most fascinating way. Whereas it was previously believed that neutrophils kill invading pathogens by intracellular uptake (phagocytosis) and subsequent killing, the discovery of NETs revealed an additional phagocytosis-independent mechanism. The released nuclear material including histones and DNA within the extracellular trap (ET) immobilize and occasionally kill several medically important bacteria, viruses, or parasites (Brinkmann et al., 2004).
Regarding the cellular pathways that lead to NET formation, most studies show that the cell in question undergoes NETosis, a process of death that differs morphologically from necrosis and apoptosis (Fuchs et al., 2007). In contrast to apoptotic or necrotic cells, cells that undergo NETosis show a prelytic decondensation of the chromatin associated with the disruption of the nuclear membrane. This disintegration of the nuclear membrane allows mixing of DNA and histones with granule components, which are then extracellularly released as web-like fibers with a diameter of approximately 15 to 17 nm, associated with globular proteins or antimicrobial peptides. NET-based antimicrobial activity remains active when cells are treated with the actin microfilament inhibitor cytochalasin D, indicating that this phenomenon is independent of phagocytosis. However, the antimicrobial activity of NETs can be abolished when NETs are treated with DNase, confirming that DNA comprises the functional backbone of the released fibers (Brinkmann et al., 2004; Fuchs et al., 2007).
The formation of NETs was initially thought to be an antimicrobial defense strategy and cell death pathway specific for neutrophils (Brinkmann et al., 2004). However, von Köckritz-Blickwede et al. (2008) mast cells were shown to also deploy mast cell extracellular traps (MCETs) in defense against bacterial pathogens. During recent years, further evidence has accumulated demonstrating ET formation occurs in eosinophils (Yousefi et al., 2008), basophils (Schorn et al., 2012), fibrocytes (Kisseleva et al., 2011), macrophages (Bartneck et al., 2010; Chow et al., 2010), and monocytes (Bartneck et al., 2010; Chow et al., 2010).
It is important to mention that some authors have demonstrated experimentally that eosinophils and neutrophils can release antimicrobial ETs in response to infection while remaining in a viable status (Yousefi et al., 2008, 2009). NET release by viable cells was confirmed in vivo in a murine model of Staphylococcus aureus skin infection (Yipp et al., 2012). Here, NET formation was seen as a dynamic process, which occurs by vesicular release of nuclear material during migration of neutrophils through the tissue. It is still unclear, however, how such budding and final release of nuclear material is initiated. Thus, based on current knowledge it seems that at least two different mechanisms can lead to NET formation: a viable form involving vesicular release and the more well-understood NETosis form associated with rupture of the nuclear membrane. Research has begun to explore how certain drugs, including statins (Chow et al., 2010) and tamoxifen (Corriden et al., 2015), modulate neutrophil functions to accentuate NET formation, which could be beneficial as an adjunctive therapy for extracellular pathogens such as S. aureus that efficiently avoid phagocytic killing by neutrophils.
In contrast to their protective effect against several infections, there is increasing evidence that a dysregulated NET release can provoke autoimmune reactions, tissue damage and impaired cellular functions (Villanueva et al., 2011; Saffarzadeh et al., 2012). Unchecked, aberrant NET formation can result in pathological damage as vascular thrombosis (Fuchs et al., 2010) or chronic lung inflammation in cystic fibrosis (Papayannopoulos et al., 2011). Countermeasures to the excessive NET formation may be of therapeutic utility in such cases as for example DNAse treatment in patients with cystic fibrosis (Fuchs et al., 1994) or the usage of anti-histone antibodies to alleviate vascular thrombosis (Semeraro et al., 2011). Since sustained blockade of NET formation may carry a risk of increased susceptibility to certain infections, anti-NET therapy might be targeted to severe autoimmune or inflammatory diseases, when pro-inflammatory activities of NETs outweigh their protective benefits (Saffarzadeh and Preissner, 2013).
The Role of NETs Against Infection
In several studies, NETs were found to play a protective role against various infecting organisms, often employing mutagenesis of key evasion factors of the respective organisms. It is thought that NETs can act in two ways: (1) pathogen immobilization and (2) growth inhibition or killing of the microbe. The relative importance of killing is a point of some contention in the literature (Menegazzi et al., 2012). However, based on vital immunofluorescent staining of bacteria with DNA intercalating dyes, microbial killing by NETs has been demonstrated definitively by several authors (Lauth et al., 2009; Berends et al., 2010; Halverson et al., 2015). However, since the overall killing potential of NETs is physically restricted, the cumulative effect of NETs may be functionally bacteriostatic (Baums and von Köckritz-Blickwede, 2015).
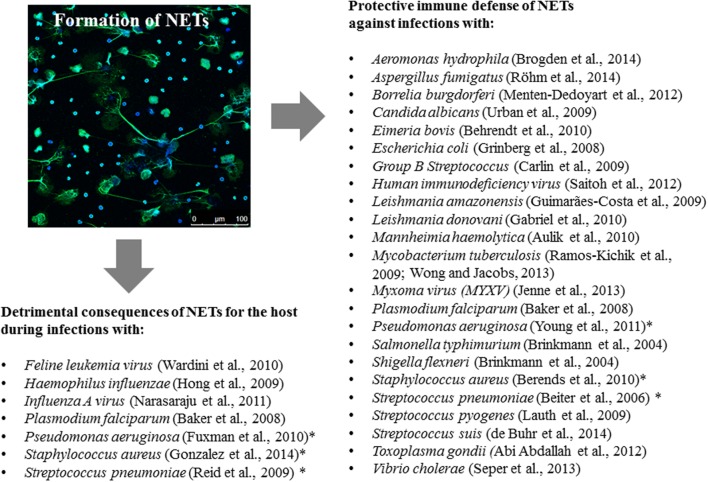
Because some bacteria have evolved highly efficient resistance strategies against antimicrobial activity of NETs, in some specific circumstances, NETs can help to establish an infectious niche. For example, in the case of a primary influenza A infection of the middle ear which boosts formation of NETs by infiltrating neutrophils, resistant Streptococcus pneumoniae can use those NETs to multiply and persist in the middle ear cavity (Short et al., 2014). Additionally, some studies show that S. pneumoniae and Haemophilus influenzae can incorporate NETs into biofilms that promote their persistence in the host (Hong et al., 2009; Reid et al., 2009). In the end, it depends on the pathogen, its array of immune resistance factors and the anatomical site of infection, as to whether NETs can serve a protective function for the host during an infection (Figure 1).
FIGURE 1.
Extracellular trap formation during infections: consequences for the host. The figure summarizes the protective versus detrimental role of NETs for the host during an infection with respective pathogens. In some cases (highlighted with an asterisk), there is benefit and harm depending on site, timing and magnitude of infection. The immunofluorescence micrograph is showing the release of NETs from human blood-derived neutrophils. NETs were stained with antibodies against histone-DNA complexes (green) and DAPI to stain the nuclei and nuclear DNA (blue).
Categories of Bacterial NET Evasion Factors
Neutrophil extracellular trap evasion factors can be classified in three different phenotypes: (1) NET degradation, (2) resistance to the intrinsic antimicrobial effectors within NETs, or (3) the suppression of NET production (von Köckritz-Blickwede and Nizet, 2009). The best-studied NET evasion factor is the activity of microbial nucleases that degrade NETs deployed by innate immune cells to escape entrapment. Membrane-bound or released nucleases have been shown to be expressed by the following microbes as NET evasion factors: Aeromonas hydrophila (Brogden et al., 2012), Escherichia coli (Möllerherm et al., 2015), Leptospira sp. (Scharrig et al., 2015), Neisseria gonorhoeae (Juneau et al., 2015), S. aureus (Berends et al., 2010), S. agalactiae (Derré-Bobillot et al., 2013), S. pneumoniae (Beiter et al., 2006), S. pyogenes (Buchanan et al., 2006; Chang et al., 2011), Streptococcus synguinis (Morita et al., 2014), S. suis (de Buhr et al., 2014), Vibrio cholera (Seper et al., 2013), and Yersinia enterocolitica (Möllerherm et al., 2015). Whereas, resistance to antimicrobial effectors in ETs is mainly mediated by surface-bound virulence factors, e.g., exopolysaccharide capsules in case of S. pyogenes (Cole et al., 2010) or S. pneumonia (Wartha et al., 2007), the suppression of NET formation is mainly carried out by released factors including proteases (Zinkernagel et al., 2008).
Bacterial Exotoxins that Modulate NET Formation
During the last 10 years, there is increasing evidence in the literature that different exotoxins released by Gram-positive or Gram-negative bacteria are able to modulate the process of NET formation (Table 1): to date, at least 11 different exotoxins have been published to modulate NET formation, with nine of them reported to enhance NET formation while two suppress the process (Table 1). First we will set our attention on those toxins that induce NET formation.
Table 1.
Effect of bacterial exotoxins on formation of extracellular traps.
| Microbe | Exoprotein | Effect on cells | Mechanism | Cell death | Putative consequences for the host | Reference |
|---|---|---|---|---|---|---|
| Bordetella pertussis | Adenylate cyclase toxin (ACT) | Suppression of NET formation and apoptosis | Generation of cAMP and inhibition of oxidative burst | Impairment of cell lysis | ACT promotes neutrophil infiltration by inhibiting neutrophil death | Eby et al., 2014 |
| Escherichia coli | Hemolysin | Induction of ETs in murine and human macrophages | Not known | Not known | Not known | Aulik et al., 2012 |
| Mannheimia haemolytica | Leukotoxin | Induction of ETs in bovine neutrophils, as well as bovine, murine, and human macrophages | CD18- and NADPH-oxidase dependent | Delayed LDH release, no necrosis, no aptoptosis | Trapping and killing of M. haemolytica | Aulik et al., 2010, 2012 |
| Mycobacterium tuberculosis | Early secretory antigen-6 protein | Induction of secondary necrosis and ET formation of phosphatidylserine externalized neutrophils | Intracellular Ca2+ overload | Cell lysis | Necrotic granulomas during tuberculosis | Francis et al., 2014 |
| Pseudomonas aeruginosa | Pyocyanin | Induction of NETs | NADPH- oxidase- and Jun N-terminal kinase-dependent | Cell lysis | Inflammatory condition during cystic fibrosis | Rada et al., 2013 |
| Staphylococcus aureus | N-terminal ArgD peptides | Induction of NETs | Unknown | Cell lysis | Aggravation of skin lesions | Gonzalez et al., 2014 |
| Staphylococcus aureus | Leukotoxin GH | Induction of NETs | Non-specific cytolysis | Non-specific cytolysis | Entrapment of S. aureus | Malachowa et al., 2013 |
| Staphylococcus aureus | Panton-Valentin-leukocidin | Induction of rapid nuclear NET formation | Vesicular release of nuclear DNA, independent of NADPH- oxidase | No cell lysis | Entrapment of S. aureus | Pilsczek et al., 2010 |
| Staphylococcus epidermidis | Phenol-soluble-modulin γ (δ-toxin) | Induces NET formation and colocalizes with NETs and host antimicrobial peptides | Physically binding to host derived antimicrobial peptides and DNA | Cell lysis | Cooperates with host antimicrobial peptides against bacterial pathogens | Cogen et al., 2010 |
| Streptocococus pyogenes | M1 protein | Induces formation of NETs and MCETs | Unknown | Cell lysis | Trapping and killing of S. pyogenes | Lauth et al., 2009; Oehmcke et al., 2009 |
| Streptocococus pyogenes | Streptolysin O | Suppression of NET formation | Impairment of oxidative burst | Sublytic con-centrations | Severe infection | Uchiyama et al., 2015 |
The M1-protein of the Gram-positive bacterium S. pyogenes, also known as group A Streptococcus (GAS), was the first exotoxin described to induce formation of ETs by neutrophils and mast cells (Lauth et al., 2009). The surface-anchored M1 protein is a classical virulence factor that promotes resistance to phagocytosis. However, after proteolytic release from the S. pyogenes surface, the M1 protein forms a proinflammatory supramolecular network with fibrinogen that contributes to the pathophysiology of streptococcal toxic shock-like syndrome (Herwald et al., 2004). Two parallel studies showed in 2009, that the M1 protein is able to mediate formation of NETs as well as MCETs, and thereby contribute to entrapment and killing of the bacteria (Lauth et al., 2009; Oehmcke et al., 2009). Besides induction of ETs, M1 protein promotes resistance to the human cathelicidin antimicrobial peptide LL-37, an important effector of bacterial killing by neutrophils and mast cells (Lauth et al., 2009; LaRock et al., 2015).
Staphylococcus epidermidis is a common colonizer of healthy human skin and is hypothesized to play a mutually beneficial role in the cutaneous niche. Cogen et al. (2010) demonstrated that S. epidermidis phenol-soluble-modulin γ (δ-toxin) boosts NET production and further colocalizes with endogenous host antimicrobial peptides within the architecture of the expressed NETs. In antimicrobial assays against the pathogen S. pyogenes, δ-toxin cooperated with host-derived antimicrobial peptides cathelicidins (human LL-37 and murine CRAMP) and human beta-defensins (hBD2 and hBD3) to kill the pathogenic streptococci. Coimmunoprecipitation and tryptophan spectroscopy demonstrated direct binding of δ-toxin to LL-37, CRAMP, hBD2, and hBD3, as well as DNA. These data suggest that commensal S. epidermidis-derived δ-toxin cooperates with the host-derived antimicrobial peptides in the innate immune system to reduce survival of an important human bacterial pathogen. This could be corroborated in a mouse wound model where S. pyogenes survival was reduced when the wounds were pretreated with δ-toxin. These data described a novel therapeutic application of a bacterial toxin against pathogenic bacteria to enhance formation of NETs and support the host innate immune system.
Mannheimia haemolytica leukotoxin (LKT) induces formation of extracellular traps in bovine neutrophils and macrophages (Aulik et al., 2010, 2012). LKT is a member of the repeats-in-toxin (RTX) family of exoproteins produced by a wider variety of Gram-negative bacteria. In addition to the native fully active LKT, its non-cytolytic pro-LKT precursor also stimulated macrophage extracellular traps (METs) formation. Formation of METs in response to LKT required NADPH oxidase activity, as previously demonstrated for NETosis. METs induced in response to LKT trapped and killed a portion of the toxin-producing M. haemolytica cells. In contrast to NETosis, which is reported to occur between 10 min to 4 h after pathogen exposure, LKT-induced MET formation was extremely rapid, with significant accumulation of extracellular DNA within 2 min after macrophage stimulation.
Interestingly, the LKT-mediated cytotoxic effects are specific to ruminants, since LKT binds to amino acids 5–17 of the signal sequence of CD18, which is not present on mature leukocytes from humans and other mammalian species (Shanthalingam and Srikumaran, 2009). CD18 was confirmed by Aulik et al. (2010) to play a role in LKT-dependent NET formation in bovine phagocytes. Similarly, to the LKT, the related RTX family toxin, uropathgenic E. coli (UPEC) hemolysin, induced NET formation in the mouse and human monocyte/macrophage cell lines indicating that NET induction may be a general phenomenon in response to active RTX toxins (Aulik et al., 2012). At this point it remains difficult to assess whether NET production in response to RTX toxins leads to a protective host defense against M. haemolytica or other Gram-negative bacteria. In the case of LKT, bacterial cells entrapped in NETs can continue to secrete LKT, an important virulence determinant, which could exacerbate lung inflammation (Aulik et al., 2010, 2012).
The Pseudomonas aeruginosa virulence factor pyocyanin stimulates the release of NETs in a NADPH oxidase-dependent manner (Rada et al., 2013). Pyocyanin is a redox-active pigment associated with diminished lung function in cystic fibrosis. In cystic fibrosis airways, P. aeruginosa resides in biofilms protected from neutrophil phagocytic activity or from entrapment by NETs (Rada et al., 2013). The authors speculate that enhanced ROS-dependent NET formation by P. aeruginosa pyocyanin contributes to inflammatory conditions observed in chronically infected cystic fibrosis airways. Parenthetically, chronic granulomatous disease (CGD) patients, whose neutrophils are unable to make NETs, are not recognized to be disproportionately susceptible to infections with Pseudomonas species (Rada and Leto, 2008).
A specific activity of an exotoxin was shown for the Mycobacterium tuberculosis leukocidin ESAT-6, which induced NET formation only in a subpopulation of neutrophils with externalized phosphatidylserine as a marker for apoptosis (Francis et al., 2014). Thus, ESAT-6 induced NET formation was similar to secondary necrosis of pre-activated neutrophils and dependent on Ca2+. In this case, increased NET formation was also speculated to contribute to virulence of tuberculosis, since it was recently observed that the development of necrotic granulomas in a mouse model of progressive tuberculosis were associated with the presence of extracellular bacteria, neutrophil necrosis and NET-like structures (Francis et al., 2014).
In the case of the leading human pathogen S. aureus, three different exotoxins enhance the release of NETs: N-terminal AgrD peptides (Gonzalez et al., 2014), leukotoxin GH (Malachowa et al., 2013), also known as LukAB (Dumont et al., 2011), thus named here LukGH/AB, and Panton-Valentin leukocidin (PVL; Pilsczek et al., 2010). AgrD is the precursor for the auto-inducing peptide in a well-known quorum sensing system regulating virulence phenotypes of S. aureus. A recent mass spectrometry-based study identified formylated and non-formylated peptide variants derived from AgrD N-terminal leader domain in S. aureus cell-free culture supernatant to act cytotoxic, modulate neutrophil chemotaxis and induce formation of NETs. As a consequence a detrimental effect for the host was hypothesized as indicated by aggravation of skin lesions in vivo in a murine model. The cellular pathways mediating this process of AgrD induced NET formation remain unclear (Gonzalez et al., 2014).
Staphylococcus aureus LukGH/AB, also promotes formation of NETs in association with death of the neutrophil (Malachowa et al., 2013). LukGH/AB is a pore-forming cytolytic toxin with proinflammatory properties, similar to those established for PVL. But unlike PVL, LukGH/AB did not prime human neutrophils for increased production of reactive oxygen species nor did it enhance binding and/or uptake of S. aureus. LukGH/AB promoted the release of NETs, which in turn ensnared but did not achieve killing of S. aureus. These authors found that electropermeabilization of human neutrophils, used to create pores in the neutrophil plasma membrane, induced NET formation in a similar way. This finding indicated that NETs can be generated during non-specific cytolysis.
The above phenomemon stands in contrast to NET formation initiated by PVL production in S. aureus. Pilsczek et al. (2010) demonstrated a novel rapid (5–60 min) process of NET formation that did not require cell lysis or even breach of the plasma membrane. The authors show that neutrophils treated with S. aureus supernatant show rounded and condensed nuclei, followed by the separation of the inner and outer nuclear membrane and budding of vesicles filled with nuclear DNA. The vesicles are extruded intact into extracellular space where they rupture, release the chromatin and form NETs. PVL was identified as one key effector of NET formation present in the S. aureus supernatant, but other yet unidentified molecules aside from PVL cannot be excluded as contributors to NET production. This rapid process of NET formation against S. aureus was dubbed “dynamic NETosis” and was recently proven to serve as an efficient host defense strategy during S. aureus skin infections in man and mice (Yipp et al., 2012). Since, PVL targets a different receptor on the neutrophil compared to the LukGH/AB, namely the C5aR receptor (Spaan et al., 2013) and the CD11b receptor (Dumont et al., 2013), respectively, it still remains to be determined if the receptor-mediated signaling leads to the different NET phenotypes.
Two toxins have been described so far to suppress NET formation, perhaps representing an immune evasion strategy by the respective pathogens: Bordetella pertussis adenylate cyclase toxin (Eby et al., 2014) and S. pyogenes streptolysin O (SLO; Uchiyama et al., 2015). Both mechanisms are coupled to suppression of neutrophil oxidative burst. In case of S. pyogenes SLO, this mechanism plays a key role of SLO in the pathogen’s resistance to immediate neutrophil killing. In case of B. pertussis, the relevance of NET inhibition by the toxin is still unclear, since it is not known whether or not NETs are able to entrap and clear B. pertussis. This study highlighted how convalescent phase serum from humans following clinical pertussis blocked the ACT-mediated suppression of NET formation (Eby et al., 2014). Based on this finding, the authors mention that their data should alert investigators to the ability for ACT, and antibodies to ACT, to dysregulate neutrophil death mechanisms and potentially influence local tissue damage during infection with B. pertussis.
Concluding Comments
With increasing publications in the NET field it is well-known that NETs are on one hand protective against several infections, but may also result in detrimental effects when released in excessive amount. The complexity may be compared with the release of cytokines during infection and inflammation, which serve an essential role in an efficient immune response of the host against infections, but in which overwhelming cytokine storm can lead to septic shock and accelerate death of the host. The cumulative balance between NET formation and NET degradation – similar to cytokine release – defines the protective versus detrimental effects on the organism. Currently, it is under discussion in the literature if and how NETs can act as a novel therapeutic or prophylactic target for boosting immunity to bacterial infections or mitigating inflammatory diseases associated with detrimental NET formation. To rationally and effectively pharmacologically interfere with the process of NET formation, the cellular processes mediating this phenomenon need to be understood more in detail. Identification of bacterial factors, especially exotoxins, with specific roles in NET modulation, may serve as probes to understand the molecular basis of NET generation and antimicrobial activity. Furthermore, exotoxins might themselves harbor therapeutic potential when their effects against the host cells are fully characterized.
Author Contributions
SB collected the literature, MK-B and VN wrote the manuscript. All authors have proofread the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
SB was funded by a fellowship of the Ministry of Science and Culture of Lower Saxony (Georg-Christoph-Lichtenberg Scholarship) within the framework of the Ph.D. program ‘EWI-Zoonoses’ of the Hannover Graduate School for Veterinary Pathobiology, Neuroinfectiology, and Translational Medicine (HGNI).
References
- Abi Abdallah D. S., Lin C., Ball C. J., King M. R., Duhamel G. E., Denkers E. Y. (2012). Toxoplasma gondii triggers release of human and mouse neutrophil extracellular traps. Infect. Immun. 80 768–777. 10.1128/IAI.05730-5711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aulik N. A., Hellenbrand K. M., Czuprynski C. J. (2012). Mannheimia haemolytica and its leukotoxin cause macrophage extracellular trap formation by bovine macrophages. Infect. Immun. 80 1923–1933. 10.1128/IAI.06120-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aulik N. A., Hellenbrand K. M., Klos H., Czuprynski C. J. (2010). Mannheimia haemolytica and its leukotoxin cause neutrophil extracellular trap formation by bovine neutrophils. Infect. Immun. 78 4454–4466. 10.1128/IAI.00840-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker V. S., Imade G. E., Molta N. B., Tawde P., Pam S. D., Obadofin M. O., et al. (2008). Cytokine-associated neutrophil extracellular traps and antinuclear antibodies in Plasmodium falciparum infected children under six years of age. Malar. J. 7:41 10.1186/1475-2875-7-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartneck M., Keul H. A., Zwadlo-Klarwasser G., Groll J. (2010). Phagocytosis independent extracellular nanoparticle clearance by human immune cells. Nano Lett. 10 59–63. 10.1021/nl902830x [DOI] [PubMed] [Google Scholar]
- Baums C. G., von Köckritz-Blickwede M. (2015). Novel role of DNA in neutrophil extracellular traps. Trends Microbiol. 23 330–331. 10.1016/j.tim.2015.04.003 [DOI] [PubMed] [Google Scholar]
- Behrendt J. H., Ruiz A., Zahner H., Taubert A., Hermosilla C. (2010). Neutrophil extracellular trap formation as innate immune reactions against the apicomplexan parasite Eimeria bovis. Vet. Immunol. Immunopathol. 133 1–8. 10.1016/j.vetimm.2009.06.012 [DOI] [PubMed] [Google Scholar]
- Beiter K., Wartha F., Albiger B., Normark S., Zychlinsky A., Henriques-Normark B. (2006). An endonuclease allows Streptococcus pneumoniae to escape from neutrophil extracellular traps. Curr. Biol. 16 401–407. 10.1016/j.cub.2006.01.056 [DOI] [PubMed] [Google Scholar]
- Berends E. T., Horswill A. R., Haste N. M., Monestier M., Nizet V., von Köckritz-Blickwede M. (2010). Nuclease expression by Staphylococcus aureus facilitates escape from neutrophil extracellular traps. J. Innate Immun. 2 576–586. 10.1159/000319909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinkmann V., Reichard U., Goosmann C., Fauler B., Uhlemann Y., Weiss D. S., et al. (2004). Neutrophil extracellular traps kill bacteria. Science 303 1532–1535. 10.1126/science.1092385 [DOI] [PubMed] [Google Scholar]
- Brogden G., Krimmling T., Adamek M., Naim H. Y., Steinhagen D., von Köckritz-Blickwede M. (2014). The effect of β-glucan on formation and functionality of neutrophil extracellular traps in carp (Cyprinus carpio L.). Dev. Comp. Immunol. 44 280–285. 10.1016/j.dci.2014.01.003 [DOI] [PubMed] [Google Scholar]
- Brogden G., von Köckritz-Blickwede M., Adamek M., Reuner F., Jung-Schroers V., Naim H. Y., et al. (2012). β-Glucan protects neutrophil extracellular traps against degradation by Aeromonas hydrophila in carp (Cyprinus carpio). Fish Shellfish Immunol. 33 1060–1064. 10.1016/j.fsi.2012.08.009 [DOI] [PubMed] [Google Scholar]
- Buchanan J. T., Simpson A. J., Aziz R. K., Liu G. Y., Kristian S. A., Kotb M., et al. (2006). DNase expression allows the pathogen group a Streptococcus to escape killing in neutrophil extracellular traps. Curr. Biol. 16 396–400. 10.1016/j.cub.2005.12.039 [DOI] [PubMed] [Google Scholar]
- Carlin A. F., Uchiyama S., Chang Y. C., Lewis A. L., Nizet V., Varki A. (2009). Molecular mimicry of host sialylated glycans allows a bacterial pathogen to engage neutrophil Siglec-9 and dampen the innate immune response. Blood 113 3333–3336. 10.1182/blood-2008-11-187302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang A., Khemlani A., Kang H., Proft T. (2011). Functional analysis of Streptococcus pyogenes nuclease A (SpnA), a novel group A streptococcal virulence factor. Mol. Microbiol. 79 1629–1642. 10.1111/j.1365-2958.2011.07550.x [DOI] [PubMed] [Google Scholar]
- Chow O. A., Köckritz-Blickwede M., von Bright A. T., Hensler M. E., Zinkernagel A. S., Cogen A. L., et al. (2010). Statins enhance formation of phagocyte extracellular traps. Cell Host Microbe 8 445–454. 10.1016/j.chom.2010.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cogen A. L., Yamasaki K., Muto J., Sanchez K. M., Crotty Alexander L., Tanios J., et al. (2010). Staphylococcus epidermidis antimicrobial delta-toxin (phenol-soluble modulin-gamma) cooperates with host antimicrobial peptides to kill group a Streptococcus. PLoS ONE 5:e8557 10.1371/journal.pone.0008557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole J. N., Pence M. A., von Köckritz-Blickwede M., Hollands A., Gallo R. L., Walker M. J., et al. (2010). M protein and hyaluronic acid capsule are essential for in vivo selection of covRS mutations characteristic of invasive serotype M1T1 group A Streptococcus. MBio 1:e191 10.1128/mBio.00191-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corriden R., Hollands A., Olson J., Derieux J., Lopez J., Chang J. T., et al. (2015). Tamoxifen augments the innate immune function of neutrophils through modulation of intracellular ceramide. Nat. Commun. 13:8369 10.1038/ncomms9369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Buhr N., Neumann A., Jerjomiceva N., Köckritz-Blickwede M., Baums C. G. (2014). Streptococcus suis DNase SsnA contributes to degradation of neutrophil extracellular traps (NETs) and evasion of NET-mediated antimicrobial activity. Microbiology 160 385–395. 10.1099/mic.0.072199-0 [DOI] [PubMed] [Google Scholar]
- Derré-Bobillot A., Cortes-Perez N. G., Yamamoto Y., Kharrat P., Couvé E., Da Cunha V., et al. (2013). Nuclease A (Gbs0661), an extracellular nuclease of Streptococcus agalactiae, attacks the neutrophil extracellular traps and is needed for full virulence. Mol. Microbiol. 89 518–531. 10.1111/mmi.12295 [DOI] [PubMed] [Google Scholar]
- Dumont A. L., Nygaard T. K., Watkins R. L., Smith A., Kozhaya L., Kreiswirth B., et al. (2011). Characterization of a new cytotoxin that contributes to Staphylococcus aureus pathogenesis. Mol. Microbiol. 79 814–825. 10.1111/j.1365-2958.2010.07490.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumont A. L., Yoong P., Day C. J., Alonzo F., III, McDonald W. H., Jennings M. P., et al. (2013). Staphylococcus aureus LukAB cytotoxin kills human neutrophils by targeting the CD11b subunit of the integrin Mac-1. Proc. Natl. Acad. Sci. U.S.A. 110 10794–10799. 10.1073/pnas.1305121110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eby J. C., Gray M. C., Hewlett E. L. (2014). Cyclic AMP-mediated suppression of neutrophil extracellular trap formation and apoptosis by the Bordetella pertussis adenylate cyclase toxin. Infect. Immun. 82 5256–5269. 10.1128/IAI.02487-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis R. J., Butler R. E., Stewart G. R. (2014). Mycobacterium tuberculosis ESAT-6 is a leukocidin causing Ca2+ influx, necrosis and neutrophil extracellular trap formation. Cell Death Dis. 5:e1474 10.1038/cddis.2014.394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs H. J., Borowitz D. S., Christiansen D. H., Morris E. M., Nash M. L., Ramsey B. W., et al. (1994). Effect of aerosolized recombinant human DNase on exacerbations of respiratory symptoms and on pulmonary function in patients with cystic fibrosis. The pulmozyme study group. N. Engl. J. Med. 331 637–642. 10.1056/NEJM199409083311003 [DOI] [PubMed] [Google Scholar]
- Fuchs T. A., Abed U., Goosmann C., Hurwitz R., Schulze I., Wahn V., et al. (2007). Novel cell death program leads to neutrophil extracellular traps. J. Cell Biol. 176 231–241. 10.1083/jcb.200606027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs T. A., Brill A., Duerschmied D., Schatzberg D., Monestier M., Myers D. D., Jr., et al. (2010). Extracellular DNA traps promote thrombosis. Proc. Natl. Acad. Sci. U.S.A. 107 15880–15885. 10.1073/pnas.1005743107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuxman Bass J. I., Russo D. M., Gabelloni M. L., Geffner J. R., Giordano M., Catalano M., et al. (2010). Extracellular DNA: a major proinflammatory component of Pseudomonas aeruginosa biofilms. J. Immunol. 184 6386–6395. 10.4049/jimmunol.0901640 [DOI] [PubMed] [Google Scholar]
- Gabriel C., McMaster W. R., Girard D., Descoteaux A. (2010). Leishmania donovani promastigotes evade the antimicrobial activity of neutrophil extracellular traps. J. Immunol. 185 4319–4327. 10.4049/jimmunol.1000893 [DOI] [PubMed] [Google Scholar]
- Gonzalez D. J., Corriden R., Akong-Moore K., Olson J., Dorrestein P. C., Nizet V. (2014). N-terminal ArgD peptides from the classical Staphylococcus aureus Agr system have cytotoxic and proinflammatory activities. Chem. Biol. 21 1457–1462. 10.1016/j.chembiol.2014.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinberg N., Elazar S., Rosenshine I., Shpigel N. Y. (2008). Beta-hydroxybutyrate abrogates formation of bovine neutrophil extracellular traps and bactericidal activity against mammary pathogenic Escherichia coli. Infect. Immun. 76 2802–2807. 10.1128/IAI.00051-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guimarães-Costa A. B., Nascimento M. T., Froment G. S., Soares R. P., Morgado F. N., Conceição-Silva F., et al. (2009). Leishmania amazonensis promastigotes induce and are killed by neutrophil extracellular traps. Proc. Natl. Acad. Sci. U.S.A. 106 6748–6753. 10.1073/pnas.0900226106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halverson T. W., Wilton M., Poon K. K., Petri B., Lewenza S. (2015). DNA is an antimicrobial component of neutrophil extracellular traps. PLoS Pathog. 11:e1004593 10.1371/journal.ppat.1004593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herwald H., Cramer H., Mörgelin M., Russell W., Sollenberg U., Norrby-Teglund A., et al. (2004). M protein, a classical bacterial virulence determinant, forms complexes with fibrinogen that induce vascular leakage. Cell 116 367–379. 10.1016/S0092-8674(04)00057-1 [DOI] [PubMed] [Google Scholar]
- Hong W., Juneau R. A., Pang B., Swords W. E. (2009). Survival of bacterial biofilms within neutrophil extracellular traps promotes nontypeable Haemophilus influenzae persistence in the chinchilla model for otitis media. J. Innate Immun. 1 215–224. 10.1159/000205937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenne C. N., Wong C. H., Zemp F. J., McDonald B., Rahman M. M., Forsyth P. A., et al. (2013). Neutrophils recruited to sites of infection protect from virus challenge by releasing neutrophil extracellular traps. Cell Host Microbe. 13 169–180. 10.1016/j.chom.2013.01.005 [DOI] [PubMed] [Google Scholar]
- Juneau R. A., Stevens J. S., Apicella M. A., Criss A. K. (2015). A thermonuclease of Neisseria gonorrhoeae enhances bacterial escape from killing by neutrophil extracellular traps. J. Infect. Dis. 212 316–324. 10.1093/infdis/jiv031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisseleva T., Köckritz-Blickwede M., Reichart D., McGillvray S. M., Wingender G., Kronenberg M., et al. (2011). Fibrocyte-like cells recruited to the spleen support innate and adaptive immune responses to acute injury or infection. J. Mol. Med. 89 997–1013. 10.1007/s00109-011-0756-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaRock C. N., Döhrmann S., Todd J., Corriden R., Olson J., Johannssen T., et al. (2015). Group a streptococcal M1 protein sequesters cathelicidin to evade innate immune killing. Cell Host Microbe 18 471–477. 10.1016/j.chom.2015.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauth X., von Köckritz-Blickwede M., McNamara C. W., Myskowski S., Zinkernagel A. S., Beall B., et al. (2009). M1 protein allows Group A streptococcal survival in phagocyte extracellular traps through cathelicidin inhibition. J. Innate Immun. 1 202–214. 10.1159/000203645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malachowa N., Kobayashi S. D., Freedman B., Dorward D. W., DeLeo F. R. (2013). Staphylococcus aureus leukotoxin GH promotes formation of neutrophil extracellular traps. J. Immunol. 191 6022–6029. 10.4049/jimmunol.1301821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menegazzi R., Decleva E., Dri P. (2012). Killing by neutrophil extracellular traps: fact or folklore? Blood 119 1214–1216. 10.1182/blood-2011-07-364604 [DOI] [PubMed] [Google Scholar]
- Menten-Dedoyart C., Faccinetto C., Golovchenko M., Dupiereux I., Van Lerberghe P. B., Dubois S., et al. (2012). Neutrophil extracellular traps entrap and kill Borrelia burgdorferi sensu stricto spirochetes and are not affected by Ixodes ricinus tick saliva. J. Immunol. 189 5393–5501. 10.4049/jimmunol.1103771 [DOI] [PubMed] [Google Scholar]
- Möllerherm H., Neumann A., Schilcher K., Blodkamp S., Zeitouni N. E., Dersch P., et al. (2015). Yersinia enterocolitica-mediated degradation of neutrophil extracellular traps (NETs). FEMS Microbiol. Lett. 362:fnv192 10.1093/femsle/fnv192 [DOI] [PubMed] [Google Scholar]
- Morita C., Sumioka R., Nakata M., Okahashi N., Wada S., Yamashiro T., et al. (2014). Cell wall-anchored nuclease of Streptococcus sanguinis contributes to escape from neutrophil extracellular trap-mediated bacteriocidal activity. PLoS ONE 9:e103125 10.1371/journal.pone.0103125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narasaraju T., Yang E., Samy R. P., Ng H. H., Poh W. P., Liew A. A., et al. (2011). Excessive neutrophils and neutrophil extracellular traps contribute to acute lung injury of influenza pneumonitis. Am. J. Pathol. 179 199–210. 10.1016/j.ajpath.2011.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oehmcke S., Mörgelin M., Herwald H. (2009). Activation of the human contact system on neutrophil extracellular traps. J. Innate. Immun. 1 225–230. 10.1159/000203700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papayannopoulos V., Staab D., Zychlinsky A. (2011). Neutrophil elastase enhances sputum solubilization in cystic fibrosis patients receiving DNase therapy. PLoS ONE. 6:e28526 10.1371/journal.pone.0028526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilsczek F. H., Salina D., Poon K. K., Fahey C., Yipp B. G., Sibley C. D., et al. (2010). A novel mechanism of rapid nuclear neutrophil extracellular trap formation in response to Staphylococcus aureus. J. Immunol. 185 7413–7425. 10.4049/jimmunol.1000675 [DOI] [PubMed] [Google Scholar]
- Rada B., Jendrysik M. A., Pang L., Hayes C. P., Yoo D. G., Park J. J., et al. (2013). Pyocyanin-enhanced neutrophil extracellular trap formation requires the NADPH oxidase. PLoS ONE 8:e54205 10.1371/journal.pone.0054205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rada B., Leto T. L. (2008). Oxidative innate immune defenses by Nox/Duox family NADPH oxidases. Contrib. Microbiol. 15 164–187. 10.1159/000136357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Kichik V., Mondragón-Flores R., Mondragón-Castelán M., Gonzalez-Pozos S., Muñiz-Hernandez S., Rojas-Espinosa O., et al. (2009). Neutrophil extracellular traps are induced by Mycobacterium tuberculosis. Tuberculosis 89 29–37. 10.1016/j.tube.2008.09.009 [DOI] [PubMed] [Google Scholar]
- Reid S. D., Hong W., Dew K. E., Winn D. R., Pang B., Watt J., et al. (2009). Streptococcus pneumoniae forms surface-attached communities in the middle ear of experimentally infected chinchillas. J. Infect. Dis. 199 786–794. 10.1086/597042 [DOI] [PubMed] [Google Scholar]
- Röhm M., Grimm M. J., D’Auria A. C., Almyroudis N. G., Segal B. H., Urban C. F. (2014). NADPH oxidase promotes neutrophil extracellular trap formation in pulmonary aspergillosis. Infect. Immun. 82 1766–1777. 10.1128/IAI.00096-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saffarzadeh M., Juenemann C., Queisser M. A., Lochnit G., Barreto G., Galuska S. P., et al. (2012). Neutrophil extracellular traps directly induce epithelial and endothelial cell death: a predominant role of histones. PLoS ONE 7:e32366 10.1371/journal.pone.0032366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saffarzadeh M., Preissner K. T. (2013). Fighting against the dark side of neutrophil extracellular traps in disease: manoeuvres for host protection. Curr. Opin. Hematol. 20 3–9. 10.1097/MOH.0b013e32835a0025 [DOI] [PubMed] [Google Scholar]
- Saitoh T., Komano J., Saitoh Y., Misawa T., Takahama M., Kozaki T., et al. (2012). Neutrophil extracellular traps mediate a host defense response to human immunodeficiency virus-1. Cell Host Microbe 12 109–116. 10.1016/j.chom.2012.05.015 [DOI] [PubMed] [Google Scholar]
- Scharrig E., Carestia A., Ferrer M. F., Cédola M., Pretre G., Drut R., et al. (2015). Neutrophil Extracellular Traps are involved in the innate immune response to infection with Leptospira. PLoS Negl. Trop Dis. 9:e0003927 10.1371/journal.pntd.0003927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schorn C., Janko C., Latzko M., Chaurio R., Schett G., Herrmann M. (2012). Monosodium urate crystals induce extracellular DNA traps in neutrophils, eosinophils, and basophils but not in mononuclear cells. Front. Immunol. 3:27 10.3389/fimmu.2012.0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semeraro F., Ammollo C. T., Morrissey J. H., Dale G. L., Friese P., Esmon N. L., et al. (2011). Extracellular histones promote thrombin generation through platelet-dependent mechanisms: involvement of platelet TLR2 and TLR4. Blood 118 1952–1961. 10.1182/blood-2011-03-343061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seper A., Hosseinzadeh A., Gorkiewicz G., Lichtenegger S., Roier S., Leitner D. R., et al. (2013). Vibrio cholerae evades neutrophil extracellular traps by the activity of two extracellular nucleases. PLoS Pathog. 9:e1003614 10.1371/journal.ppat.1003614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanthalingam S., Srikumaran S. (2009). Intact signal peptide of CD18, the beta-subunit of beta2-integrins, renders ruminants susceptible to Mannheimia haemolytica leukotoxin. Proc. Natl. Acad. Sci. U.S.A. 106 15448–15453. 10.1073/pnas.0906775106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short K. R., von Köckritz-Blickwede M., Langereis J. D., Chew K. Y., Job E. R., Armitage C. W., et al. (2014). Antibodies mediate formation of neutrophil extracellular traps in the middle ear and facilitate secondary pneumococcal otitis media. Infect. Immun. 82 364–370. 10.1128/IAI.01104-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaan A. N., Henry T., van Rooijen W. J., Perret M., Badiou C., Aerts P. C., et al. (2013). The staphylococcal toxin Panton-Valentine Leukocidin targets human C5a receptors. Cell Host Microbe 13 584–594. 10.1016/j.chom.2013.04.006 [DOI] [PubMed] [Google Scholar]
- Uchiyama S., Döhrmann S., Timmer A. M., Dixit N., Ghochani M., Bhandari T., et al. (2015). Streptolysin o rapidly impairs neutrophil oxidative burst and antibacterial responses to group a Streptococcus. Front. Immunol. 6:581 10.3389/fimmu.2015.00581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urban C. F., Ermert D., Schmid M., Abu-Abed U., Goosmann C., Nacken W., et al. (2009). Neutrophil extracellular traps contain calprotectin, a cytosolic protein complex involved in host defense against Candida albicans. PLoS Pathog. 5:e1000639 10.1371/journal.ppat.1000639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villanueva E., Yalavarthi S., Berthier C. C., Hodgin J. B., Khandpur R., Lin A. M., et al. (2011). Netting neutrophils induce endothelial damage, infiltrate tissues, and expose immunostimulatory molecules in systemic lupus erythematosus. J. Immunol. 187 538–552. 10.4049/jimmunol.1100450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Köckritz-Blickwede M., Nizet V. (2009). Innate immunity turned inside-out: antimicrobial defense by phagocyte extracellular traps. J. Mol. Med. 87 775–783. 10.1007/s00109-009-0481-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Köckritz-Blickwede M., von Goldmann O., Thulin P., Heinemann K., Norrby-Teglund A., Rohde M., et al. (2008). Phagocytosis-independent antimicrobial activity of mast cells by means of extracellular trap formation. Blood 111 3070–3080. 10.1182/blood-2007-07-104018 [DOI] [PubMed] [Google Scholar]
- Wardini A. B., Guimarães-Costa A. B., Nascimento M. T., Nadaes N. R., Danelli M. G., Mazur C., et al. (2010). Characterization of neutrophil extracellular traps in cats naturally infected with feline leukemia virus. J. Gen. Virol. 91 259–264. 10.1099/vir.0.014613-0 [DOI] [PubMed] [Google Scholar]
- Wartha F., Beiter K., Albiger B., Fernebro J., Zychlinsky A., Normark S., et al. (2007). Capsule and D-alanylated lipoteichoic acids protect Streptococcus pneumoniae against neutrophil extracellular traps. Cell Microbiol. 9 1162–1171. 10.1111/j.1462-5822.2006.00857.x [DOI] [PubMed] [Google Scholar]
- Wong K. W., Jacobs W. R., Jr. (2013). Mycobacterium tuberculosis exploits human interferon γ to stimulate macrophage extracellular trap formation and necrosis. J. Infect. Dis. 208 109–119. 10.1093/infdis/jit097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yipp B. G., Petri B., Salina D., Jenne C. N., Scott B. N., Zbytnuik L. D., et al. (2012). Infection-induced NETosis is a dynamic process involving neutrophil multitasking in vivo. Nat. Med. 18 1386–1393. 10.1038/nm.2847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young R. L., Malcolm K. C., Kret J. E., Caceres S. M., Poch K. R., Nichols D. P., et al. (2011). Neutrophil extracellular trap (NET)-mediated killing of Pseudomonas aeruginosa: evidence of acquired resistance within the CF airway, independent of CFTR. PLoS ONE 6:e23637 10.1371/journal.pone.0023637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yousefi S., Gold J. A., Andina N., Lee J. J., Kelly A. M., Kozlowski E., et al. (2008). Catapult-like release of mitochondrial DNA by eosinophils contributes to antibacterial defense. Nat. Med. 14 949–953. 10.1038/nm.1855 [DOI] [PubMed] [Google Scholar]
- Yousefi S., Mihalache C., Kozlowski E., Schmid I., Simon H. U. (2009). Viable neutrophils release mitochondrial DNA to form neutrophil extracellular traps. Cell Death Differ. 16 1438–1444. 10.1038/cdd.2009.96 [DOI] [PubMed] [Google Scholar]
- Zinkernagel A. S., Timmer A. M., Pence M. A., Locke J. B., Buchanan J. T., Turner C. E., et al. (2008). The IL-8 protease SpyCEP/ScpC of group A Streptococcus promotes resistance to neutrophil killing. Cell Host Microbe 4 170–178. 10.1016/j.chom.2008.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]